Abstract
Aim
The purpose of this study is to detail the course of substance use disorders (SUDs) over 10 years of prospective follow-up among patients with borderline personality disorder (BPD) and axis II comparison subjects.
Design
This study uses data from the McLean Study of Adult Development (MSAD), a multifaceted study of the longitudinal course of BPD using reliable repeated measures administered every two years over a decade of prospective follow-up.
Setting
All subjects were initially inpatients at McLean Hospital in Belmont Massachusetts.
Participants
A total of 290 patients with BPD and 72 axis II comparison subjects were assessed at baseline and five waves of follow-up.
Measurements
The Structured Clinical Interview for DSM-III-R Axis I Disorders (SCID-I), the Revised Diagnostic Interview for Borderlines (DIB-R), and the Diagnostic Interview for DSM-III-R Personality Disorders (DIPD-R) were administered six times. Generalized estimating equations were used to assess longitudinal prevalence of SUDs. Kaplan–Meier analyses were used to assess time-to-remission, recurrence, and new onsets of SUDs.
Results
The prevalence of SUDs among borderline patients and axis II comparison subjects declined significantly over time, while remaining significantly more common among those with BPD. Over 90% of borderline patients meeting criteria for a SUD at baseline experienced a remission by 10-year follow-up. Recurrences and new onsets of SUDs were less common (35-40% and 21-23%).
Conclusions
Remissions of alcohol and drug abuse/dependence among borderline patients are both common and relatively stable. Results also suggest that new onsets of these disorders are less common than might be expected.
Clinical experience suggests that substance use disorders (SUDS) are common among patients with borderline personality disorder (BPD). Cross-sectional studies have found that 23-84% of borderline patients (median=65.1%) report meeting criteria for any substance use disorder [1-7]. Cross-sectional studies have also found that 23.8-66% of borderline patients report meeting criteria for alcohol abuse or dependence (median=47%) [5-13] and 19-87% report meeting criteria for drug abuse or dependence (median=44.1) [5-13].
In addition, four longitudinal studies have assessed the prevalence of substance use disorders in samples of criteria-defined borderline patients [14-17] Two of these studies were large-scale, follow-back studies of the long-term course of BPD in former inpatients [14,15]. The first of these studies was Stone’s study of borderline patients who had initially been hospitalized at the New York State Psychiatric Institute [14]. It was found that 14.7% met criteria for alcoholism and 45.5% met criteria for drug abuse during the years since discharge (mean of 16 years). The second of these studies was Paris’ study of former inpatients at the Jewish General Hospital in Montreal, Canada [15]. At a mean of 27 years of follow-up, it was found that 4.7% had active substance abuse.
The other two studies were prospective follow-up studies of former inpatients [16,17]. Links and his colleagues assessed the point prevalence of alcohol and drug use disorders at a mean of seven years after discharge from the psychiatric unit of one of four general hospitals in Ontario, Canada [16]. It was found that 7.0% of the borderline patients met criteria for alcoholism at the time of the interview and 5.3% met criteria for drug abuse at this point in time.
The prevalence of alcohol abuse/dependence and drug abuse/dependence was studied over six years of prospective follow-up in the McLean Study of Adult Development (MSAD) [17]. It was found that the prevalence of both alcohol (50.3% at baseline and 11.4% at six-year follow-up) and drug (46.6% at baseline and 12.9% at six-year follow-up) use disorders declined significantly over time in patients with BPD. However, the prevalence of alcohol abuse/dependence but not drug abuse/dependence remained significantly higher among borderline patients than axis II comparison subjects. In addition, it was found that co-occurring substance use disorders slowed time-to-remission of BPD more than any other type of axis I disorder, including major depression and PTSD.
The current study, which is an extension of the MSAD study mentioned above, is the first longitudinal study to assess the prevalence of these disorders over 10 years of prospective follow-up in a large and well-defined sample of borderline patients and axis II comparison subjects. It is also the first study to assess time-to-remission, time-to-recurrence, and time-to-new onset of each of these substance use disorders in borderline patients (followed prospectively for a decade).
Methods
The methodology of this study has been described in detail elsewhere [18]. Briefly, all subjects were initially inpatients at McLean Hospital in Belmont, Massachusetts. Each patient was first screened to determine that he or she: 1) was between the ages of 18-35; 2) had a known or estimated IQ of 71 or higher; 3) had no history or current symptoms of schizophrenia, schizoaffective disorder, bipolar I disorder, or an organic condition that could cause psychiatric symptoms; and 4) was fluent in English.
After the study procedures were explained, written informed consent was obtained. Each patient then met with a masters-level interviewer blind to the patient’s clinical diagnoses for a thorough diagnostic assessment. Three semistructured diagnostic interviews were administered. These diagnostic interviews were: 1) the Structured Clinical Interview for DSM-III-R Axis I Disorders (SCID-I) [19], 2) the Revised Diagnostic Interview for Borderlines (DIB-R) [20], and 3) the Diagnostic Interview for DSM-III-R Personality Disorders (DIPD-R) [21]. The inter-rater and test-retest reliability of all three of these measures have been found to be good-excellent [22,23].
At each of five follow-up assessments, separated by 24 months, axis I and II psychopathology was reassessed via interview methods similar to the baseline procedures by staff members blind to baseline diagnoses. After informed consent was obtained, our diagnostic battery was readministered (with the SCID I focusing on the past two years and not as at baseline, lifetime axis I psychopathology). The follow-up interrater reliability (within one generation of follow-up raters) and follow-up longitudinal reliability (from one generation of raters to the next) of these three measures have also been found to be good-excellent [22,23].
Definition of Remission, Recurrence, and New Onset of SUDs
We defined remission as any two-year period (any follow-up period) in which the criteria for alcohol abuse/dependence or drug abuse/dependence were no longer met. We chose this length of time at the start of the study to mirror our definitions of remission of BPD and its constituent symptoms [18]. In addition, a recurrence or new onset was defined as any one-month period in which the criteria for alcohol abuse/dependence or drug abuse/dependence were met.
Statistical Analyses
Generalized estimating equations, with diagnosis and time of follow-up as main effects, were used in longitudinal analyses of prevalence data. Tests of diagnosis by time interactions were conducted. These analyses modeled the log prevalence, yielding an adjusted risk ratio (RR) and 95% confidence interval (95%CI) for diagnosis and time. Gender was also included in these analyses as a covariate as borderline patients were significantly more likely than axis II comparison subjects to be female. Alpha was set at the p<0.05 level, two-tailed.
The Kaplan-Meier product-limit estimator (of the survival function) was used to assess time-to-remission of substance use disorders, time-to-recurrence of these disorders, and time-to-new onsets. We defined time-to-remission of each of the two substance use disorders studied as the follow-up period at which remission was first achieved. Thus, possible values for this time-to-remission measure were 2, 4, 6, 8, or 10 years, with time=2 years for persons first achieving a remission of the disorders studied during the first follow-up period, time=4 years for persons first achieving such a remission during the second follow-up period, etc. We defined time-to-new onset in a like manner. However it should be noted that we were studying two separate types of new onset. One is a new onset over the years of follow-up that has as its risk set all subjects who did not meet current (past month) criteria for alcohol or drug abuse/dependence at baseline. The other is a lifetime new onset and only includes in its risk set those who did not have a lifetime diagnosis of alcohol or drug abuse/dependence at baseline. We defined time-to-recurrence in a somewhat different manner (i.e., the number of years after a remission had been achieved that recurrence first occurred). Thus, time-to-recurrences were 2, 4, 6, or 8 years after first remission.
Results
Two hundred and ninety patients met both DIB-R and DSM-III-R criteria for BPD and 72 met DSM-III-R criteria for at least one non-borderline axis II disorder (and neither criteria set for BPD). Of these 72 comparison subjects, 4% met DSM-III-R criteria for an odd cluster personality disorder, 33% met DSM-III-R criteria for an anxious cluster personality disorder, 18% met DSM-III-R criteria for a non-borderline dramatic cluster personality disorder, and 53% met DSM-III-R criteria for personality disorder not otherwise specified (which was operationally defined in the DIPD-R as meeting all but one of the required number of criteria for at least two of the 13 axis II disorders described in DSM-III-R).
Baseline demographic data have been reported before [18]. Briefly, 77.1% (N=279) of the subjects were female and 87% (N=315) were white. The average age of the subjects was 27 years (SD=6.3), the mean socioeconomic status was 3.3 (SD=1.5) (where 1=highest and 5=lowest) [24], and their mean GAF score was 39.8 (SD=7.8) (indicating major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood).
In terms of continuing participation, 90.4% (N=309) of surviving patients were re-interviewed at all five follow-up assessment points. More specifically, 91.9% of surviving borderline patients (249/271) and 84.5% of surviving axis II comparison subjects (60/71) were evaluated six times (baseline and five follow-up periods).
Table 1 details the prevalence of substance use disorders reported by borderline patients and axis II comparison subjects over 10 years of prospective follow-up. As can be seen, a significantly higher percentage of borderline patients than axis II comparison subjects reported experiencing any substance use disorder, alcohol abuse/dependence, drug abuse/dependence, and both alcohol and drug abuse/dependence. For both borderline patients and axis II comparison subjects, the rates of these disorders declined significantly over time. No interaction between diagnosis and time was found to be significant, indicating that the rates of decline were similar for both groups of patients.
Table 1.
Prevalence of Substance Use Disorders among Borderline Patients and Axis II Comparison Subjects Over 10 Years of Prospective Follow-up
| Borderline Patients | Axis II Comparison Subjects | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BL (N=290) | 2 Yr FU (N=275) | 4 Yr FU (N=269) | 6 Yr FU (N=264) | 8 Yr FU (N=255) | 10 Yr FU (N=249) | BL (N=72) | 2 Yr FU (N=67) | 4 Yr FU (N=64) | 6 Yr FU (N=63) | 8 Yr FU (N=61) | 10 Yr FU (N=60) | Risk Ratio Diagnosis Time | 95% CI Diagnosis Time | |
| Any Substance Abuse/Dependence | 62.1 (N=180) | 29.8 (N=82) | 23.8 (N=64) | 18.9 (N=50) | 15.3 (N=39) | 13.7 (N=34) | 45.8 (N=33) | 14.9 (N=10) | 10.9 (N=7) | 7.9 (N=5) | 13.1 (N=8) | 8.3 (N=5) | 1.65 0.16 | 1.28, 2.14 0.19, 0.23 |
| Any Alcohol Abuse/Dependence | 50.3 (N=146) | 20.4 (N=56) | 14.5 (N=39) | 11.4 (N=30) | 8.6 (N=22) | 8.8 (N=22) | 38.9 (N=28) | 9.0 (N=6) | 7.8 (N=5) | 4.8 (N=3) | 6.6 (N=4) | 1.7 (N=1) | 1.21 0.03 | 0.71, 2.06 0.01, 0.19 |
| Any Drug Abuse/Dependence | 46.6 (N=135) | 20.4 (N=56) | 15.2 (N=41) | 12.9 (N=34) | 9.0 (N=23) | 7.2 (N=18) | 34.7 (N=25) | 10.5 (N=7) | 6.3 (N=4) | 3.2 (N=2) | 8.2 (N=5) | 6.7 (N=4) | 1.62 0.10 | 0.98, 2.69 0.03, 0.39 |
| Both Alcohol and Drug Abuse/Dependence | 34.5 (N=100) | 10.9 (N=30) | 6.0 (N=16) | 5.3 (N=14) | 2.4 (N=6) | 2.4 (N=6) | 27.8 (N=20) | 4.9 (N=3) | 3.1 (N=2) | 0.0 (N=0) | 1.6 (N=1) | 0.0 (N=0) | 1.52 0.02 | 1.04, 2.20 0.01, 0.05 |
P-level results for diagnosis were any substance abuse/dependence, <0.001; any alcohol, .008; any drug, .001; both alcohol and drug, 0.029
P-level results for time were all <0.001
However as the risk ratios (RRs) for diagnosis and time in the table contain more fine grained information, we believe that an example would be useful. As can be seen, about 62% of borderline patients (and about 46% of axis II comparison subjects) had a history of any substance use disorder at the time of their index admission. By the time of their 10-year follow-up, these prevalence rates had declined to about 14% and 8% respectively. The RR of 1.65 indicates that borderline patients were about 1½ times more likely, at any follow-up time, to report experiencing any substance use disorder as axis II comparison subjects. The RR of 0.16 indicates that the chance of experiencing substance abuse or dependence over the course of the study for all subjects considered together decreased by 84% ([1-0.16]×100%).
Figure 1 details the estimated rates of remission, recurrence, and new onsets of alcohol abuse or dependence for borderline patients. As can be seen, about 92% of borderline patients reporting this disorder at baseline (N=48) experienced a remission (N=37) by the time of the 10-year follow-up. In terms of the stability of these remissions, 40% of borderline patients reporting a remission of alcohol abuse or dependence reported a recurrence (N=13) of this disorder. As can also be seen, about 23% of borderline patients who did not report having alcohol abuse/dependence at baseline (N=242) reported a new onset (N=48) of this disorder. (Note that the estimated rates of remission, recurrence, and new onsets cannot be directly determined using the numbers presented above because of censoring [i.e., subjects lost to follow-up].)
Figure 1. Rates of Remission, Recurrence, and New Onsets of Alcohol Abuse/Dependence among Borderline Patients over Ten Years of Prospective Follow-up.
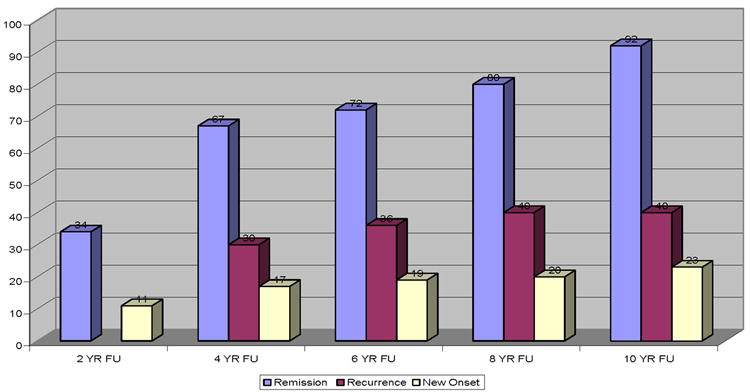
Note: Since a recurrence can only occur after a remission, there is no possibility of a recurrence occurring at the 2-year follow up. Even though recurrences are displayed in this figure at the 4, 6, 8, and 10-year follow-up periods, these recurrences are actually occurring 2, 4, 6, and 8 years after the remission.
Figure 2 details the rates of remission, recurrence, and new onsets of drug abuse or dependence among borderline patients. As can be seen, about 95% of borderline patients reporting this disorder at baseline (N=51) experienced a remission (N=41) by the time of the 10-year follow-up. In terms of the stability of these remissions, 35% of borderline patients reporting a remission of drug abuse or dependence reported a recurrence (N=10) of this disorder. As can also be seen, about 21% of borderline patients who did not report having drug abuse/dependence at baseline (N=239) reported a new onset (N=44) of this disorder. (As noted above, estimated rates of remission, recurrence, and new onsets cannot be determined using the numbers presented above because of censoring [i.e., subjects lost to follow-up].)
Figure 2. Rates of Remission, Recurrence, and New Onsets of Drug Abuse/Dependence among Borderline Patients over Ten Years of Prospective Follow-up.
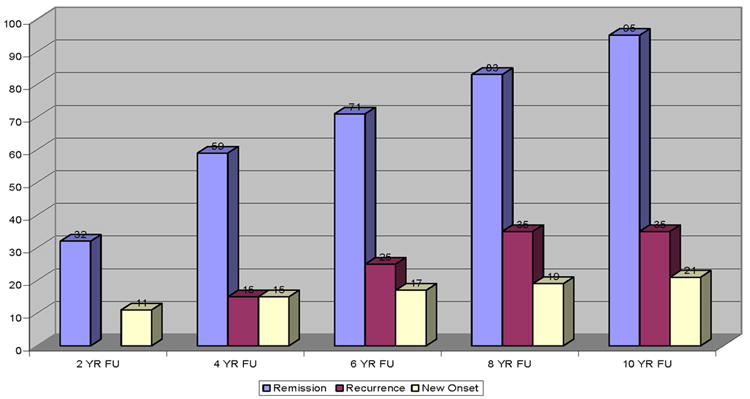
Note: Since a recurrence can only occur after a remission, there is no possibility of a recurrence occurring at the 2-year follow up. Even though recurrences are displayed in this figure at the 4, 6, 8, and 10-year follow-up periods, these recurrences are actually occurring 2, 4, 6, and 8 years after the remission.
However, it should be noted that 60.4% (29/48) of borderline patients reporting a new onset of alcohol abuse or dependence during one of the study’s five follow-up periods actually had met lifetime (but not current) criteria for alcohol abuse or dependence at baseline. In a like manner, 56.8% (25/44) of borderline patients reporting a new onset of drug abuse/dependence actually had met lifetime (but not current) criteria for drug abuse or dependence at baseline. Looked at another way, only 19 borderline patients (6.6%) developed a totally new problem with alcohol over the 10 years of follow-up and the exact same number and percent developed a totally new problem with drugs over the decade they were followed. It should also be noted that only three of these 38 subjects (7.9%) met criteria for both alcohol and drug abuse/dependence over the years of follow-up
Discussion
Five main findings have emerged from the results of this study. The first finding is that the prevalence of each of these substance use disorders, which was about almost two times more common than the prevalence of alcohol abuse/dependence [25] and almost five times the prevalence of drug abuse/dependence [26] in the general population, declined significantly over time for borderline patients (and axis II comparison subjects). More specifically, the prevalence of any substance abuse/dependence declined 84% for borderline patients, the prevalence of alcohol abuse/dependence declined 97%, the prevalence of drug abuse/dependence declined 90%, and the prevalence of both alcohol and drug abuse/dependence declined 98%. These findings are consistent with and extend the findings of our six-year follow-up study of this sample [17].
The second finding is that both alcohol abuse/dependence and drug abuse/dependence were significantly more common among borderline patients than among axis II comparison subjects. More specifically, borderline patients were 21% more likely than axis II comparison subjects to report alcohol abuse/dependence and 62% more likely to report drug abuse/dependence. All told, borderline patients were 65% more likely than axis II comparison subjects to report any substance abuse/dependence and 52% more likely than axis II comparison subjects to report both alcohol and drug abuse/dependence. These findings too are consistent with and extend the findings of our six-year follow-up study of this sample [17].
The third finding is that over 90% of those borderline patients meeting criteria for alcohol abuse/dependence and drug abuse/dependence at baseline experienced a remission by the time of the 10-year follow-up. This is a new finding and lends hope to those treating substance use disorders in patients with BPD. Not surprisingly, these remission rates are substantially higher than those found in 8-10 year follow-up studies of subjects with primary substance use disorders [27,28]. It is our impression that many of these cases involved substance abuse rather than substance dependence—a pattern of disordered drinking that is probably less severe than that found in those with primary substance use disorders.
The fourth finding is that recurrences of alcohol abuse/dependence and drug abuse/dependence were less common than remissions among borderline patients with a recent history of abusing substances. More specifically, 40% of borderline patients whose alcohol disorder remitted later experienced a recurrence of problematic drinking. In a similar vein, 35% of borderline patients whose drug disorder remitted later experienced a recurrence of drug abuse or dependence. This finding too is new but tempers somewhat the optimism associated with the high rates of remission discussed above. Interestingly, our rate of recurrence of alcohol abuse/dependence was almost identical to the 45% found by Vaillant in an eight-year follow-up study of patients initially hospitalized for alcohol withdrawal [29]. However, our recurrence rates of alcohol and drug abuse/dependence were substantially lower than those found in a short-term follow-up study (18 months) of patients initially hospitalized with alcohol and /or drug dependence [30]. It is not surprising that recurrence rates of those with BPD and secondary SUDS would be lower than the recurrence rates of those initially hospitalized for alcohol or drug dependence.
The fifth finding is that new onsets of alcohol abuse/dependence and drug abuse/dependence were relatively uncommon among borderline patients who did not meet criteria for alcohol or drug abuse at baseline. More specifically, 20% of borderline patients who did not meet criteria for alcohol abuse or dependence at baseline later developed a new onset of problematic drinking and 21% of borderline patients who did not meet criteria for drug abuse/dependence at baseline later developed a new onset of drug abuse or dependence. These rates are similar to those found in a seven-year follow-up study of new onsets of SUDS in patients with BPD [31]. It is also consistent with the rate of new onsets of alcohol abuse/dependence found in a 10-year follow-up study of non-problem drinkers [32].
However, it is a new finding that about 60% of borderline patients with a new onset of alcohol abuse or drug abuse over the years of follow-up had actually had a lifetime diagnosis of the same disorder prior to their entry into the study. This suggests that these disorders represent a recurrent but intermittent problem for some borderline patients. They also suggest that a truly new SUD is uncommon for borderline patients followed prospectively after an initial inpatient hospitalization, a finding that should be encouraging for clinicians treating borderline inpatients who have no history of substance abuse.
Taken together, the results of this study suggest that there might be three subtypes of borderline patients: those who never have had a substance use problem, those who have a time-limited problem that they overcome, and those with an intermittent problem with alcohol and/or drugs. Future studies are needed to determine the ways in which these types of patients are similar and different. Future studies are also needed to determine what treatment works best for different types of substance abusing borderline patients. Dialectical behavior therapy (DBT) has been found to be more effective than a 12-step program plus the supportive strategy of validation for women with BPD and opioid dependence [33]. However, it is not clear if DBT would be the most efficacious or cost-effective treatment for borderline patients with a history of abusing rather than being dependent on alcohol or drugs. It is also not clear if borderline patients with an alcohol problem would respond to the same treatment as a borderline patient with drug abuse or dependence.
This study has three main limitations. The first is that all of the patients were seriously ill inpatients at the start of the study. A second limitation is that about 90% of those in both patient groups were in individual therapy and taking psychotropic medications at baseline and about 70% were participating in each of these outpatient modalities during each follow-up period [34]. Thus, it is difficult to know if these results would generalize to a less disturbed group of patients or people meeting criteria for BPD who are not in treatment. A third limitation is that we did not differentiate between abuse and dependence. Such a distinction might well have had a clinically meaningful impact on our rates of remission, recurrence, and new onsets.
The results of this study may lend encouragement to clinicians treating patients with borderline personality disorder and co-occurring substance use disorders. Clearly, sustained remissions of two years or more are common and totally new onsets of a substance use problem are rare. However, the 30-40% rates of recurrence found in this study temper somewhat the optimism engendered by our high rates of remission and relatively low rates of completely new onsets in patients without a prior history of substance use disorders.
Acknowledgments
This study was supported by NIMH grants MH47588 and MH62169 and NIDA grant K24 DA022288.
Footnotes
The authors report no conflict of interest.
References
- 1.Pope HG, Jonas JM, Hudson JI, Cohen BM, Gunderson JG. The validity of DSM-III borderline personality disorder A phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry. 1983;40:23–30. doi: 10.1001/archpsyc.1983.01790010025003. [DOI] [PubMed] [Google Scholar]
- 2.Andrulonis PA, Vogel NG. Comparison of borderline personality subcategories to schizophrenic and affective disorders. Brit J Psychiat. 1984;144:358–363. doi: 10.1192/bjp.144.4.358. [DOI] [PubMed] [Google Scholar]
- 3.Frances A, Clarkin JF, Gilmore M, Hurt SW, Brown R. Reliability of criteria of borderline personality disorder: a comparison of DSM-III and the Diagnostic Interview for Borderline Patients. Am J Psychiatry. 1984;141:1080–1084. doi: 10.1176/ajp.141.9.1080. [DOI] [PubMed] [Google Scholar]
- 4.Akiskal HS, Chen SE, Davis GC, Puzantian VR, Kashgarian M, Bolinger JM. Borderline: an adjective in search for a noun. J Clin Psychiatry. 1985;46:41–48. [PubMed] [Google Scholar]
- 5.Zanarini MC, Gunderson JG, Frankenburg FR. Axis I phenomenology of borderline personality disorder. Compr Psychiatry. 1989;30:149–156. doi: 10.1016/0010-440x(89)90067-9. [DOI] [PubMed] [Google Scholar]
- 6.Zanarini MC, Frankenburg FR, Dubo E, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155:1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman M, Mattia JI. Axis I diagnostic comorbidity and borderline personality disorder. Compr Psychiatry. 1999;40:245–252. doi: 10.1016/s0010-440x(99)90123-2. [DOI] [PubMed] [Google Scholar]
- 8.Perry JC, Cooper SH. Psychodynamics, symptoms, and outcome in borderline and antisocial personality disorders and bipolar type II affective disorder. In: McGlashan TH, editor. The Borderline: Current Empirical Research. Washington, DC: American Psychiatric Press; 1985. pp. 19–41. [Google Scholar]
- 9.Links PS, Steiner M, Offord DR, Eppel A. Characteristics of borderline personality disorder: a Canadian study. Can J Psychiatry. 1988;33:336–340. doi: 10.1177/070674378803300504. [DOI] [PubMed] [Google Scholar]
- 10.Swartz MS, Blazer DG, George LK, Winfield I, Zakris J, Dye E. Identification of borderline personality disorder with the NIMH Diagnostic Interview Schedule. Am J Psychiatry. 1989;146:200–205. doi: 10.1176/ajp.146.2.200. [DOI] [PubMed] [Google Scholar]
- 11.Coid JW. An affective syndrome in psychopaths with borderline personality disorder? Br J Psychiatry. 1993;162:641–650. doi: 10.1192/bjp.162.5.641. [DOI] [PubMed] [Google Scholar]
- 12.Shearer SL. Dissociative phenomena in women with borderline personality disorder. Am J Psychiatry. 1994;151:1324–1328. doi: 10.1176/ajp.151.9.1324. [DOI] [PubMed] [Google Scholar]
- 13.McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, et al. The collaborative longitudinal personality disorders study: baseline axis I/II and axis II/II co-occurrence. Acta Psychiatr Scand. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- 14.Stone MH. The fate of borderline patients: successful outcome and psychiatric practice. New York, NY: The Guilford Press; 1990. [Google Scholar]
- 15.Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry. 2001;42:482–487. doi: 10.1053/comp.2001.26271. [DOI] [PubMed] [Google Scholar]
- 16.Links PS, Heslegrave RJ, Mitton JE, Van Reekum R, Patrick J. Borderline psychopathology and recurrences of clinical disorders. J Nerv Ment Dis. 1995;183:582–586. doi: 10.1097/00005053-199509000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry. 2004;161:2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- 18.Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry. 2003;160:274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- 19.Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R (SCID). I: History, rational, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 20.Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The Revised Diagnostic Interview for Borderlines: discriminating BPD from other axis II disorders. J Pers Disord. 1989;3:10–18. [Google Scholar]
- 21.Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG. The Diagnostic Interview for Personality Disorders: inter-rater and test-retest reliability. Compr Psychiatry. 1987;28:467–480. doi: 10.1016/0010-440x(87)90012-5. [DOI] [PubMed] [Google Scholar]
- 22.Zanarini MC, Frankenburg FR, Vujanovic AA. The inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines (DIB-R) J Pers Disord. 2002;16:270–276. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- 23.Zanarini MC, Frankenburg FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Compr Psychiatry. 2001;42:369–374. doi: 10.1053/comp.2001.24556. [DOI] [PubMed] [Google Scholar]
- 24.Hollingshead AB. Two factor index of social position. New Haven, CT: Yale University; 1957. [Google Scholar]
- 25.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 26.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 27.Hser Y, Hoffman V, Grella CE, Anglin D. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry. 2001;58:503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- 28.Vaillant GE, Clark W, Cyrus C, Milofsky ES, Kopp J, Wulsin VW, et al. Prospective study of alcoholism treatment: eight-year follow-up. Am J Med. 1983;75:455–463. doi: 10.1016/0002-9343(83)90349-2. [DOI] [PubMed] [Google Scholar]
- 29.Vaillant GE. A long-term follow-up of male alcohol abuse. Arch Gen Psychiatry. 1996;53:243–249. doi: 10.1001/archpsyc.1996.01830030065010. [DOI] [PubMed] [Google Scholar]
- 30.Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002;59:375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- 31.Walter M, Gunderson JG, Zanarini MC, Sanislow CA, Grilo CM, McGlashan TH, et al. New onsets of substance use disorders in borderline personality disorder over 7 years of follow-ups: findings from the Collaborative Longitudinal Personality Disorders Study. Addiction. 2009;104:97–103. doi: 10.1111/j.1360-0443.2008.02413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schutte KK, Nichols KA, Brennan PI, Moos RH. A ten-year follow-up of older former problem drinkers: Risk of relapse and implications of successfully sustained remission. J Stud Alcohol. 2003;64:367–374. doi: 10.15288/jsa.2003.64.367. [DOI] [PubMed] [Google Scholar]
- 33.Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, et al. Dialectical behavioral therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;67:13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- 34.Zanarini MC, Frankenburg FR, Hennen J, Silk KR. Mental health service utilization of borderline patients and axis II comparison subjects followed prospectively for six years. J Clin Psychiatry. 2004;65:28–36. doi: 10.4088/jcp.v65n0105. [DOI] [PubMed] [Google Scholar]


