Abstract
NF-κB–inducing kinase (NIK) is an essential upstream kinase in noncanonical NF-κB signaling. NIK-dependent NF-κB activation downstream of several TNF receptor family members mediates lymphoid organ development and B cell homeostasis. Peripheral T cell populations are normal in the absence of NIK, but the role of NIK during in vivo T cell responses to antigen has been obscured by other developmental defects in NIK-deficient mice. Here, we have identified a T cell–intrinsic requirement for NIK in graft-versus-host disease (GVHD), wherein NIK-deficient mouse T cells transferred into MHC class II mismatched recipients failed to cause GVHD. Although NIK was not necessary for antigen receptor signaling, it was absolutely required for costimulation through the TNF receptor family member OX40 (also known as CD134). When we conditionally overexpressed NIK in T cells, mice suffered rapid and fatal autoimmunity characterized by hyperactive effector T cells and poorly suppressive Foxp3+ Tregs. Together, these data illuminate a critical T cell–intrinsic role for NIK during immune responses and suggest that its tight regulation is critical for avoiding autoimmunity.
Introduction
Naive T cells require several signals to become activated in vivo. TCR stimulation and costimulation via CD28 are required for cell division and IL-2 production, but in the absence of infection or damage, these 2 signals are insufficient for an effective T cell response, and T cells die or become anergic after initial proliferation (1). Additional costimulation (signal 3) is required for continued clonal expansion, survival, and differentiation into effector subsets, and TNF receptor family members (TNFRs) constitute an important group of costimulatory molecules that relay signal 3 to antigen activated T cells (2). In particular, OX40 (also known as CD134 and TNFRSF4) is critical for optimal CD4+ T cell expansion, survival, differentiation, and memory responses to a variety of infectious and noninfectious immune challenges, including autoimmunity and allogeneic responses in the context of graft-versus-host disease (GVHD) (3).
OX40, like other TNFRs as well as the TCR complex itself, activates NF-κB (3). Activation of NF-κB can be described in terms of 2 interrelated pathways (4). The canonical NF-κB pathway depends on inhibitor of NF-κB kinase (IKK) subunit β, which rapidly phosphorylates inhibitory IκB proteins, leading to their degradation. This releases active dimers composed primarily of p50:RelA or p50:c-rel subunits to translocate to the nucleus and induce proinflammatory gene transcription. In contrast, the noncanonical (also known as alternative) NF-κB pathway depends on accumulation of NF-κB–inducing kinase (NIK) and subsequent phosphorylation of IKK subunit α, which then targets the inhibitory subunit p100 (also known as NF-κB2) for partial degradation, producing the active p52 subunit. In this pathway, gene transcription is mediated primarily by active p52:RelB dimers. Kinetics also distinguish the canonical from the noncanonical NF-κB pathways, in that activation of the canonical pathway is immediate, but its duration short as a result of rapid negative feedback, whereas activation of the noncanonical pathway is more delayed but sustained (4).
While lesions in the canonical NF-κB pathway have devastating effects on the immune system (4), genetic manipulation of the noncanonical NF-κB pathway has more limited effects because of the limited number of receptors that activate this pathway. NIK knockout mice and alymphoplasia (aly) mice, which harbor a naturally occurring loss-of-function mutation in NIK (5), have disorganized lymphoid structure in the spleen and thymus, no LNs, and few peripheral B cells (6). These defects have been attributed to defective signaling by lymphotoxin β receptor (LTβR) and other TNFRs on lymphoid organ stromal cells and lack of survival signals transmitted by B cell activating factor receptor (BAFFR) on peripheral B cells (7–9). In addition, some defects in APC function have been attributed to defective signaling though CD40 (10, 11).
In contrast, steady-state peripheral T cell populations are fairly normal in NIK-deficient mice, and the role of NIK in T cell function remains unclear. Autoimmunity has been reported in aly/aly mice (12), but this appears to be due to a lack of TNFR signaling in thymic epithelial cells that mediate negative selection and development of Tregs (13). Similarly, although aly/aly mice do not reject skin grafts, this was attributed to their lack of LNs, rather than a T cell–intrinsic defect (6, 14). Findings of in vitro investigations of NIK-deficient T cells have been equivocal. Unfractionated aly/aly T cells showed a diminished response to anti-CD3 stimulation, but allogeneic proliferative responses were normal (15), and sorted naive aly/aly T cells were subsequently shown to be hyperresponsive to TCR stimulation in vitro and in vivo (16). In contrast, 3 in vivo studies showed that NIK-deficient T cells fail to induce autoimmune disease in mouse models of arthritis and EAE (17–19).
To explain these contradictory data, we propose that NIK is required for naive T cell responses in vivo by signaling downstream of costimulatory TNFRs that promote acquisition of effector functions and survival after antigen exposure. To test this hypothesis, we used a model of GVHD in which we could isolate effects of donor T cells that do or do not express functional NIK, and in which we could manipulate the level of costimulation. We report here that NIK was essential for lethal GVHD in a CD4+ T cell–intrinsic manner. Naive NIK-deficient T cells responded normally to TCR stimulation in vitro and to alloantigen in vivo under conditions of low costimulation in which T cells divide but do not differentiate or cause disease. In contrast, NIK was absolutely essential for OX40-mediated costimulation of alloresponsive T cells in vivo, and OX40 activated the NIK-dependent noncanonical NF-κB pathway in primary T cells. Finally, overexpression of NIK in T cells led to an aggressive lethal autoimmunity associated with decreased function of Tregs and effector T cells that are resistant to suppression. We therefore concluded that NIK is essential for T cell function in vivo and that its tight regulation in T cells is crucial to prevent autoimmunity.
Results
NIK-deficient CD4+ T cells do not cause lethal GVHD.
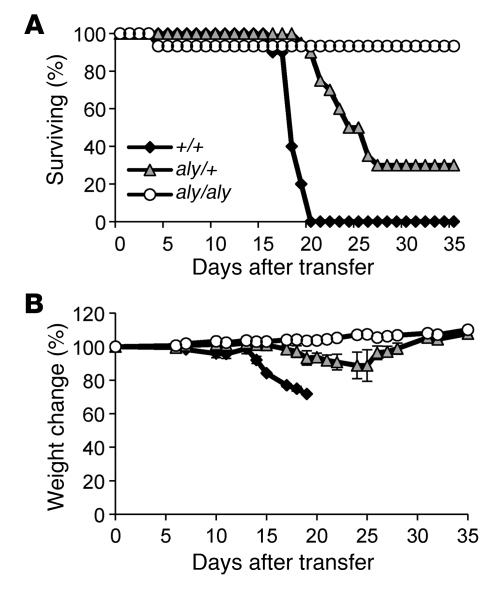
To test whether NIK is required in a T cell–intrinsic manner for allogeneic responses, we sorted naive CD4+ T cells from aly/aly mutant mice or littermate controls and transferred them into sublethally irradiated MHC class II mismatched congenic (H-2bm12×CD45.1)F1 recipients. Transfer of T cells with 2 normal copies of NIK caused lethal GVHD in 100% of recipient mice, which was preceded by rapid weight loss starting 2 weeks after transfer (Figure 1). In stark contrast, aly/aly T cells caused no GVHD lethality or weight loss. Interestingly, recipients of heterozygous aly/+ T cells showed an intermediate phenotype, experiencing delayed disease and a 70% mortality rate. The importance of NIK levels seen here mirrors recent reports showing that loss of a single copy of NIK can rescue TNF receptor–associated factor 2 and TNF receptor–associated factor 3 knockout mice from perinatal lethality (20, 21). The failure of NIK-deficient T cells to induce lethal GVHD is likely a result of poor accumulation of allospecific T cells in the recipients, as illustrated in a separate experiment in which we transferred a smaller, nonlethal number (1 × 105) of naive CD4+ T cells into sublethally irradiated (H-2bm12×CD45.1)F1 recipients. In this case, despite lack of overt disease, control CD4+ T cells accumulated in mismatched recipients, and 10-fold more control CD4+ T cells than aly/aly T cells were recovered from recipient spleens 1 month after transfer (Table 1).
Figure 1. NIK-deficient CD4+ T cells do not cause lethal GVHD.
1 × 106 naive +/+, aly/+, or aly/aly CD4+ T cells were injected intravenously into sublethally irradiated (H-2bm12×CD45.1)F1 recipients. (A) Survival is combined data from 4 independent experiments; each genotype was represented in 2–4 experiments. P < 0.05, +/+ versus aly/+ and aly/+ versus aly/aly; log-rank test. (1 mouse in the aly/aly group died only 4 days after transfer, which is much earlier than GVHD onset in this model). (B) Body weight data (± SEM) are representative of 2 independent experiments.
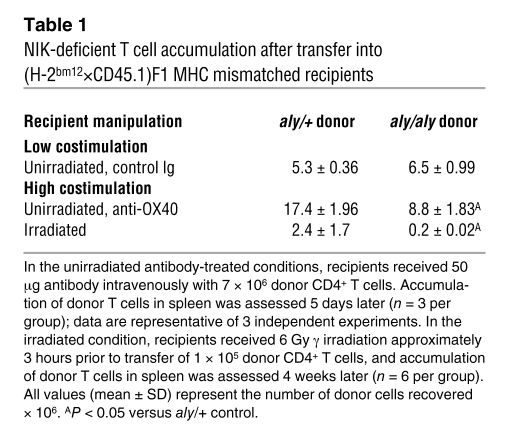
Table 1 .
NIK-deficient T cell accumulation after transfer into (H-2bm12×CD45.1)F1 MHC mismatched recipients
NIK-deficient T cells respond normally to TCR stimulation.
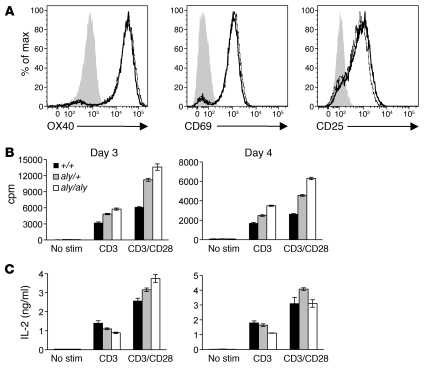
Some reports have found diminished T cell responsiveness to TCR signals in the absence of NIK, which could explain the failure of aly/aly CD4+ T cells to induce GVHD (15). We tested the ability of naive aly/aly and control CD4+ T cells to respond in vitro to TCR stimulation with or without CD28 costimulation. aly/aly and control T cells upregulated OX40, CD69, and CD25 to the same extent (Figure 2A). Moreover, aly/aly T cells proliferated as well as or better than controls in all conditions (Figure 2B). Similarly, with TCR plus CD28 costimulation, aly/aly T cells produced normal amounts of IL-2, and in the absence of CD28 costimulation, aly/aly T cells produced only slightly less IL-2 (Figure 2C). Upon addition of IL-12 to cultures, aly/aly T cells produced IFN-γ at levels comparable to those of control T cells (Supplemental Figure 1; supplemental material available online with this article; doi: 10.1172/JCI44943DS1), which indicates that NIK is not required for Th1 polarization. These results are similar to recent reports that also used sorted naive NIK-deficient CD4+ T cells (16, 19) and suggest that the inability of aly/aly T cells to cause GVHD is not likely to be caused by signaling defects downstream of the TCR.
Figure 2. NIK-deficient CD4+ T cells respond normally to TCR signaling.
Sorted naive T cells (CD4+CD25–CD44lo) were stimulated with plate-bound anti-CD3 with (A–C) or without (B and C) anti-CD28. (A) Upregulation of OX40, CD69, and CD25 was assessed on day 2. Gray represents Ox40–/– (for OX40) or +/+ unstimulated (for CD69 and CD25); thin line represents +/+ stimulated; bold line represents aly/aly stimulated. (B) Proliferation was measured by tritiated thymidine incorporation on days 3 and 4. (C) IL-2 was measured by ELISA of culture supernatants on days 3 and 4. Data (± SD) are representative of 1 (A) or 2 (B and C) independent experiments.
NIK is required for OX40-mediated costimulation of CD4+ T cells.
In B cells and lymphoid organ stromal cells, NIK acts downstream of TNFRs such as BAFFR and LTβR. Activated T cells also express TNFRs that function as important costimulatory molecules, and several, such as OX40, CD30, HVEM, and 4-1BB, have previously been shown to contribute to GVHD in mouse models (22). In particular, OX40 is essential for lethality when B6 CD4+ T cells are transferred into irradiated H-2bm12 recipients (23), and we confirmed that naive Ox40–/– CD4+ T cells did not cause lethal GVHD in our similar model (Supplemental Figure 2). Therefore, we considered the possibility that the inability of NIK-deficient T cells to mediate lethal GVHD might be owing to a requirement for NIK downstream of OX40 and perhaps other TNFRs.
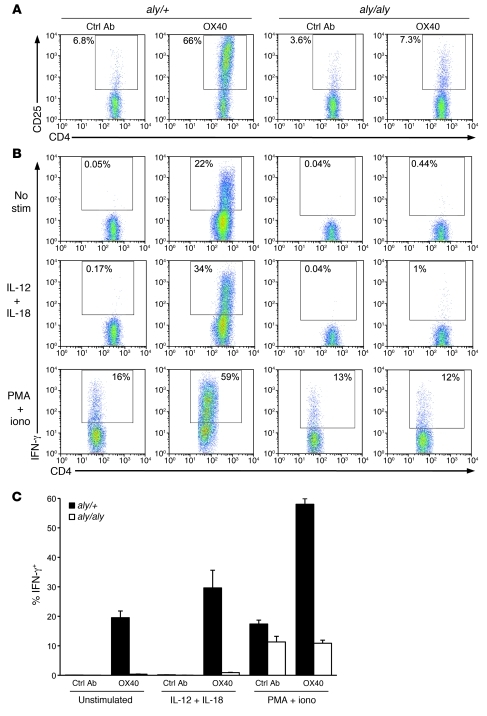
To test this hypothesis, we used a model of GVHD previously described by our lab, in which costimulation by agonist anti-OX40 antibody produces lethal GVHD in unirradiated (H-2bm12×CD45.1)F1 recipients of B6 CD4+ T cells. Without irradiation of recipients and without anti-OX40, donor CD4+ T cells proliferate and accumulate, but are rendered anergic and do not acquire effector function (24), because in the absence of irradiation damage and inflammation, costimulatory molecules are not upregulated (22). The OX40 stimulus causes alloreactive donor T cells to differentiate to IFN-γ producers. It acts directly on donor cells, as shown by lack of a response by Ox40–/– donor T cells transferred alone into in WT (H-2bm12×CD45.1)F1 recipients (24). We tested naive aly/aly or littermate control donor CD4+ T cells in this model to assess whether NIK is essential for OX40-mediated costimulation. When naive CD4+ T cells were cotransferred with control antibody and assayed 5 days later, aly/aly and control CD4+ T cells behaved identically: both proliferated more than 7 times, as assessed by complete CFSE dilution (data not shown); both expanded to similar numbers (Table 1); and neither upregulated CD25 or produced IFN-γ upon ex vivo stimulation (Figure 3). In contrast, coadministration of agonist anti-OX40 antibody had very disparate effects on control versus aly/aly donor T cells. In recipients of control CD4+ T cells, anti-OX40 increased cell accumulation 3-fold (Table 1), induced massive CD25 upregulation (Figure 3A), and induced effector differentiation such that donor cells produced copious IFN-γ upon ex vivo stimulation with IL-12 and IL-18 or with PMA and ionomycin (Figure 3, B and C). Moreover, approximately 20% of control T cells made IFN-γ even without stimulation (Figure 3, B and C). In contrast, anti-OX40 administration had almost no effect on aly/aly T cells, as assessed by cell numbers, CD25 upregulation, and IFN-γ production (Table 1 and Figure 3). We conclude that NIK is essential for OX40 to costimulate and impart a lethal phenotype to responding alloreactive CD4+ T cells.
Figure 3. NIK-deficient CD4+ T cells do not respond to OX40 signaling.
7 × 106 naive aly/aly or aly/+ CD4+ T cells were injected intravenously into unirradiated (H-2bm12×CD45.1)F1 recipients along with 50 μg agonist anti-OX40 or control antibody. Spleens were harvested 5 days later and stained immediately for CD25 (A) or stimulated for 5 hours with medium alone, IL-12 and IL-18, or PMA and ionomycin and then stained for intracellular IFN-γ (B and C). (A and B) Plots are gated on CD45.1– CD4+ (transferred) cells; numbers reflect percent CD25+ or IFN-γ+ gated cells. Data are representative of 3 mice per group in 1 representative experiment of 3. (C) Percent IFN-γ+ CD45.1– donor CD4+ T cells. Data (± SEM) are representative of 3 independent experiments.
Because NIK is required for normal thymic epithelial cell development, we more stringently tested the T cell–intrinsic role of NIK using aly/aly or control T cells obtained from BM chimeras in which the BM recipients (and thus thymic stroma) were WT. aly/aly T cells that developed in a NIK sufficient thymus also failed to respond to costimulation through OX40 by upregulating CD25 or acquiring the capacity to secrete IFN-γ (Supplemental Figure 3).
In addition to costimulating effector T cells, OX40 may also augment immune responses in some situations by inhibiting Treg differentiation (25–27). We tested whether this function of OX40 also relies on signaling through NIK by inducing Treg differentiation in vitro in the presence or absence of agonist anti-OX40 antibody. OX40 inhibited induced Treg (iTreg) differentiation by approximately 40% in NIK-sufficient CD4+ T cells, whereas it had no effect on iTreg induction in aly/aly CD4+ T cells (Supplemental Figure 4).
OX40 activates noncanonical NF-κB in a NIK-dependent manner.
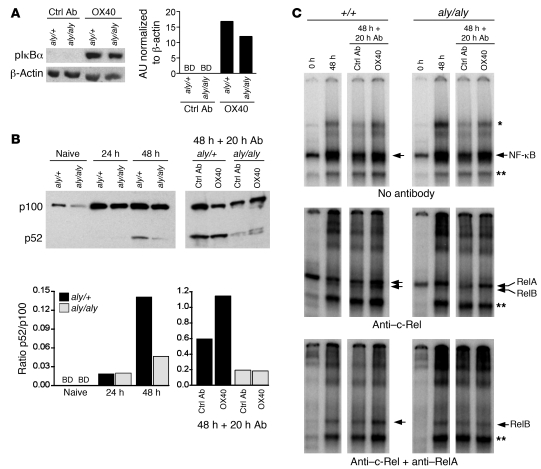
NIK is necessary to activate the noncanonical NF-κB pathway downstream of a limited number of TNFRs, including BAFFR, LTβR, and CD40. To assess whether OX40 also depends on NIK to activate the noncanonical NF-κB pathway, we examined canonical and noncanonical NF-κB signaling downstream of OX40 in aly/aly and littermate control T cells. We stimulated purified naive aly/aly or control CD4+ T cells with anti-CD3 and anti-CD28, and after 48 hours we added control antibody or agonist anti-OX40 for 5 minutes or 20 hours to assess NF-κB activation. Stimulation with anti-OX40 for 5 minutes induced equivalent IκBα phosphorylation in T cells of both genotypes (Figure 4A), which indicates that OX40 initiates robust canonical NF-κB signaling, as previously reported (28), and that this pathway is NIK independent.
Figure 4. OX40 activates canonical and noncanonical NF-κB pathways in CD4+ T cells, and the noncanonical pathway depends on NIK.
Purified naive CD4+ T cells were stimulated with anti-CD3 plus anti-CD28, and anti-OX40 or control antibody was added 48 hours later. (A and B) Whole-cell extracts were assessed for phosphorylated IκBα (pIκBα) and p100/p52 by Western blot. BD, below level of detection. In B, separated blots are from different gels run at the same time. Note the differing y axis scales in the left and right graphs of B. (C) Nuclear extracts were assessed by EMSA with the indicated supershifting antibodies. Single asterisks denote c-Rel/RelA heterodimers and RelA homodimers; double asterisks denote nonspecific bands. For each set of panels (top, middle, bottom) all 8 lanes were run on the same gel but were noncontiguous. Data are representative of 2 independent experiments.
We examined the effect of OX40 ligation on noncanonical NF-κB activation by assessing p100 processing in whole-cell extracts. Naive CD4+ T cells contained low levels of p100 (Figure 4B). As previously reported (16), naive aly/aly T cells expressed less p100 than control T cells, but by 48 hours after TCR stimulation, p100 levels were the same between genotypes (Figure 4B and Supplemental Figure 5). Although p100 expression increased upon TCR stimulation in both control and aly/aly T cells, processing to p52 was minimal at 24 and 48 hours; 20 hours later (i.e., 68 hours of TCR stimulation), the p52/p100 ratio had increased in both control and aly/aly cultures (Figure 4B), showing that after 2–3 days of in vitro stimulation, CD4+ T cells processed p100 in a partially NIK-independent manner. However, agonist anti-OX40 antibody augmented p100 processing in control T cells, but had no effect on aly/aly T cells (Figure 4B). Thus, although TCR stimulation alone induced both NIK-dependent and NIK-independent p100 processing, OX40 further increased p100 processing, and this effect was entirely NIK-dependent.
To assess downstream events in the NF-κB pathway, we performed EMSA on nuclear extracts from OX40-stimulated aly/aly and control cells. We found maximal DNA binding activity 48 hours after TCR stimulation, which then declined by 20 hours later with control antibody (Figure 4C, top). Anti-OX40 treatment maintained NF-κB binding, and this effect was similar between control and aly/aly T cells. This reflects the dominant contribution of canonical NF-κB activation downstream of the TCR and OX40. Supershift analysis using anti–c-Rel antibody or combined anti–c-Rel and anti-RelA antibodies allowed discrimination of discrete RelA and RelB bands, indicative of canonical and noncanonical NF-κB signaling, respectively. OX40 stimulation upregulated RelA DNA binding activity in both aly/aly and control T cells (Figure 4C, middle). In contrast, OX40 stimulation upregulated RelB DNA-binding activity only in control, but not in aly/aly, CD4+ T cells (Figure 4C, middle and bottom). Together, these data showed that OX40 activated both canonical and noncanonical NF-κB pathways in T cells, but only activation of the noncanonical NF-κB pathway required NIK. By extension, these data indicate that the seemingly minor contribution of RelB to total NF-κB activity may be essential to the function of OX40 in vivo.
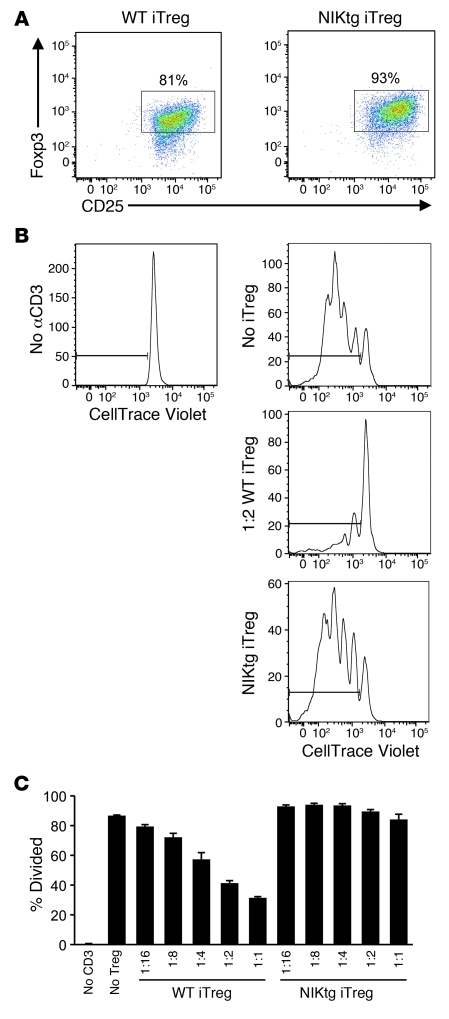
NIK overexpression in T cells causes lethal T cell–mediated inflammation and iTreg-mediated suppression.
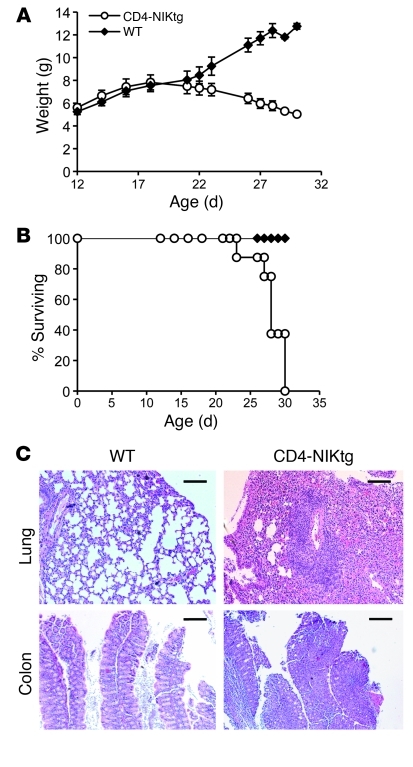
Given the essential role for NIK in our model of OX40-induced GVHD, we asked whether overexpression of NIK in the absence of OX40 or other TNFR costimulation was sufficient to recapitulate this effect. To this end, we obtained conditional NIK transgenic mice in which a single copy NIK-IRES-GFP transgene preceded by a loxP-flanked stop cassette is inserted into the ubiquitously expressed ROSA-26 locus (referred to herein as NIKtg mice; ref. 29). We crossed NIKtg mice with CD4-Cre transgenic mice — generating mice referred to herein as CD4-NIKtg — in order to turn on expression of the NIK transgene specifically in T cells, as confirmed by flow cytometry (Supplemental Figure 6). Expression of the NIK transgene in T cells caused an upregulation of NF-κB2 (p100 plus p52) and an increase in processing of p100 to p52 that was similar to the level of p100 processing seen in WT B cells (Supplemental Figure 7). Unexpectedly, CD4-NIKtg mice died before weaning. They were born at a normal Mendelian frequency of 50%, but began to lose weight rapidly around day 20 (Figure 5A), developed loose stools, and quickly became moribund, requiring euthanasia between days 23 and 30 (Figure 5B). The lungs of all moribund CD4-NIKtg mice examined had moderate to massive lymphocytic infiltration (7 of 7), as did the colons of 6 of 7 CD4-NIKtg mice (Figure 5C). Age-matched littermate control organs were all normal (4 of 4).
Figure 5. Overexpression of NIK in T cells causes lethal inflammation.
(A and B) CD4-NIKtg and age-matched littermate WT control mice were weighed and euthanized when moribund. Data in A show average weights (± SD) from 2 combined litters. (C) Sections of colon and lungs from moribund CD4-NIKtg and age-matched littermate WT control mice were assessed for leukocyte infiltrates by hematoxylin-eosin stain. Scale bars: 100 μm. Data are from 2 combined litters.
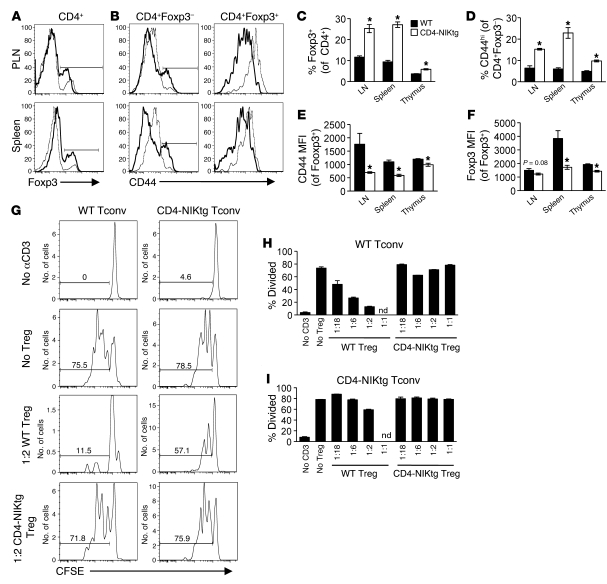
The rapid-onset mortality accompanied by lymphocytic infiltration of multiple organs that we observed in CD4-NIKtg mice was similar to the phenotype of Foxp3–/– and FoxP3scurfy mice, which harbor an inactivating mutation in Foxp3 (30). These mice die of T cell–mediated autoimmunity resulting from lack of regulation by Foxp3+ Tregs. To determine whether NIK overexpression interferes with Treg and/or effector T cell development, we assessed lymphocyte populations from CD4-NIKtg mice at day 11, before onset of outward disease symptoms. Spleen and thymus cellularity were similar between CD4-NIKtg and control littermates (Supplemental Figure 8), but peripheral and mesenteric LNs were noticeably larger (data not shown). The proportion of CD8+ T cells was slightly lower in LN and spleen of CD4-NIKtg mice, and the proportion of total CD4+ T cells was the same in spleen and LN and slightly lower in the thymus of CD4-NIKtg mice (Supplemental Figure 8). To our surprise, when we examined CD4+ T cells more closely, we found that a significantly greater percentage of CD4+ T cells was Foxp3+ in CD4-NIKtg lymphoid organs compared with lymphoid organs of control littermates (Figure 6, A and C). Despite this large increase of Foxp3+ T cells, the conventional T cell subsets (CD8+ and Foxp3–CD4+) showed an activated phenotype, as assessed by a 2- to 3-fold increase in the percentage of CD44hi cells (Figure 6, B and D, and data not shown), which suggests they are poorly regulated by Tregs. In CD4-NIKtg mice, both Foxp3+ and Foxp3– T cell populations overexpress NIK, so it was unclear whether CD4-NIKtg Tregs are poor regulators or whether CD4-NIKtg conventional T cells (Tconvs) are resistant to regulation. CD4-NIKtg Foxp3+CD4+ T cells had significantly lower CD44 and Foxp3 expression compared with control littermates (Figure 6, E and F), consistent with poorer Treg function (31). To directly address this possibility, we performed in vitro Treg suppression assays using combinations of WT and CD4-NIKtg Tregs and Tconvs. In this assay, WT Tregs inhibited the ability of WT Tconvs to proliferate in response to polyclonal stimulation with anti-CD3 and APCs. While WT Tregs efficiently suppressed WT Tconvs, showing suppression at a 1:18 Treg/Tconv ratio, CD4-NIKtg Tregs were incapable of suppressing WT Tconvs, even at a 1:1 Treg/Tconv ratio (Figure 6, G and H). In addition, CD4-NIKtg Tconvs were difficult to suppress, showing only modest regulation by WT Tregs, even at the highest 1:2 Treg/Tconv ratio (Figure 6, G and I). This suggested that overexpression of NIK both increases Tconv resistance to Treg-mediated suppression and impairs Treg function.
Figure 6. CD4-NIKtg mice have increased populations of activated T cells and nonfunctional Tregs.
(A–F) Organs were harvested from 11-day-old CD4-NIKtg (bold lines and white bars) and age-matched littermate WT control mice (narrow lines and black bars) and assessed for surface markers and intracellular Foxp3 by flow cytometry. (G–I) Naive CD4+ T cells and Tregs were sorted from 11-day-old CD4-NIKtg and littermate WT control spleens and LNs. Naive T cells were labeled with CFSE and cultured with WT APCs and soluble anti-CD3 at various ratios with Tregs. Gates in G indicate proportion of T cells that underwent at least 1 cell division. nd, not done. Data (± SD) are representative of 2 independent experiments. *P < 0.05.
Despite in vitro resistance to Treg-mediated suppression, CD4-NIKtg Tconvs were suppressible in vivo, as assessed by BM chimeras. Lethally irradiated CD45.1 recipients of a mixture of CD4-NIKtg and congenically marked WT BM remained healthy for at least 10 months and did not show signs of inflammation such as enlarged LNs. The same was true for recipients of CD4-NIKtg BM alone, due to radioresistant Tregs that reconstitute the host after irradiation and have previously been shown to prevent disease after transplantation of Foxp3scurfy BM (32). The mixed BM chimeras demonstrated that the CD4-NIKtg Tconv and Treg phenotypes are intrinsic rather than secondary to inflammation, because although the mice remained healthy, (a) the CD4-NIKtg Tconvs had an expanded population of CD44hi cells; (b) WT Tregs were expanded relative to CD4-NIKtg Tregs; and (c) NIKtg Tregs showed decreased CD44 expression, a phenotype consistent with poor regulatory capacity (Supplemental Figure 9).
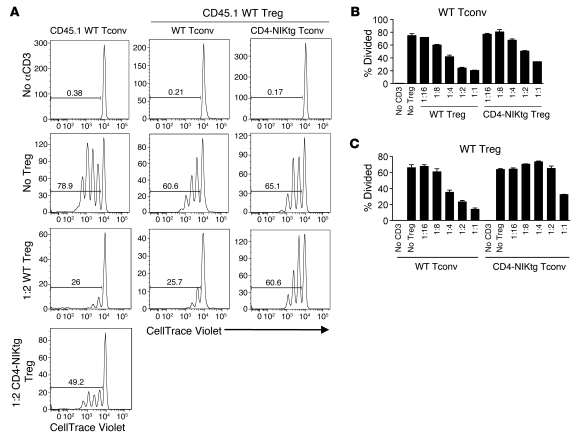
These chimeras also allowed us to obtain CD4-NIKtg Tregs from healthy mice to stringently test the Treg-intrinsic role of NIK. The decreased suppressive capacity of CD4-NIKtg Tregs from 11-day-old CD4-NIKtg mice could have been secondary to an inflammatory environment in these prediseased mice, rather than an intrinsic effect of NIK in Tregs. We sorted CD4-NIKtg and WT Tregs and Tconvs from healthy BM chimeras and performed in vitro Treg suppression assays using various combinations of Treg and Tconv cell populations. The results of this experiment were similar to those obtained using 11-day-old CD4-NIKtg mice: CD4-NIKtg Tregs from healthy BM chimeras were poorer suppressors of WT Tconvs than were WT Tregs, and CD4-NIKtg Tconvs were more resistant to suppression by WT Tregs than were WT Tconvs (Figure 7). However, CD4-NIKtg Tregs from the healthy mice were only modestly impaired in suppressive capacity, which suggests that both Treg-intrinsic and inflammatory phenomena contribute to the demise of Treg function in CD4-NIKtg mice.
Figure 7. NIK intrinsically inhibits Treg-suppressive capacity and increases Tconv resistance to suppression.
CD4-NIKtg and littermate WT control Tregs and naive T cells were sorted from spleen and LN of healthy BM chimeras and cultured with CD45.1 Tregs or naive T cells plus WT APCs and soluble anti-CD3. (A) Naive T cells were labeled with CellTrace Violet to assess division over the course of 3 days. Gates indicate proportion of T cells that underwent at least 1 cell division. (B and C) Data (± SD) are representative of 2 independent experiments.
These in vitro data suggested that overexpression of NIK in T cells causes aggressive lethal autoimmunity via intrinsic effects on both Tconvs and Tregs; combined, these effects lead to hyperactive effector T cells. Furthermore, the observation that lethally irradiated CD45.1 WT recipients of CD4-NIKtg BM (which harbor radioresistant WT host Tregs) remained healthy, but Rag1–/– recipients (which lack host Tregs) succumbed to disease (data not shown), suggested that WT Tregs can regulate CD4-NIKtg effector T cells and, by extension, that CD4-NIKtg Tregs cannot. To formally test this, we made mixed BM chimeras in which 1:1 mixtures of CD4-NIKtg plus Foxp3scurfy BM or CD4-NIKtg plus WT (FoxP3scurfy littermate) BM were used to reconstitute Rag1–/– recipients. In this experiment, the sole difference between the groups was the absence or presence of WT Foxp3+ Tregs. We found that 80% of the CD4-NIKtg plus WT BM recipients survived, but nearly all of the CD4-NIKtg plus FoxP3scurfy BM recipients succumbed to disease within 8 weeks (Supplemental Figure 10). We thus concluded that CD4-NIKtg Tregs have poor regulatory function in vivo.
In our genetic systems of NIK induction, T cells overexpressed NIK from the double-positive thymocyte stage. We wondered whether acute NIK induction in mature Tregs would have the same effect, so we developed a system to induce NIK expression in vitro using TAT-Cre fusion protein transduction, in which we attained approximately 50%–70% transduction efficiency. We treated purified NIKtg or control CD4+ T cells with TAT-Cre, cultured under Treg-inducing conditions, and then sorted iTregs from control cultures and GFP+ iTregs from NIKtg cultures. NIK overexpression did not interfere with iTreg differentiation in these conditions, as assessed by Foxp3 and CD25 expression (Figure 8A and data not shown). However, when we tested these sorted iTregs for suppressive function against WT Tconvs, we found that iTregs in which NIK was acutely expressed were much poorer suppressors than TAT-Cre–treated control iTregs (Figure 8, B and C). This showed that NIK overexpression affected Treg function independently of developmental effects that could occur during selection in the thymus.
Figure 8. Acute overexpression of NIK in mature T cells inhibits iTreg suppressive capacity.
CD4+ T cells were magnetically purified from NIKtg and littermate WT control spleen and LN, treated with TAT-Cre, and cultured under iTreg-inducing conditions for 3 days. Tregs were then sorted on the basis of CD4, CD25, and GFP, and cultured with CD45.1 naive T cells plus WT APCs and soluble anti-CD3 for an additional 3 days. (A) After iTreg induction and sorting, WT and NIKtg iTregs expressed equivalent Foxp3 and CD25. Plots are gated on live T cells. Numbers reflect percent Foxp3+ T cells. (B) Naive CD45.1 CD4+ T cells were labeled with CellTrace Violet to assess division over the course of 3 days. (C) Data (± SD) are representative of 2 independent experiments.
Discussion
NIK has been studied primarily in terms of its role in immune system organogenesis, lymphoid architecture, and naive B cell survival. Here, we identify a role for NIK as a critical mediator of T cell responses following antigen exposure by signaling downstream of OX40 and probably other costimulatory TNFRs. We found that NIK was absolutely required for lethal CD4–mediated GVHD, but not for initial naive T cell responses through the antigen receptor in vitro. Likewise, in unirradiated recipients without exogenous costimulation, NIK-deficient T cells expanded normally.
Recently, Hofmann et al. showed that NIK is important for DCs to prime effective T cell responses (18). They found that whereas single Nik–/– BM chimeras are resistant to EAE, single Nik+/– BM chimeras and mixed Nik–/–Rag–/– BM chimeras (which harbor WT DCs) are susceptible to EAE. However, it is unclear in this experiment whether there is also a role for NIK in the T cells, since the authors compared the mixed chimeras with single Nik+/– BM chimeras whose DCs are not WT, but heterozygous for NIK. We and others have shown that NIK heterozygosity confers a significant in vivo effect in various cell types, and it is likely that Nik+/– DCs are also at least partially impaired. Indeed, similar to Jin et al. (19), Hofmann et al. also showed that purified NIK KO T cells transferred into WT hosts (with WT DCs) could not mediate EAE (18). Although NIK is clearly important in DCs and other APCs to elicit optimal T cell responses, in our experiments, we carefully purified T cells to be able to identify T cell–intrinsic effects of NIK in vivo and in vitro. Furthermore, we identified OX40 as a specific receptor expressed by T cells that relies absolutely on NIK to mediate its T cell costimulatory effects.
Several lines of evidence suggested to us that NIK might act downstream of costimulatory TNF receptors on T cells. First, known receptors that rely on NIK to activate the noncanonical NF-κB pathway are TNFRs. Second, several of the TNF receptors expressed on T cells have previously been shown to induce constitutive p100 processing when overexpressed in cell lines (33), and OX40-induced NF-κB activation in HEK293 cells was inhibited by transduction with dominant-negative NIK (34). TNFRII on human primary T cells was recently shown to induce p100 processing (35). Finally, the T cell phenotypes of NIK-deficient mice are surprisingly similar to those of Ox40–/– mice. T cell development and peripheral populations are near normal in Ox40–/– mice, as are most in vitro responses and initial clonal expansion upon antigen recognition in vivo. However, maximum T cell expansion and differentiation to effector function depend on OX40/OX40L interactions in vivo (3). Particularly relevant to our studies, Ox40–/– and Ox40l–/– mice suffer much milder disease in models of autoimmunity and GVHD (3). When we tested the role of NIK in OX40-mediated GVHD, we found that the costimulatory effects of OX40 activation were almost completely abrogated in NIK-deficient T cells, demonstrating a direct requirement for NIK downstream of OX40. Likewise, the ability of OX40 to inhibit iTreg induction was abolished in NIK-deficient T cells. Although we cannot rule out other possible roles for NIK in the CD4+ T cell response to OX40 signaling, we believe sustained activation of NF-κB through the noncanonical pathway may be necessary. In support of this concept, we showed that OX40 activated the noncanonical NF-κB pathway in primary CD4+ T cells, and that this was NIK dependent.
It is likely that OX40 is not unique among T cell costimulatory TNF receptors in using NIK to activate the noncanonical NF-κB pathway. Jin et al. showed that costimulatory effects of LIGHT in vitro depend in part on NIK (19), and, as mentioned above, activation of TNFRII can induce p100 processing in T cells (35). Other likely candidates include CD30 and 4-1BB, both of which contribute to GVHD (22, 23), and both of which have been shown to induce p100 processing when overexpressed in cell lines (33).
It is somewhat surprising that NIK deficiency had such a profound effect on T cell responses to OX40, given that canonical NF-κB activation was preserved and that the noncanonical pathway seemed to make a minor contribution to overall NF-κB activity (Figure 4). However, it should be noted that in other cell types, small differences in noncanonical NF-κB activation have profound biological consequences. In conditional NIK transgenic B cells, for example, processing of p100 to p52 is increased only 30% above WT B cell levels, yet peripheral B cell numbers are increased 3-fold (29). It may be that specific OX40 target genes depend on p52:RelB dimers to induce their transcription, as has been shown for LTβR target genes (36). Another possibility, not mutually exclusive from the former, is that NIK-driven activation of the noncanonical NF-κB pathway may prolong NF-κB signaling via degradation of p100, which is induced by NF-κB activation and acts like an IκB to inhibit both canonical and noncanonical NF-κB activation (37, 38). This might explain how small differences in the level of NIK (i.e., a 2-fold decrease in aly/+ heterozygous mice) could mediate large physiologic effects: NIK-induced degradation of p100 could simultaneously activate the noncanonical NF-κB pathway and relieve a brake on both NF-κB pathways.
Likewise, we found that a modest increase in NIK expression in T cells exerted profound physiological effects. The conditional NIK transgene induced p100 processing in T cells similar to that in WT resting B cells, yet T cells became highly activated, and mice succumbed to rapid fatal autoimmunity. Surprisingly, this occurred despite increased numbers of Foxp3+ Tregs. NIK overexpression affected both Tconvs and Tregs, with the combined result being overactivated effector T cells that were not controlled by Tregs. WT Tregs could control the disease mediated by CD4-NIKtg T cells in vivo, whereas NIKtg Tregs could not. This suggests that NIK overexpression in Tregs is critical for disease induction, but does not rule out a role for NIK in Tconvs. In particular, even in healthy mixed BM chimeras, NIKtg Tconvs retained an activated phenotype and remained difficult to suppress in vitro. Thus, we believe that NIK overexpression in both Tconvs and Tregs contributes to the rapid-onset autoimmunity observed in CD4-NIKtg mice.
Constitutive activation of the noncanonical NF-κB pathway via a ubiquitously expressed p52 transgene also predisposes mice to multiorgan autoimmunity, and the p52 transgenic T cells are more activated and more resistant to apoptosis (39). Moreover, although p52 transgenic mice do not suffer early postnatal mortality, normal or transgenic expression of p52 in the absence of the inhibitory p100 subunit leads to a lethal inflammatory syndrome, although the role of T cells in mediating autoimmunity was not tested (40, 41). The exacerbated disease caused by the absence of p100 indicates that NIK overexpression may have provided a powerful T cell stimulus in our experiments by relieving p100-mediated NF-κB inhibition as well as by increasing p52-mediated gene transcription.
In many ways, NIK overexpression in T cells mimicked constitutive OX40 activation, which induces an activated phenotype, enhances cell survival, and, importantly, confers resistance to Treg-mediated suppression in Tconvs (3). OX40 ligation not only enhances T cell responses to foreign antigens, tumor antigens, and alloantigens, but also can exacerbate autoimmune diseases when used as an adjuvant along with self-antigen. Interestingly, OX40L transgenic mice develop a T cell–mediated autoimmune syndrome characterized by a large population of CD44hi memory CD4+ T cells and colon and lung leukocyte infiltration reminiscent of our CD4-NIKtg mice, but with delayed kinetics (42). The phenotype of CD4-NIKtg Tregs also paralleled observed effects of OX40 on this cell type. Numerous studies have shown that activation of OX40 inhibits the suppressive function of Tregs (25–27). Although some studies have also shown that OX40 signaling increases Treg-mediated suppression, this appears to result from positive effects of OX40 on Treg homeostasis and expansion, such that lack of OX40 in vivo reduces Treg numbers, rather than affecting Treg function on a per-cell basis (43, 44). Additionally, 2 other TNFR ligands that inhibit Treg function may rely, at least in part, on NIK for signaling. Glucocorticoid-induced TNF receptor family related protein ligand (GITRL) and TNF-α both have been shown to activate NF-κB in Tregs and to inhibit Treg function (45, 46), and as mentioned above, activation of TNFRII induces modest p100 processing in human Tconvs (35). Curiously, NIK KO Tregs are hyperproliferative upon GITR ligation, which may be caused by a disproportionate increase of cells in the Treg subset that possess an activated/memory phenotype (47). This is suggestive of complex effects of NIK in Tregs that may depend on activation of particular receptors and/or integration with other signals.
How does upregulation of NIK interfere with the Treg program? Comparing the essentially nonfunctional CD4-NIKtg Tregs from prediseased mice (Figure 6) with the moderately impaired CD4-NIKtg Tregs from healthy chimeras (Figure 7) suggests that NIK overexpression impairs Treg function sufficiently to allow Tconvs to escape suppression, and the ensuing inflammatory environment further degrades Treg function in a positive feedback loop. A similar phenomenon occurs when Dicer is conditionally deleted in Foxp3+ Tregs to block microRNA production. Those mice develop a severe fatal autoimmune syndrome similar to that observed in our CD4-NIKtg mice (48). Foxp3+ Tregs are expanded, but nonfunctional. Like CD4-NIKtg Tregs, the Dicer–/– Tregs are functionless in the inflammatory environment of the sick males, but retain some function in healthy heterozygous females. Together, these data show that diverse mechanisms are required to maintain optimal Treg function, and modest Treg destabilization can easily tip the balance to frank autoimmunity.
Our data suggest that manipulating levels of NIK in T cells may have therapeutic value. While a large number of NF-κB blocking compounds are in clinical development and trials, we are aware of none shown to be specific for NIK or the noncanonical NF-κB pathway. Decreasing NIK activity in T cells might significantly ameliorate autoimmune and alloresponses, like GVHD and transplant rejection, without crippling the immune system as severely as do inhibitors of canonical NF-κB activation. The fact that even heterozygous aly/+ mice were partially protected from lethal GVHD is promising, as it suggests complete ablation of NIK is not necessary for drug efficacy. Moreover, GVHD is ameliorated when the noncanonical NF-κB subunit, RelB, is eliminated in APCs (49). Therefore, combined inhibition of the noncanonical NF-κB pathway in T cells and APCs might be a particularly effective therapy. Conversely, upregulating NIK in DCs has been suggested as a potential therapeutic to increase vaccine efficacy (50). We showed here that upregulation of NIK provided a strong activation stimulus in T cells as well. As above, this suggests that combined modulation of NIK in T cells and DCs could have additive or synergistic effects, particularly in the setting of cancer immunotherapy, in which a major obstacle is overcoming Treg-mediated suppression of immune responses. However, caution clearly needs to be employed in developing therapies aimed at increasing NIK, since the potential for devastating autoimmunity and lymphomagenesis is present when the noncanonical NF-κB pathway is not tightly regulated (29, 39, 51, 52).
Methods
Mice.
Mice were housed under specific pathogen–free conditions at the Oregon Health and Science University animal facility. B6.Thy1.1, B6.CD45.1, FoxP3scurfy, and Rag1–/– mice were from The Jackson Laboratory. (H-2bm12×CD45.1)F1 mice were made by crossing B6.C-H2bm12/KhEg mice (The Jackson Laboratory) to B6.CD45.1 mice. Aly/NscJcl mice (CLEA Japan) were maintained by breeding female aly/+ to male aly/aly mice. Offspring were genotyped by assessing serum IgA levels as described previously (6). The +/+ mice, with 2 normal copies of NIK on the aly background, were made by aly/+ to aly/+ crosses and were genotyped by PCR. ROSA26StopflNik transgenic mice were provided by K. Rajewsky (Harvard Medical School, Boston, Massachusetts, USA) and M. Schmidt-Supprian (Max Plank Institute of Biochemistry, Munich, Germany), and mice heterozygous for the NIK transgene were bred to Cd4-Cre homozygous transgenic mice (53) (Taconic). Female heterozygous FoxP3scurfy mice were bred to male C57BL/6 mice. Male FoxP3scurfy offspring were identified phenotypically and by FACS analysis of T cells. Primers used for genotyping aly/aly mice were 5′-GACATCCCGAGCTACTTCAACA-3′ and 5′-CGTGTTCCTATTTCCTCATCATCACCA-3′. Primers used for genotyping CD4-NIKtg mice (EGFP amplification) were 5′-ATGAAGCAGCACGACTTCTTCAAGTCCGCC-3′ and 5′-TGGCGGATCTTGAAGTTCACCTTGATGCCG-3′
Antibodies.
Rat anti-OX40 (clone OX86), anti–IL-4, and anti–IFN-γ blocking antibodies were from BioXCell. Control rat IgG was from Capell, ICN Pharmaceuticals. Anti-CD3 was from eBiosciences, and anti-CD28 was from Biolegend. Rabbit anti–phospho-IκBα was from Cell Signaling Technology, rabbit anti-actin and rabbit anti-Erk2 were from Santa Cruz Biotechnology, rabbit anti–mouse-p100/p52 was a gift from S. Ley (National Institute for Medical Research, London, United Kingdom), and HRP-conjugated goat anti-rabbit was from BD Biosciences. Fluorescently conjugated antibodies used for FACS were anti-CD44–FITC, anti-CD4–PerCP-Cy5.5 or –PE-Cy7, anti-CD8–PE-Cy7, anti-CD45.1–PE or –PE-Cy7, anti-CD25–PE or –biotin, anti–IFN-γ–allophycocyanin, anti-CD69–FITC, anti-Foxp3–Alexa Fluor 647, anti-CD3–biotin, polyclonal chicken anti-OX40–biotin, and streptavidin-allophycocyanin. All staining antibodies were from eBiosciences except anti-CD25–biotin (BD Biosciences) and chicken anti-OX40 (gift from A. Weinberg, Earle A. Chiles Research Institute, Portland, Oregon, USA).
Flow cytometry.
Spleen cell suspensions were stained directly ex vivo or stimulated for 5 hours and then stained for surface markers and intracellular cytokines as previously described (54). Foxp3 staining was performed per the manufacturer’s instructions (Biolegend Foxp3 Fix/Perm Buffer kit). Cells were analyzed on a FACSCalibur or LSR II flow cytometer (BD Biosciences) and analyzed using FlowJo (Tree Star).
Adoptive transfers.
Donor lymphocyte single-cell suspensions were prepared from spleen, and total CD4+ T cells were purified by magnetic negative selection (Easy Sep; Stem Cell Technologies). Naive CD4+ T cells (CD4+CD25–CD44int/lo) were then sorted on a FACSVantage (BD Biosciences) to greater than 98% purity. In some experiments, cells were CFSE labeled prior to transfer. 2–7 × 106 cells were injected intravenously with 50 μg anti-OX40 or control rat IgG into unirradiated (H-2bm12×B6.CD45.1)F1 recipients. 1 × 106 cells were injected intravenously without antibody into recipients that had received 6 Gy γ irradiation that day. For lethal GVHD studies, mice were monitored daily and euthanized when moribund.
In vitro T cell stimulation.
Total or naive CD4+ T cells were purified as described in Adoptive transfers and stimulated for 48–96 hours with immobilized anti-CD3 (2–10 μg/ml) and anti-CD28 (2–5 μg/ml). Culture supernatants were collected for cytokine analysis by ELISA (BioLegend ELISA MAX IL-2 and IFN-γ Set standards). To assess proliferation, 1 μCi/well thymidine, [methyl-3H] (Perkin Elmer), was added 24 hours before cell harvest. Separate cultures were stained for expression of surface activation markers. For assessment of NF-κB signaling, cultures were treated at 48 hours with soluble anti-OX40 or control rat IgG (10 μg/ml) for varying times.
Western blot and EMSA analysis.
Whole-cell extracts for Western blot and nuclear extracts for EMSA were prepared as described previously (37). For Western blot, whole-cell extract was electrophoresed through a 10% polyacrylamide gel and transferred onto PVDF membranes. Membranes were blocked overnight at 4°C, probed with primary rabbit antibody at 1:1,000 (β-actin), 1:2,000 (p100, phospho-IκBα), or 1:3,000 (ERK2), probed with secondary HRP-conjugated goat anti-rabbit at 1:5,000, and developed with SuperSignal West Pico developing reagent (Thermo Fisher Scientific). EMSA to assess NF-κB binding activity was performed as described previously (37).
In vitro natural Treg functional assay.
Lymphocyte single-cell suspensions were prepared from spleen plus LN of CD4-NIKtg, littermate control, B6.CD45.1, or chimeric mice. Magnetically enriched CD4+ T cells were sorted for naive CD4+ T cells (CD4+CD25–CD44int/lo) and Tregs (CD4+CD25+) as well as relevant congenic markers on a FACSVantage to greater than 98% purity. CD4-NIKtg naive T cells and Tregs were also sorted for GFP expression. APCs were prepared by red blood cell lysis and 10 Gy γ irradiation of single-cell spleen suspensions. Naive T cells were labeled with CFSE or Cell Trace Violet (Invitrogen), and 5 × 104 naive T cells were cultured with 1 × 105 APCs, varying numbers of Tregs, and 0.5 μg/ml soluble anti-CD3 for 3–4 days.
iTreg differentiation.
Magnetically purified CD4+ T cells were cultured on anti-CD3– and anti-CD28–coated plates (5 μg/ml each) with 10 U/ml IL-2 (55), 2–8 ng/ml TGF-β (PeproTech), 10 mM all-trans retinoic acid (Sigma-Aldrich), 2 μg/ml anti–IFN-γ (MG1.2), and 1.4 μg/ml anti–IL-4 (11B11) for 3 days. In aly/aly experiments, control IgG or agonist anti-OX40 (10 μg/ml) was added at the beginning of the cultures. iTreg purity after culture was assessed by CD4 and Foxp3 stain.
TAT-Cre transduction and iTreg functional assay.
His-tagged TAT-Cre fusion protein was grown and purified as described previously (56) from plasmid 13763: pTriEx-HTNC (contributed to Addgene by K. Rajewsky, Harvard Medical School, Boston, Massachusetts, USA, and F. Edenhofer, University of Bonn, Bonn, Germany). CD4+ T cells from NIKtg and littermate control mice were incubated in serum-free media with 100 μg/ml TAT-Cre for 45 minutes, washed in serum-containing media, and cultured as described in iTreg differentiation. After 3 days, iTregs were sorted as CD4+CD25+ and, for NIKtg only, GFP+. Sorted cells of both genotypes were approximately 90% pure when assessed for Foxp3 expression. Sorted iTregs were then cultured with congenically marked Cell Trace Violet–labeled WT naive CD4+ T cells, APCs, and anti-CD3 as described in In vitro natural Treg functional assay.
BM chimeras.
BM was harvested from femurs and tibias of 11- to 18-day-old CD4-NIKtg mice, littermate CD4-Cre control mice, FoxP3scurfy mice, or WT control littermates of FoxP3scurfy mice or from femurs and tibias of adult aly/aly mice or +/+ mice. Single-cell suspensions of BM were depleted of mature T cells via magnetic separation using anti-CD3–biotin. 0.25–1.0 × 106 BM cells were injected intravenously into lethally irradiated (12 Gy, split dose) CD45.1 recipients or sublethally irradiated (6 Gy, single dose) Rag1–/– recipients. For CD4-NIKtg plus FoxP3scurfy and CD4-NIKtg plus WT BM chimeras, CD4-NIKtg BM was parked in Rag1–/– mice for 3 weeks prior to making the mixed BM chimeras. This was due to difficulty in precisely timing B6×FoxP3scurfy and CD4-Cre×NIKtg pregnancies.
Histology.
Mouse organs were fixed with 10% (v/v) buffered formalin and embedded in paraffin. Sections were stained with hematoxylin and eosin.
Statistics.
The significance of differences between groups was calculated using 2-tailed Student’s t test. Log-rank test was used to assess differences in survival between aly genotypes. Differences with a P value less than 0.05 were considered statistically significant.
Study approval.
All protocols in the present studies were reviewed and approved by the Institutional Animal Care and Use Committee of Oregon Health and Science University.
Supplementary Material
Acknowledgments
We thank A. Weinberg and S. Ley for anti-OX40 and anti-p100 antibodies, respectively; K. Rajewsky and M. Schmidt-Supprian for NIKtg mice; M. Boyd for cell sorting; P. Stork and M. Takaguchi for histology analysis; K. Rajewsky and F. Edenhofer for providing the TAT-Cre plasmid to Addgene (plasmid 13763); and T. Thauland for critical manuscript review. This work was supported by NIH grants AI077032 and AI092080 (to D.C. Parker), HL007781 (to S.E. Murray), HL007781 (to A.M. Rowe), and GM071573 (to A. Hoffman). S. Basak thanks Wellcome Trust DBT India Alliance for fellowship.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2011;121(12):4775–4786. doi:10.1172/JCI44943.
Alexander M. Rowe’s present address is: Department of Ophthalmology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA.
Soumen Basak’s present address is: National Institute of Immunology, New Delhi, India.
References
- 1.Kearney ER, Pape KA, Loh DY, Jenkins MK. Visualization of peptide-specific T-cell immunity and peripheral tolerance in vivo. Immunity. 1994;1(4):327–339. doi: 10.1016/1074-7613(94)90084-1. [DOI] [PubMed] [Google Scholar]
- 2.Watts T. TNF/TNFR family members in costimulation of T cell responses. Annu Rev Immunol. 2005;23:23–68. doi: 10.1146/annurev.immunol.23.021704.115839. [DOI] [PubMed] [Google Scholar]
- 3.Croft M. Control of immunity by the TNFR-related molecule OX40 (CD134). Annu Rev Immunol. 2010;28:57–78. doi: 10.1146/annurev-immunol-030409-101243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beinke S, Ley SC. Functions of NF-kappaB1 and NF-kappaB2 in immune cell biology. Biochem J. 2004;382(pt 2):393–409. doi: 10.1042/BJ20040544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shinkura R, et al. Alymphoplasia is caused by a point mutation in the mouse gene encoding Nf-kappa b-inducing kinase. Nat Genet. 1999;22(1):74–77. doi: 10.1038/8780. [DOI] [PubMed] [Google Scholar]
- 6.Miyawaki S, et al. A new mutation, aly, that induces a generalized lack of lymph nodes accompanied by immunodeficiency in mice. Eur J Immunol. 1994;24(2):429–434. doi: 10.1002/eji.1830240224. [DOI] [PubMed] [Google Scholar]
- 7.Akiyama T, et al. The tumor necrosis factor family receptors RANK and CD40 cooperatively establish the thymic medullary microenvironment and self-tolerance. Immunity. 2008;29(3):423–437. doi: 10.1016/j.immuni.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 8.Claudio E, Brown K, Park S, Wang H, Siebenlist U. BAFF-induced NEMO-independent processing of NF-kappa B2 in maturing B cells. Nat Immunol. 2002;3(10):958–965. doi: 10.1038/ni842. [DOI] [PubMed] [Google Scholar]
- 9.Yin L, et al. Defective lymphotoxin-beta receptor-induced NF-kappaB transcriptional activity in NIK-deficient mice. Science. 2001;291(5511):2162–2165. doi: 10.1126/science.1058453. [DOI] [PubMed] [Google Scholar]
- 10.Lind EF, et al. Dendritic cells require the NF-kappaB2 pathway for cross-presentation of soluble antigens. J Immunol. 2008;181(1):354–363. doi: 10.4049/jimmunol.181.1.354. [DOI] [PubMed] [Google Scholar]
- 11.Coope HJ, et al. CD40 regulates the processing of NF-kappaB2 p100 to p52. Embo J. 2002;21(20):5375–5385. doi: 10.1093/emboj/cdf542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsubata R, et al. Autoimmune disease of exocrine organs in immunodeficient alymphoplasia mice: a spontaneous model for Sjogren’s syndrome. Eur J Immunol. 1996;26(11):2742–2748. doi: 10.1002/eji.1830261129. [DOI] [PubMed] [Google Scholar]
- 13.Kajiura F, et al. NF-kappa B-inducing kinase establishes self-tolerance in a thymic stroma-dependent manner. J Immunol. 2004;172(4):2067–2075. doi: 10.4049/jimmunol.172.4.2067. [DOI] [PubMed] [Google Scholar]
- 14.Lakkis FG, Arakelov A, Konieczny BT, Inoue Y. Immunologic ‘ignorance’ of vascularized organ transplants in the absence of secondary lymphoid tissue. Nat Med. 2000;6(6):686–688. doi: 10.1038/76267. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto M, et al. Essential role of NF-kappa B-inducing kinase in T cell activation through the TCR/CD3 pathway. J Immunol. 2002;169(3):1151–1158. doi: 10.4049/jimmunol.169.3.1151. [DOI] [PubMed] [Google Scholar]
- 16.Ishimaru N, Kishimoto H, Hayashi Y, Sprent J. Regulation of naive T cell function by the NF-kappaB2 pathway. Nat Immunol. 2006;7(7):763–772. doi: 10.1038/ni1351. [DOI] [PubMed] [Google Scholar]
- 17.Aya K, Alhawagri M, Hagen-Stapleton A, Kitaura H, Kanagawa O, Novack DV. NF-(kappa)B-inducing kinase controls lymphocyte and osteoclast activities in inflammatory arthritis. J Clin Invest. 2005;115(7):1848–1854. doi: 10.1172/JCI23763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hofmann J, Mair F, Greter M, Schmidt-Supprian M, Becher B. NIK signaling in dendritic cells but not in T cells is required for the development of effector T cells and cell-mediated immune responses. J Exp Med. 2011;208(9):1917–1929. doi: 10.1084/jem.20110128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jin W, Zhou XF, Yu J, Cheng X, Sun SC. Regulation of Th17 cell differentiation and EAE induction by MAP3K NIK. Blood. 2009;113(26):6603–6610. doi: 10.1182/blood-2008-12-192914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zarnegar BJ, et al. Noncanonical NF-kappaB activation requires coordinated assembly of a regulatory complex of the adaptors cIAP1, cIAP2, TRAF2 and TRAF3 and the kinase NIK. Nat Immunol. 2008;9(12):1371–1378. doi: 10.1038/ni.1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vallabhapurapu S, et al. Nonredundant and complementary functions of TRAF2 and TRAF3 in a ubiquitination cascade that activates NIK-dependent alternative NF-kappaB signaling. Nat Immunol. 2008;9(12):1364–1370. doi: 10.1038/ni.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Socie G, Blazar BR. Acute graft-versus-host disease: from the bench to the bedside. Blood. 2009;114(20):4327–4336. doi: 10.1182/blood-2009-06-204669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blazar BR, et al. Ligation of OX40 (CD134) regulates graft-versus-host disease (GVHD) and graft rejection in allogenic bone marrow transplant (BMT) recipients. Blood. 2003;101(9):3741–3748. doi: 10.1182/blood-2002-10-3048. [DOI] [PubMed] [Google Scholar]
- 24.Huddleston CA, Weinberg AD, Parker DC. OX40 (CD134) engagement drives differentiation of CD4+ T cells to effector cells. Eur J Immunol. 2006;36(5):1093–1103. doi: 10.1002/eji.200535637. [DOI] [PubMed] [Google Scholar]
- 25.Piconese S, Valzasina B, Colombo MP. OX40 triggering blocks suppression by regulatory T cells and facilitates tumor rejection. J Exp Med. 2008;205(4):825–839. doi: 10.1084/jem.20071341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Valzasina B, Guiducci C, Dislich H, Killeen N, Weinberg AD, Colombo MP. Triggering of OX40 (CD134) on CD4(+)CD25+ T cells blocks their inhibitory activity: a novel regulatory role for OX40 and its comparison with GITR. Blood. 2005;105(7):2845–2851. doi: 10.1182/blood-2004-07-2959. [DOI] [PubMed] [Google Scholar]
- 27.Vu MD, et al. OX40 costimulation turns off Foxp3+ Tregs. Blood. 2007;110(7):2501–2510. doi: 10.1182/blood-2007-01-070748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Song J, So T, Croft M. Activation of NF-kappaB1 by OX40 contributes to antigen-driven T cell expansion and survival. J Immunol. 2008;180(11):7240–7248. doi: 10.4049/jimmunol.180.11.7240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sasaki Y, et al. NIK overexpression amplifies, whereas ablation of its TRAF3-binding domain replaces BAFF:BAFF-R-mediated survival signals in B cells. Proc Natl Acad Sci U S A. 2008;105(31):10883–10888. doi: 10.1073/pnas.0805186105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4(+)CD25(+) regulatory T cells. Nat Immunol. 2003;4(4):330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 31.Liu T, Soong L, Liu G, Konig R, Chopra AK. CD44 expression positively correlates with Foxp3 expression and suppressive function of CD4+ Treg cells. Biol Direct. 2009;4:40. doi: 10.1186/1745-6150-4-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Komatsu N, Hori S. Full restoration of peripheral Foxp3+ regulatory T cell pool by radioresistant host cells in scurfy bone marrow chimeras. Proc Natl Acad Sci U S A. 2007;104(21):8959–8964. doi: 10.1073/pnas.0702004104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hauer J, et al. TNF receptor (TNFR)-associated factor (TRAF) 3 serves as an inhibitor of TRAF2/5-mediated activation of the noncanonical NF-kappaB pathway by TRAF-binding TNFRs. Proc Natl Acad Sci U S A. 2005;102(8):2874–2879. doi: 10.1073/pnas.0500187102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takaori-Kondo A, Hori T, Fukunaga K, Morita R, Kawamata S, Uchiyama T. Both amino- and carboxyl-terminal domains of TRAF3 negatively regulate NF-kappaB activation induced by OX40 signaling. Biochem Biophys Res Commun. 2000;272(3):856–863. doi: 10.1006/bbrc.2000.2860. [DOI] [PubMed] [Google Scholar]
- 35.Rauert H, et al. Membrane tumor necrosis factor (TNF) induces p100 processing via TNF receptor-2 (TNFR2). J Biol Chem. 2010;285(10):7394–7404. doi: 10.1074/jbc.M109.037341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dejardin E, et al. The lymphotoxin-beta receptor induces different patterns of gene expression via two NF-kappaB pathways. Immunity. 2002;17(4):525. doi: 10.1016/S1074-7613(02)00423-5. [DOI] [PubMed] [Google Scholar]
- 37.Basak S, et al. A fourth IkappaB protein within the NF-kappaB signaling module. Cell. 2007;128(2):369–381. doi: 10.1016/j.cell.2006.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Legarda-Addison D, Ting AT. Negative regulation of TCR signaling by NF-kappaB2/p100. J Immunol. 2007;178(12):7767–7778. doi: 10.4049/jimmunol.178.12.7767. [DOI] [PubMed] [Google Scholar]
- 39.Wang Z, Zhang B, Yang L, Ding J, Ding HF. Constitutive production of NF-kappaB2 p52 is not tumorigenic but predisposes mice to inflammatory autoimmune disease by repressing Bim expression. J Biol Chem. 2008;283(16):10698–10706. doi: 10.1074/jbc.M800806200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ishikawa H, Carrasco D, Claudio E, Ryseck RP, Bravo R. Gastric hyperplasia and increased proliferative responses of lymphocytes in mice lacking the COOH-terminal ankyrin domain of NF-kappaB2. . J Exp Med. 1997;186(7):999–1014. doi: 10.1084/jem.186.7.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang L, et al. Loss of negative feedback control of nuclear factor-kappaB2 activity in lymphocytes leads to fatal lung inflammation. Am J Pathol. 2010;176(6):2646–2657. doi: 10.2353/ajpath.2010.090751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murata K, Nose M, Ndhlovu LC, Sato T, Sugamura K, Ishii N. Constitutive OX40/OX40 ligand interaction induces autoimmune-like diseases. J Immunol. 2002;169(8):4628–4636. doi: 10.4049/jimmunol.169.8.4628. [DOI] [PubMed] [Google Scholar]
- 43.Griseri T, Asquith M, Thompson C, Powrie F. OX40 is required for regulatory T cell-mediated control of colitis. J Exp Med. 2010;207(4):699–709. doi: 10.1084/jem.20091618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ruby CE, et al. Cutting Edge: OX40 agonists can drive regulatory T cell expansion if the cytokine milieu is right. J Immunol. 2009;183(8):4853–4857. doi: 10.4049/jimmunol.0901112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ji HB, et al. Cutting edge: the natural ligand for glucocorticoid-induced TNF receptor-related protein abrogates regulatory T cell suppression. J Immunol. 2004;172(10):5823–5827. doi: 10.4049/jimmunol.172.10.5823. [DOI] [PubMed] [Google Scholar]
- 46.Nagar M, et al. TNF activates a NF-kappaB-regulated cellular program in human CD45RA- regulatory T cells that modulates their suppressive function. . J Immunol. 2010;184(7):3570–3581. doi: 10.4049/jimmunol.0902070. [DOI] [PubMed] [Google Scholar]
- 47.Lu LF, Gondek DC, Scott ZA, Noelle RJ. NF kappa B-inducing kinase deficiency results in the development of a subset of regulatory T cells, which shows a hyperproliferative activity upon glucocorticoid-induced TNF receptor family-related gene stimulation. J Immunol. 2005;175(3):1651–1657. doi: 10.4049/jimmunol.175.3.1651. [DOI] [PubMed] [Google Scholar]
- 48.Liston A, Lu LF, O’Carroll D, Tarakhovsky A, Rudensky AY. Dicer-dependent microRNA pathway safeguards regulatory T cell function. J Exp Med. 2008;205(9):1993–2004. doi: 10.1084/jem.20081062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MacDonald KP, et al. Effector and regulatory T-cell function is differentially regulated by RelB within antigen-presenting cells during GVHD. Blood. 2007;109(11):5049–5057. doi: 10.1182/blood-2007-01-067249. [DOI] [PubMed] [Google Scholar]
- 50.Andreakos E, Williams RO, Wales J, Foxwell BM, Feldmann M. Activation of NF-kappaB by the intracellular expression of NF-kappaB-inducing kinase acts as a powerful vaccine adjuvant. Proc Natl Acad Sci U S A. 2006;103(39):14459–14464. doi: 10.1073/pnas.0603493103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gardam S, Beyaert R. The kinase NIK as a therapeutic target in multiple myeloma. Expert Opin Ther Targets. 2011;15(2):207–218. doi: 10.1517/14728222.2011.548861. [DOI] [PubMed] [Google Scholar]
- 52.Sun SC. Non-canonical NF-kappaB signaling pathway. Cell Res. 2011;21(1):71–85. doi: 10.1038/cr.2010.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee PP, et al. A critical role for dnmt1 and DNA methylation in T cell development, function, and survival. Immunity. 2001;15(5):763–774. doi: 10.1016/S1074-7613(01)00227-8. [DOI] [PubMed] [Google Scholar]
- 54.Lathrop SK, Huddleston CA, Dullforce PA, Montfort MJ, Weinberg AD, Parker DC. A signal through OX40 (CD134) allows anergic, autoreactive T cells to acquire effector cell functions. J Immunol. 2004;172(11):6735–6743. doi: 10.4049/jimmunol.172.11.6735. [DOI] [PubMed] [Google Scholar]
- 55.Karasuyama H, Melchers F. Establishment of mouse cell lines which constitutively secrete large quantities of interleukin 2, 3, 4 or 5, using modified cDNA expression vectors. Eur J Immunol. 1988;18(1):97–104. doi: 10.1002/eji.1830180115. [DOI] [PubMed] [Google Scholar]
- 56.Peitz M, Pfannkuche K, Rajewsky K, Edenhofer F. Ability of the hydrophobic FGF and basic TAT peptides to promote cellular uptake of recombinant Cre recombinase: a tool for efficient genetic engineering of mammalian genomes. Proc Natl Acad Sci U S A. 2002;99(7):4489–4494. doi: 10.1073/pnas.032068699. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.