Abstract
Introduction
The antegrade pressure measurement (APM) or perfusion pressure-flow test (Whitaker test) is a method of antegrade measurement of pressure in the upper urinary tract. In this study, we present the long-term follow-up results of APMs performed in our institution in the late 1980s and early 1990s to see whether the diagnostic decisions that were based on the outcomes of the test prove to be correct in the long term.
Materials and methods
We conducted a retrospective study by searching our hospital’s electronic database. We found a total of 16 APMs performed between 1987 and 1995 (10 boys, six girls; mean age 61 months).
Results
In nine cases, action was undertaken immediately after the APM had been performed; in seven cases, this was a surgical procedure (re-implantation/re-calibration or pyeloplasty) after obstruction was demonstrated. In two cases (both postoperative after previous pyeloplasty), absence of obstruction was demonstrated and nephrostomy tubes were subsequently closed. In one case, this resulted in hydronephrosis that had to be treated with a new JJ stent. In all the seven cases in which no action was deemed necessary as a result of the outcome of the APM, long-term follow-up showed that intervention had indeed not been necessary.
Conclusion
Although not often used anymore, the APM seems to be a safe and valuable diagnostic tool in the work up for possible urinary tract obstruction in children, especially in cases in which there is serious doubt concerning conservative watchful waiting.
Keywords: Whitaker test, Antegrade pressure recording, Antegrade pressure measurement, UPJ stenosis, UVJ stenosis
Introduction
Antegrade pressure measurement (APM), also called the perfusion pressure-flow or Whitaker test, is a method of antegrade measurement of pressure in the upper urinary tract. It was first described by Whitaker in 1973 and was designed to establish whether or not urinary tract dilatation is caused by obstruction (Fig. 1) [1]. The test can be used to investigate a suspected ureteropelvic junction (UPJ) obstruction or ureterovesical junction (UVJ) obstruction. At our institution, the method was used in the late 1980s and early 1990s in order to evaluate the possible presence of UPJ and UVJ obstruction. However, since then the use of APM as a diagnostic tool in the evaluation of possible UVJ and UPJ obstruction has mostly been discarded. The main goal of this study is to evaluate whether there is still a place for APMs, by assessing the long-term follow-up results from the late 1980s and early 1990s and by reviewing relevant literature on this issue.
Fig. 1.
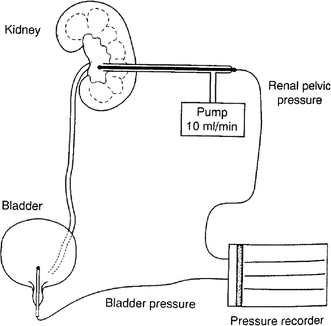
Antegrade pressure measurement set-up. Both pelvic and bladder pressures are measured in order to investigate suspected obstructing of the higher urinary tract (Image: De Jong TPVM, Van Gool JD. Pelviureteric junctional hydronephrosis. In: Atwell JD (red.) Pediatric Surgery. London: Arnold, 1998: 617–624.)
Materials and methods
A retrospective search was performed in the hospital’s electronic database. Sixteen APMs performed between 1987 and 1996 were traced (10 boys, six girls; mean age 61 months). Review of the histories showed doubt persisted on the presence or absence of obstruction with ultrasounds demonstrating dilated systems and inconclusive MAG3 or I-Hippuran renography. In all cases, remained serious doubt persisted on the presence or absence of obstruction after ultrasound of the dilated systems and inconclusive MAG3 or I-Hippuran renography. As shown in Table 1, the tests were performed for suspected UPJ or UVJ obstruction. In nine cases, there was a possible UPJ obstruction. These patients had a clinical image of obstructive uropathy with slightly deteriorating renal function, and some also had recurrent urinary tract infections. Ultrasound examination demonstrated a dilated pelvis in all of these patients. In seven cases, a possible UVJ obstruction was observed with the clinical image of an obstructive mega-ureter with or without nephropathy. In four cases, the patients had already had previous operations for UPJ or UVJ obstruction, and the APM was used to investigate possible recurrent obstruction. In two cases, the APM was carried out postoperatively shortly after a pyeloplasty, to examine possible recurrence of UPJ obstruction. In most cases (n = 13), the test was performed in the operating room under general anaesthesia. A ‘bedside’ evaluation was carried out in three cases where a nephrostomy tube had been placed because of acute pyelonephritis in a dilated system.
Table 1.
Patients who underwent APMs between 1987 and 1996
| Pt. | Agea | Sex | Indicationb | Locationc | Outcome (flow rates) | Action | Timed | Follow-upe |
|---|---|---|---|---|---|---|---|---|
| 1 | 13.8 | M | UPJOf suspected | OR | <10 cm H2O (at 20 ml/min) | PPg | 13.4 | No intervention |
| 2 | 59.2 | F | UVJOh suspected | OR | 25 cm H2O (at 6 ml/min) after infusing 125 ml | RC/RIi | 6.8 | No re-intervention |
| 3 | 114.2 | F | Re-UPJO suspected (pain, dilatation, ↓ renal function after previous pyeloplasty) | OR | <10 cm H2O (at 12 ml/min) | None | 14.2 | No re-intervention |
| 4 | 165.6 | M | UVJO suspected | Bedside | <10 cm H2O (at 20 ml/min) | None | 16 | No intervention |
| 5 | 22.6 | M | Re-UVJO suspected after previous re-calibration and re-implantation | OR | 17 cm H2O (at 5 ml/min): 26 cm H2O (at 10 ml/min) | RI | 14.5 | No re-intervention |
| 6 | 17.4 | F | UVJO suspected | OR | 0 cm H2O (at 10 ml/min): 10 cm H2O (at 20 ml/min) | None | 9.9 | No intervention |
| 7 | 92.7 | M | UVJO suspected | OR | 20 cm H2O (at 10 ml/min) | RC/RI | 3.5 | No re-intervention |
| 8 | 13.4 | M | UPJO suspected | OR | >20 cm H2O (at 10 ml/min) | PP | 5.7 | No re-intervention |
| 9 | 39 | F | UPJO suspected | OR | 0 cm H2O (at 20 ml/min) | None | 15.8 | No intervention |
| 10 | 19.9 | M | UVJO suspected | OR | Failure, pelvis too small | RC/RI | 8 | No re-intervention |
| 11 | 195 | M | UPJO suspected | OR | 0 cm H2O (at 10 ml/min) | None | 17.5 | No intervention |
| 12 | 102.5 | F | UVJO suspected | OR | >40 ml H2O (10 ml/min) | RI | 9.5 | No re-intervention |
| 13 | 4.2 | M | UPJO suspected | OR | <10 cm H2O (at 10 ml/min) | None | 15.5 | No intervention |
| 14 | 82.2 | M | Re-UPJO suspected | OR | 7 cm H2O (at 10 ml/min) | None | 4.8 | No intervention |
| 15 | 34.1 | F | Re-UPJO suspected after previous pyeloplasty | Bedside | 17 cm H2O (at 10 ml/min) | Nephrostomy closed | 13.8 | Needed new JJ-stent later on |
| 16 | 0.1 | M | Evaluation after pyeloplasty complicated by urinoma (treated by nephrostomy) | Bedside | 10 cm H2O (at 10 ml/min); if abdominal pressure rises: 20 cm H2O (at 10 ml/min) | Nephrostomy closed | 12.5 | No intervention |
aAge in months, at the time APM was performed
bReason for the APM
cPlace where APM was performed: at OR (operating room) or a bedside test
dDuration of follow-up (peripheral or in our own centre) in years
eWas there a re-intervention or intervention during follow-up?
fUreteropelvic junction obstruction
gPyeloplasty (Anderson-Hynes)
hUreterovesical junction obstruction
i RC re-calibration; RI re-implantation
Subsequently, the clinical records of all the patients who had undergone APM were studied carefully to see how these patients fared clinically in the years following the APM test. Special attention was given to complaints, physical examination, ultrasound (dilatation), renal functioning and the necessity of re-intervention in the long term. The latter was especially of interest, given that the aim of the present study was to evaluate the diagnostic value of the APM in the long term.
Procedure
During an APM, the differential pressure across a suspected obstruction is measured (Fig. 1). This is done by an infusion of 10 ml/min saline or watery contrast medium in case of fluoroscopy, through a nephrostomy tube (or a percutaneously inserted needle) with a 3Fr Micro-tip catheter in the renal pelvis inserted through this catheter or needle, while bladder pressure is measured by a 6Fr Micro-tip catheter inserted transurethrally. In all patients, the same flow rate was used. The intrapelvic and bladder pressures are measured with a standard urodynamic set-up (MMS®). The differential pressure between pelvis and bladder is given by the detrusor pressure channel. During the study, the filling state of both the renal pelvis and the bladder is controlled by ultrasound or fluoroscopy to make sure that a steady state of dilatation has been reached and that no bladder overdistension occurs.
Differential pressures of between 12 and 15 cm H2O were considered normal, whereas pressures of over 20 cm H2O were considered obstructive. Values between 15 and 20 mm H2O were considered to be indeterminate. If high pressures were measured, patients were subsequently treated for existing UPJ obstruction with a dismembered pyeloplasty and for UVJ obstruction with re-calibration and re-implantation (Politano-Leadbetter method with a Starr type plication of the ureter). If pressures were found to be normal or low, no surgical procedures were performed and the patients were followed using regular ultrasound control and, if feasible, renograms.
Results
The results are also displayed in Table 1; flow rates are given between bars. Sometimes, when no obstruction could be demonstrated using low flow rates (10 ml/min), higher flow rates up till 20 ml/min were tried.
No complications occurred during or shortly after the tests. In seven cases, surgical procedures were performed immediately after the test. In two cases (both bedside tests), nephrostomy tubes were closed because no obstruction was found during the test. In nine cases, no action was taken following the APM since no obstruction could be demonstrated. No surgical intervention was performed, and conservative measures were taken.
Mean follow-up after the test was 12 years (range 3.5–17.5 years). After a mean follow-up of 2 years, most patients were referred back to peripheral pediatricians. Here, they were seen back once a year. None of the patients who were not treated surgically because the APM showed low differential pressures, needed intervention later on during follow-up (n = 7). The interpretation of the APM was right about the absence of obstruction in 100% of cases, suggesting a high negative predictive value of the test. All these patients kept doing well clinically and developed no signs or symptoms of higher urinary tract obstruction in the long term. Only one case (patient no. 15) needed re-intervention; however, this patient can be considered an exceptional case. In this patient, a differential pressure of <20 cm H2O was measured during a bedside test. This test was carried out to evaluate the possible presence of re-stenosis after previous pyeloplasty. Since no obstruction was demonstrated, the nephrostomy tube was closed. The patient started to develop clinically apparent hydronephrosis soon after the closure, treated with a temporary JJ-stent. This was the only case in which re-intervention was needed.
Discussion
Isotope scan and ultrasound, the current routine tools, are used to determine whether a hydronephrosis represents a dilated or an obstructed system, sometimes fail to give a definitive answer. This may be the case in kidneys with a severe impairment of function or in patients with bilateral dilated upper tracts. In those cases, APM can discriminate between dilatation and obstruction.
We reviewed the APMs performed in our institution in the late 1980s and early 1990s to see whether, at long-term follow-up, APM proved to be a reliable diagnostic tool. In patients who were operated on after APM, it will always be impossible to prove that the decision, made on the outcome of APM, was completely justified. However, in patients that were followed conservatively, absence of progression of obstruction can be used as a tool to measure the efficacy and safety of the APM. In our series, the APM proved to be a reliable diagnostic tool to evaluate the presence or absence of UPJ or UVJ obstruction, with only one wrongly interpreted outcome in 16 cases (patient no. 15). Of particular note is that for the seven patients with negative Whitaker evaluations only one required a temporary ureteral stent during long-term follow-up, supporting that the Whitaker test has a high negative predictive value. Also, since no complications were reported, the test seems to be safe. With this in mind, the question arises why APM is not used more often nowadays.
The APM certainly has its drawbacks [2]. First, the test does not actually define or measure obstruction: It only records the pressure in the renal pelvis during unphysiologically high flow rates. At normal flow rates, these pressures may never occur. In children, the pelvis and ureter are usually rather compliant, making such high pressures even more unlikely in the physiological situation. Only few patients with a poor renal concentrating ability will ever reach a flow rate of >10 ml/min. Bearing this in mind, it is imported to note that although some clinicians prefer to adjust flow rates to body size (i.e., increasing flow rates in larger patients), this will probably result in more false-positive outcomes, decreasing the reliability of the test; this is also the reason why we chose to use the same amounts of pressure in all patients, regardless of patient body size. In addition, there is also the risk that the test is terminated before the pyelocaliceal system is full or before the bladder has been filled to capacity. This means that ultrasound control or fluoroscopy is needed during pressure measurement to make sure that a true steady state has been reached. A further drawback is the invasive nature of the APM. Non-invasive alternatives are widely available and have proven their diagnostic value in most cases. These alternatives include the diuretics renogram and MRI; the latter has only recently been introduced [2]. In kidneys with a huge dilatation or with a differential function of less than 20%, both renogram and MRI can fail to give a definitive diagnosis.
Given these drawbacks, the main question is whether there is still a role for the APM in contemporary (pediatric) urological practice. As early as 1979, Whitaker commented on his own method that “it is not a panacea for all obstructions and should not be used as a short cut to a quick diagnosis” [3]. He never intended his own test to be a first-line diagnostic tool and neither did he advocate blind obedience to a pathognomonic number; the test is meant for a select group of patients in which crucial clinical decisions were hampered by the limitations of accepted diagnostic tests [4]. Later, in 1984, Whitaker et al. [5] showed that the renogram failed to confirm the absence or presence of equivocal urinary tract obstruction as shown by the APM in 39% of all cases (n = 32), thus showing the added value of the APM in the diagnostic work up of urinary tract obstruction. However, once again, the APM was considered an extra measure in the event of equivocal results from the previous examinations. Wolf et al. [6] showed in 1996 that in adults, urography and diuretic scintigraphy are sufficient in the standard diagnostic work up for urinary tract obstruction; the APM is again mentioned to be ‘additional’. A study similar to the one undertaken by Whitaker in 1984 was conducted in 1999 in 34 children by Dacher et al. [7]. This study demonstrated that pressure-flow tests can be considered in children with equivocal outcomes of their (99 m)-Tc-DTPA furosemide diuresis renography. More recently, Lupton et al. [8] reviewed their 25 years of experience with APM in 143 patients who had all undergone at least one APM. Taking diuresis renography as the gold standard, they found that the APM predicted the right outcome in 77% of all cases (both obstructed and non-obstructed). They concluded that the APM indeed has a role to play in modern urology under the following circumstances: (1) equivocal results from less invasive tests, (2) suspected obstruction with poor kidney function, (3) loin pain with a negative diuresis renogram (in the event of poor renal function, the diuretic renogram may be falsely negative because the diuretic may not sufficiently raise the urine flow), (4) suspected intermittent obstruction and (5) gross dilatation with a positive diuresis renogram.
Most important advantage of this study is that the message about the value of the Whitaker test becomes clear. Also, its results are consistent with the previous literature. The main drawback of this study is the relative small sample size of 16 patients. Also, due to the retrospective nature of this series and the varying indications why the Whitaker test was eventually performed in these patients, many details like outcomes of renal scintigraphy performed during follow-up were not available (anymore).
It can be concluded that under certain circumstances, the APM has indeed a role to play in the evaluation of equivocal higher urinary tract obstruction, especially when previous performed non-invasive investigations as renal scintigraphy and ultrasound are non-conclusive. Our study group is too small to reach a definite conclusion; however, the long-term result of the absence of obstruction in our group and previously published studies shows that, in selected cases, APM still has a role to play as a diagnostic tool in modern-day urology.
Conclusion
Although not used very often anymore, the APM seems to be a safe and valuable diagnostic tool in the work up for possible urinary tract obstruction in children in whom routine investigations fail to give a definitive answer about the presence or absence of obstruction.
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- APM
Antegrade pressure recording
- IVP
Intravenous pyelography
- MRI
Magnetic resonance imaging
- UPJ
Ureteropelvic junction
- UVJ
Ureterovesical junction
References
- 1.Whitaker RH. Methods of assessing obstruction in dilated ureters. Br J Urol. 1973;45(1):15–22. [PubMed] [Google Scholar]
- 2.Thoeny HC, Binser T, Roth B, et al. Noninvasive assessment of acute ureteral obstruction with diffusion-weighted MR imaging: a prospective study. Radiology. 2009;252:721. doi: 10.1148/radiol.2523082090. [DOI] [PubMed] [Google Scholar]
- 3.Djurhuus JC, Sorensen SS, Jorgensen TM, et al. Predictive value of pressure flow studies for the functional outcome of reconstructive surgery for hydronephrosis. Br J Urol. 1985;57:6–9. doi: 10.1111/j.1464-410X.1985.tb08974.x. [DOI] [PubMed] [Google Scholar]
- 4.Tchetgen MB, Bloom DA, Robert H. Whitaker and the APR: a pressure-flow study of the upper urinary tract. Urology. 2003;61(1):253–256. doi: 10.1016/S0090-4295(02)01545-5. [DOI] [PubMed] [Google Scholar]
- 5.Whitaker RH, Buxton-Thomas MS. A comparison of pressure flow studies and renography in equivocal upper urinary tract obstruction. J Urol. 1984;131:446. doi: 10.1016/s0022-5347(17)50442-5. [DOI] [PubMed] [Google Scholar]
- 6.Wolf JS, Jr, Siegel CL, Brink JA, Clayman RV. Imaging for ureteropelvic junction obstruction in adults. J Endourol. 1996;10(2):93–104. doi: 10.1089/end.1996.10.93. [DOI] [PubMed] [Google Scholar]
- 7.Dacher J, Pfister C, Thoumas D, Véra P, Liard-Zmuda A, Chomant J, Mitrofanoff P, Le Dosseur P. Shortcomings of diuresis scintigraphy in evaluating urinary obstruction: comparison with pressure flow studies. Pediatr Radiol. 1999;29(10):742–747. doi: 10.1007/s002470050687. [DOI] [PubMed] [Google Scholar]
- 8.Lupton EW, George NJ. The APR: 35 years on. BJU Int. 2010;105(1):94–100. doi: 10.1111/j.1464-410X.2009.08609.x. [DOI] [PubMed] [Google Scholar]


