Abstract
Objective
To identify an appropriate diagnostic tool for the early diagnosis of Acute Traumatic Coagulopathy (ATC) and validate this modality through prediction of transfusion requirements in trauma hemorrhage.
Design
Prospective observational cohort study
Setting
Level 1 trauma centre
Patients
Adult trauma patients who met the local criteria for full trauma team activation. Exclusion criteria included emergency department (ED) arrival >2 hours after injury, >2000ml of intravenous fluid before ED arrival or transfer from another hospital.
Interventions
None
Measurements
Blood was collected on arrival in ED and analysed with laboratory prothrombin time (PT), point of care (PoC) PT and rotational thromboelastometry (ROTEM). Prothrombin ratio (PTr) was calculated and ATC defined as laboratory PTr>1.2. Transfusion requirements were recorded for the first 12 hours following admission.
Main Results
300 patients were included in the study. Laboratory PT results were available at median 78 (62-103) minutes. PoC PTr had reduced agreement with laboratory PTr in patients with ATC, with 29% false negative results. In ATC the ROTEM Clot Amplitude at 5 minutes (CA5) was diminished by 42% and this persisted throughout clot maturation. ROTEM clotting time was not significantly prolonged. A CA5 threshold ≤35mm had a detection rate of 77% for ATC with a false positive rate of 13%. Patients with CA5 ≤35mm were more likely to receive red cell (46% vs 17%, p<0.001) and plasma (37% vs 11%, p<0.001) transfusions. The CA5 could identify patients who would require massive transfusion (detection rate of 71%, vs 43% for PTr >1.2, p<0.001).
Conclusions
In trauma hemorrhage PTr is not rapidly available from the laboratory and PoC devices can be inaccurate. ATC is functionally characterised by a reduction in clot strength. With a threshold of CA5 ≤35mm ROTEM can identify ATC at 5 minutes and predict the need for massive transfusion.
Keywords: ROTEM, Trauma, Hemorrhage, Coagulopathy, Diagnosis, Transfusion
INTRODUCTION
Hemorrhage accounts for over a third of early trauma deaths (1) and is a leading cause of preventable mortality (2). Up to 25% of severely injured patients arrive at hospital with a significant coagulopathy. Patients presenting with this Acute Traumatic Coagulopathy (ATC) have a mortality approaching 50% and significantly greater transfusion requirements, organ injury, septic complications and critical care stay (3-5). Management strategies targeting ATC may allow significant improvement in outcomes (6-8). These damage control resuscitation approaches require early identification of ATC to allow rapid activation of transfusion protocols. Prediction of ATC from admission clinical parameters is unreliable, while laboratory-based clotting tests have logistic issues limiting their utility in acute trauma care (9-10).
In the absence of a rapid diagnostic tool, current ATC management relies on empirical transfusion strategies activated on the basis of clinical surrogates or physician gestalt (11-13). This results in delayed correction of ATC and is associated with suboptimal blood product usage (14-15). Inadequate transfusion is associated with poor outcomes (12) but over-transfusion results in additional donor exposure and is wasteful of a precious resource. The need for an accurate modality to rapidly diagnose ATC has prompted a renewed interest in viscoelastic coagulation tests. These functional tests such as Rotational Thromboelastometry (ROTEM - Pentapharm, Munich, Germany) and Thromboelastography (TEG - Haemoscope Corp., Niles, IL) analyse whole blood and evaluate all stages of secondary haemostasis (16). The clinical application of this technology to guide blood replacement has been widely used in liver transplantation (17), cardiac surgery (18-19) and emergency vascular procedures (20). Emerging evidence suggests ROTEM may have diagnostic capability in ATC (21) and could potentially direct transfusion therapy in trauma hemorrhage (22-23).
The overall objective of the study was to identify an appropriate diagnostic tool for the early diagnosis of ATC. The first aim of the study was to evaluate Point of Care (PoC) Prothrombin Time (PT) as an alternative to the laboratory measurement of clotting times. The second aim was to determine the thromboelastometry profile of ATC. Third we aimed to identify a rapidly available parameter for the identification of patients with ATC. Lastly we wished to validate this threshold by its ability to predict transfusion requirements in trauma hemorrhage.
MATERIALS AND METHODS
Study design
This was a single centre, prospective, cohort study of trauma patients presenting directly to a level 1 trauma centre between January 2007 and June 2009. The study was reviewed and approved by the UK National Research Ethics Committee. We analysed baseline laboratory coagulation parameters on arrival for comparison with PoC PT, ROTEM, and base deficit (BD).
Setting
Major urban trauma centre with over 1400 trauma team activations per year of which 25% are severely injured with an injury severity score (ISS) >15. Penetrating trauma accounts for 21% of workload.
Massive Hemorrhage Protocol
Activation of the massive hemorrhage protocol was on the basis of clinical markers of shock (systolic blood pressure <90 mmHg, poor response to initial fluid infusion and suspicion of on-going hemorrhage) and provided immediate access to emergency PRBC units. FFP was subsequently provided with PRBCs with the aim of delivering a 2:3 ratio. Platelets and cryoprecipitate were automatically administered after the first four units of FFP if hemorrhage was ongoing. In the acute bleeding phase, transfusion was not guided by laboratory markers.
Patient Selection
All adult trauma patients (>15 years) who met the local criteria for full trauma team activation were eligible for enrolment and recruited into the study when research personnel were present (08:00-20:00 daily). Exclusion criteria were arrival in the emergency department (ED) more than 2 hours after injury; the administration of more than 2000ml of intravenous fluid prior to ED arrival; transfer from another hospital and burns covering more than 5% of the total body surface area. Patients were retrospectively excluded if they declined to give consent to use research samples collected; were found to be taking anticoagulant medications; had moderate or severe liver disease or a known bleeding diathesis.
Sampling Technique
A 20 mL research sample of blood was drawn from either the femoral vein or antecubital fossa along with the standard trauma laboratory tests within 20 minutes of arrival in ED. Blood for ROTEM analysis was drawn into a 2.7ml citrated vacutainer (0.109 M buffered sodium citrate, 3.2% - Becton Dickinson, Plymouth, UK) and processed in the trauma research laboratory. Samples for PT, PTT and fibrinogen were collected into 4.5ml glass vacutainers (0.109 M buffered sodium citrate, 3.2% - Becton Dickinson, Plymouth, UK) for standard processing by the central hospital laboratory along with a standard full blood count (FBC). PoC PT analysis was performed using a CoaguChek XS device (Roche Diagnostics Ltd, Burgess Hill, UK). Prothrombin ratio (PTr) was calculated as observed PT divided by mean control PT for both laboratory and PoC PT values to enable direct comparison. Arterial blood analysis for base deficit (BD) was performed simultaneously with the research sample collection.
ROTEM Analysis
Samples were processed within one hour of blood draw at 37°C on a ROTEM delta instrument (Pentapharm GmbH, Munich, Germany) and all treating clinicians were blinded to the results. The methodology and the parameters of ROTEM have previously been described in detail (16). 20μl of recalcitrant (STARTEM) and 20μl of tissue factor derived from rabbit brain (EXTEM) were placed into the test cuvette after which 300μl of the blood sample was added. Activation with tissue factor is performed to standardize the in vitro coagulation process and produce a more rapid result. All pipetting steps and the mixing of reagents with samples were performed as standard using the automated electronic pipette program. Clotting time (CT), alpha angle (α), clot formation time (CFT), clot amplitude at 5 minutes (CA5) and maximum clot firmness (MCF) were reported for each sample analyzed.
Data Collection and Analysis
Data were collected prospectively on patient demographics, time of injury, mechanism (blunt or penetrating), prehospital fluid administration, time of arrival in the ED, baseline vital signs and total transfusion requirements in the first 12 hours of admission. Injury was classified using the Injury Severity Score (ISS) as severe (>15) or uninjured (<5) (24). Hypoperfusion was defined as BD >6mEq/l (25-26). Massive transfusion was defined as a requirement of 10 or more units of blood in the first 12 hours.
ATC was defined as a laboratory PTr >1.2 (4-5, 27). In trauma PTr>1.2 has been shown to be a clinically relevant threshold associated with significant increases in mortality and transfusion requirements (27). We defined the Detection Rate as the proportion of patients with ATC that would be positively identified by PoC or ROTEM; and the False Positive Rate (FPR) as the proportion of patients without ATC that would be incorrectly identified as positive. We determined normal values for ROTEM parameters from patients without ATC (PTr ≤1.2, non-coagulopathic) as mean +/− 1 standard deviation. For analysis of ROTEM parameters not directly comparable to the PTr (eg. clot strength parameters), we also used the pathophysiologic basis of ATC to select a cohort of high-risk patients with a combination of severe injury (ISS >15) and shock (BD >6mEq/L) (27-28). Normal quantile plots were used to test for normal distribution. Non-parametric data are expressed as median, interquartile range and analysed with Mann-Whitney U test. Parametric data are expressed as mean ± 95% confidence intervals. Two-group analysis was performed with a two tailed unequal variance Student’s t test. A Bland Altman plot was used to test the clinical agreement between PoC and central laboratory PTr results. ROTEM changes over time were analysed using two-way ANOVA. To eliminate survivor bias, patients who died within 12 hours of admission we excluded from analysis of transfusion outcomes. A sensitivity analysis was performed to assess the impact of this methodology on test performance.
RESULTS
There were 325 patients enrolled into the study over the 19-month period. ROTEM sample analysis was incomplete in three patients, consent processes could not be completed in 15 cases and there were seven retrospective exclusions leaving 300 patients available for analysis. Clinical characteristics, admission physiology and laboratory parameters are detailed in Table 1. Median time from injury to blood sampling was 86 (69-112) minutes. Minimal intravenous fluid was administered prior to baseline sample collection and no patient received artificial colloid or vasoactive agents before the first blood draw.
Table 1. Clinical characteristics of trauma patients.
| Patients | |
| Number | 300 |
| Age | 33 (23-48) |
| Male | 246 (82%) |
| Times (minutes) | |
| Injury to ED arrival | 76 (57-101) |
| ED arrival to sampling | 9 (5-14) |
| Sampling to available laboratory PT result | 78 (62-102) |
| Injuries | |
| Injury severity score (ISS) | 12 (4-25) |
| ISS >15 | 126 (42%) |
| Penetrating injury | 62 (21%) |
| Admission physiology | |
| Systolic blood pressure <100 mmHg | 53 (18%) |
| Base deficit >6 mEq/L | 47 (14%) |
| Median PT (secs) | 10.9 (10.4-11.5) |
| PTr >1.2 | 23 (8%) |
| Intravenous fluids prior to baseline sample (mL) | 0 (0-400) |
| Transfusion requirements (first 12 hours) | |
| Any PRBC | 68 (23%) |
| PRBC >10 | 11 (4%) |
| FFP | 46 (15%) |
Values are median (IQR) or number of patients (%)
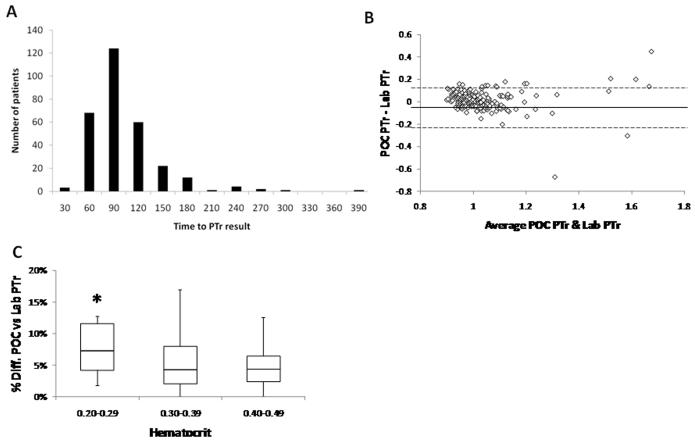
Laboratory PT results were available to clinicians via the hospital electronic record system with a median time of 78 (62-103) minutes (Figure 1A). In only two cases were results available in less than 30 minutes. Overall there was good agreement between the PoC and laboratory PTr results, with a mean bias of −1.4% (Figure 1B). However this agreement was confined to patients without coagulopathy, where 99% of PoC values were within 95% confidence intervals. Accuracy was lost in patients with ATC when only 71% of PoC PTr values were in agreement with the laboratory values (Figure 1B). 29% of PoC readings were false negative for ATC, and PoC had an overall ATC detection rate of 77% and a false positive rate of 23%. Low haematocrit (<0.30) was associated with larger discrepancies between PoC and laboratory results (vs 0.3-0.39, p =0.05; vs 0.4-0.49, p =0.04, Figure 1C).
Figure 1. Comparison and limitations of central laboratory PTr (Prothrombin Time ratio) and Point of Care (PoC) PTr measurements.
A: Histogram representation of the time delays incurred from individual blood draw (PTr sample acquisition) to availability of result on electronic patient record.
B: Comparison according to Bland and Altman of laboratory PTr assay with point of care (PoC) PTr assay. Solid line = mean bias (−0.015). Dotted line = 95% limits of agreement (−0.197 - 0.168).
C: Association of lower hematocrit levels in trauma hemorrhage with higher discrepancies between laboratory and PoC PTr assays. Median, inter-quartile and minimum/maximum ranges (Hematocrit: 0.2-0.29 vs 0.3-0.39, p =0.05; vs 0.4-0.49, p =0.04)
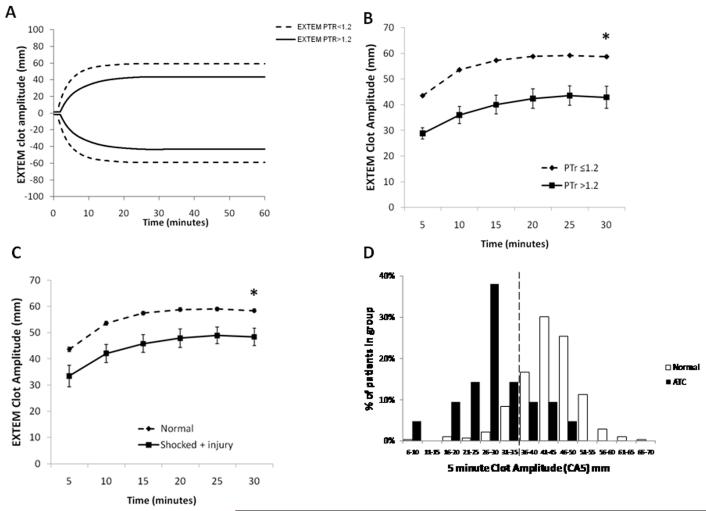
Computer simulated ROTEM graphs averaging data derived from all patients in the study produced a characteristic trace for patients with ATC (Figure 2A). Clot strength was diminished by 42% at 5 minutes (CA5 normal vs ATC, p<0.001) and persisted throughout clot maturation (40% reduction in MCF compared to normal, p<0.001 - Figure 2B). Comparing the two groups there was complete separation between all clot strength parameters but an overlap in ROTEM clotting times with only a trend toward prolongation in coagulopathic patients (116 vs 66 seconds, p=0.068) (Table 2).
Figure 2. Comparison of ROTEM traces and clot amplitudes from non-coagulopathic (PTr ≤1.2) vs coagulopathic (PTr >1.2) and the effect of shock and injury on thromboelastometry profiles.
A: Computer simulated EXTEM trace from averaged ROTEM data of all non-coagulopathic vs all coagulopathic patients.
B: Comparison of EXTEM clot amplitude over time from non-coagulopathic vs coagulopathic patients. Mean values ± SEM. 2-way ANOVA (p<0.001).
C: Combined effects of trauma (injury severity score >15) and shock (base deficit >6) on the ROTEM trace. Comparison of clot amplitudes over time: “normal” trauma patients (uninjured and no shock) vs patients with severe injury and shock. Mean values ± SEM. 2-way ANOVA (p<0.001).
D: Histogram demonstrating spread of clot amplitude at 5 minutes (CA5) amongst normal and ATC patients. Dotted line represents new threshold for ATC (CA5 ≤35mm).
Table 2. Comparison of ROTEM and clotting screen parameters: normal vs coagulopathic patients.
| Normal | ATC | p value | |
|---|---|---|---|
|
| |||
| EXTEM | |||
| CT (secs) | 66 (63-69) | 116 (62-170) | 0.068 |
| CFT (secs) | 97 (92-101) | 169 (135-203) | <0.001 |
| Alpha angle (°) | 71 (71-72) | 61 (57-65) | <0.001 |
| CA5 (mm) | 44 (43-44) | 28 (23-33) | 0.001 |
| MCF (mm) | 60 (59-60) | 46 (40-52) | 0.001 |
| Clotting screen | |||
|
Platelets
(x106/L) |
245 (237-253) | 174 (146-201) | <0.001 |
|
Fibrinogen
(g/dL) |
2.2 (2.13-2.28) | 0.96 (0.74- 1.18) |
<0.001 |
Patients defined as Normal: Prothrombin Time ratio (PTr) ≤1.2 or ATC: PTr >1.2. Values are mean (95% confidence intervals). P value: unpaired Student’s t test. Clotting Time (CT), Clot Formation Time (CFT), Clot Amplitude at 5 minutes (CA5), Maximum Clot Firmness (MCF).
As clot strength is not directly comparable with the PTr we also analysed the ROTEM signatures of patients at high risk of ATC (combination of injury and shock). This cohort had significantly lower clot strengths compared to uninjured, non-shocked patients (p<0.001) (Figure 2C). The co-existence of shock and injury had a synergist negative effect on clot strength (22% reduction in CA5; 15% reduction in MCF) compared to uninjured patients without shock (Table 3). The clotting time was only mildly prolonged in patients with combined injury and shock (Table 3). ATC is thus characterised by a reduction in clot strength and only minimal changes in clotting times.
Table 3. Influence of shock and injury on ROTEM measures of coagulation.
| Non- shocked without injury |
Shocked without injury |
Injury without shock |
Injury with shock |
|
|---|---|---|---|---|
|
| ||||
| n | 64 | 3 | 7 | 33 |
| CT (secs) | 69 (64-74) | 58 (19-97) | 61 (56-66) | 88 (51-125)* |
| CFT (secs) | 92 (86-98) | 89 (17-160) | 94 (83-105) | 132 (114- 150)* |
| Alpha angle (°) | 72 (71-73) | 72 (59-85) | 72 (70-74) | 66 (63-68)* |
| CA5 (mm) | 44 (43-46) | 43 (25-61) | 45 (43-47) | 34 (31-38)* |
| MCF (mm) | 60 (59-61) | 57 (42-72) | 61 (59-62) | 52 (48-56)* |
| PTr>1.2 (%) | 3.1% | 0.0% | 4.9% | 33.3%* |
|
CA5 ≤35mm
(%) |
9.2% | 33.3% | 11.5% | 60.6%* |
Shock and injury defined as base deficit (BD) >6 mmol/l and injury severity score (ISS) >15 respectively. Values are mean (95% confidence intervals). Clotting Time (CT), Clot Formation Time (CFT), Clot Amplitude at 5 minutes (CA5), Maximum Clot Firmness (MCF).
p<0.05 compared to shock(−) injury (−) cohort (unpaired Student’s t test or chi squared for percentages).
Therefore we examined the potential for ROTEM to detect patients with ATC based on a clot strength parameter. We chose the 5-minute clot amplitude as there was good separation of normal and ATC curves at this time-point (Figure 2B and 2C) and set a threshold of CA5 at 35mm, representing one standard deviation below normal – Table 2). 54 patients (18%) had a low CA5 compared to 23 (8%) patients with PTr >1.2. The CA5 ≤35mm threshold had a detection rate of 77% for patients with ATC and a false positive rate of 13% (Figure 2D). For the high-risk cohort (severe injury and shock), 61% of patients had CA5 ≤35 compared to 33% with a PTr >1.2 (Table 3).
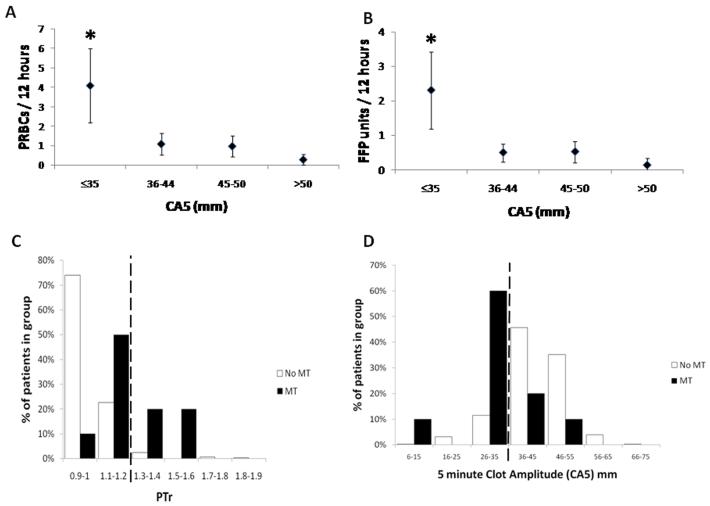
Average PRBC transfusion requirements for patients with CA5≤35 were 4 vs 1 units (p<0.001) (Figure 3A) and this cohort were three times more likely to receive PRBCs (46% vs 17%, p<0.001). Patients with low CA5 also had a greater likelihood of receiving FFP (37% vs 11%, p<0.001) with average plasma transfusion requirements of 2 vs 0 units (p<0.001) (Figure 3B). The CA5 ≤35mm threshold was able to predict massive transfusion (10+ PRBC units) with a detection rate of 71% compared to 43% for a PTr-based definition of ATC (Table 4). A sensitivity analysis demonstrated that the inclusion of patients who died within 12 hours of admission produced only a minimal effect on the accuracy of the model (73% detection rate for 10+ PRBC units). Nearly 60% of patients requiring massive transfusion had a normal PTr but only 30% had a normal CA5 (Figures 3C & 3D). Overall CA5 >35mm had a negative predictive value (NPV) of 83% for any red cell transfusion and 99% for massive transfusion (10+ units) (Table 4) with an AUC of 0.803 (95% CI: 0.635 to 0.972).
Figure 3. Average transfusion requirements based on ROTEM clot strength at 5 minutes.
A: Mean PRBC transfusion requirement. p<0.001 comparing CA5≤35 with CA5 36-44, CA5 45-50 and CA5>50. Mean ± 95% confidence intervals. Clot Amplitude at 5 minutes (CA5).
B: Mean FFP transfusion requirement. p<0.001 comparing CA5≤35 with CA5 36-44, CA5 45-50 and CA5>50. Mean ± 95% confidence intervals.
C: Histogram of proportional distribution in PTr for patients receiving massive transfusion (MT) vs those not receiving MT. Dotted line represents threshold for ATC (PTr >1.2).
D: Histogram of proportional distribution of CA5 for patients receiving MT vs those not receiving MT. Dotted line represents new ROTEM threshold for ATC based on clot strength (CA5 ≤35mm).
Table 4. Prediction of blood products and massive transfusion.
| Transfusion | Detection Rate |
FPR | PPV | NPV |
|---|---|---|---|---|
|
| ||||
| Any PRBC | ||||
| PTr >1.2 | 17.5% | 3.9% | 55.0% | 81.0% |
| CA5≤35 mm | 33.3% | 12.1% | 42.9% | 82.9% |
| CT >94 s | 17.7% | 10.8% | 30.6% | 80.2% |
| α angle <65° | 23.8% | 7.4% | 46.8% | 81.6% |
|
Massive
Transfusion |
||||
| PTr >1.2 | 42.9% | 5.9% | 15.0% | 98.4% |
| CA5≤35 mm | 71.4% | 15.3% | 10.2% | 99.2% |
| CT >94 s | 28.6% | 12.2% | 5.4% | 98.1% |
| α angle <65° | 42.9% | 10.1% | 9.4% | 98.5% |
| FFP | ||||
| PTr >1.2 | 21.4% | 4.4% | 45.0% | 88.0% |
| CA5≤35 mm | 35.7% | 13.4% | 30.6% | 89.0% |
| CT >94 s | 14.6% | 11.9% | 16.7% | 86.4% |
| α angle <65° | 26.2% | 8.4% | 34.4% | 88.1% |
Performance of coagulation parameters for the prediction of packed red blood cell (PRBC), Massive Transfusion (10 or more units of PRBC) and fresh frozen plasma (FFP) transfusion using laboratory Prothrombin Time ratio (PTr) and ROTEM: CA5 (Clot Amplitude at 5 minutes), CT (Clotting Time). Detection Rate (Sensitivity); FPR (False Positive Rate: 1-Specificity); PPV (Positive Predictive Value) and NPV (Negative Predictive Value).
DISCUSSION
This study is the largest prospective evaluation of diagnostic modalities for ATC to date. We have confirmed that laboratory clotting times are not available within clinically useful timeframes, and that PoC devices that measure prothrombin time can be inaccurate in ATC and trauma hemorrhage. ATC has a characteristic thromboelastogram which is characterised by a reduction in clot strength with much smaller changes in laboratory clotting times. Based on these results a clot strength parameter derived from the thromboelastometry curve at 5 minutes may provide a more clinically relevant definition of ATC and can more accurately predict the need for massive transfusion than standard clotting tests.
Traditional coagulation screening tests are the basis of current definitions of ATC. PT and APTT however do not assess the whole coagulation system and use clot formation as their endpoint, which occurs when only a limited proportion of all physiologically relevant thrombin is formed. These static tests identify variable reductions in the levels of coagulant factors but may have limited value in managing severe hemorrhage (29-32). ATC however is not thought to be a consumptive coagulopathy and levels of clotting factors are probably preserved initially (33). CT, the ROTEM equivalent of PT, is not significantly prolonged in ATC. In the setting of ATC, the PT is the least correlated parameter with ROTEM and provides only partial information on clot initiation with no information on clot strength, the rate of clot propagation or clot lysis. Based on the evidence from this study and others it appears that both laboratory and PoC PT assays are inadequate for the diagnosis of ATC in trauma hemorrhage (34).
ATC has a thromboelastometry signature profile characterised by slow clot formation and persistently reduced clot strength of around 40%. The low uptake of ROTEM and TEG in clinical practice may be due to perceived difficulties in the interpretation of the visco-elastic clot traces. We have shown that a reliable and clinically important diagnostic reading can be made after 5 minutes using a single parameter. A CA5 ≤35mm threshold identifies more coagulopathic patients than PTr 1.2 and we found this ROTEM definition to be more sensitive than PTr for predicting the need for massive transfusion. This finding is supported by a previous study of 44 combat casualties which found that TEG maximum amplitude within the first 24 hours was a better predictor of transfusion than conventional clotting tests (35). All ROTEM parameters had negative predictive values approaching 100% for massive transfusion. A normal ROTEM trace may allow timely termination of massive hemorrhage protocols and preservation of blood stocks.
This study has several limitations. Firstly samples were only collected at a single time point on arrival and serial sampling during initial resuscitation may have yielded higher diagnostic accuracy and predictive power. Secondly a single PoC device was evaluated and the inaccuracies at high PT values may not translate to other technologies. Thirdly the aim of the study was to examine ATC and not multifactorial pathology of trauma induced coagulation (TIC). This study only focused on the measurement of a hypocoagulable state in bleeding patients and we did not attempt to examine hyperfibrinolysis which is an important component of ATC (36-37). The new definition of ATC may therefore not be a definition of TIC and applicable to patients with longer prehospital times or those who receive large volume crystalloid resuscitation. Further studies are needed to validate the CA5≤35mm diagnostic threshold for ATC.
CONCLUSIONS
Conventional clotting screening assays, whether laboratory-based or point-of-care, have significant limitations restricting their utility in trauma hemorrhage. ATC is primarily characterized by a reduction in clot strength and has a specific thromboelastometry signature which can be diagnosed by the clot amplitude at five minutes. ROTEM can rapidly identify patients who are likely to require massive transfusion. Prospective evaluation is required to assess whether ROTEM can be used to activate massive hemorrhage protocols and guide transfusion therapy.
Acknowledgements
The authors would like to acknowledge Professor Joan Morris for her assistance with the statistical analysis of this study
Funding Sources
Supported by the National Institute for Health Research: Programme Grant for Applied Research (RP-PG-0407-10036). Rupert Pearse is a National Institute for Health Research (UK) Clinician Scientist. Pentapharm GmbH (Munich, Germany) provided ROTEM reagent and equipment on an unrestricted basis.
Footnotes
Dr. Davenport and Dr. Brohi received unrestricted reagent/equipment grants from ROTEM. The remaining authors have not disclosed any potential conflicts of interest.
Institution
Trauma Sciences, Blizard Institute, Bart’s and the London School of Medicine & Dentistry, Queen Mary University of London
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, et al. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995 Feb;38(2):185–93. doi: 10.1097/00005373-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006 Sep;244(3):371–80. doi: 10.1097/01.sla.0000234655.83517.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. J Trauma. 2003 Jun;54(6):1127–30. doi: 10.1097/01.TA.0000069184.82147.06. [DOI] [PubMed] [Google Scholar]
- 4.Maegele M, Lefering R, Yucel N, Tjardes T, Rixen D, Paffrath T, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 2007 Mar;38(3):298–304. doi: 10.1016/j.injury.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 5.MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma. 2003 Jul;55(1):39–44. doi: 10.1097/01.TA.0000075338.21177.EF. [DOI] [PubMed] [Google Scholar]
- 6.Gunter OL, Jr., Au BK, Isbell JM, Mowery NT, Young PP, Cotton BA. Optimizing outcomes in damage control resuscitation: identifying blood product ratios associated with improved survival. J Trauma. 2008 Sep;65(3):527–34. doi: 10.1097/TA.0b013e3181826ddf. [DOI] [PubMed] [Google Scholar]
- 7.Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008 Sep;248(3):447–58. doi: 10.1097/SLA.0b013e318185a9ad. [DOI] [PubMed] [Google Scholar]
- 8.Maegele M, Lefering R, Paffrath T, Tjardes T, Simanski C, Bouillon B. Red-blood-cell to plasma ratios transfused during massive transfusion are associated with mortality in severe multiple injury: a retrospective analysis from the Trauma Registry of the Deutsche Gesellschaft fur Unfallchirurgie. Vox Sang. 2008 Aug;95(2):112–9. doi: 10.1111/j.1423-0410.2008.01074.x. [DOI] [PubMed] [Google Scholar]
- 9.Toulon P, Ozier Y, Ankri A, Fleron MH, Leroux G, Samama CM. Point-of-care versus central laboratory coagulation testing during haemorrhagic surgery. A multicenter study. Thromb Haemost. 2009 Feb;101(2):394–401. [PubMed] [Google Scholar]
- 10.Segal JB, Dzik WH. Paucity of studies to support that abnormal coagulation test results predict bleeding in the setting of invasive procedures: an evidence-based review. Transfusion. 2005 Sep;45(9):1413–25. doi: 10.1111/j.1537-2995.2005.00546.x. [DOI] [PubMed] [Google Scholar]
- 11.Malone DL, Hess JR, Fingerhut A. Massive transfusion practices around the globe and a suggestion for a common massive transfusion protocol. J Trauma. 2006 Jun;60(6 Suppl):S91–6. doi: 10.1097/01.ta.0000199549.80731.e6. [DOI] [PubMed] [Google Scholar]
- 12.Geeraedts LM, Jr., Demiral H, Schaap NP, Kamphuisen PW, Pompe JC, Frolke JP. ‘Blind’ transfusion of blood products in exsanguinating trauma patients. Resuscitation. 2007 Jun;73(3):382–8. doi: 10.1016/j.resuscitation.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007 Feb;62(2):307–10. doi: 10.1097/TA.0b013e3180324124. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez EA, Moore FA, Holcomb JB, Miller CC, Kozar RA, Todd SR, et al. Fresh frozen plasma should be given earlier to patients requiring massive transfusion. J Trauma. 2007 Jan;62(1):112–9. doi: 10.1097/01.ta.0000250497.08101.8b. [DOI] [PubMed] [Google Scholar]
- 15.Hess JR, Hiippala S. Optimizing the use of blood products in trauma care. Crit Care. 2005;9(Suppl 5):S10–4. doi: 10.1186/cc3780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ganter MT, Hofer CK. Coagulation monitoring: current techniques and clinical use of viscoelastic point-of-care coagulation devices. Anesth Analg. 2008 May;106(5):1366–75. doi: 10.1213/ane.0b013e318168b367. [DOI] [PubMed] [Google Scholar]
- 17.Kang Y. Thromboelastography in liver transplantation. Semin Thromb Hemost. 1995;21(Suppl 4):34–44. [PubMed] [Google Scholar]
- 18.Shore-Lesserson L, Manspeizer HE, DePerio M, Francis S, Vela-Cantos F, Ergin MA. Thromboelastography-guided transfusion algorithm reduces transfusions in complex cardiac surgery. Anesth Analg. 1999 Feb;88(2):312–9. doi: 10.1097/00000539-199902000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Spiess BD, Gillies BS, Chandler W, Verrier E. Changes in transfusion therapy and reexploration rate after institution of a blood management program in cardiac surgical patients. J Cardiothorac Vasc Anesth. 1995 Apr;9(2):168–73. doi: 10.1016/S1053-0770(05)80189-2. [DOI] [PubMed] [Google Scholar]
- 20.Johansson PI, Stensballe J. Effect of Haemostatic Control Resuscitation on mortality in massively bleeding patients: a before and after study. Vox Sang. 2009 Feb;96(2):111–8. doi: 10.1111/j.1423-0410.2008.01130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rugeri L, Levrat A, David JS, Delecroix E, Floccard B, Gros A, et al. Diagnosis of early coagulation abnormalities in trauma patients by rotation thrombelastography. J Thromb Haemost. 2007 Feb;5(2):289–95. doi: 10.1111/j.1538-7836.2007.02319.x. [DOI] [PubMed] [Google Scholar]
- 22.Schochl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert G, et al. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM(R))-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care. 2010 Apr 7;14(2):R55. doi: 10.1186/cc8948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brenni M, Worn M, Bruesch M, Spahn DR, Ganter MT. Successful rotational thromboelastometry-guided treatment of traumatic hemorrhage, hyperfibrinolysis and coagulopathy. Acta Anaesthesiol Scand. 2010 Jan;54(1):111–7. doi: 10.1111/j.1399-6576.2009.02132.x. [DOI] [PubMed] [Google Scholar]
- 24.Baker SP, O’Neill B, Haddon W, Jr., Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974 Mar;14(3):187–96. [PubMed] [Google Scholar]
- 25.Eastridge BJ, Malone D, Holcomb JB. Early predictors of transfusion and mortality after injury: a review of the data-based literature. J Trauma. 2006 Jun;60(6 Suppl):S20–5. doi: 10.1097/01.ta.0000199544.63879.5d. [DOI] [PubMed] [Google Scholar]
- 26.Davis JW, Parks SN, Kaups KL, Gladen HE, O’Donnell-Nicol S. Admission base deficit predicts transfusion requirements and risk of complications. J Trauma. 1996 Nov;41(5):769–74. doi: 10.1097/00005373-199611000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Frith D, Goslings JC, Gaarder C, Maegele M, Cohen MJ, Allard S, et al. Definition and drivers of acute traumatic coagulopathy: clinical and experimental investigations. J Thromb Haemost. 2010 Jun 10; doi: 10.1111/j.1538-7836.2010.03945.x. [DOI] [PubMed] [Google Scholar]
- 28.Brohi K, Cohen MJ, Ganter MT, Matthay MA, Mackersie RC, Pittet JF. Acute traumatic coagulopathy: initiated by hypoperfusion: modulated through the protein C pathway? Ann Surg. 2007 May;245(5):812–8. doi: 10.1097/01.sla.0000256862.79374.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Counts RB, Haisch C, Simon TL, Maxwell NG, Heimbach DM, Carrico CJ. Hemostasis in massively transfused trauma patients. Ann Surg. 1979 Jul;190(1):91–9. doi: 10.1097/00000658-197907000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuan S, Ferrell C, Chandler WL. Comparing the prothrombin time INR versus the APTT to evaluate the coagulopathy of acute trauma. Thromb Res. 2007;120(1):29–37. doi: 10.1016/j.thromres.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Miller RD, Robbins TO, Tong MJ, Barton SL. Coagulation defects associated with massive blood transfusions. Ann Surg. 1971 Nov;174(5):794–801. doi: 10.1097/00000658-197111000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ciavarella D, Reed RL, Counts RB, Baron L, Pavlin E, Heimbach DM, et al. Clotting factor levels and the risk of diffuse microvascular bleeding in the massively transfused patient. Br J Haematol. 1987 Nov;67(3):365–8. doi: 10.1111/j.1365-2141.1987.tb02359.x. [DOI] [PubMed] [Google Scholar]
- 33.Hess JR, Brohi K, Dutton RP, Hauser CJ, Holcomb JB, Kluger Y, et al. The coagulopathy of trauma: a review of mechanisms. J Trauma. 2008 Oct;65(4):748–54. doi: 10.1097/TA.0b013e3181877a9c. [DOI] [PubMed] [Google Scholar]
- 34.Kashuk JL, Moore EE, Sawyer M, Le T, Johnson J, Biffl WL, et al. Postinjury coagulopathy management: goal directed resuscitation via POC thrombelastography. Ann Surg. 2010 Apr;251(4):604–14. doi: 10.1097/SLA.0b013e3181d3599c. [DOI] [PubMed] [Google Scholar]
- 35.Plotkin AJ, Wade CE, Jenkins DH, Smith KA, Noe JC, Park MS, et al. A reduction in clot formation rate and strength assessed by thrombelastography is indicative of transfusion requirements in patients with penetrating injuries. J Trauma. 2008 Feb;64(2 Suppl):S64–8. doi: 10.1097/TA.0b013e318160772d. [DOI] [PubMed] [Google Scholar]
- 36.Schochl H, Frietsch T, Pavelka M, Jambor C. Hyperfibrinolysis after major trauma: differential diagnosis of lysis patterns and prognostic value of thrombelastometry. J Trauma. 2009 Jul;67(1):125–31. doi: 10.1097/TA.0b013e31818b2483. [DOI] [PubMed] [Google Scholar]
- 37.Brohi K, Cohen MJ, Ganter MT, Schultz MJ, Levi M, Mackersie RC, et al. Acute coagulopathy of trauma: hypoperfusion induces systemic anticoagulation and hyperfibrinolysis. J Trauma. 2008 May;64(5):1211–7. doi: 10.1097/TA.0b013e318169cd3c. discussion 7. [DOI] [PubMed] [Google Scholar]