Abstract
The rise of obesity in the United States over the past 25 years has resulted in an increase in the number of research studies published related to the causes, consequences, and possible solutions to the problem. Most would agree that obesity is a multi-dimensional problem that requires a range of solutions related to individual diet and activity, food and built environment, and public policy. Examination of complex relationships between food choice, time use patterns, sociodemographic characteristics and obesity has been limited by data availability and disciplinary focus. Using the theory of the production of health capital, this paper links empirical data from the Consumer Expenditure, Current Population, and American Time Use Surveys to provide estimates of the impacts of food expenditure and time use patterns on obesity in single female headed households of 31–50 years of age.
Introduction
Studies about obesity reveal a wide variety of disciplinary foci, from medicine to nutrition, and economics to transportation and public policy. Methods vary across disciplines, as does variable measurement. Hamersh (1) notes the problem of data availability. Sturm (2) and McKinnon et al. (3) identify problems with measuring the food and built environments and physical activity. In order to move the obesity research agenda forward, the academic community must recognize both the challenges and opportunities that exist when data are complex, measures differ across disciplinary lines, and no one dataset or methodology can capture all the variables that contribute to obesity (3). This study explores the possibility of linking three population-based nationally representative databases to better understand the impact that food patterns, time use, and demographic characteristics have on obesity, based on the concept that individuals produce health using available resources (4,5).
Nutritionists focus on relationships between intake of foods and obesity (6,7,8). Economists focus on expenditures on food and budget shares (9,10). Recently, nutrition scholars have recognized the importance of both household purchasing behaviors and the characterization of the achievement and maintenance of a healthy weight as “work” that must be “managed” (11). In the consumer economics field, the household production model has been a framework of choice for research (4) and has been expanded to include the production of health (5). However, studying the production of a healthy weight is still in the exploratory stage (1,12,13,14).
The number of eating occasions, including snacking, in addition to where people consume food, i.e., at home, in restaurants or at fast food establishments, influence obesity. That is partly due to an increase in the average portion sizes of snack foods, soft drinks and in all restaurant settings (15,16,17). Snacking impacts total daily caloric intake as people fail to compensate by eating less at subsequent meals (18).
A body of work related to time spent in meal production and eating is developing (1,19). While still largely anecdotal, there is some evidence that knowledge of cooking increases healthy food intake and the United States is a nation that cannot or does not cook (20). Research has also found that a decrease in the number of meals prepared “from scratch” increased the probability of being overweight in a national sample (12). But people perceive less time to cook (21,22).
Other time uses are linked to obesity. Time spent in front of a computer or television (screen time) as well as other forms of inactivity are detrimental to health (23,24). Americans fall short of meeting exercise guidelines, spending less than 20 min daily in exercise, sports, or recreation but over 2 hours watching television (25). Sleep (or lack thereof) may be connected to overweight (26).
Research links obesity with demographic characteristics including educational attainment, gender, race, and age (27,28,29,30). Other factors include attributes of the built environment. Research has linked walkability, urban location, and use of non-motorized transportation modes to decreased obesity (31,32).
The conceptual basis for this study is Grossman's (5) model of the demand for health capital, an extension of Becker's (4) theory of the allocation of time. The details are described elsewhere (12,13). Building stocks of health capital, one measure of which is a healthy weight, is a decision made at the household level. Individuals, given an initial stock of health, produce health rather than consume it from the market as they would in a traditional neoclassical demand model. The model allows the examination of the effects of time use, purchased inputs and household characteristics on the production of a healthy weight. Certain time uses result in energy output, e.g., physical activity. Other time uses result in less energy output, e.g., sedentary behaviors including screen time. Some time is combined with purchased inputs and results in energy input, e.g., cooking time and purchased food for consumption at home.
However, research on measuring food and physical activity environments is relatively recent, at an early stage of development, and few standard measures exist (3). Any conceptual model which attempts to incorporate multiple factors related to obesity becomes increasingly complex. We estimate a multivariate version of the health capital model that permits the testing of several hypotheses, Ceteris Paribus. H1 and H2 are derived from the literature, which has relied mostly on bivariate statistics to examine relationships between demographic variables and obesity. H3, H4, and H5 are formulated based on the energy balance equation (24).
H1: Demographic characteristics of lower income, lower education, rural location, and being of black or Hispanic ethnicity are associated with increased obesity;
H2: Food time use patterns that include more “cooking time” and “mindful eating” are associated with decreased obesity;
H3: Food patterns that include more fast and other food away from home are associated with increased obesity;
H4: Time use patterns that involve more sedentary behaviors are associated with increased obesity; and
H5: Time use patterns that involve more physically active behaviors are associated with decreased obesity.
Methods and Procedures
Necessary data include food expenditures, time use, demographic characteristics and measures of height and weight. No one nationally representative database contains all this information. Therefore, the Eating and Health Module of the American Time Use Survey (ATUS) is linked with individual data from the Current Population Survey and grouped data from the Consumer Expenditure Survey (CE). The CE has been available yearly since 1984 from the Bureau of Labor Statistics (http://www.bls.gov/cex/) and contains information neither about height nor weight. In the time diary portion of the ATUS (http://www.bls.gov/tus), respondents sequentially report activities they did between 4:00 on the day before the interview until 4:00 on the day of the interview. The ATUS Eating and Health Module provides height and weight information. Cross sectional data from 2006 to 2007 were pooled.
This analysis includes single female headed households of 31–50 years of age without a disability. Use of this subsample is based on a variety of disciplinary findings. The Food Guide Pyramid and the 2005 Dietary Guidelines for Americans (DGA) (33) make recommendations by gender and age: 18–30, 31–50, and individuals over the age of 50; our selection follows that categorization. People with disabilities were excluded to ensure that time use was dictated by personal choice and not physical limits. Underweight and pregnant women were excluded; underweight presents a distinct public health issue, and pregnant women may have a higher BMI without being overweight. Time use patterns differ across the life stage (34). Individuals with a BMI >50 were excluded, since morbid obesity presents additional and more serious health problems and does not parallel overweight or moderate obesity trends (35).
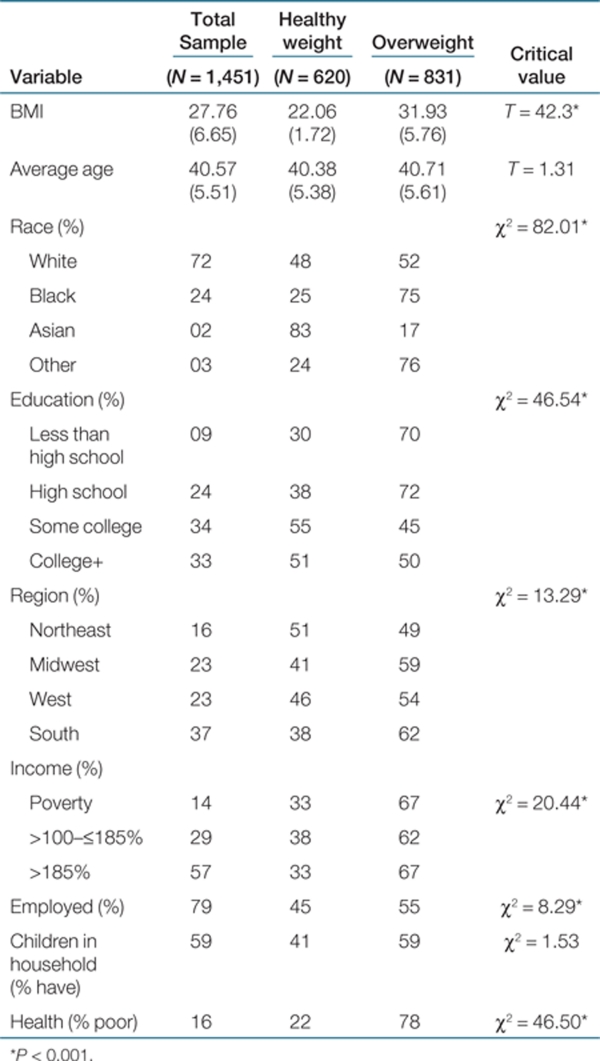
We reference both the Food Guide Pyramid and DGA to identify food patterns (33). We combined or renamed the CE broad food expenditure categories to correspond to the specific food groups identified in the DGA (33). A content analysis conducted by two registered dieticians recommended that expenditures be recoded as well as regrouped into categories that more closely mirror the DGA categorization. Average expenditures from the CE were assigned to individuals in the ATUS through a matching based on three demographic variables: gender, income, and family composition. These have all been linked as major predictors of both food expenditures and time use patterns in addition to being correlated to obesity (36). In addition, that combination of variables preserves the most variability within the expenditure data. Hundreds of matches were made. An example of the assignment methodology is as follows: according to the CE, in 2007, the average weekly expenditure on chicken for an adult single female headed household without children earning less than $10,000 per year was $1.63. Each 2007 ATUS respondent who was a single female head of household without children who earned less than $10,000 per year was then assigned a weekly chicken expenditure of $1.63. Similarly, the average value for all other food groups was assigned to each category of income and household composition. This matching method preserves individual data for demographic and time use variables in the ATUS data and assigns grouped data for food expenditures in the CE. Table 1 presents characteristics of the 1,451 respondents in the linked sample and each healthy and overweight cohort. Weight status differs significantly across race, education, region of residence, income, employment status, and self-reported health status. These relationships are consistent with other research (27,28,29,30).
Table 1. Demographic characteristics of the sample.
Next, expenditure shares for 28 food categories were calculated. Initially, only the major DGA categories were used. These included combined categories of animal and non-animal protein, dairy, fruits, vegetables, carbohydrate, added fats, added sugars, and included the additional categories of beverages, miscellaneous foods, fast food, and full service food away from home. Early analysis revealed that regardless of income level and family composition, the share of expenditures did not differ significantly across demographic groups. Therefore, DGA categories were further disaggregated. Using the expertise of dietitians, the DGA categories, and available expenditures in the CE data resulted in expenditure shares that were diverse enough to show variation across respondents, yet aggregated enough to allow interpretation within the DGA guidelines.
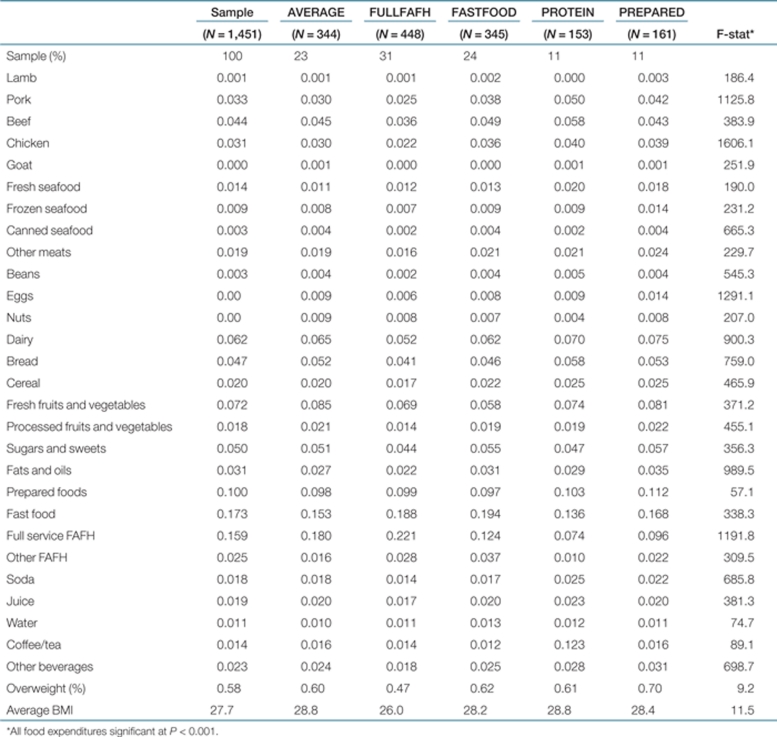
The method of two-step cluster analysis using the log-likelihood distance measure and Schwarz's Bayesian Criterion in the Statistical Package for Social Sciences (SPSS 15.0; SPSS, Chicago, IL) was used to identify food patterns. Cluster analysis is typically sensitive to the variables included in the clustering. In the case of food, all 30 of the DGA food groups were included. There were no additions or deletions of variables that could influence the cluster results. Cluster analysis has been used across disciplines to define distinct dietary patterns using both food intake and expenditure data (8,37,38). When the relationships among several variables are unknown and several variables may be considered dependent, cluster analysis can give an indication of complex patterns within a dataset, not easily accomplished with economic, sociological, or even social-ecological models, which tend to lead to regression type approaches to empirical analysis (14,39,40). Five patterns clusters emerged; about average across food categories (AVERAGE; 23 percent), higher full-service food away from home (FULLFAFH; 31 percent), higher fast food away from home (FASTFOOD; 24 percent), higher animal protein and beverages at home (PROTEIN; 11 percent), and higher processed and prepared foods at home (PREPARED; 11 percent). Table 2 describes these clusters. The AVERAGE group has about average expenditure shares when compared with the total sample. They do have higher shares for fresh fruits and vegetables and full service food away from home, and a lower fast food share. The FULLFAFH cluster has the lowest shares allocated to sugars and sweets, fats and oils, soda and juice. The PREPARED cluster appears to take time saving routes to food purchasing. This cluster has the highest shares for prepared foods, other meats (includes cold cuts) and eggs (quick cooking protein), and the largest shares for sugars/sweets and fats/oils. The PROTEIN cluster spends almost one-fifth of its food budget on animal protein and five percent on soda and juice. The CE does not provide a breakdown on the type of beverage beyond these, nor whether the beverages are sugar sweetened or low calorie. The PROTEIN cluster has among the lowest shares for sugars/sweets. The PREPARED food cluster has the highest proportion of overweight respondents (70 percent), followed by FASTFOOD (62 percent), PROTEIN (61 percent), AVERAGE (60 percent) and FULLFAFH (47 percent). The percentage of overweight respondents differs significantly across clusters, as do expenditure shares on individual foods. On average, all clusters are classified as overweight.
Table 2. Expenditure shares for food by food pattern cluster.
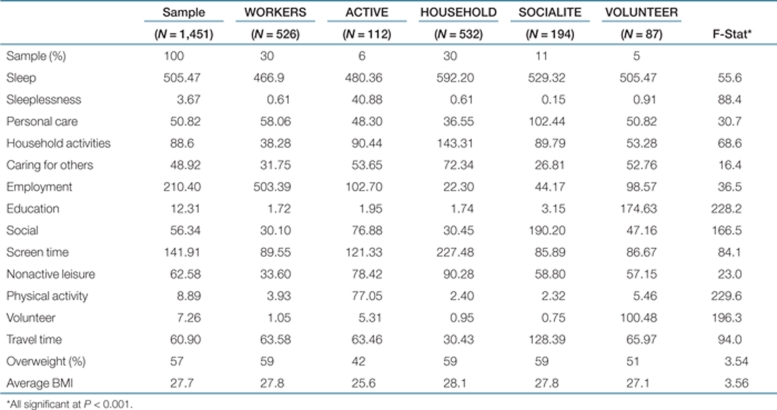
Next, time use patterns were examined. Household work, personal care, caring for others, work hours, education hours, volunteer hours, sleep, sleeplessness, physical activity, commuting time, socializing, non-active leisure, and screen time were included in a cluster analysis, as described above. As with the food groups, there were no additions or deletions of time use in the cluster analysis that could lead to sensitivity in the emerging clusters. Table 3 describes the five clusters that emerged. Paid workers (WORKERS; 30 percent) spent over 8 h per day in paid employment. The most physically active cluster (ACTIVE; 6 percent) spent over 1 h per day in physical activity, had the highest levels of sleeplessness and the lowest percentage of overweight respondents (42 percent). Respondents who spent the most time in household activities and caring for others, more than 3 h per day (HHWORK; 30 percent), also reported getting the most sleep (~6 h), screen time, and time in non-active leisure (more than 5 h). SOCIALITE (11 percent) spent the most time socializing (more than 3 hours) and reported the most time in personal care activities. VOLUNTEERS (5 percent) spent the most time in non-paid work, both in volunteering (more than 1.5 h) and pursuing education (almost 3 h). Time uses differ significantly across clusters as do the percentages of overweight respondents. On average, all clusters are overweight.
Table 3. Minutes of time use for each time use cluster.
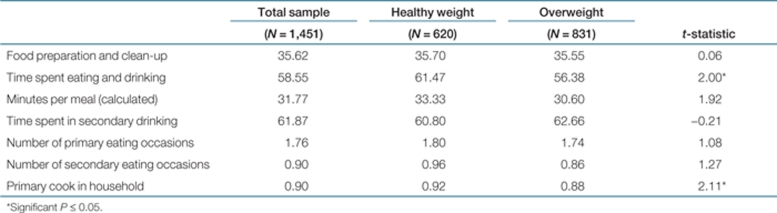
Standard t-tests were run to examine differences in food-related time uses and behaviors between healthy weight and overweight cohorts. Data included: number of primary and secondary eating occasions, time spent in secondary drinking (other than water), the primary cook in the household, and time spent in meal preparation and clean-up. Significant differences were found between healthy weight and overweight individuals in time spent eating and drinking, total minutes per meal and whether the respondent is the major cook in the household. Healthy weight individuals report spending more time eating and drinking and a larger percentage are the major cook for the household. Table 4 presents these results.
Table 4. Food-related behaviors.
Bivariate results presented in Tables 1–4 show that the percentage of overweight respondents differs significantly across demographics and eating and time use patterns, with fewer differences in time use related to eating and drinking. Next, we regressed demographic, eating, and time use pattern variables on both the probability of being overweight and on BMI. The method of truncated regression is used. A variation of the Tobit model, the probability of a non-limit outcome is determined separately from the level of the non-limit outcome. When applied to a model of overweight, the estimation of BMI is determined separately for healthy weight and overweight individuals, given the probability of being overweight. Truncated regression allows the sign of individual coefficients to differ in the estimation of the probabilities compared to the degree of overweight, which is not possible in the Tobit regression model (for details of the statistical approach, see refs. 41,42).
Three models are estimated. The dependent variables are the probability of being overweight (BMI ≥25), BMI for BMI ≥25 and BMI for BMI >18 and <25. Results of the estimation includes the probability of crossing the overweight threshold and the effect of the independent variables on BMI for both healthy weight and overweight individuals. Because the focus of this paper is on overweight, we omit the healthy weight results. Independent variables include the food pattern and time use clusters. Because these are 0/1 “dummy variables,” we leave out the HHWORK time use and AVERAGE food pattern cluster as the reference group. While any group can be the reference group, we chose to use the food pattern group closest to the sample average and the time use pattern group with the most time in spent in the household. There was no “average” time use cluster. The HHWORK cluster represented 30 percent of the total sample and had a percentage of overweight individuals that was closest to the national average. We also included the individual food-related time use variables: number of primary eating and drinking occasions, number of secondary eating occasions, time spent in secondary drinking, time spent in food preparation and clean-up, time spent in primary eating and drinking, minutes per meal (every additional 10 min per primary eating and drinking occasion), whether the respondent is the major cook in the household and an interaction term between major cook and cooking/clean-up time. The demographic variables age, race, education, income, presence of children, region of residence, living in a metropolitan area, and self-reported poor health status are also included.
Results
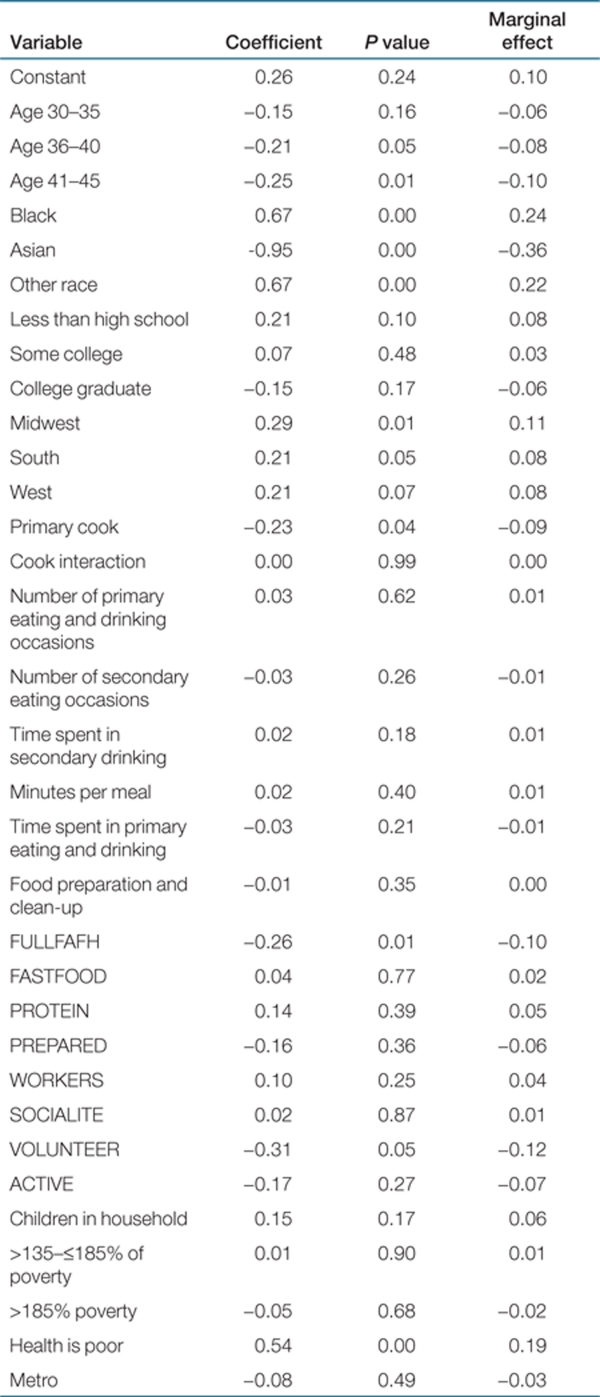
Tables 5 and 6 present regression results. The last column of Table 5 presents the marginal effect on the probability of being overweight. Each marginal effect is interpreted, “holding all the other included variables constant, the effect of (independent variable x) increases/decreases the probability of being overweight by…” For example, holding all other included variables constant, the effect of being Black on the sample as a whole increases the probability of being overweight by 24 percent. The model predicts the probability of being overweight correctly in 80 percent of the cases. For individuals in the >35– ≤40 age group and the >40– ≤45 age group, the probabilities of being overweight compared to those age 50 and older are 0.08 and 0.09 probability points lower. Even in this limited age cohort, the probability of being overweight increases with age. Being black or of a race other than white increases the probability of being overweight by 0.24 and 0.22 probability points, respectively. Being Asian decreases the probability of overweight by 0.36 points. Compared to those living in the Northeast, the Midwestern, Southern and Western residents all have higher probabilities of being overweight. Those in poor health have a probability of being overweight 0.19 points higher. Education (reference group is high school graduate) and income (reference group is <135 percent of poverty level), are insignificant. Ceteris Paribus, income has no effect on the probability of being overweight.
Table 5. Probit estimates of the probability of overweight (N = 831).
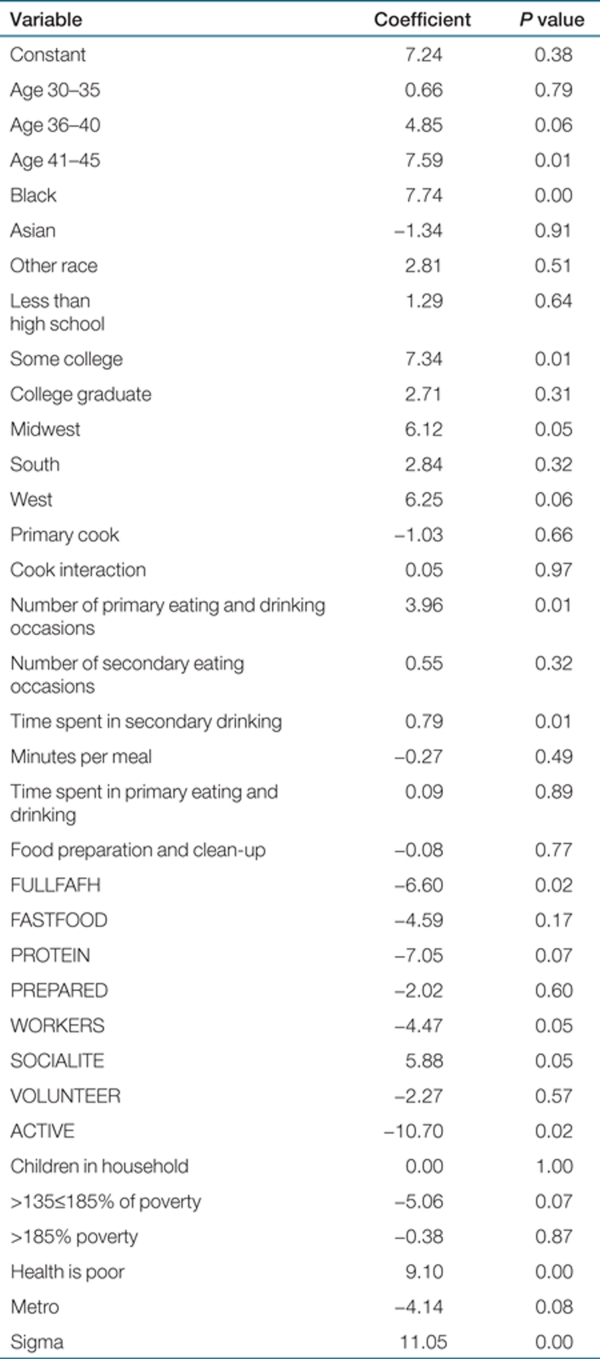
Table 6. Truncated regression: estimates for overweight level of BMI (≥25) (N = 831).
The probability of the full service restaurant pattern (FULLFAFH) cluster being overweight that is 0.10 points lower than the AVERAGE group. The time use cluster that spends more time in education and volunteer activities (VOLUNTEER) has a probability of being overweight that is 0.12 points lower compared with the reference HHWORK group. And, while, individual eating behaviors are not significant in predicting the probability of being overweight, their influence becomes apparent when the level of BMI is predicted, given an individual has crossed the overweight threshold, as seen below.
Table 6 presents results of the truncated regression estimates that predict BMI for overweight individuals. The coefficients are interpreted, “what is the incremental effect on BMI of each individual independent variable, given an individual has a BMI greater than 25 and less than 50?” Demographic variables and time use and food patterns significantly impact BMI. While the probability estimates showed that individuals in the >35– ≤40 and >40– ≤45 age groups had a lower probability of being overweight compared to those of >45– ≤50 years of age, if overweight, their BMI is predicted to be 4.85 and 7.59 points higher than the oldest group. While all of the included racial groups, compared to whites, were significant in predicting the probability of overweight, only blacks have a significantly higher BMI once they are overweight, increasing BMI by 7.74 points. Education was insignificant in predicting the probability of being overweight. If an individual is overweight, individuals with some college education have a predicted BMI 7.34 points higher compared to having completed high school. Poor health was significant in predicting the probability of being overweight. It increases BMI 9.10 points for an overweight individual. While income was insignificant in predicting the probability of overweight, individuals with incomes >135% and ≤185% of the federal poverty level had a predicted BMI 5.06 points lower than individuals earning incomes less than 135% of poverty.
Individual time uses related to food were insignificant in predicting the probability of being overweight. However, once an individual crosses the overweight threshold, these time uses are significant in predicting BMI. Each additional reported primary eating occasion increases BMI by 3.96 points. For every additional 10 min spent in secondary drinking, predicted BMI increases by 0.55 points. Interpreting the effects of being the primary cook and time spent in food preparation and clean-up is more complicated because of the included interaction effect. Isolating the effect of being the primary cook is calculated as: −1.03 primary cook + (0.05 primary cook × food preparation and clean-up) ÷ 0.08 food preparation and clean-up.
Being the primary cook decreases BMI 1.72 points for overweight individuals. Isolating the effect of food preparation and clean-up time reveals that an additional 10 min spent cooking and cleaning-up decreases BMI by 0.13 points.
Two food pattern clusters are significant in predicting BMI for overweight individuals. Those in the full service food away from home cluster (FULLFAFH) have a predicted BMI 6.60 points lower than those in the AVERAGE cluster. Individuals in the higher protein (PROTEIN) at home cluster have a predicted BMI 7.05 points lower compared with the AVERAGE cluster.
Three time use clusters are significant. Given an individual is overweight, those classified as having the most time spent in social activities (SOCIALIATE), have a predicted BMI 5.88 points higher. Those classified as spending most time in volunteer activities (VOLUNTEER) have a predicted BMI 2.27 points lower compared to the HHWORK cluster. And, the ACTIVE cluster has a predicted BMI 10.70 points lower compared to the HHWORK cluster.
Discussion
This research adds to the literature in several ways. Three population-based data sets are linked to obtain a richer set of variables for which to analyze the factors that contribute to the probability of being overweight and BMI for both overweight and healthy weight individuals. This study shows the importance of isolating the effect of these factors on the probability of being overweight separate from their effects on BMI once the individual becomes overweight.
For single headed female households between the ages of 31and 50, variables that impact the probability of being overweight and variables that predict BMI for overweight individuals differ in significance, magnitude, and in some cases direction of effect. Lifestyle pattern clusters of time use and food patterns impact both the probability of being overweight and BMI. The impact of individual food-related time uses shows that knowledge of cooking and eating patterns affect the BMI of overweight individuals. Increases in cooking time are associated with a decrease in BMI.
Previous literature links demographic characteristics and obesity. When time use and eating pattern clusters are accounted for, race and region of residence continue to be significant predictors of the probability of being overweight. People residing in the northeast have a lower probability of being overweight and given they are overweight have a lower BMI, except when compared to people living in the south. The effect of income is not found to be as robust as other research but this research controls for other variables (6,10,36). In our limited age cohort, being older within the age range increases BMI only for already overweight individuals. These results stress the importance of maintaining a healthy weight in early adulthood. H1 is partially supported, and the effect of demographic variables depends on whether the dependent variable is the prediction of the probability of overweight or the prediction of BMI once the overweight threshold is passed.
Results also show that for overweight individuals, more primary eating and drinking occasions and time spent in secondary drinking increase BMI. While results for the truncated regression to estimate BMI for healthy weight individuals are not presented in this paper, more drinking occasions are associated with a decrease in BMI and number of primary eating occasions has no impact on BMI. This study is one of the first, in a multivariate analysis, to show that cooking at home has a mitigating effect on BMI for overweight individuals. Results corroborate the idea that a resurgence of home economics type classes within school curriculum and community cooking skills interventions might serve a useful purpose (43).
Our results also show that a lifestyle that includes larger budget shares allocated to full-service restaurants (FULLFAFH) is associated with a lower probability of being overweight and a lower BMI for the overweight sample compared to the AVERAGE cluster. Looking across expenditure shares in Table 2, the AVERAGE cluster spends “about” the average on most food categories, including food away from home, while the FULLFAFH group spends less on several at home categories, including protein (looking across meats, eggs, and nuts), dairy, breads, cereals, sugars and sweets, fats and oils, and soda and juice. Further research is necessary to investigate whether those who spend a larger share of their budget on full-service food away from home substitute more expensive, lower in overall calorie foods for food at home and have a lower overall calorie intake compared to the AVERAGE cluster which has average shares on most food categories and higher than average shares on full-service food away from home. The higher protein (PROTEIN) overweight cluster also has significantly lower BMIs compared to the AVERAGE cluster. Looking at other shares in the PROTEIN group reveals that this cluster has the lowest expenditure shares for both fast and full-service food away from home. Further research is needed to investigate whether the FULLFAFH cluster substitutes restaurant meals for food at home and the PROTEIN cluster substitutes food at home for restaurant meals, while the AVERAGE cluster eats both at and away from home. For the overweight sample, being in the fast food cluster (FASTFOOD) has no effect on BMI. Therefore, this study does not show that being classified in a cluster with higher than average food away from home shares is associated with a higher probability of being overweight or a higher BMI if overweight, as has been suggested, though not overwhelmingly supported, in some of the literature (12,15,44,45,46). It appears that food away from home must be interpreted within overall dietary patterns. H2 cannot be supported by this analysis.
This study also shows that certain time use patterns are associated with being overweight and BMI level. Belonging to the cluster that spent the most time in educational and volunteer activities decreased the probability of being overweight by 0.12 probability points, but had no significant effect on BMI for overweight individuals. On the other hand, while spending more time in the labor market (WORKERS), in physical activity (ACTIVES), or socializing (SOCIALITE) did not significantly impact the probability of being overweight, individuals in these clusters had predicted BMIs 4.47 lower, 10.70 lower, and 5.88 points higher compared to the HHWORK cluster. The SOCIALITE clusters had the lowest levels of physical activity of all clusters, and spent the most time traveling and in personal care activities. While total calorie expenditure for travel can vary if an individual actively commutes either by walking or by using a bicycle, research shows less than 4 percent of the US population uses these transportation modes (47). The SOCIALITE cluster is sedentary compared to the other clusters. The ACTIVE group has the lowest predicted BMI in the overweight group. H3 and H4, both having to do with energy expenditure, are supported for overweight persons.
Overall, considering time use and food expenditure patterns in the context of a household health production model adds to the understanding of the impact of time use and food expenditure patterns, in addition to the importance of demographic characteristics on obesity. The results provide insight into the complex array of factors that are associated with obesity and points to both target groups and obesity prevention programs. For example, blacks and minorities in the “other” group (including Hispanics) remain a priority target group for obesity prevention. Policies in the workplace should encourage both places and time for physical activity. Alternatives to screen time and non-active leisure alternatives must continue to be developed and marketed, especially to people who spend much of their time at home caring for others. The obesity epidemic is complex; a combination of variables jointly contribute to the probability of being overweight and to BMI.
There are limitations to this study. First, we have tested our approach on one cohort of individuals: single female headed households aged 31–50 years. The analysis should be replicated on other cohorts. Second, only two of the datasets used are linked by individual. More complete, nationally represented datasets are needed. Third, food expenditures do not mean the same thing as food intake. Future research should investigate the possibility of linking the ATUS with the National Health and Examination Survey. However, 2007–2008 National Health and Examination Survey data are still not fully available. Fourth, in order to handle the complexity of the data, many of the included variables are proxy measures. For example, the composite SOCIALITE cluster gives an indication of a variety of sedentary lifestyle behaviors and that individuals in this cluster who are already overweight may be engaging in more energy intake and less energy output when participating in their social activities. Future studies should build on this research, and investigate more complexities in lifestyle patterns, including examining interaction effects between time use and food expenditure patterns.
When obesity is viewed within a model of health production, the results corroborate what has been found in the hundreds of focused studies related to the causes of obesity, and add to the literature by identifying the impact of individual variables holding the effect of others constant. Such comprehensive analysis should be replicated using other demographic profiles, including family types, ages, and gender of household head. Other datasets should be explored, and interactions between food and time use patterns should be explored. Overall, this study motivates further studies at both the focused and complex levels.
The authors declared no conflict of interest.
REFERENCES
- Hamermesh D. Time to eat: household production under increasing income inequality. Am J Agric Econ. 2001;89:852–853. [Google Scholar]
- Sturm R. Economics and physical activity: a research agenda. Am J Prev Med. 2005;28:141–149. doi: 10.1016/j.amepre.2004.10.021. [DOI] [PubMed] [Google Scholar]
- McKinnon RA, Reedy J, Handy SL, Rodgers AB. Measuring the food and physical activity environments: shaping the research agenda. Am J Prev Med. 2009;36:S81–S85. doi: 10.1016/j.amepre.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Becker GS. A theory of the allocation of time. Econ J. 1965;75:493–517. [Google Scholar]
- Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972;80:223–255. [Google Scholar]
- Deshmukh-Taskar P, Nicklas TA, Yang SJ, Berenson GS. Does food group consumption vary by differences in socioeconomic, demographic, and lifestyle factors in young adults? The Bogalusa Heart Study. J Am Diet Assoc. 2007;107:223–234. doi: 10.1016/j.jada.2006.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Hoelscher D. Increasing fruit and vegetable intake by changing environments, policy and pricing: restaurant-based research, strategies, and recommendations. Prev Med. 2004;39 Suppl 2:88–93. doi: 10.1016/j.ypmed.2004.03.002. [DOI] [PubMed] [Google Scholar]
- James DC. Cluster analysis defines distinct dietary patterns for African-American men and women. J Am Diet Assoc. 2009;109:255–262. doi: 10.1016/j.jada.2008.10.052. [DOI] [PubMed] [Google Scholar]
- Smallwood DM, Blaylock JR, Lutz S, Blisand N. Americans spending a smaller share of income on food. Food Rev. 1996;18:16–19. [Google Scholar]
- Lutz SM, Smallwood DM, Blaylock JR. Limited financial resources constrain food choices. Food Rev. 1995;18:13–17. [Google Scholar]
- Welch N, Hunter W, Butera K.et al. Women's work. Maintaining a healthy body weight Appetite 2009539–15. [DOI] [PubMed] [Google Scholar]
- Kolodinsky J, DeSisto T.A household production approach to overweight: A model and preliminary estimatesIn: Nitsch D (ed). Consumer Interests Annual American Council on Consumer Interests 53rd Annual Conference: St. Louis, MO,200753–54. [Google Scholar]
- Kolodinsky J, Goldstein A.Time use and food intake patterns: More insight into energy balance Proceedings CD-ROM of the 1st Joint EAAE/AAEA Seminar: The Economics of Food, Food Choice and Health European Association of Agricultural Economics: Freising, Germany; 2010. pp 8B-1. [Google Scholar]
- Lakdawalla D, Philipson T. Labor supply and weight. J Hum Resour. 2007;42:85–166. [Google Scholar]
- Bowman SA, Vinyard BT. Fast food consumption of U.S. adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23:163–168. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- Diliberti N, Bordi PL, Conklin MT, Roe LS, Rolls BJ. Increased portion size leads to increased energy intake in a restaurant meal. Obes Res. 2004;12:562–568. doi: 10.1038/oby.2004.64. [DOI] [PubMed] [Google Scholar]
- Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health. 2002;92:246–249. doi: 10.2105/ajph.92.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral TV, Rolls BJ. Energy density and portion size: their independent and combined effects on energy intake. Physiol Behav. 2004;82:131–138. doi: 10.1016/j.physbeh.2004.04.063. [DOI] [PubMed] [Google Scholar]
- Hamrick K, Hopkins D, McClelland K.How much time do Americans spend eating? Amber Waves: The Economics of Food, Farming, Natural Resources, and Rural America 2008;6 . < http://www.ers.usda.gov/AmberWaves/June08/DataFeature/ >. Accessed 30 March 2010. [Google Scholar]
- Brown BJ, Hermann JR. Cooking classes increase fruit and vegetable intake and food safety behaviors in youth and adults. J Nutr Educ Behav. 2005;37:104–105. doi: 10.1016/s1499-4046(06)60027-4. [DOI] [PubMed] [Google Scholar]
- Jabs J, Devine CM. Time scarcity and food choices: an overview. Appetite. 2006;47:196–204. doi: 10.1016/j.appet.2006.02.014. [DOI] [PubMed] [Google Scholar]
- Mancino L, Newman C.Who has time to cook?: How family resources influence food preparation United States Department of Agriculture: Washington, DC; < http://ddr.nal.usda.gov/ dspace/bitstream/10113/19386/1/CAT30995251.pdf > ( 2007 [Google Scholar]
- Hancox RJ, Milne BJ, Poulton R. Association between child and adolescent television viewing and adult health: a longitudinal birth cohort study. Lancet. 2004;364:257–262. doi: 10.1016/S0140-6736(04)16675-0. [DOI] [PubMed] [Google Scholar]
- Hill JO, Peters JC, Wyatt HR. Using the energy gap to address obesity: a commentary. J Am Diet Assoc. 2009;109:1848–1853. doi: 10.1016/j.jada.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics Leisure time on an average day. American Time Use Survey < http://www.bls.gov/tus/charts/leisure.htm > ( 2008. Accessed 7 June 2009.
- Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Bowman BA, Ford ES.et al. The continuing epidemics of obesity and diabetes in the United States J Am Diet Assoc 20012861195–1200. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR.et al. Prevalence of overweight and obesity in the United States, 1999-2004 J Am Diet Assoc 20062951549–1555. [DOI] [PubMed] [Google Scholar]
- Parker S, Keim KS. Emic perspectives of body weight in overweight and obese white women with limited income. J Nutr Educ Behav. 2004;36:282–289. doi: 10.1016/s1499-4046(06)60396-5. [DOI] [PubMed] [Google Scholar]
- Robinson WR, Gordon-Larsen P, Kaufman JS, Suchindran CM, Stevens J. The female-male disparity in obesity prevalence among black American young adults: contributions of sociodemographic characteristics of the childhood family. Am J Clin Nutr. 2009;89:1204–1212. doi: 10.3945/ajcn.2007.25751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot. 2003;18:47–57. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. 2004;27:87–96. doi: 10.1016/j.amepre.2004.04.011. [DOI] [PubMed] [Google Scholar]
- US Department of Agriculture Dietary Guidelines for Americans Department of Health and Human Services and the Department of Agriculture: Washington, DC; < http://www.health.gov/ dietaryguidelines/dga2005/document/html/chapter3.htm > ( 2005 [Google Scholar]
- Monna B, Gauthier AH. A review of the literature on the social and economic determinants of parental time. J Fam Econ Issues. 2008;29:634–653. [Google Scholar]
- Sturm R. Increases in morbid obesity in the USA: 2000-2005. Public Health. 2007;121:492–496. doi: 10.1016/j.puhe.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- Fan JX, Brown BB, Kowaleski-Jones L, Smith KR. Household food expenditure patterns: a cluster analysis. Monthly Lab Rev. 2007;130:38–51. [Google Scholar]
- Wirfält AK, Jeffery RW. Using cluster analysis to examine dietary patterns: nutrient intakes, gender, and weight status differ across food pattern clusters. J Am Diet Assoc. 1997;97:272–279. doi: 10.1016/s0002-8223(97)00071-0. [DOI] [PubMed] [Google Scholar]
- Moussavi N, Gavino V, Receveur O. Is obesity related to the type of dietary fatty acids? An ecological study. Public Health Nutr. 2008;11:1149–1155. doi: 10.1017/S1368980007001541. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Kelly S, Brunner E, Lobstein T, Wilkinson RG. Wider income gaps, wider waistbands? An ecological study of obesity and income inequality. J Epidemiol Community Health. 2005;59:670–674. doi: 10.1136/jech.2004.028795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cragg JG. Some statistical models for limited dependent variables with application to the demand for durable goods. Econometrica. 1971;39:829–844. [Google Scholar]
- Greene W.Limdep User's Manual and Reference Guide7th edn. Econometric Software: Bellport, NY; 1995 [Google Scholar]
- Lichtenstein AH, Ludwig DS. Bring back home economics education. J Am Diet Assoc. 2010;303:1857–1858. doi: 10.1001/jama.2010.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffey KJ, Gordon-Larsen P, Jacobs DR, Jr, Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr. 2007;85:201–208. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- Pereira MA, Kartashov AI, Ebbeling CB.et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis Lancet 200536536–42. [DOI] [PubMed] [Google Scholar]
- Prentice AM, Jebb SA. Fast foods, energy density and obesity: a possible mechanistic link. Obes Rev. 2003;4:187–194. doi: 10.1046/j.1467-789x.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- US Census Bureau Commuting Characteristics by Sex US Census Bureau American FactFinder; < http://factfinder.census.gov/servlet/ STTable?_bm=y&-geo_id=01000US&-qr_name=ACS_2008_3YR_G00_S0801&-ds_name= ACS_2008_3YR_G00_&-_lang=en&-redoLog=false&-format=&-CONTEXT=st > ( 2009. Accessed 10 September 2010. [Google Scholar]