1. Introduction
Primary care physicians are expected to form partnerships with patients, address a wide range of acute and chronic biomedical and psychosocial issues, provide preventive care, coordinate care with specialists, and ensure informed decision-making that respects patients’ needs and preferences (Fiscella and Epstein 2008). In the course of a typical workday, an internist in private practice sees 20–25 patients (Murray, Davies et al. 2007) and it is clear from anecdotal and research reports that doctors do not get done all they would like let alone what they are instructed to do by standard-setting bodies. In addition to pre-scheduled visits which can still present unpredictable demands on time, same-day visits must also be accommodated (Murray and Tantau 2000) along with phone calls and emails from patients, other physicians, and health plans. Record keeping and other administrative and office management tasks add yet another layer of demand on doctor’s time. Doctors feel rushed and overwhelmed. They are growing more frustrated with “productivity standards” imposed by managed care organizations which translate to volume targets that must be met in order to reach revenue targets (Lin, Albertson et al. 2001; Virtanen, Oksanen et al. 2007).
This paper studies how physicians allocate their clinic time in caring for patients during office visits. We formulate and test two alternative hypotheses. The first hypothesis is based on the premise that with time so scarce, physicians have powerful incentives to allocate it efficiently. Our simple model of efficient time allocation implies that the physician equalizes the marginal value of time across patients. The second, alternative hypothesis states that physicians allocate the same time to each patient, regardless of how much the patient benefits from the time at the margin. For our empirical work, we examine the presence of a sharply increasing subjective shadow price of time around the “target” time.
Our data are videotaped encounters between primary care physicians in the U.S. and their elderly patients supplemented by survey of participating patients and physicians. Obviously, physicians do not spend exactly the same amount of time per patient, so the strict version of the alternative hypothesis does not hold. However, we find evidence of a rapidly increasing shadow price of time around a target, consistent with the alternative hypothesis and inconsistent with the “efficient” time allocation hypothesis.
Several studies in the U.S. have examined how much time physicians spend with patients, reporting an average of around 16–18 minutes per visit. Mechanic and colleagues (2001) analyzed data from the National Ambulatory Medical Care Survey (NAMCS) and the American Medical Association’s Socioeconomic Monitoring System (SMS) to examine the trends in visit lengths from 1989 through 1998, a period when managed care expanded rapidly. In the NAMCS, the duration of visit is reported by the physician or a member of the physician’s staff. The SMS-derived average visit duration was obtained by dividing the average number of hours the physician reported spending with patients in his or her office each week by the average number of patients the physician reported seeing per week. The average duration of an office visit was 16.3 minutes according to NAMCS and 20.4 minutes according to SMS in 1989. Surprisingly, average visit duration trended upward over the next ten years.1 Glied and Zivin (2002) also used NAMCS data (from 1993 to 1996) to study visit duration by insurance status (FFS, HMO, Medicare, Medicaid). Although mean visit times differed by payer source (FFS 18.3 minutes, HMO 17.0, Medicaid 16.1, and Medicare 18.5), most of this variation was due to the different doctors seen by patient with the different payers. Within a practice, average visit times were similar across payers, a counterintuitive finding if some payers are more profitable than others. Glied and Zivin (2002) argued that a fixed cost could account for this result, but the finding is also consistent with physicians setting a practice-wide rule on the basis of the overall payer mix. These papers and our own prior work (Tai-Seale, McGuire et al. 2007) find that patient factors, such as age or health status, only have very modest influence on length of time in a visit in comparison to the greater impact of organizational settings and financial incentives. The existing literature is largely descriptive, however, and has not attempted, as far as we know, to test explicit hypotheses about how doctors decide about visit time allocation.
A finding from Tai-Seale, McGuire et al. (2007) stimulated our interest in the subject of the current paper. The 2007 paper structured physician and patient talk time into “topics” pertaining to discrete issues addressed during a visit. A visit then consists of a sequence of topics to which time and effort are allocated. We found that factors that increased topic length generally did not increase visit length. For example, if a “major topic” (as we defined it in the paper) was concerned with a mental health issue as opposed to a general medical topic, the length of time talking about the topic was 37% longer. The total length of the visit was, however, not affected by this longer topic. This is curious since total time for a visit is just the sum of time spent on topics. If total visit time is unaffected, it must be that the physician cuts back on time available for other topics within the visit in response to a time-intensive mental health issue, as opposed to spreading the extra time needed over all patients seen during the day. As patients usually have multiple issues that they would discuss with their physicians, how time is allocated within the visit, what topics get discussed and how much time they receive, can impact the patients’ experience with care, their health outcomes, and their subsequent use of additional services. We examine the decision to end a visit and the factors that influence that decision. In particular, we look at the relationship between elapsed time during a visit and the decision to end.
2. The Decision to End a Visit
We assume the physician, not the patient, ends the visit.2 We make use of the concept of a topic to describe what happens during a visit. A visit ends when the physician decides discussion on the current topic is over, and no more topics will be admitted. Conversely, a visit continues after the current topic if the doctor allows the patient to raise a new topic to be discussed. In general terms, we regard the physician as making the decision about allowing a new topic on the basis of expected benefits and costs, where benefits are how much the physician expects to be able to help the patient regarding the new topic and costs are the subjective costs of the time involved. We assume that physician revenue (and profit) are secondary considerations (and can be ignored) in the decision about the marginal topic within an office visit. Neither the visits nor the topics we consider involve procedures that generate extra payment.3 We return to the issue of revenue incentives and consequences associated with changing rules for time allocation in the Discussion section below.
We posit that the physician treats a given number of patients during a work day. Patients are scheduled such that the physician can always move to the next patient without delay. Patients’ medical problems are referred to as “topics.” A topic might be hip pain, or trouble with sleeping, or questions about medications. Assume for purposes of this discussion that each topic takes the same fixed amount of time, say two minutes, for the physician to handle.4 Although each topic takes the same amount of time, the value (benefit) of the physician dealing with each topic varies according to the nature of the topic and characteristics of the patient. Topics are more or less serious, and the physician may have more or less to contribute to patient welfare depending on the problem and the patient’s situation. The physician makes a series of sequential decisions during visit about whether to bring it to an end.
2.1 Expected value of a new topic
The expected value of a new topic is affected by patient factors, such as the health state of the patient, the nature of the patient’s medical conditions, how long it has been since the physician has seen the patient, how well the physician and patient communicate with each other, and what has already been discussed in the visit. Some of these factors the physician might know at the beginning of the visit (e.g., the health care history of the patient), but some information about the current health status of the patient will only emerge during the visit. The expectation the physician has about the value of an additional topic is thus conditioned on characteristics of the patient, as well as the nature of the medical problems in all of the topics discussed up to the current topic.
Suppose a physician is considering whether to admit a new topic after t topics have already been discussed. When deciding about whether to admit topic t+1 the physician knows the characteristics of the patient and the information contained in topics 1 through t. The expected value of admitting topic t+1, V̂t+1, is determined by physician’s expectation on the benefit of topic t+1 given what she already know about the patient and the prior topics 1 to t.
A critical issue for both theory and empirical work around the decision to close a visit is the order in which topics are raised during a visit. Physicians very often initiate visits with an open-ended question, some version of, “What brings you here today?” inviting the patient to initiate the first, and, at least in the patient’s eyes, one of the major topics in the visit.5 Following introduction of the one or more topics the patient regards to be important, clinical logic may set the next topic. For example, discussion of the topic of movement to a nursing home may follow discussion of complications due to change of medications associated with the move. Most elderly patients have a range of health problems that could be covered during a visit. Our viewing of the videotapes leads us to question whether patients and physicians order topics according to severity. A “non-serious” topic is often introduced early in a visit (by the physician as well as the patient) to establish rapport. In one visit, an extensive discussion about depression and suicide ideation (2nd topic) was carried out only after a discussion of acute bronchitis (1st topic). Physician folklore points to the hand-on-the-door knob ploy: “by the way, doctor, my chest has been hurting lately.” Patients may avoid talking about uncomfortable subjects until a visit is almost over, or, even behave strategically and grab extra time by saving the most severe issue for last.
We are most interested in the order of topics in terms of “seriousness,” or, in terms of our model, of the doctor’s assessment of the benefits of spending time on the topic. One polar case is that potential topics are ranked by importance and the most important topics are covered first. We consider V̂t+1 in terms of the physician’s belief about the benefits to the patient for the next topic, and while the benefit a physician provides to a patient on a topic probably contains a substantial stochastic component, an expected benefit function might have a smooth downward slope. Alternatively, the ordering of topics in terms of importance might be random. The downward-sloping expected benefit function actually presents more of a challenge when it comes to the empirical work, since a topic occurring later might be more likely to be last if it is less serious as well as if time has elapsed. If topics are “random” in terms of seriousness, there would be no expected correlation of unobserved indicators of severity with time elapsed. We will continue with our theoretical discussion as if physician’s expected benefit function declines with more topics. In other words, we assume V̂t > V̂t+1.
The expected benefit function works together with the physician’s shadow price of time to determine when a visit concludes. We propose two hypotheses about the determinants of the shadow price of time, and formulate an empirical test that distinguishes these hypotheses.
2.2 Hypotheses about topics and time allocation
The physician’s time is used efficiently when she deals with the topics that have the highest value to the patients she sees that day. A patient with many serious health problems would benefit from receiving more of a physician’s time than a patient with few problems or with problems the physician can do little about. Likewise, a topic within the physician’s expertise (e.g., joint pain) would benefit from receiving more time than a topic outside medical expertise (e.g, denture repair). The efficient allocation of the physician’s time can be described by a threshold value or shadow price, call it λ, such that any topic with value greater than λ is dealt with by the physician, and any topic with value less than λ is not. The value of λ is set so as to just use all of the time the physician has available. Another interpretation is that the physician has another activity with a constant value of λ. This other activity might, for example, be “administrative work,” that can be done during the day or handled at the end of the day.
This formulation of efficient use of the physician’s time ignores any other costs and benefits of health care, such as ancillary services that might result from additional topics, or benefits external to the patient. It also ignores patient waiting time, a subject we take up later.
H0: Physicians maximize the sum of the expected net benefits of their time to patients
Our null hypothesis is that physicians maximize the expected net benefit of their time with patients, in other words, allocate their time efficiently. Maximizing total expected benefit over all patients subject to an hours-in-the-day constraint (or a value of an alternative activity) leads to the rule that a physician admits a new topic if and only if V̂t+1≥λ. Our assumption about declining expected benefit of topics implies that there will be a unique number of topics admitted in each visit, and that this first-order condition is sufficient to characterize the allocation of topics that maximizes total patient benefit.
HA: A behavioral rule about visit length
Our alternative hypothesis is that physicians have a “target” amount of time that they desire to spend with each patient.6 If patients are scheduled four per hour, for example, that target would be 15 minutes. One way to model a “target” is to regard the shadow price of time to be zero up to the target and infinite after the target (McGuire and Pauly 1991). More generally and realistically, we could characterize the physician as being subject to a rapidly rising shadow price of time around the target. If we let τ be the time elapsed during a visit, the shadow price of time for a physician under HA is λ(τ), with λ′ > 0. Under HA the physician admits a new topic if and only if V̂t+1 ≥λ(τ). Patients as well as physicians might be the underlying source of norms about visit length. Patients might be “offended” if a visit is too short, for example. In this case, “avoiding offense” would be a kind of benefit to early topics that we can think of as being embedded in the lower subjective physician shadow price of time.7
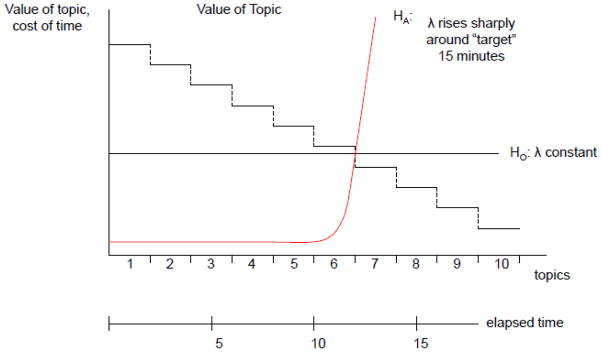
Two possible shadow price of time functions are depicted in Figure 1: the constant shadow price implied by H0 and the rapidly rising shadow price around a target time of 15 minutes implied by HA. If the shadow price of time were constant at λ, this visit would end after the sixth topic at about 12 minutes, and only factors associated with topics would explain whether a topic is the last (since λ is a constant). Under HA, this visit would also end at around 12 minutes, and factors explaining whether a topic is the last under HA include time elapsed as well as characteristics of the topic, since λ varies as time proceeds in a visit. This observation motivates our empirical test.
Figure 1. Physician Decision to End Visit.
HO: Topic 6 is last topic, topic value determines last, elapsed time has no effect
HA: Topic 6 is last topic, topic value and time elapsed determine last.
Testing H0 versus HA
The difference between the rule for HA and the rule for H0 is the presence of elapsed time during the visit, τ, in the decision rule. H0 implies an estimated coefficient of zero on τ in a model explaining whether a new topic is admitted, and HA implies τ will be negatively related to the likelihood of admitting a new topic.
2.3 Time within a topic
We complement the empirical analysis of ending a visit with an analysis of ending discussion on the current topic. Our null hypothesis, that physicians allocate time with an equal shadow price, predicts that time within a visit should not matter for topic time length. The alternative behavioral hypothesis is that physician’s shadow price rises rapidly around the target, and time on topic is less as visit time elapses.
3. Data
3.1 Physician and Patient Participants
We analyze videotapes of elderly patients and office-based physicians. Data were originally collected to test the Assessment of Doctor-Elderly Patient Transactions (ADEPT) system and to examine the relationship between physician communication behavior and patient outcomes (Cook 2002). All of the participating medical practices were located in the US, including an academic medical center in the Southwest, a private managed care group in a Midwest suburb, and a number of fee-for-service solo practitioners in a Midwest inner city. Physicians in the academic medical center were paid by salary. They did not have explicit service volume targets therefore they did not have the incentive to see many patients. Physicians in managed care group and the inner city were paid by fee-for-service. They had a strong incentive to see more patients. After being told the purpose of the study, physicians who expressed an interest in participating were contacted by the site program coordinator who described the study in detail and obtained written consent. Physicians and patients were informed that the videotapes would be used to study and improve patient-physician interaction, and that the videotapes would be archived and available for use by other researchers and medical educators.8
Thirty-five physicians, all of whom had completed their training, enrolled in the study. Patients had to be at least 65 years of age, identify the participating physician as their usual source of care, and provide informed consent. Specifically, patients were identified from their primary care physicians’ patient panels provided by office managers of the participating clinics. When these patients came to the participating clinic for a visit, regardless of the nature of the visit (e.g., acute upper respiratory infection, or for routine checkup for diabetes or hypertension), they were invited to participate in the study. If they expressed willingness to participate, informed consent was obtained and their visits were videotaped. The visits were recorded between 1998 and 2000. The final sample contained 385 videotaped visits. Nineteen of the visits were multiple visits between a few patient-physician “dyads,” i.e., pairs of patient and physician. Sensitivity analyses excluding these visits obtained similar results as the full sample. We used the full sample in this paper.
Human subject protection protocols for the original study were approved by all relevant institutional review boards. The current paper conducts secondary analyses of the data to address a set of research questions that are different from the original study.
3.2 Data from direct observation
Video recordings of the visits allow us to examine the length and content of visits. A number of coding approaches are available to study patient-physician interactions. One of them is the multidimensional interaction analysis (MDIA) system which codes an interaction based on topics sequentially introduced by patient or physician (Charon, Greene et al. 1994). We chose the MDIA over alternatives because it enabled us to examine the “topics” in a visit which we view as the unit of clinical decision making. Alternative coding systems (Roter 2003) usually use the visit as the unit of analysis which is a higher level of aggregation of the conversation and does not facilitate the sequential topic-by-topic analysis that we intend to do. In the MDIA, a topic is operationalized as a distinct clinical issue raised by either participant. The topics reflect the essential contents of the visit for which patients seek professional service from physicians. Coding of the videotaped visits consisted of identifying topics through partitioning a visit into topics similar to the MDIA topics and further aggregated several groups of MDIA topics so that there are 21 groups of topics. Further, we went beyond the MDIA and coded the time a topic was introduced, and the length of talk time by each participant.9 Furthermore, we categorized the topics according to the leading causes of disabilities.10 Details of the coding procedures have been reported previously (Tai-Seale, McGuire et al. 2007). The analysis file consists of 2,502 topics in 385 visits.
Direct observation of office visits using video data offers a number of advantages for our purposes. Direct observation avoids recall bias, self-perception bias (Dunning, Heath et al. 2004), and reporting error (Stange, Zyzanski et al. 1998; Gottschalk and Flocke 2005). Furthermore, it provides a complete representation of the patient-physician encounter, unlike a chart review which can be influenced by physicians’ charting patterns and their tendency to underreport delivery of some services or over-report other services (Stange, Zyzanski et al. 1998).
Coded data on initiation time of each topic enables us to examine topics as sequential discrete events unfolding over time which allows us to test whether physicians are characterized by a rising shadow price of time over the course of the visit. The transition from low to high shadow price is illustrated by the following exchange in one visit. At the start of the visit, when asked how she was doing, this 77 year-old woman responded that she had “mixed emotions.” The physician returned to this phrase 5 minutes, 35 seconds into the visit with an open-ended question:
Physician: So, what’s the mixed emotion about?
Patient: Well, I’m unsteady. I fall into things. I did this one other time, but it wasn’t that bad. But it’s gotten to the point that every day this happens. I can get up and turn into a chair.
Physician: You get dizzy when you turn?
Patient: Not necessarily dizzy; I’m just off balance.
Physician: Off balance. Why don’t you stand with your back to the wall; let’s see you walk here.
Patient: Ok.
Physician: I just want you to walk heel-to-toe over to me.
Patient: Ho, Ho, you’ve got to be kidding.
Physician: No, try again. Can’t do that? You’re doing pretty good.
The physician continued pursuing the topic of balance, potentially associated with the side effects of psychotropic medications, for a total of 10.5 minutes (physician spoke for 7.1 minutes, patient spoke for 1.6 minutes) spent on this topic alone.11
Twelve minutes later, at 17:15, after the physician has reviewed the patient’s medication with her, the physician is trying to wrap up the visit.
Physician: The girls are going to set up a follow-up appointment in two weeks and we will see how we’re doing. You’re going to stop the Lorazepam, stop Lorazepam,12 take Vitamin E, water pill, …
Patient: [Raising her hand as though to signal she has something to say] Now, …
Physician: [Taking her hand, shaking it, and continuing to talk] … everything else stays the same, including the Wellbutrin and we’re going to see you back in two weeks.
Patient: But now, you said on that Vitamin E, 1000 twice a day, 200013?
Physician: Yes, ma’am.
Patient: Ok.
Physician: That’s what the study states. It’s written down here. Ok?
Patient: Yeah, sure.
Physician: [Moving to help patient down from exam table and starts walking towards the door] There you go. We’ll try a little ‘addition by subtraction’ and hope that by stopping the Lorazepam that will stop your coordination difficulties and maybe the Wellbutrin we can continue.
Patient: You can talk to John14 about that. I’ve gotten bad.
Physician: [Both now walking out door] Your memory or your coordination?
Patient: Both.
Physician: Well, we’ll see; that’s why we’re bringing you back here.
An economic interpretation of this interaction is that seventeen minutes into the visit, the shadow price of the physician’s time is elevated. He ignored her raised hand, or more accurately, transformed it into a good-bye hand shake, and escorted her from the room. It seems likely that the patient had something she wanted to bring up, but the physician, at that point, was not prepared to hear it. During the same encounter, this physician is by turns patient and inquisitive (minute 5), and brisk and dismissive (minute 17).
3.3 Survey data
Surveys of the participating patients and physicians complement the video data. Variables from the surveys were chosen for analysis based on research about how patient-physician interaction is influenced by patient health (Bertakis, Callahan et al. 1993), gender and race (Roter, Hall et al. 2002; Balsa, McGuire et al. 2005) education (Waitzkin 1985), and physician gender (Roter, Hall et al. 2002; Roter and Hall 2004). Patient’s health status was measured by normed Medical Outcomes Study 36-item Short Form Survey (SF-36) scores (Ware, Kosinski et al. 2000). The length of the patient-physician relationship was measured by the number of years the patient had seen the physician (Waitzkin 1985).
4. Specification and Estimation
We test for the presence of an upward sloping shadow price of time during the visit. We first model the probability of a topic being the last. The key explanatory variables are four binary indicators of τ: initiation within 5 minutes of the beginning of the visit (serving as the reference group), between 5–10 minutes, between 10–15 minutes, and after 15 minutes. We also model the length of time devoted to a topic and see how this relates to these same time intervals. In both cases, we use generalized estimating equations (GEE) methods to account for the mixed-level structure of the data: topics clustered within a visit, visits clustered within a physician, and physicians clustered within a practice site.
Our model for the topic being the last is:
| (1) |
Where i indexes patients, and t indexes the current topic. Yt is an indicator variable for being the last topic when it is the tth topic of the ith patient of the jth physician and kth clinic. τt is a vector of indicator variables for the time topic t is initiated.
We employ extensive measures of the characteristics of the “seriousness” of a topic. In particular, we take advantage of the flexibility in the GEE model to include time-invariant fixed effects that are specific to individual topics (Hardin and Hilbe 2002). One indication of the importance of a topic is the nature of the topic, e.g., about biomedical issues, or psychosocial issues, measured by twenty one groups of variables described later. Another indicator of importance is whether it addresses a leading cause of disability or a major body system, say, circulatory system. If patients or physicians prioritize their use of time according to the importance of topics, we would expect to observe a pattern in which leading causes of disabilities (e.g., heart disease)would not only be addressed early during the visit rather than later, as the last topic of the visit in the extreme, but also receive more time than non-leading causes of disability (e.g., diarrhea). As mentioned earlier we account for the effect of severity of the topic by including a vector of indicator variables, Vt, corresponding to the twenty one groups of topics, five leading causes of disability: arthritis and musculoskeletal pain, heart and circulatory diseases, diabetes, mental illnesses, and lung diseases.15 Furthermore, to account for the importance of the topic according to either participant, we include a binary variable for patient initiation of the topic. We anticipate that if a patient initiates a topic, the topic may be more important to the patient.
As discussed above around (1), our expression for the expected health value of admitting a new topic, the physician forms an expectation of the value of a new topic on the basis of what has happened already in the visit and on the characteristics of the patient. We expect that the nature of topics prior to the current topic might play a role in physician’s decision about how much new information is still potentially there after what has already been discussed. Thus, we include a variable for the cumulative number of leading causes of disabilities discussed thus far into the visit, Ct, to account for the effect of information.
Xi is a vector of variables for patient i including age, gender, race, an indicator of ability to pay, physical and mental health status measured by SF36 composite scores. Xj is a vector of physician variables including age, gender, specialty (internist versus other), patient-physician being of the same race, patient-physician being of the same gender, and the number of years the patient has seen the physician as the usual source of care. Xk is a set of indicator variables telling whether the visit was at the Academic medical center, the managed care group, or the inner city solo practices. We use a logit link for the probability of a topic being the last of the visit. Descriptive statistics for key explanatory variables are contained in Table 1.
Table 1.
Descriptive Statistics on Key Variables
| Percent | Mean | |
|---|---|---|
| Topic Initiation Time | ||
| Within 5 minutes of visit | 51.27 | |
| Between 5 and 10 minutes | 24.51 | |
| Between 10 and 15 minutes | 11.92 | |
| After 15 minutes | 12.23 | |
| Topic Initiator | ||
| By patient (compared to physician) | 44.73 | |
| Nature of Topic Discussion | ||
| History, symptoms, and medical conditions | 24.66 | |
| Physical aches and pain | 11.35 | |
| Gynecological and genitourinary problems | 1.40 | |
| Prognosis, health status | 1.52 | |
| Test and diagnostic procedure: refer to specific test | 3.72 | |
| Appointment, referral | 3.52 | |
| Findings from exam, test results | 8.35 | |
| Medications | 10.51 | |
| Preventive medical measures | 5.32 | |
| Personal habits | 7.07 | |
| Living will, death, bereavement | 0.92 | |
| Care-giver, physical home, environment, family and significant others | 3.60 | |
| Health care system, money and benefits | 3.76 | |
| Intellectual exchange, small talk | 4.48 | |
| Work and leisure activities, religion | 2.56 | |
| Activity of daily living, age | 1.12 | |
| Psychological pain, suffering, concerns regarding patient’s own physical conditions | 0.68 | |
| Depression: not limited to clinically diagnosed depression | 1.48 | |
| General anxiety and worries, emotional distress, or other mood disorders | 1.40 | |
| Physician personal life | 1.60 | |
| Physician-patient relationship | 1.00 | |
| Leading Causes of Disability | ||
| Arthritis/Musculoskeletal | 8.95 | |
| Heart/Circulatory | 14.57 | |
| Diabetes | 3.13 | |
| Mental Illness | 4.00 | |
| Lung | 3.21 | |
| Not Applicable | 66.15 | |
| Physician Characteristics | ||
| Age | 50.64 | |
| Internist Physician | 36.54 | |
| Female Physician | 22.87 | |
| Patient Characteristics | ||
| Age | 74.49 | |
| Female Patient | 66.63 | |
| African American Patient | 8.43 | |
| Patient Had More than Enough Money | 82.33 | |
| SF36 Physical Health Summary | 40.06 | |
| SF36 Mental Health Summary | 51.59 | |
| Patient-Physician Dyad Characteristics | ||
| Patient-Physician Same Race | 87.33 | |
| Patient-Physician Same Gender | 49.37 | |
| Years Patient Had Seen this Physician | 6.09 | |
| Clinic Characteristics | ||
| Academic Medical Center | 36.15 | |
| Managed Care Group | 57.67 | |
| Inner City Solo Practices | 6.18 | |
Total number of topics in sample: 2,502.
The second dependent variable is the length of time allocated to each topic. Using similar notation and explanatory variables included in (1), we perform GEE regression of the length of time spent on topic t, with patient i of physician j in clinic k, with the log link function.
One issue with our empirical strategy is that initiation time (τ) may be correlated with unmeasured severity or seriousness of a topic, leading to biased estimates of a shadow-price effect. This would be the case, for example, if patients prioritize the topics they wish to speak about and leave the least serious to last. Likewise, physicians might end visits and allow less time for topics because the topics are less important, not because the shadow price of their time has gone up.
We explored including indicator variables for laboratory tests or procedures prior to the current topic as they may signify severity of illnesses. We also explored including a variable on whether there was a small talk topic prior to the current topic, e.g., weather, to approximate how much of a hurry the physician may be in. Neither variable had a significant effect in the regression analysis. Therefore these variables are not included in the final analytic model.
We recognize that topics raised later in a visit could be less important in ways we do not capture in the measures available to us in our data. We do know the order in which topics are raised, however, and we can use this to explore the implications of prioritization in terms of topic importance for our test of rationing rules. We make an assumption about how order is related to importance and include this parameterization of importance in the model. Specifically, we create an artificial variable which we call “importance” (IMP) and assume for each topic t,
where s is the index counting the sequential order in which the topic appears in a visit, and ρ is a parameter ρ > 0. If ρ = .5, for example, the importance of topics would fall with the inverse of the square root of the topic counter. If the increasing effect of time is a function of the importance of a topic, rather than the shadow price of time, including a variable that can appropriately capture the importance would make time effect less significant. We will assess the impact of our time coefficient under various values of ρ.
Analyses were performed in STATA, version 9 (Stata Corp, College Station, TX, 2005). We report the results from the logit model in Table 2 and the log-linear model in Table 3.
Table 2.
Probability of a Topic Being the Last Topic of the Visit (GEE Logit Link)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Coef. | S. E. | Coef. | S. E. | Coef. | S. E. | |
| Topic initiation time | ||||||
| Between 5 ~ 10 minutes | 1.974 | 0.184** | 1.975 | 0.217** | 1.399 | 0.234** |
| Between 10 ~ 15 minutes | 2.539 | 0.198** | 2.579 | 0.251** | 1.896 | 0.271** |
| Beyond 15 minutes | 3.009 | 0.191** | 3.122 | 0.252** | 2.368 | 0.290** |
| Topic Initiator | ||||||
| Patient Initiated topic | 0.397 | 0.141** | 0.432 | 0.142** | ||
| Nature of Topic | ||||||
| Physical aches and pain | 0.564 | 0.282* | 0.558 | 0.271* | ||
| Gynecological and genitourinary problem | 0.085 | 0.708 | 0.103 | 0.654 | ||
| Prognosis, health status | −0.495 | 1.139 | −0.523 | 1.092 | ||
| Test and diagnostic procedure | 0.912 | 0.385* | 0.844 | 0.377* | ||
| Appointment, referral | 0.740 | 0.358* | 0.760 | 0.355* | ||
| Findings from exam, test results | 0.569 | 0.319 | 0.520 | 0.308 | ||
| Medications | 1.040 | 0.263** | 1.096 | 0.257** | ||
| Preventive medical measures | 1.069 | 0.302** | 1.000 | 0.289** | ||
| Personal habits | −0.019 | 0.336 | 0.001 | 0.314 | ||
| Living will, death, bereavement | 1.702 | 0.633** | 1.762 | 0.696* | ||
| Care-giver, physical home, environment, family | 0.995 | 0.346** | 0.926 | 0.342** | ||
| Health care system, money and benefits | 1.030 | 0.349** | 1.111 | 0.369** | ||
| Intellectual exchange, small talk | 0.888 | 0.349* | 0.928 | 0.341** | ||
| Work and leisure activities, religion | 1.250 | 0.411** | 1.243 | 0.424** | ||
| Activity of daily living, age | 0.614 | 0.579 | 0.665 | 0.601 | ||
| Psychological pain, suffering, concerns | 2.290 | 0.761** | 2.372 | 0.763** | ||
| Depression: not limited to diagnosed depression | 1.694 | 0.727* | 1.911 | 0.745** | ||
| General anxiety and worries, emotional distress | 1.689 | 0.709* | 1.834 | 0.673** | ||
| Physician’s personal life | 0.663 | 0.513 | 0.688 | 0.536 | ||
| Physician -patient relationship | 1.862 | 0.504** | 1.820 | 0.557** | ||
| Leading causes of disabilities | ||||||
| Arthritis/Musculoskeletal | −0.236 | 0.294 | 0.021 | 0.288 | ||
| Heart/Circulatory | −0.090 | 0.245 | 0.137 | 0.246 | ||
| Diabetes | −0.524 | 0.503 | −0.333 | 0.484 | ||
| Mental Illness | −0.816 | 0.502 | −0.816 | 0.526 | ||
| Lung | −0.091 | 0.456 | 0.053 | 0.448 | ||
| Cumu_N leading causes§ | 0.180 | 0.052** | 0.030 | 0.058 | ||
| Physician Characteristics | ||||||
| Female | −0.115 | 0.214 | −0.132 | 0.253 | ||
| Internist | −0.185 | 0.162 | −0.248 | 0.179 | ||
| Older than 45 years of age | 0.384 | 0.242 | 0.404 | 0.275 | ||
| Patient Characteristics | ||||||
| SF36 physical health component | 0.009 | 0.009 | 0.002 | 0.010 | ||
| SF36 mental health component | 0.007 | 0.007 | 0.005 | 0.008 | ||
| 65 ~ 75 years of age | −0.002 | 0.268 | −0.068 | 0.285 | ||
| 76 ~ 85 years of age | −0.304 | 0.282 | −0.366 | 0.303 | ||
| Older than 85 years of age | −0.131 | 0.316 | −0.268 | 0.339 | ||
| African American | 0.298 | 0.345 | 0.190 | 0.374 | ||
| Female | −0.314 | 0.168 | −0.305 | 0.197 | ||
| Had More than Enough Money | −0.032 | 0.186 | −0.039 | 0.208 | ||
| Patient-Physician Dyad Characteristics | ||||||
| Same race | −0.157 | 0.208 | −0.168 | 0.231 | ||
| Same gender | −0.301 | 0.169 | −0.325 | 0.196 | ||
| Years Patient Had Seen this Physician | −0.009 | 0.009 | −0.012 | 0.010 | ||
| Practice Site | ||||||
| Academic Medical Center | −1.309 | 0.253** | −1.362 | 0.290** | ||
| Inner City FFS Solo Practices | 0.143 | 0.429 | 0.539 | 0.479 | ||
| Artificial variable for “importance” | −5.006 | 0.779** | ||||
| Constant | 0.368 | 0.125** | −2.449 | 0.934** | 0.638 | 1.078 |
Table 3.
Length of Time Spent on Discussing Each Topic (GEE with Log Link)
| Model 4 | Model 5 | Model 6 | ||||
|---|---|---|---|---|---|---|
| Coef. | S.E. | Coef. | S.E. | Coef. | S.E. | |
| Topic initiation time | ||||||
| Between 5 ~ 10 minutes | −0.451 | 0.065** | −0.242 | 0.070** | −0.039 | 0.078 |
| Between 10 ~ 15 minutes | −0.442 | 0.089** | −0.310 | 0.092** | −0.063 | 0.096 |
| Beyond 15 minutes | −0.392 | 0.085** | −0.238 | 0.114* | 0.029 | 0.111 |
| Topic initiator | ||||||
| Patient initiated topic | 0.121 | 0.059* | 0.105 | 0.056 | ||
| Nature of Topic | ||||||
| Physical aches and pain | 0.134 | 0.080 | 0.143 | 0.078 | ||
| Gynecological and genitourinary problem | 0.173 | 0.181 | 0.230 | 0.173 | ||
| Prognosis, health status | −0.145 | 0.230 | −0.268 | 0.223 | ||
| Test and diagnostic procedure | −0.212 | 0.120 | −0.195 | 0.120 | ||
| Appointment, referral | −0.302 | 0.125* | −0.358 | 0.133** | ||
| Findings from exam, test results | 0.010 | 0.144 | 0.009 | 0.132 | ||
| Medications | −0.230 | 0.083** | −0.197 | 0.086* | ||
| Preventive medical measures | −0.523 | 0.118** | −0.461 | 0.119** | ||
| Personal habits | −0.391 | 0.160* | −0.368 | 0.166* | ||
| Living will, death, bereavement | −0.330 | 0.288 | −0.263 | 0.315 | ||
| Care-giver, physical home, environment, family | −0.017 | 0.136 | −0.079 | 0.142 | ||
| Health care system, money and benefits | −0.975 | 0.137** | −1.082 | 0.141** | ||
| Intellectual exchange, small talk | −0.827 | 0.140** | −0.908 | 0.153** | ||
| Work and leisure activities, religion | −0.404 | 0.140** | −0.436 | 0.144** | ||
| Activity of daily living, age | −0.226 | 0.360 | −0.135 | 0.363 | ||
| Psychological pain, suffering, concerns | 0.102 | 0.326 | 0.234 | 0.280 | ||
| Depression: not limited to diagnosed depression | 0.139 | 0.255 | 0.124 | 0.248 | ||
| General anxiety and worries, emotional distress | −0.144 | 0.209 | −0.145 | 0.199 | ||
| Physician’s personal life | −0.791 | 0.160** | −0.879 | 0.170** | ||
| Physician -patient relationship | −0.511 | 0.236* | −0.544 | 0.239* | ||
| Leading causes of disabilities | ||||||
| Arthritis/Musculoskeletal | 0.219 | 0.086* | 0.134 | 0.086 | ||
| Heart/and Circulatory | 0.156 | 0.091 | 0.065 | 0.090 | ||
| Diabetes | 0.314 | 0.129* | 0.204 | 0.135 | ||
| Mental Illness | 0.547 | 0.183** | 0.435 | 0.174* | ||
| Lung | 0.179 | 0.130 | 0.083 | 0.126 | ||
| Cumulative # of leading causes of disability§ | −0.163 | 0.032** | −0.062 | 0.032 | ||
| Physician Characteristics | ||||||
| Female | 0.183 | 0.075* | 0.171 | 0.077* | ||
| Internist | 0.074 | 0.055 | 0.074 | 0.051 | ||
| Older than 45 years of age | −0.168 | 0.074* | −0.158 | 0.073* | ||
| Patient Characteristics | ||||||
| SF36 physical health component | −0.006 | 0.003 | −0.004 | 0.003 | ||
| SF36 mental health component | −0.003 | 0.003 | −0.002 | 0.002 | ||
| 65 ~ 75 years of age | −0.138 | 0.149 | −0.096 | 0.112 | ||
| 76 ~ 85 years of age | −0.080 | 0.152 | −0.037 | 0.116 | ||
| Older than 85 years of age | −0.213 | 0.169 | −0.146 | 0.135 | ||
| African American | −0.210 | 0.241 | −0.121 | 0.195 | ||
| Female | 0.066 | 0.069 | 0.038 | 0.072 | ||
| Had More than Enough Money | −0.068 | 0.061 | −0.051 | 0.057 | ||
| Patient-Physician Dyad Characteristics | ||||||
| Same race | 0.116 | 0.085 | 0.103 | 0.077 | ||
| Same gender | −0.055 | 0.070 | −0.052 | 0.073 | ||
| Years Patient Had Seen this Physician | −0.004 | 0.004 | −0.003 | 0.003 | ||
| Practice Site | ||||||
| Academic Medical Center | 0.479 | 0.083** | 0.454 | 0.077** | ||
| Inner City FFS Solo Practices | 0.079 | 0.271 | −0.055 | 0.230 | ||
| Artificial variable for “importance” | 1.017 | 0.164** | ||||
| Constant | 4.385 | 0.068** | 6.101 | 0.322** | 5.192 | 0.327** |
4. Results
4.1 Descriptive Statistics
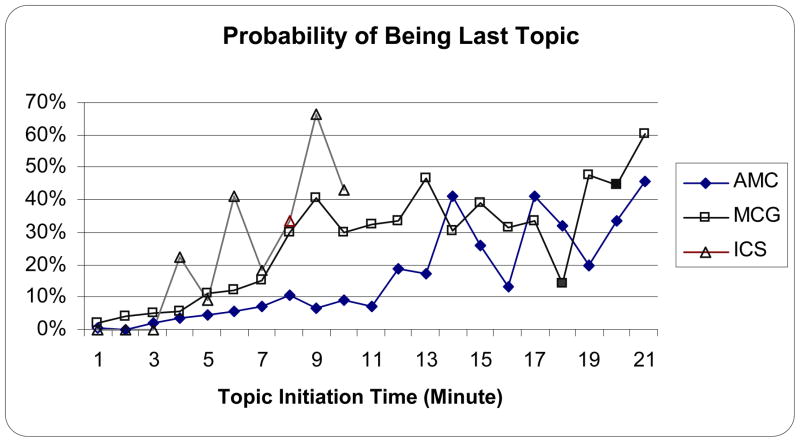
Figure 2 displays the unadjusted probability for a topic to be the last topic of a visit across the three types of practice settings according to the time the topic was initiated. The likelihood of a topic being the last rises with time of initiation in all three settings. The Academic Medical Center displays the most target-like pattern. Topics initiated around minute 14 are likely to be the last, wrapping up the visit at about 15 minutes. By the time 9 minutes have passed, the likelihood of this being the final topic at the Inner City Solo practices is very high. The Managed Care Group exhibits an elevated likelihood of a topic being the last at around 10 minutes, but the rise is not as sharp as for the other two settings.
Figure 2. Probability of A Topic to be the Last Topic across Practice Settings.
AMC: academic medical center, MCG: managed care group, ICS: inner city fee-for-service solo practitioners.
Note: due to the small number of observations for visits lasting beyond 10 minutes at the Inner City Solo (ICS) practices, we aggregated the data to 10 minutes or more.
Table 1 provides the descriptive statistics on the key variables. Out of 2,502 topics in 385 visits, 51.3 percent of topics were initiated within the first 5 minutes of a visit, followed by 24.5 percent initiated between 5 and 10 minutes, and 11.9 percent between 10 and 15 minutes, and 12.2 percent after 15 minutes into the visit.16 Patients initiated 44.7 percent of the topics. With respect to the nature of the topics addressed, the largest group of topics (24.6%) was about history, symptoms, and medical conditions. The next group of topics in frequency was physical aches and pain (11.4%) followed by medications (10.5%). Further, about 14.6 percent of the topics addressed heart diseases and circulatory illnesses, followed by 9.0 percent addressing arthritis or musculoskeletal concerns, 4 percent on mental illness, 3.2 percent on lung diseases, and 3.1 percent on diabetes. The majority of the topics (66 percent) did not address any of the five leading causes of disabilities. Among physicians, 36.5 percent were internists, 22.9 percent were female. The majority of patients were female (66.7 percent). African Americans made up 8.4 percent of the patient population. More than 82 percent of patients reported having more than enough money to make ends meet. The average score of physical component of SF36 was 40.0 whereas the average score of mental health component of SF36 was 51.6. The characteristics of the patient-physician dyad include an average of 6 years of the physician had served as the usual source of care for the patient. Over 87 percent of the dyads were of the same race and 49.4 percent of them were of the same gender. Of the three types of practices, 36.2 percent of the visits took place in the Academic Medical Center, 57.7 in the managed care practice, and 6.2 percent in the inner city solo practices.
4.2. Probability of a Topic Being the Last in a Visit
We now discuss the GEE logit estimates displayed in Table 2. The key estimates in table are the set of coefficients on the indicators of when was the topic initiated. The first set of columns (Model 1) contains estimates of the effects of the initiation times only. They show that when compared with topics introduced in the first five minutes of the visit, the probability of a topic being the last of the visit increases rapidly with initiation time. All indicator variables are highly statistically significant (p<0.01). A Wald test of the joint effect of these three time variables is also highly significant.
The second set of columns (Model 2) includes additional covariates that are related to the nature of the topic. The time variables continue to have rapidly rising and statistically significant effects, all p<0.01. Again, a Wald test shows significant joint effect of the time variables. We also find that patient initiation significantly increase the probability of the topic becoming the last topic of the visit (Coef.=0.397, S.E.=0.141). A number of the indicator variables for the nature of topics are significantly different from the referent group which is history, symptoms, and medical conditions. The coefficients for the individual leading causes of disabilities are not statistically significant although the cumulative number of leading causes of disabilities discussed thus far is statistically significant (Coef.=.180, S.E.=0.052). Topics discussed in the Academic Medical Center have lower probability of being the last (Coef.=−1.309, S.E.=0.253). None of the other sociodemographic or health status measures have statistically significant effects on the likelihood of a topic being the last.
The third set of columns (Model 3) contains results when we include the artificial variable we created to capture “importance” based on the sequence of topics. We explored several values for the parameter ρ, including 0.1, 0.5, 2, implying different rates of decay in importance according to topic sequence. We also tried taking the inverse of the exponential function of the sequential order of the topic as a measure for the importance. The results are qualitatively similar throughout. We chose to show the results for a = .5 because it is representative of the findings for other values.17 The introduction of this artificial variable slightly reduced the magnitudes of the time variables but did not affect their statistical significance. The cumulative number of leading causes of disability discussed so far in the visit is no longer a statistically significant factor. Topics discussed in the Academic Medical Center still have lower probability of being the last (Coef.=−1.362, S.E.=0.290). The coefficient for the artificial variable itself is negative (−5.006) and highly significant (S.E.=.779). These results imply that the effect of time is robust to inclusion of multiple covariates for the “importance” of a topic. After controlling for the possibility of topics introduced later in the visit being less important, the effects of the time remain statistically significant. We calculated the marginal effects for the predicted probability of the time variables and bootstrapped for standard errors. The results show that, in comparison to a topic initiated in the first five minutes, the increase in the likelihood of a topic being last increased by .168 (s.e.=.030), to .268 (s.e.=.042), to .357 (s.e.=.043) with each successive increment in the block of time for topic introduction. Overall in the data, if a topic is raised after 15 minutes, the chances that this is the last topic are .80.
The findings are consistent with the behavioral hypothesis that time elapsed in a visit affects the decision to end. The impact of covariates pertaining to the “importance” of the topic, practice setting and characteristics of patient and physician reduced the magnitudes of the point estimates somewhat but did not interfere with their statistical significance.
4.3 Analyses on Length of Time Allocated to a Topic
Findings on the impact of time on length of discussion during topics are presented in Table 3. As before, we first use only the initiation time blocks as the explanatory variables (Model 4). The point estimates show that the length of discussion on a topic declines with the time it is initiated. Estimates can be interpreted directly in minutes. For example, in comparison to a topic initiated within the first five minutes, a topic initiated between minutes 5 and 10 lasts .451 minutes (27 seconds) less. (The average topic length is less than two minutes.) The effects are highly statistically significant (p<0.01). In the second step (Model 5), we included additional explanatory variables. Similar to results in the logit analysis presented earlier, the time spent on discussion of a topic is also influenced by the initiator of the topic. Patient initiated topics are .12 minutes longer (p<0.05). The nature of discussion also plays a role in determining the amount of time given to a topic. The effects are more diverse with directions of effects differing across natures of topics. For example physical aches and pain would have longer time whereas appointment and referrals, preventive medical measures, personal habits would have shorter time.
Among topics concerning the five leading causes of disabilities, mental health topics were .547 minutes longer (S.E.=.183), diabetes topics were .314 minutes longer (S.E.=.129), and arthritis and musculoskeletal pains were .219 minutes longer (S.E.=.086), compared with topics that do not address leading causes of disabilities. Having discussed greater number of leading causes of disabilities before the current topic appears to have reduced the amount of time spent on the current topic (Coef.=−.163, S.E.=.032), but this could be partly an effect of sequence. While inner city solo practices are similar to the managed care group practice, physicians in the Academic Medical Center spend .479 minutes longer on each topic (S.E.=.083). Female physicians also spend more time whereas physician older than 45 years of age spend less time on topics. Lastly, including the artificial variable for importance based on the sequence of visit reduced the estimated impact of the time of initiation variables and rendered them statistically non-significant. A Wald test confirmed that as a group, these variables are non-significant in Model 6. Leading causes of disabilities with the exception of mental health issues no longer differ significantly from non-leading causes in discussion time. The artificial importance variable is highly significant (Coef.=1.017, S.E=.164). The effects of Academic Medical Center, physician’s gender, physician’s age remain significant.
In contrast to the results of the likelihood of a topic being the last, a parameterization of the sequence of a topic (our artificial “importance” variable) obviates the estimated effect of time of initiation. In this second set of analyses, we find no additional evidence supporting the behavioral interpretation of physician time allocation.
5. Discussion
We found evidence in favor of the behavioral rule consistent with an increasing shadow price of time during a visit in physicians’ decisions about admission of new topics, but not in time devoted to topics after we added an artificial variable that we created to capture unmeasured importance of a topic that is related to the order of the topic. We do not regard these results as being in conflict. Of course importance of a topic matters in terms of whether a new topic is admitted or in the time devoted to it. Our hypothesis about increasing shadow price of time is that in addition to this primary factor of importance, physicians also see their time as more scarce after some time in a visit has elapsed. Being pressed for time, they turn to heuristics or rules-of-thumb (Gigerenzer and Goldstein 1996). This seems to come into play in our data in physicians’ receptivity to “anything else?” as the visit proceeds.
Flexibility, in general, is a good thing. Time spent during a visit does vary in our data, and varies in response to some clinical factors in reasonable ways. Our findings question whether there should not be more flexibility in order to direct physician time to problems with the highest value. Regimented clinical schedules challenge physicians’ ability to manage time and provide good clinical services in an office visit (Tai-Seale, McGuire et al. 2007). Physician-educators have argued that cogent thinking and clear communication cannot be conducted like a race being run (Groopman 2007). This is particularly true with older patients, as in our data, who populate primary care practices and who commonly have multiple chronic and complicated problems.
We must recognize at the same time that a regimented schedule is adaptive for both physicians and patients. It can help physicians keep up with their daily work flow, and help patients by letting them know when they should expect to be seen. More flexibility in physician time allocation while keeping the same mean time per visit would have little effect, however, on average wait time for patients.
Some of the rigidity in scheduling is due to the way physicians are paid. The findings of significant differences in how visits end and in the lengths of time on topics across practice settings are important. They offer additional evidence of the influence of financial incentives on physician practices. Volume-based FFS payment system rewards physicians for seeing more patients which translates to more rushed visits.
Psychotherapists paid for a 50-minute visit give patients 50 minutes of time with little flexibility. Primary care physicians’ procedures are less tightly linked to time and do already permit considerable flexibility. More time-consuming and complex office visits can be given higher codes (see above note 3) although the fear of being audited lead physicians to “median code”. Proposals for reform of primary care payment around the idea of a ”patient-centered medical home” involve a mixed payment method in which part of the PCP’s pay is in the form of capitation (Goroll, Berenson et al. 2007), and are very consonant with the increased flexibility we propose here. Physicians less driven by procedure-based payments should be more flexible in allocation of their time that does not, per se, generate billable procedures. Salary based payment, separate from RVU adjustments, also offer physicians more freedom in tailoring their time use to needs of their patients. A case study of a patient-centered medical home (PCMH) at the Group Health of Puget Sound where physicians are salaried found the PCMH model resulted in improved patient satisfaction and physician quality of work life, reduced Emergency Department use, increased the length of office visits, but reduced office visit frequency (Reid, Fishman et al. 2009).
Applying principles from industrial engineering and queuing theory (Hall 1991), Murray and Berwick suggest that a strategy for reducing demand rests in maximizing the effectiveness of each visit by covering multiple issues at one sitting (Murray and Berwick 2003). Limiting the number of issues addressed or not addressing some of them effectively – as evidenced in our studies – may actually contribute to backlog because patients would demand more return visits to address unresolved issues. Our findings point to the necessity to prioritizing in the beginning of the visit so that patient and physician can jointly determine the agenda of the visit so that they can allocate sufficient time for the most important issues to be addressed within the visit. If there is not enough time within the visit then follow-up effort outside the visit can be continued through telephone follow-up, e-visits, or services by provided by non-physician staff of the care team.
While evidence for a time-based behavioral rule may not be surprising, the implications of this behavior may be significant. Changing physician practice so as to give patients “more time” with their doctor cannot be done without putting more resources into health care or significant re-alignment of incentives and restructuring how resources are allocated. For instance, Group Health’s PCMH restructuring involved reducing physicians’ patient panel size by half, a rather drastic change in case load which enabled physicians to spend more time with patients who are on their panel (Reid, Fishman et al. 2009). The reduced panel size also enables practices to offer advanced access, i.e., same-day scheduling, or open access (Murray and Berwick 2003) and reduce physician and staff stress (Reid, Coleman et al. 2010). For HMOs such as Group Health, reducing frequency of office visits could mean real cost savings. Recent evidence from Group Health suggests a remarkable cost savings have been achieved through its primary care redesign efforts (Reid, Coleman et al. 2010). Exploiting this potential efficiency gain at the practice level can help finance payment reform. If patients see better value on average in a practice with more flexibility, PCPs paid in a way to encourage flexibility will have a competitive advantage.
The growth in “concierge medicine” may be indicative of such an advantage in a segment of the market. Practiced by a small but growing number of physicians located mainly on the East and West Coasts of the United States, concierge care is an approach to medical practice in which physicians charge their patients a membership fee in return for enhanced services or amenities. A General Accounting Office (GAO) survey of physicians practicing concierge medicine shows that the annual patient membership fees range from $60 to $15,000 a year, with about half of respondents reporting fees of $1,500 to $1,999 (U.S. Government Accountability Office 2005). The enhanced services or amenities include same- or next-day appointments for nonurgent care, 24-hour telephone access, periodic preventive care examinations, extended and more personalized office visits (U.S. Government Accountability Office 2005), house calls, and physician accompaniment to a specialist (Majette 2009). Primary care doctors switching their practice to “concierge medicine” cite time pressure per patient in routine primary care as a major reason they make the shift (Forester 2008). Patients in concierge medicine are more likely to report that their physician spends sufficient time in clinical encounters than patients of general medicine practice (Ko, Rodriguez et al. 2009). Increasing flexibility in physician time allocation would have to overcome institutional obstacles. Patients may have expectations about physician visits that may be about time rather than health outcomes which they can’t judge very well. Patients (and doctors) may see it as “fair” to give people a certain amount of time, especially since patients at least partly are paying for the visit. Patients may resist being hustled out if their problems are minor. Flexibility sounds great if you think you will be the recipient of more time, but down-side of the mini visit may simply be difficult to accept. Hence, quite apart from marginal productivity considerations, physicians’ rationale for adopting a behavioral rule may be based on this need to be fair to all patients.
The analogy is often made between a physician and an auto mechanic. In both cases customers lack technical knowledge and must trust in the behavior of the seller. Our expectation of time is quite different however, as between these two suppliers. When we leave a car, the expectation is that the mechanic “fix it,” and the amount of time it takes may be more variable, unlike a physician office visit.
This study has several limitations. First, cross-section data on one visit may not be representative of all visits between the dyad. Second, we neither have information on when during the day the visit took place nor is there information on how long the patient waited. We also do not know how full the physician’s schedule was. It is possible that visits which took longer than their scheduled time earlier on during the day could create havoc in physician’s ability to stay to the schedule in subsequent visits. Previous research suggests this may not be as extensive as suggested by anecdotes, however. For example, Tai-Seale, McGuire and Zhang (2007) reported that visit lengths are more likely to be determined by practice setting organizational norm and financial incentives than variations in patients’ needs. Further, if the scheduler is successful at matching patient’s demand with the supply of visits lengths, (e.g., x number of 15-minute visits, y number of 20-minute visits, and z number of 45-minute visits for physical exams,) physicians may be able to close the visits within its pre-determined time frame. As more and more organizations move to advanced access, or same-day access, after working down backlogs, there may be more room in the physician’s schedule to accommodate a limited number of unexpectedly long visits (Murray and Berwick 2003). In addition, if physicians operate like professional tennis coaches who supply predetermined time independent of students’ skill levels, deviation from schedules is less likely to occur. Lastly, data on physicians’ past practice pattern was not available. Future studies will need to collect data that can capture the influence of those factors.
Footnotes
Visit times in the U.S. are generally longer than in other countries. Deveugele et al. (2002) report average visit length for GPs for six European countries: Germany (7.6 minutes), Spain (7.8), UK (9.4), Netherlands (10.2), Belgium (15.0), Switzerland (15.6). Using audiotapes, Bensing, Roter and Hulsman (2003) confirm these results for the Netherlands, finding that routine medical visits for hypertension were six minutes longer in the U.S. (15.4 vs 9.5 minutes). Bindman et al. (2007) found office visit durations were slightly lower in Australia and New Zealand in comparison to the US, though patients in Australia and New Zealand saw their primary care doctors more frequently. Patients in European countries also see their doctor more frequently than in the U.S.. Although physician and patient behavior within a visit will be affected by the incentives in various health systems, physicians everywhere face the problem of deciding when to move on to the next patient. Shorter average visits may intensify the pressure to end. While the model of physician decision making proposed here may be transportable across health care systems, we are not in a position to speculate about whether our empirical findings generalize internationally.
It is clear from the videotapes that physicians run the visits, including deciding when a visit should be wrapping up. The videotapes rarely convey the impression that the physician is open to more talking whereas the patient has decided they have nothing more to talk about.
Some information about physicians’ coding practice patterns supports this assumption. Specifically, the primary payer for all patients in our data is Medicare. For purpose of reimbursement, an office visit for any established patient is coded with one of five levels of CPT codes, from 99211 to 99215. At the lower end of the continuum, 99211 is for the evaluation and management of a minimal problem in an established patient that may not require the presence of a physician and the office or other outpatient visit takes no more than 5 minutes. At the higher end, 99215 is for taking comprehensive history, conducting comprehensive exam, making highly complex medical decisions or dealing with a high severity problem, and takes at least 40 minutes of physician time. While payments for these codes vary, physician coding practices are not very sensitive to the actual content of office visits (Calahan 2006). Physicians reportedly practice “median coding,” i.e., predominantly using 99213, the median effort level CPT (Seiber 2007).
In Tai-Seale, McGuire et al. (2007), the median time on the longest topic of each visit was five minutes, and one minute on the remaining topics during the visit. The median time on all topics was two minutes. The median number of topics was six per visit.
One of our topics is “small talk,” which amounted to about five percent of total topics. When it occurred, small talk was more likely to be the first or last topic.
Interestingly, these two rationing devices for a physician’s time are analogous to the two ways in which managed care rationing have been modeled in the literature. Beginning with Keeler et al. (1998), papers including the literature on optimal risk adjustment. Glazer and McGuire (2000) use the shadow price approach analogous to the null hypothesis where physicians ration time to maximize patient net benefit. Pauly and Ramsey (1999) is an example of a quantity rationing approach to managed care which conceives of the plan as setting quantity targets for treatment of a condition without regard for variation in the value of services to particular patients. This is analogous to our behavioral approach based on time targets per visit.
Patient waiting time raises distinct issues and as we discuss later is unlikely to be a source of a rapidly rising shadow price.
Videotapes are archived at Saint Louis University Library under the title “Assessment of Doctor-Elderly Patient Transactions,” and may be viewed by researchers after an application process.
During the course of a visit, a topic may be discussed, interrupted or discontinued, and returned to later in the visit. We set the time of introduction of a topic to be the first time the topic is discussed. The total time spent on a topic is the sum of the time of all instances the topic is discussed.
We also categorized the biomedical topics according to the major body systems, e.g., circulatory, endocrine, etc, and obtained very similar results to those reported here. To avoid multicollinearity, we only employed the vector of variables on leadings causes of disabilities in the empirical models below.
In total, this visit contained six topics. The contents and length of time (in minutes) spent on them were: (1) anxiety over difficulties with balancing and memory loss potentially related to side effects of psychotropic medications, 10.53 minutes; (2) thyroid function tests, 0.82 minutes; (3) cholesterol and triglycerides test results, 1.25 minutes; (4) follow-up on blood pressure, 2.95 minutes; (5) review of medications, 1.03 minutes; and (6) chest pain and medication for controlling it, 1.12 minutes.
Stopping Lorazepam (a Benzodiazepine drug) so suddenly without careful tapering could exacerbate anxiety.
The current United States dietary guidelines do not recommend vitamin E supplementation; however, the guidelines do set an upper tolerable intake limit of up to 1,500 IU (international units) per day. Use of high-doses of vitamin E supplements, in excess of 400 IU, is associated with a higher overall risk of dying in one report (Miller et al 2005).
Pseudonym for patient’s husband.
See NCHS (2007). An alternative model that included indicators for major body systems in place of the leading causes of disabilities produced qualitatively similar results.
Different tempos appear across sites (not tabulated): more than fifty percent of the topics in the managed care and inner city settings were introduced in the first 5 minutes of the visit whereas 42 percent of the topics were introduced during the same period. Over eighty percent of the topics were initiated within 10 minutes of the visit in the managed care practice and inner city settings compared with only sixty three percent of the topics initiated in the same period in the Academic Medical Center.
The magnitudes of the coefficients on the first time variable (5–10 minutes after beginning of visit) changed from 1.60, to 1.43, to 1.38 with the increase in value of ρ from 0.1. to 0.5, to 2. The coefficients on the second time variable (10–15 minutes after beginning of visit) changed from 2.19, to 1.93, to 1.90. The coefficients on the third time variable (15 minutes after beginning of visit) changed from 2.74, to 2.38, to 2.37. All are statistically significant at p<0.01 level.
6. Conflict of Interest:
None.
References
- Balsa AI, McGuire TG, et al. Testing for statistical discrimination in health care. Health Services Research. 2005;40(1):227–252. doi: 10.1111/j.1475-6773.2005.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertakis KD, Callahan EJ, et al. The effect of patient health status on physician practice style. Family Medicine. 1993;25(8):530–535. [PubMed] [Google Scholar]
- Charon R, Greene MG, et al. Multi-dimensional interaction analysis: a collaborative approach to the study of medical discourse. Social Science & Medicine. 1994;39(7):955–965. doi: 10.1016/0277-9536(94)90207-0. [DOI] [PubMed] [Google Scholar]
- Cook M. Final Report: Assessment of Doctor-Elderly Patient Encounters, Grant No. R44 AG5737-S2. Washington, D.C: National Institute of Aging; 2002. [Google Scholar]
- Dunning D, Heath C, et al. Flawed self-assessment: Implications for health, education, and the workplace. Psychological Science in the Public Interest. 2004;5(3):69–106. doi: 10.1111/j.1529-1006.2004.00018.x. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Epstein RM. So Much to Do, So Little Time: Care for the Socially Disadvantaged and the 15-Minute Visit. Arch Intern Med. 2008;168(17):1843–1852. doi: 10.1001/archinte.168.17.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forester R. A new model of charitable care: The Robin Hood Practice. Family Practice Management. 2008;15(2):12–16. [PubMed] [Google Scholar]
- Gigerenzer G, Goldstein D. Reasoning the Fast and Frugal Way: Model of Bounded Rationality. Psychological Review. 1996;103(4):650–669. doi: 10.1037/0033-295x.103.4.650. [DOI] [PubMed] [Google Scholar]
- Glied S, Zivin JG. How do doctors behave when some (but not all) of their patients are in managed care? Journal of Health Economics. 2002;21(2):337–353. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- Goroll AH, Berenson RA, et al. Fundamental Reform of Payment for Adult Primary Care: Comprehensive Payment for Comprehensive Care. Journal of General Internal Medicine. 2007;22:410–415. doi: 10.1007/s11606-006-0083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottschalk A, Flocke SA. Time Spent in Face-to-Face Patient Care and Work Outside the Examination Room. Ann Fam Med. 2005;3(6):488–493. doi: 10.1370/afm.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groopman J. How Doctors Think. New York: Houghton Mifflin Company; 2007. [Google Scholar]
- Hall R. Queuing Methods for Services and Manufacturing. Englewood Cliffs, NJ: Prentice Hall; 1991. [Google Scholar]
- Hardin JW, Hilbe JM. Generalized Estimating Equations. Boca Raton, Fl: Chapman & Hall/CRC; 2002. [Google Scholar]
- Ko JM, Rodriguez HP, et al. Paying for Enhanced Service: Comparing Patients’ Experiences in a Concierge and General Medicine Practice. The Patient: Patient-Centered Outcomes Research. 2009;2(2):95–103. doi: 10.2165/01312067-200902020-00005. 110.2165/01312067-200902020-200900005. [DOI] [PubMed] [Google Scholar]
- Lin C, Albertson G, et al. Is patients’ perception of time spent with the physician a determinant of ambulatory patient satisfaction? Archives of Internal Medicine. 2001;161(11):1437–1442. doi: 10.1001/archinte.161.11.1437. [DOI] [PubMed] [Google Scholar]
- Majette GR. From Concierge Medicine to Patient-Centered Medical Homes: International Lessons & the Search for a Better Way to Deliver Primary Health Care in the U.S. American Journal of Law & Medicine. 2009;35(4):585–619. doi: 10.1177/009885880903500404. [DOI] [PubMed] [Google Scholar]
- McGuire TG, Pauly MV. Physician response to fee changes with multiple payers. Journal of Health Economics. 1991;10(4):385–410. doi: 10.1016/0167-6296(91)90022-f. [DOI] [PubMed] [Google Scholar]
- Murray M, Berwick D. Advanced access: reducing waiting and delays in primary care. JAMA. 2003;289(8):1035–1040. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- Murray M, Davies M, et al. Panel size: How many patients can one doctor manage? Family Practice Management. 2007;14(4):44–51. [PubMed] [Google Scholar]
- Murray M, Tantau C. Same-Day Appointments: Exploding the Access Paradigm. Family Practice Management. 2000;7(8):45–50. [PubMed] [Google Scholar]
- Reid RJ, Coleman K, et al. The Group Health Medical Home At Year Two: Cost Savings, Higher Patient Satisfaction, And Less Burnout For Providers. Health Aff. 2010;29(5):835–843. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- Reid RJ, Fishman PA, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care. 2009;15(9):e71–87. [PubMed] [Google Scholar]
- Roter D. Observation on methodological and measurement challenges in the assessment of communication during medical exchanges. Patient Educ Couns. 2003;50(1) doi: 10.1016/s0738-3991(03)00074-0. [DOI] [PubMed] [Google Scholar]
- Roter D, Hall J. Physician gender and patient-centered communication: a critical review of empirical research. Annual Review of Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- Roter DL, Hall JA, et al. Physician gender effects in medical communication: a meta-analytic review. Journal of American Medical Association. 2002;288(6):756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- Stange KC, Zyzanski SJ, et al. How valid are medical records and patient questionnaires for physician profiling and health services research? A comparison with direct observation of patients visits. Medical Care. 1998;36(6):851–867. doi: 10.1097/00005650-199806000-00009. [DOI] [PubMed] [Google Scholar]
- Tai-Seale M, McGuire T, et al. Time allocation in primary care office visits. Health Services Research. 2007;42(5):1871–1894. doi: 10.1111/j.1475-6773.2006.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Government Accountability Office. Physician Services: Concierge Care Characteristics and Considerations for Medicare : Report to Congressional Committees. Washington, D.C: U.S. Government Accountability Office; 2005. [Google Scholar]
- Virtanen P, Oksanen T, et al. Work stress and health in primary health care physicians and hospital physicians. Occupational and Environmental Medicine. 2007:1–9. doi: 10.1136/oem.2007.034793. [DOI] [PubMed] [Google Scholar]
- Waitzkin H. Information giving in medical care. Journal of Health and Social Behavior. 1985;26(2):81–101. [PubMed] [Google Scholar]
- Ware J, Kosinski M, et al. How to Score Version 2 of the SF-36 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]