Abstract
Purpose
To compare the effects of existing patient awareness of lens-related complications and underlying risk factors on actual patient behavior during contact lens wear and care practices in two different clinical study populations.
Methods
Established contact lens wearers (n=281) completed an anonymous written questionnaire upon presenting to their habitual eye care practitioner in the Dallas-Fort Worth (DFW) metroplex. Data were analyzed and compared against a second study population which was comprised of established contact lens wearers (n=152) who were sequentially evaluated following their routine contact lens examination at the University of Texas Southwestern Medical Center at Dallas, TX (UTSW). All patients were questioned regarding his or her lens care practices and knowledge of complications and risk factors associated with contact lens wear.
Results
58% of patients in the general community could identify by name a complication associated with lens wear compared to 91% within the medical center. The most frequent complications reported were related to comfort and handling (72%, DFW) and infection (47%, UTSW). The majority of patients could correctly identify risk factors associated with lens-related complications; awareness for topping-off solutions, tap water exposure, and hygiene varied between groups. Overall, 85% of patients perceived themselves as compliant with their lens wear and care practices. Using a standard scoring model to determine actual compliance, 2% of patients demonstrated good compliance; however, only 0.4% of patients were fully compliant with contact lens wear and care practices.
Conclusions
The data reveals some study bias in complication and risk awareness between populations; however, despite this limitation, a significant proportion of patients exhibited actual non-compliant behavior despite acknowledged awareness of risk. While most patients consider themselves to be complying with standard practitioner guidelines for lens wear and care practices, essentially all contact lens wearing patients exhibit behavioral non-compliance with resulting increased risk for significant complications.
Keywords: contact lenses, care solutions, lens storage case, compliance, complications
Introduction
Non-compliance with practitioner recommended contact lens wear and care regimens remains a persistent clinical problem. Historically, overall rates of non-compliance with contact lens wear are routinely cited in the literature as ranging from 40-91%.1-6 Areas of non-compliance currently under scrutiny include failure to adhere to recommended wear and replacement schedules,7-9 inadequate lens and lens storage case hygiene procedures10-18, and exposure to non-sterile water;17, 19 which has also been repeatedly identified as a significant risk factor for Acanthamoeba infection.20-22 Even with the high rates of non-compliance reported, the incidence of severe complications associated with contact lens wear is relatively low and has remained constant for more than three decades regardless of changes in lens materials and the introduction of daily disposables and no-rub care solutions.23-27 While there are no definitive studies linking non-compliant behavior with increased risk of lens-related complications, high levels of lens case contamination leading to heavy biofilm formation combined with the inappropriate use of currently available contact lens care solutions are inarguably suspect. In support of this view, a recent report evaluating the relationship between non-compliance and lens-related adverse events suggest a potential correlation with an increased incidence of contact lens-related complications evident among non-compliant lens wearers.8
Current strategies to improve compliance are limited. Patient education is paramount and has been the gold standard for decades. Recent findings however, suggest that recommendations amongst eye care practitioners are highly variable necessitating more effective practitioner educational programs to eliminate this ambiguity.28 Likewise, the ability to identify and correct non-compliant behavior is confounded by the fact that many patients are unaware that their behavior practices are non-compliant.1, 29 We recently investigated the relationship between patient compliance and awareness of risk factors associated with contact lens-related adverse events.30 Importantly, findings from that work suggested that awareness of risk did not influence patient compliance within our study population. One consideration when interpreting those early findings was the potential for study bias in ascertaining actual awareness levels among subjects within a university medical center. To confirm and extend those previous findings, in this study we investigated the relationship between compliance and awareness of risk associated with contact lens wear in the general community using an anonymous written questionnaire and compared these results with our earlier findings from direct patient interviews within a University-based medical setting.
Methods
Study Population
Two clinical populations were evaluated in this study. In the first population, anonymous self-reported questionnaires were mailed out to 200 randomly selected optometrists within the Dallas-Fort Worth (DFW) metroplex between June and August 2010. Optometrists were selected using a random number generator in Excel from an initial mailing list of 500 practitioners within the DFW metroplex. Optometrists were asked to distribute the questionnaires to 25 consecutive established contact lens wearers at check in prior to their examination. Office staff were excluded from participating. To maintain anonymity, optometrists were not asked to review or confirm any patient information following completion of the questionnaire. Questionnaires were returned via a self-addressed stamped envelope and each participating optometrist was asked to specify their type of practice with respect to a private, stand alone facility or a commercial/retail entity. 281 patients aged 18 and above from 17 different optometric practices participated in the study. For comparative analysis, a second population of patients seen in a university-affiliated health center used in a previously published study was also evaluated.30 In this latter study, patient interviews were performed between June and August 2009. Only data from patients 18 and up were included in this report. All participants who had worn contact lenses for less than one month or for therapeutic purposes were excluded from this study. Approval for this study was obtained through the Institutional Review Board at the University of Texas Southwestern Medical Center, Dallas, Texas.
Study Procedures
Participants were given an anonymous self-reported questionnaire and asked to complete twenty-two questions for information on their demographics, contact lens usage, care practices, perceived overall compliance, and their knowledge of contact lens-related complications. To determine perceived compliance, patients were asked the question: Do you think you are compliant with your contact lenses? To assess knowledge and history of contact-lens related complications, patients were first asked, on a scale from 1 to 5, with 1 being very uncommon to 5 being very common, to rate the occurrence of contact lens-related complications. Patients were subsequently asked whether they could name a contact lens-related complication and whether they had experienced a contact-lens related adverse event. To determine actual compliance, patients were questioned on their behavior practices, including method and frequency, using a forced choice design strategy. Actual compliance was ascertained using a compliance scoring model. To determine awareness of risk, patients were queried on ten behaviors routinely evaluated as critical factors in compliance as well as risk factors for contact lens-related adverse events1, 3, 6, 11, 18, 23, 27, 31-36 as to whether they increased, decreased, had no effect or were unsure of the effect on the risk of having a contact lens-related complication. Consecutive patients were questioned in both study populations to eliminate any selection bias. Participation was voluntary and those who did not complete the questionnaire were excluded.
Statistical Analysis
For the purpose of this study, perceived compliance was defined as whether or not the patient identified themselves as compliant with their contact lens care. Actual compliance was defined based upon a compliance score and was then grouped into one of three categories similar to a previous study by Morgan et al.35 As reported in a prior publication, the compliance score was calculated for the UTSW population using the number of positive behavior responses divided by the total number of behaviors analyzed.30 As comparisons were made between populations, only the 8 behaviors investigated in both data sets were included. A correct response was identified as “yes” or “no”, frequency of the behavior was not included in the initial phase of the study. In the DFW self-reported questionnaire, responses were assigned a score of 0, 1 or 2 depending if the response was considered non-compliant “0”, partially compliant “1” or fully compliant “2”. For both populations, sleeping in lenses was considered compliant only if the patient reported that extended wear had been prescribed by their eye care practitioner. A patient was considered to have good compliance when receiving a score of 90% or better. Average compliance was defined as receiving a score of 70 – 89% and poor compliance was defined as 69% or below. For univariate analysis, Chi-square or Fisher's exact tests were used to investigate if there were significant differences in categorical variables between groups such as risk factor awareness (does a factor increase, decrease, have no effect or are not sure on risk of having a contact lens-related complication) and patient behavior or perceived compliance and behavior. Analysis of these findings was completed using two levels of behavior (correct response noted as increased or decreased versus the incorrect response which included no effect and not sure). Student's t-tests were used to examine if there were significant differences in continuous variables between two groups (such as age and contact lens wearing years). Statistical significance was set at p<0.05.
Results
Demographics of both patient populations are listed in Table 1. There were 281 respondents from the DFW self-reported questionnaire group and 152 respondents included from the UTSW patient interview. Of the respondents from the DFW group, 258 (92%) were from private or stand alone practices. The remaining 8% (23 respondents) were from optometry clinics in retail settings. The educational profile of the DFW group consisted of 89 (32%) of respondents having completed 1-3 years of education past high school, 93 (33%) had completed 4-5 years of college, 56 (20%) had completed 6 or more years, while 34 (12%) had not received any education past high school. Three percent did not specify. Educational data was unavailable for the UTSW study population. There was no difference between gender or type of lens wear between groups. The majority of respondents were soft lens wearers; 2.8% reported wearing daily disposables. Lens material and modality of disposable lens wear (2-/4-week) was not included in this study. The DFW population was slightly younger (p<0.004) compared to UTSW and had correspondingly shorter years of lens wear experience (p<0.001).
Table 1. Wearer demographics.
| DFW n (%) |
UTSW n (%) |
|
|---|---|---|
| Gender | ||
| Male | 99 (35) | 51 (34) |
| Female | 182 (65) | 101 (66) |
| Age (years) | ||
| Mean ± SD | 36 ± 14 | 40 ± 14 |
| Range | 18 - 73 | 18 - 75 |
| Lens type | ||
| Soft | 246 (88) | 128 (84) |
| Rigid | 13 (5) | 22 (14) |
| Specialty | 1 (<1) | 2 (1) |
| Not specified | 21 (7) | NA |
| Lens wear experience | ||
| Mean ± SD | 15 ± 10 | 18 ± 12 |
| 0-2 | 15 (5) | 12 (8) |
| 3-5 | 38 (14) | 10 (7) |
| 6-10 | 80 (29) | 29 (19) |
| >10 | 143 (52) | 101 (66) |
There was a difference between the perceived frequency of contact lens-related complications between groups (p<0.001). Specifically, respondents within the UTSW group perceived lens-related complications to occur more frequently than DFW respondents. The responses are summarized in Table 2. Likewise, in the group that perceived lens-related complications as more common, a greater number of respondents were able to identify a complication by name (p<0.001). The predominant complications reported were related to comfort and handling issues and infection. The proportion of respondents identifying comfort and handling as a complication when compared to infection also varied between groups (p<0.001). Awareness of lens-related complications did not appear to be driven by past history, as there was no difference in the number of positive responses to having had a complication between groups (p=1.000).
Table 2. Past history and awareness.
| DFW n (%) |
UTSW n (%) |
p value | |
|---|---|---|---|
| How common are contact lens-related complications?* | |||
| 1 | 128 (47) | 34 (24) | |
| 2 | 81 (29) | 44 (24) | |
| 3 | 35 (13) | 56 (39) | |
| 4 | 9 (3) | 13 (9) | |
| 5 | 22 (8) | 6 (4) | |
| Mean score | 2.0 | 2.5 | <0.001 |
| Can you name a complication? | |||
| Yes | 160 (58) | 139 (91) | |
| No | 118 (42) | 13 (9) | <0.001 |
| If so, what? | |||
| Comfort & handling | 115 (72) | 50 (36) | |
| Infection | 31 (19) | 65 (47) | <0.001 |
| Have you had a complication? | |||
| Yes | 112 (41) | 63 (41) | |
| No | 161 (59) | 89 (59) | 0.909 |
| If so, what? | |||
| Comfort & handling | 70 (63) | 23 (37) | |
| Infection | 18 (16) | 18 (29) | 0.011 |
Grading scale: 1 = very uncommon; 5 = very common
The majority of patients expressed awareness of the risk associated with sleeping in lenses and replacing lenses less frequently than recommended by their eye care practitioners. When questioned about solution usage, differences were seen both between and within groups. Specifically, within the DFW group, there was a significant difference between respondents reporting awareness on the importance of always using fresh solution compared to respondents reporting awareness of the risk of topping off their solution in the lens case (p<0.001). Swimming or participating in water sports, tap water exposure and showering also indicated areas where awareness levels were not optimum, with only 2/3 of the study population associating swimming, water sports and tap water as risk factors for contact lens-related adverse events and an even lower number of respondents correctly identifying showering while wearing lenses. The findings are summarized in Table 3.
Table 3. Risk factor awareness.
| Risk Factor | DFW n (%) |
UTSW n (%) |
p value |
|---|---|---|---|
| Lens usage | |||
| Sleeping in lenses | 257 (92) | 141 (93) | 1.000 |
| Replacing less frequently than recommended | 225 (82) | 138 (91) | 0.098 |
| Solutions | |||
| Using fresh solution | 248 (90) | 149 (98) | 0.037 |
| Topping-off | 151 (54) | 145 (95) | <0.001 |
| Water exposure | |||
| Swim/water sports | 170 (62) | 106 (70) | 0.296 |
| Tap water | 200 (72) | 134 (88) | 0.008 |
| Showering | 102 (36) | NA | - |
| Lens case replacement | 228 (82) | 126 (83) | 1.000 |
| Hygiene | 250 (90) | 152 (100) | 0.004 |
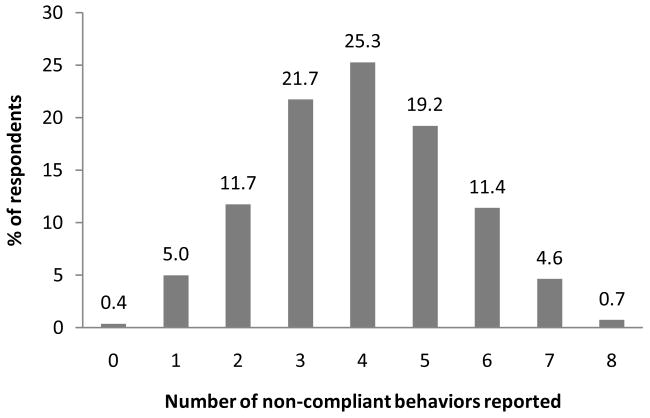
Similar to our previous report, the majority of patients in the metroplex described themselves as compliant with their contact lens wear and care practices (p=0.955 compared to UTSW), despite low levels of good compliance. A comparison of perceived compliance versus actual compliance for each population using a scoring model is detailed in Table 4. A distribution of the individual non-compliant behaviors performed is listed in Table 5. Water exposure was the most frequent non-compliant behavior reported. Not included in this list is showering while wearing lenses, which was reported to occur at variable frequency by 85% of lens wearers. Calculation of the number of wearers that performed one or more non-compliant behaviors is shown in Figure 1. The median number of actual non-compliant behaviors out of the eight behaviors evaluated was 4.
Table 4. Perceived versus actual compliance.
| DFW n (%) |
UTSW n (%) |
P value | |
|---|---|---|---|
| Perceived compliance | 0.955 | ||
| Yes | 237 (85) | 132 (86) | |
| No | 36 (13) | 21 (14) | |
| Not specified | 7 (3) | N/A | |
| Actual compliance | <0.001 | ||
| Good | 5 (2) | 15 (11) | |
| Average | 36 (13) | 80 (57) | |
| Poor | 240 (85) | 46 (33) |
Table 5. Non-compliant behavior.
| Non-compliant Behavior | DFW n (%) |
|---|---|
| Lens usage | |
| Sleeping in lenses | |
| Naps, once or less per week, once or more per week | 158 (56) |
| Lens replacement frequency | |
| Few extra days, a week or more longer than recommended | 146 (52) |
| Solutions | |
| Using fresh solution | |
| Never or occasionally re-use | 79 (28) |
| Topping-off | |
| Occasionally or every night | 118(42) |
| Water exposure | |
| Swim/water sports | |
| Occasionally or always | 181 (64) |
| Tap water | |
| All water exposure | 161 (57) |
| Lenses only | 25 (9) |
| Case only | 146 (52) |
| Lens storage case | |
| Replacement frequency | |
| Never or only if Dr. gives new case at yearly visit | 131 (47) |
| Hygiene | |
| Hand washing before handling lenses | |
| Never, occasionally or at least with water | 139 (49) |
Figure 1.
Frequency distribution of the number of non-compliant behaviors reported in the DFW population. Only the eight behaviors used in the determination of actual compliance have been included. The average contact lens wearer is compliant with 50% of the behaviors assessed in this study. Only 1 patient was fully compliant with all eight behaviors (n=281).
Discussion
The results from this study indicate that the overwhelming majority of contact lenses wearers demonstrate a reasonable level of knowledge with respect to compliance with practitioner recommended wear and care procedures. This was particularly evident with respect to overall lens usage, the importance of using fresh solution on a daily basis and regular lens case replacement; however, this study also revealed three areas where education outside a medical center population may be lacking: topping off solutions, tap water exposure and hygiene. All of these have been previously identified as modifiable risk factors for contact lens-related microbial keratitis.20-22, 26 The latter of the three, hygiene, while statistically significant is not likely clinically significant, as most patients acknowledged the need for and importance of hand washing before lens handling. Moreover, the difference between populations is likely reflective of care given in an institutional medical setting, where hand washing is consistently re-enforced in patient examination rooms and lavatories. The response to topping off solutions however, warrants future studies, particularly given that this behavior has been previously implicated as a key factor in a recent outbreak of contact lens-related fungal keratitis37, 38 and is currently listed on the FDA website as an important contact lens care warning to patients.39 This also indicates a huge disparity in the understanding and perception of lens care cleaning regimens, as 90% of patients indicated the significance of using fresh solution daily, but failed to recognize the importance of removing pre-existing solution prior to adding new.
Exposure to water during contact lens wear or during cleaning remains has been repeatedly indicated as a significant risk factor for Acanthamoeba infection.20-22 While historically the incidence of Acanthamoeba keratitis is relatively low during contact lens wear, these infections are often devastating and can result in substantial vision loss if not identified early and allowed to progress to stromal disease.40 In this study, water exposure was broken down into three categories which included swimming or participating in water sports while wearing lenses, the use of tap water for lens cleaning, and wearing lenses while showering. Showering while wearing lenses was recently implicated in the Chicago area Acanthamoeba outbreak following changes in municipal water disinfection standards.41 In this study, only one third of the patients queried correctly identified showering as a risk factor. While swimming and tap water scored much higher, only two thirds of the patients, regardless of study population, were able to correctly identify either as a risk factor for a contact lens-related adverse event.
Unlike risk factors that contribute to contact lens-related adverse events, the ability of patients to identify contact lens-related complications outside a medical center environment was not as strong. Within the medical center, 91% of patients stated they were able to identify a contact lens-related complication. In contrast to the medical center practice, a significantly fewer number of patients were able to identify a lens-related complication and of those that could, the majority of patients identified issues directly related to comfort and handling, with dryness being the most frequent response among this category. The difference in the ability of the two populations to identify complications appeared to be a bias that existed between these groups of patients. This bias was not directed by patient history, as there was no difference between the self-reported incidence of a complication for either group. This apparent bias between study populations is likely reflective of both an enriched population of medically-trained personnel, student trainees, and biomedical researchers, as well as a high number of patients with significant pathology due to the referral-based tertiary care nature of our clinic. This includes a high volume specialty lens practice for patients with pre-existing ocular disease and post-surgical lens requirements which may be subject to a higher rate of lens-related adverse events.
While there were marginal differences in the self-reported incidence of complications between the two groups, comfort and handling remained the most common for both, followed by infection. Although handling issues are not categorized clinically as a contact lens-related complication, respondents in both study groups perceived this as one. Likewise, the high self-reported incidence of infection in this study compared to the actual established incidence of culture proven microbial keratitis associated with lens wear is also likely due to patient perception as no diagnostic criteria were used to ascertain whether an event was a true infectious event. A more likely scenario involves a patient with a red, irritated eye that necessitated a clinical visit which may or may not have been directly related to lens wear and subsequently received some form of topical treatment. Regardless of the underlying etiology of the event, these were perceived by lens wearers as contact lens-related events and in this study, appeared to have no bearing on their subsequent behavior.
The second important finding in this study lies in the overall impression of both populations that they maintain good compliant practices, despite overwhelming low actual compliance scores. This observation was valid for both study populations examined. Significantly, approximately 85% of patients in both groups, when asked reported they were compliant with lens wear and care practices. When actual behavior was examined using a binary scale (yes or no), more than 10% of patients were identified that exhibited good levels of compliance.30 In contrast, when behavioral practices were stratified by frequency and/or methodology, the level of actual good compliance rapidly declined to 2%, which more closely approximates a recent study out of the UK demonstrating levels of compliance ranging from 0.3% for daily lens wear and 2.7% for extended wear.35 In terms of actual behaviors, water exposure was the most common behavior reported, followed by sleeping in lenses, stretching lenses longer than recommended, failing to wash hands or replace the lens case, and lastly, solution misuse. In this study 47% of patients reported never replacing their lens case or only replacing their case if given a new case by their eye care practitioner at their yearly visit. This finding is also in close agreement with a recent study on lens storage case compliance which found that 48% of patients reported replacing their lenses cases annually or longer.10
While organisms cultured from the cornea during an active microbial keratitis are often also recovered from the lens storage case, the clinical significance of regular case replacement in reducing the incidence of contact lens-related adverse events has not yet been established. Previous studies have shown that up to 81% of lens storage cases are contaminated and age of the lens case has been identified as a predisposing factor in microbial contamination with cases 9 months or older have the highest rate of contamination.12, 42-45 This is in agreement with studies in our laboratory that support that lens storage cases 9 months or older have high levels of protein and cellular debris which form a scaffold that enhances Pseudomonas aeruginosa adherence and subsequent biofilm formation (unpublished data). Biofilm formation in the lens storage case presents challenges, as currently available multipurpose solutions have reduced efficacy against heavier, mature biofilms in lens storage cases.44, 46, 47 While we did not assess cleaning regimens in this study, the need for practitioners to begin educating their patients on the need for lens case replacement appears paramount and should be reinforced at each follow-up visit.
A recent report by Dumbleton et al.8 suggests that a relationship exists between poor compliance with contact lens wear and care regimens and contact lens-related complications. In this study, when we assessed the frequency of non-compliant behaviors performed by patients, the average contact lens wearer only performed 50% of the recommended behaviors and only 1 patient was fully compliant, indicating a compliance rate of 0.4% in the population. This number is lower than the 2% reported in our scoring model, but it must clarified that the scoring model which assigned a score of 0, 1 or 2 points depending on the frequency of the behavior, considered a score of 90% and above to be compliant which accounts for this disparity. Given the overwhelming majority of patients that correctly identified risk factors, a compliance rate of 0.4% indicates that awareness of risk alone is not a driving factor establishing compliant behavior.
One of the primary limitations in this study is the small sample size. While a large number of practitioners were invited to participate, despite follow-up by the study coordinator, only 17 practitioners returned completed questionnaires. The randomized method of practitioner selection which encompassed a relatively large area was used to minimize any selection bias. Regardless of a relatively small sample size, there were detectable differences in overall patient knowledge of complications and risk awareness between the two populations evaluated. In agreement with our previous study however,30 there remained a significant proportion of patients that exhibited non-compliant behavior despite awareness of risk. While most patients considered themselves to be compliant with lens wear and care practices, essentially all contact lens wearing patients exhibited some level of non-compliance. This study identifies potential areas that may benefit from increased patient education; however, while education alone may stimulate a short term improvement in compliance, it is not likely to significantly sustain behavior in the long term.11, 48, 49 Non-compliant behavior continues to hinder efforts to maximize contact lens safety. New strategies and approaches to effectively modify inherent patient non-compliance are urgently needed.
Acknowledgments
This study was presented as a paper at the American Academy of Optometry Annual Meeting, November 17-20, 2010 in San Francisco, California.
Supported in Part by NIH Grant R01 EY018219 (DMR), NEI Core Grant EY020799, OneSight Research Foundation, Dallas, Texas (DMR), and a Career Development Award (DMR) and an unrestricted grant from Research to Prevent Blindness, Inc., New York, New York.
Footnotes
CR: none
References
- 1.Collins MJ, Carney LG. Patient compliance and its influence on contact lens wearing problems. Am J Optom Physiol Opt. 1986;63:952–956. doi: 10.1097/00006324-198612000-00004. [DOI] [PubMed] [Google Scholar]
- 2.De Oliveira PR, Temporini-Nastari ER, Alves MR, Kara-Jose N. Self-evaluation of contact lens wearing and care by college students and health care workers. Eye Contact Lens. 2003;29:164–167. doi: 10.1097/01.ICL.0000072829.76899.B5. [DOI] [PubMed] [Google Scholar]
- 3.Claydon BE, Efron N. Non-compliance in contact lens wear. Ophthalmic Physiol Opt. 1994;14:356–364. [PubMed] [Google Scholar]
- 4.Donshik PC, Ehlers WH, Anderson LD, Suchecki JK. Strategies to better engage, educate, and empower patient compliance and safe lens wear: compliance: what we know, what we do not know, and what we need to know. Eye Contact Lens. 2007;33:430–433. doi: 10.1097/ICL.0b013e318157f62a. [DOI] [PubMed] [Google Scholar]
- 5.Efron N. The truth about compliance. Cont Lens Anterior Eye. 1997;20:79–86. doi: 10.1016/s1367-0484(97)80002-1. [DOI] [PubMed] [Google Scholar]
- 6.Sokol JL, Mier MG, Bloom S, Asbell PA. A study of patient compliance in a contact lens wearing population. CLAO J. 1990;16:209–213. [PubMed] [Google Scholar]
- 7.Dumbleton K, Woods C, Jones L, Fonn D, Sarwer DB. Patient and practitioner compliance with silicone hydrogel and daily disposable lens replacement in the United States. Eye Contact Lens. 2009;35:164–171. doi: 10.1097/ICL.0b013e3181ac4a8d. [DOI] [PubMed] [Google Scholar]
- 8.Dumbleton KA, Richter D, Woods CA, Jones LW, Fonn D. Relationship between compliance with lens replacement and contact lens-related problems in silicone hydrogel wearers. Cont Lens Anterior Eye. 2011 Apr 12; doi: 10.1016/j.clae.2011.03.001. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Dumbleton K, Richter D, Woods C, Jones L, Fonn D. Compliance with contact lens replacement in Canada and the United States. Optom Vis Sci. 2010;87:131–139. doi: 10.1097/OPX.0b013e3181ca32dc. [DOI] [PubMed] [Google Scholar]
- 10.Hickson-Curran S, Chalmers RL, Riley C. Patient attitudes and behavior regarding hygiene and replacement of soft contact lenses and storage cases. Cont Lens Anterior Eye. 2011 Jan 10; doi: 10.1016/j.clae.2010.12.005. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.Yung AM, Boost MV, Cho P, Yap M. The effect of a compliance enhancement strategy (self-review) on the level of lens care compliance and contamination of contact lenses and lens care accessories. Clin Exp Optom. 2007;90:190–202. doi: 10.1111/j.1444-0938.2007.00147.x. [DOI] [PubMed] [Google Scholar]
- 12.Wu YT, Zhu H, Harmis NY, Iskandar SY, Willcox M, Stapleton F. Profile and frequency of microbial contamination of contact lens cases. Optom Vis Sci. 2010 Jan 22; doi: 10.1097/OPX.0b013e3181cf86ee. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Wu YT, Zhu H, Willcox M, Stapleton F. Impact of air-drying lens cases in various locations and positions. Optom Vis Sci. 2010;87:465–468. doi: 10.1097/OPX.0b013e3181e172a1. [DOI] [PubMed] [Google Scholar]
- 14.Wu YT, Zhu H, Willcox M, Stapleton F. The effectiveness of various cleaning regimens and current guidelines in contact lens case biofilm removal. Invest Ophthalmol Vis Sci. 2011 April 7; doi: 10.1167/iovs.10-6785. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Wu YT, Zhu H, Willcox M, Stapleton F. Removal of biofilm from contact lens storage cases. Invest Ophthalmol Vis Sci. 2010;51:6329–6333. doi: 10.1167/iovs.10-5796. [DOI] [PubMed] [Google Scholar]
- 16.Pens CJ, da Costa M, Fadanelli C, Caumo K, Rott M. Acanthamoeba spp. and bacterial contamination in contact lens storage cases and the relationship to user profiles. Parasitol Res. 2008;103:1241–1245. doi: 10.1007/s00436-008-1120-3. [DOI] [PubMed] [Google Scholar]
- 17.Bowden T, Nosch DS, Harknett T. Contact lens profile: a tale of two countries. Cont Lens Anterior Eye. 2009;32:273–282. doi: 10.1016/j.clae.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Wu YT, Carnt N, Stapleton F. Contact lens user profile, attitudes and level of compliance to lens care. Cont Lens Anterior Eye. 2010;33:183–188. doi: 10.1016/j.clae.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Wu YT, Tran J, Truong M, Harmis N, Zhu H, Stapleton F. Do swimming goggles limit microbial contamination of contact lenses? Optom Vis Sci. 2011;88:456–460. doi: 10.1097/OPX.0b013e31820f15a6. [DOI] [PubMed] [Google Scholar]
- 20.Radford CF, Minassian DC, Dart JK. Acanthamoeba keratitis in England and Wales: incidence, outcome, and risk factors. Br J Ophthalmol. 2002;86:536–542. doi: 10.1136/bjo.86.5.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thebpatiphat N, Hammersmith KM, Rocha FN, Rapuano CJ, Ayres BD, Laibson PR, Eagle RC, Cohen EJ. Acanthamoeba keratitis: a parasite on the rise. Cornea. 2007;26:701–706. doi: 10.1097/ICO.0b013e31805b7e63. [DOI] [PubMed] [Google Scholar]
- 22.Joslin CE, Tu EY, Shoff M, Booton GC, Fuerst PA, McMahon TT, Anderson RJ, Dworkin MS, Sugar J, Davis FG, Stayner LT. The association of contact lens solution use and Acanthamoeba keratitis. Am J Ophthalmol. 2007;144:169–180. doi: 10.1016/j.ajo.2007.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dart JKG, Radford CF, Misassian D, Verma S, Stapleton F. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology. 2008;115:1647–1654. doi: 10.1016/j.ophtha.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Schein OD, Glynn RJ, Poggio EC, Seddon JM, Kenyon KR. The relative risk of ulcerative keratitis among users of daily-wear and extended-wear soft contact lenses. A case-control study. Microbial keratitis study group. N Engl J Med. 1989;321:773–778. doi: 10.1056/NEJM198909213211201. [DOI] [PubMed] [Google Scholar]
- 25.Poggio EC, Glynn RJ, Schein OD, Seddon JM, Shannon MJ, Scardino VA, Kenyon KR. The incidence of ulcerative keratitis among users of daily-wear and extended-wear soft contact lenses. N Engl J Med. 1989;321:779–783. doi: 10.1056/NEJM198909213211202. [DOI] [PubMed] [Google Scholar]
- 26.Radford CF, Misassian D, Dart JKG, Stapleton F, Verma S. Risk factors for nonulcerative contact lens complications in an ophthalmic accident and emergency department: a case-control study. Ophthalmology. 2009;116:385–392. doi: 10.1016/j.ophtha.2008.09.053. [DOI] [PubMed] [Google Scholar]
- 27.Stapleton F, Keay L, Edwards K, Naduvilath T, Dart JKG, Brian G, Holden BA. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115:1655–1662. doi: 10.1016/j.ophtha.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Wu YT, Carnt N, Willcox M, Stapleton F. Contact lens and lens storage case cleaning instructions: whose advice should we follow? Eye Contact Lens. 2010;36:68–72. doi: 10.1097/ICL.0b013e3181cf8aff. [DOI] [PubMed] [Google Scholar]
- 29.Koetting RA, Castellano CF, Wartmann R. Patient compliance with EW instructions. Contact Lens Spect. 1986;1:23–30. [Google Scholar]
- 30.Bui TH, Cavanagh HD, Robertson DM. Patient compliance during contact lens wear: perceptions, awareness, and behavior. Eye Contact Lens. 2010;36:334–339. doi: 10.1097/ICL.0b013e3181f579f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saw SM, Ooi PL, Tan DT, Khor WB, Fong CW, Lim J, CU HY, Heng D, Chew SK, Aung T, Tan AL, Chan CL, Ting S, Tambyah PA, Wong TY. Risk factors for contact lens-related fusarium keratitis: a case-control study in Singapore. Arch Ophthalmol. 2007;125:611–617. doi: 10.1001/archopht.125.5.611. [DOI] [PubMed] [Google Scholar]
- 32.Radford CF, Minassian D, Dart JKG, Stapleton F, Verma S. Risk factors for nonulcerative contact lens complications in an ophthalmic accident and emergency department. Ophthalmology. 2009;116:385–392. doi: 10.1016/j.ophtha.2008.09.053. [DOI] [PubMed] [Google Scholar]
- 33.Donshik PC, Ehlers WH, Anderson LD, Suchecki JK. Strategies to better engage, educate, and empower patient compliance and safe lens wear: compliance: what we know, what we do not know, and what we need to know. Eye & Contact Lens. 2007;33:430–433. doi: 10.1097/ICL.0b013e318157f62a. [DOI] [PubMed] [Google Scholar]
- 34.Claydon BE, Efron N. Non-compliance in contact lens wear. Ophthal Physiol Opt. 1994;14(4):356–364. [PubMed] [Google Scholar]
- 35.Morgan PB. Contact lens compliance and reducing the risk of keratitis. Optician. 2007:20–25. [Google Scholar]
- 36.Radford CF, Woodward EG, Stapleton F. Contact lens hygiene compliance in a university population. J Br Contact Lens Assoc. 1993;16:105–111. [Google Scholar]
- 37.Levy B. Risk factors for contact lens related Fusarium keratitis. Arch Ophthalmol. 2007;125:1715–1716. doi: 10.1001/archopht.125.12.1715. [DOI] [PubMed] [Google Scholar]
- 38.Chang DC, Grant GB, O'Donnell K, Wannemuehler KA, Noble-Wang J, Rao CY, Jacobson LM, Crowell CS, Sneed RS, Lewis FMT, Schaffzin JK, Kainer MA, Genese CA, Alfonso EC, Jones DB, Srinivasan A, Fridkin SK, Park BJ. Multistate outbreak of Fusarium keratitis associated with use of a contact lens solution. J Am Med Assoc. 2006;296:953–963. doi: 10.1001/jama.296.8.953. [DOI] [PubMed] [Google Scholar]
- 39.American Optometric Association. What you need to know about contact lens hygiene and compliance. [Accessed May 26, 2011]; Available at: http://www.fda.gov/medicaldevices/productsandmedicalprocedures/homehealthandconsumer/consumerproducts/contactlenses/default.htm.
- 40.Robertson DM, McCulley JP, Cavanagh HD. Severe acanthamoeba keratitis after overnight orthokeratology. Eye Contact Lens. 2007;33:121–123. doi: 10.1097/01.icl.0000244110.70378.8c. [DOI] [PubMed] [Google Scholar]
- 41.Joslin CE, Tu EY, McMahon TT, Passaro DJ, S LT, Sugar J. Epidemiological characteristics of a Chicago-area Acanthamoeba keratitis outbreak. Am J Ophthalmol. 2006;142:212–217. doi: 10.1016/j.ajo.2006.04.034. [DOI] [PubMed] [Google Scholar]
- 42.Willcox M, Carnt N, Diec J, Naduvilath T, Evans V, Stapleton F, Iskandar S, Harmis N, de la Jara PL, Holden BA. Contact lens case contaminatino during daily wear of silicone hydrogels. Optom Vis Sci. 2010;87:456–464. doi: 10.1097/OPX.0b013e3181e19eda. [DOI] [PubMed] [Google Scholar]
- 43.Gray TB, Cursons RTM, Sherwan JF, Rose PR. Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases. Br J Ophthalmol. 1995;79:601–605. doi: 10.1136/bjo.79.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson LA, Sawant AD, Simmons RB, Ahearn DG. Microbial contamination of contact lens storage cases and solutions. Am J Ophthalmol. 1990;110:193–198. doi: 10.1016/s0002-9394(14)76991-0. [DOI] [PubMed] [Google Scholar]
- 45.Devonshire P, Munro FA, Abernethy C, Clark BJ. Microbial contamination of contact lens cases in the west of Scotland. Br J Ophthalmol. 1993;77:41–45. doi: 10.1136/bjo.77.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Szczotka-Flynn LB, Imamura Y, Chandra J, Yu C, Mukherjee PK, Pearlman E, Ghannoum MA. Increased resistance of contact lens-related bacterial biofilms to antimicrobial activity of soft contact lens care solutions. Cornea. 2009;28:918–926. doi: 10.1097/ICO.0b013e3181a81835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilson LA, Sawant AD, Ahearn DG. Comparative efficacies of soft contact lens disinfectant solutions against microbial films in lens cases. Arch Ophthalmol. 1991;109:1155–1157. doi: 10.1001/archopht.1991.01080080115043. [DOI] [PubMed] [Google Scholar]
- 48.Claydon BE, Efron N, Woods C. A prospective study of the effect of education on non-compliant behaviour in contact lens wear. Ophthalmic and Physiol Opt. 1997;17:137–146. [PubMed] [Google Scholar]
- 49.Cardona G, Lloveet I. Compliance amongst contact lens wearers: comprehension skills and reinforcement with written instrucutions. Cont Lens Anterior Eye. 2004;27:75–81. doi: 10.1016/j.clae.2004.02.005. [DOI] [PubMed] [Google Scholar]