Abstract
Introduction:
Little is known about the influence of prepartum menthol cigarette use on postpartum smoking abstinence or how race/ethnicity might moderate this relationship. The current study addressed that gap by testing these relationships among racially/ethnically diverse women who quit smoking during pregnancy (N = 244; 33% African American, 31% Latina, 36% White).
Methods:
Continuation ratio logit models were used to examine the effects of prepartum menthol cigarette use on biochemically confirmed, continuous abstinence through 26 weeks postpartum using an intent-to-treat approach. Analyses controlled for age, race/ethnicity, partner status, income, education, treatment, number of prequit cigarettes smoked per day, time to the first cigarette of the day, and time (Week 8 or 26 data collection timepoint). An additional model tested the moderating effects of race/ethnicity by including an interaction term.
Results:
Prepartum menthol cigarette use was not significantly associated with postpartum smoking abstinence in the overall sample. However, the interaction between menthol use and race/ethnicity was significant (p = .02). Among White women, menthol use was associated with significantly lower odds of maintaining postpartum smoking abstinence (p = .03; odds ratio = .19 [.04–.89]), and the effect approached significance among African American women (p = .08).
Conclusions:
This study provides the first evidence that prepartum menthol cigarette use may increase the risk of postpartum smoking relapse among White, and possibly African American, women who quit smoking during or immediately before pregnancy. Results suggest that White and African American prepartum menthol users may require different or more intensive cessation services to aid in the maintenance of postpartum smoking abstinence. Replication with larger samples, and a focus on understanding the mechanisms that underlie these relationships, are warranted.
Introduction
Although the Family Smoking Prevention Tobacco Control Act (Act HR 1256, 2009) banned the use of flavorings in cigarettes, mentholated cigarettes were excluded from this ban due to the need for more research about their impact, relative to non-mentholated cigarettes, on smoking and quitting behaviors. Researchers have suggested that menthol cigarettes may be more addictive than non-menthol cigarettes, that menthol cigarette users may have a more difficult time quitting smoking, and that (because of the higher rates of menthol cigarette use among racial/ethnic minority smokers) this may be a contributor to racial/ethnic smoking-related health disparities (Ahijevych & Garrett, 2004; Clark, Gardiner, Djordjevic, Leischow, & Robinson, 2004; Gardiner & Clark, 2010; Healton et al., 2010; Okuyemi et al., 2003; Williams et al., 2007). A number of studies have investigated the relationship between menthol use and smoking cessation, and the moderating effects of race/ethnicity on that relationship, with mixed results (Foulds, Hooper, Pletcher, & Okuyemi, 2010; Fu et al., 2008; Gandhi, Foulds, Steinberg, Lu, & Williams, 2009; Gundersen, Delnevo, & Wackowski, 2009; Hyland, Garten, Giovino, & Cummings, 2002; Muscat, Richie, & Stellman, 2002; Okuyemi, Faseru, Sanderson Cox, Bronars, & Ahluwalia, 2007; Okuyemi, Lawrence, Hammons, & Alexander, 2010; Pletcher et al., 2006; Stahre, Okuyemi, Joseph, & Fu, 2010; Trinidad, Perez-Stable, Messer, White, & Pierce, 2010). To our knowledge, however, no previous studies have examined the effect of menthol cigarette use on postpartum smoking relapse among women who quit smoking during or immediately prior to pregnancy.
The purpose of this study was to examine the effects of prepartum menthol cigarette use on the maintenance of continuous abstinence through 26 weeks postpartum among pregnant women who quit smoking because of their pregnancy, and to examine whether effects were moderated by race/ethnicity. Participants were racially/ethnically diverse, predominantly low-income women who spontaneously quit smoking prior to the 33rd week of pregnancy.
Methods
Participants
Data were collected as part of a randomized clinical trial evaluating the efficacy of a Motivation and Problem Solving (MAPS) treatment for the prevention of postpartum relapse (Reitzel et al., 2010; Vidrine, Reitzel, Velasquez, Mazas, Cinciripini, & Wetter, 2011). Women were eligible to participate if they were English speaking, in their 30th to 33rd week of pregnancy at the time of study enrollment, ≥18 years old, self-reported smoking ≥1 cigarette daily for the year prior to pregnancy, and stopped smoking either during their pregnancy or within 2 months prior to becoming pregnant. Women reporting a high-risk pregnancy were excluded. The parent project used proactive recruitment strategies including newspaper, radio, bus, and clinic advertisements to enroll 251 participants from Houston, TX, between October 2004 and April 2008. Recruitment and flow through the study are detailed elsewhere (Reitzel et al., 2010).
Procedures
The University of Texas MD Anderson Cancer Center Institutional Review Board approved this study. Written informed consent was obtained before data collection. Participants attended three in-person assessment visits (baseline [30–33 weeks pregnant] and weeks 8 and 26 postpartum). Participants were randomized by computer into Usual Care (n = 115), MAPS (n = 68), or MAPS+ (n = 68) following the baseline visit. All participants were given self-help materials and 5–10 min of Guideline-based brief relapse prevention advice (Fiore, Jaen, & Baker, 2008). The MAPS and MAPS+ groups also received six telephone-based counseling sessions, and the MAPS+ group received two additional in-person counseling sessions.
Measures
Questionnaires were administered and completed via computer. Data collection was completed by January 2009. Variables of interest are below.
Demographics
Demographics collected at baseline included participant age, race/ethnicity (African American, Latina, White, Other), partner status (single/widowed/divorced vs. married/living with partner), income (<$20,000/year vs. ≥$20,000/year annual household income), and educational achievement (<high school/General Equivalency Degree [GED] vs. ≥high school/GED). The only variable with missing data was income (n = 27 missing). Missing data were maintained in adjusted analyses. Also, too few participants endorsed the “Other” race/ethnicity for inclusion as a separate category (n = 5), so these women were dropped from the present sample prior to analysis.
Prequit Smoking Characteristics
Prequit smoking characteristics collected at baseline included menthol use status, the number of cigarettes smoked per day, and time to the first cigarette of the day (≤5 min or ≥5 min). Menthol use status was assessed by a single item asking if participant's regular brand of cigarettes was menthol or non-menthol. Results yielded a binary predictor variable (non-menthol vs. menthol; reference group = non-menthol). Two participants did not answer this item, and missing values were maintained in analyses.
Smoking Abstinence
Continuous abstinence from smoking, defined as no smoking since the delivery date, was assessed at weeks 8 and 26 postpartum via self-report and was biochemically verified through expired carbon monoxide levels (CO) <10 ppm (Hajek et al., 2001) and/or a cotinine value of <20 ng/ml (McBride et al., 1999). Cotinine, collected in a saliva sample by mail, was used if a participant had relocated and was unable to return to the clinic for a CO assessment (n = 8 at Week 8 and n = 11 at Week 26). The percentage of participants with missing smoking status was 21% at Week 8 and 28% at Week 26. An intention-to-treat procedure was followed, whereby those lost to follow-up were considered relapsed. Because the focus was on continuous abstinence, relapse at Week 8 automatically resulted in classification as relapsed at Week 26.
Data Analysis
Analyses were performed using SAS v. 9.2 (SAS Institute, Cary, NC). Preliminary analyses explored differences in demographic and smoking characteristics by menthol use status using chi-square tests for categorical variables and analyses of variance for continuous variables. Primary analyses examined the effect of menthol use on continuous abstinence from smoking through 26 weeks postpartum using continuation ratio (CR) logit models (PROC GENMOD; Agresti, 2002; Bender & Benner, 2000; McGowan, 2000). The CR logit models operate by modeling the conditional probability of being abstinent at the current assessment point given that a participant has been abstinent through the most recent assessment point. Model 1 tested the unadjusted relationship between menthol use status and continuous smoking abstinence. Model 2 tested the adjusted relationship between menthol use status and continuous smoking abstinence by including age, race/ethnicity, partner status, income, education, the number of prequit cigarettes smoked per day, and the time to the first cigarette of the day. Model 3 tested the interaction of menthol use status and race/ethnicity by additionally including the interaction term in the adjusted model. All models additionally controlled for treatment group and time.
Secondary analyses were also conducted to ensure that any effects resulting from the primary analyses were resilient to the inclusion of the 27 participants who declined to provide data on their income. This was accomplished by assigning those with missing income data to a “refused to answer” income category so that their data would be maintained in adjusted analyses (see Ko et al., 2010; Quach et al., 2011 for precedent) and re-running the analyses described above.
Results
Participant Characteristics
Participants (N = 244) were racially/ethnically diverse (33% African American, 31% Latina, 36% White) women with an average age of 25 years (Table 1). The sample was almost evenly divided by menthol use status (menthol users n = 123, non-menthol users n = 121). Participant characteristics by menthol use status are in Table 1. Menthol users were significantly younger than non-menthol users and smoked fewer cigarettes per day. There were also significant differences between menthol and non-menthol users by race/ethnicity, partner status, income, and educational achievement.
Table 1.
Participant Characteristics by Menthol Use Status
| Covariates/outcome | Menthol (n = 123) | Non-Menthol (n = 121) | Total (N = 244) | p Value |
| M (SD)/n (%) | M (SD)/n (%) | M (SD)/n (%) | ||
| Age | 23.6 (4.6) | 25.7 (5.8) | 24.6 (5.3) | .002 |
| Race/ethnicity | <.001 | |||
| African American | 70 (56.9) | 11 (9.1) | 81 (33.2) | |
| Latina | 33 (26.8) | 42 (34.7) | 75 (30.7) | |
| White | 20 (16.3) | 68 (56.2) | 88 (36.1) | |
| Partner status | .008 | |||
| Single/divorced/widowed | 57 (46.3) | 36 (29.8) | 93 (38.1) | |
| Married/living with partner | 66 (53.7) | 85 (70.2) | 151 (61.9) | |
| Annual household income | .002 | |||
| <$20,000/year | 48 (44.0) | 26 (24.1) | 74 (34.1) | |
| ≥$20,000/year | 61 (56.0) | 82 (75.9) | 143 (65.9) | |
| Educational achievement | .037 | |||
| <High school/GED | 29 (23.6) | 16 (13.2) | 45 (18.4) | |
| ≥High school/GED | 94 (76.4) | 105 (86.8) | 199 (81.6) | |
| Cigarettes per day | 9.2 (6.8) | 11.2 (8.4) | 10.2 (7.7) | .045 |
| Time to first cigarette | .051 | |||
| ≥5 min | 90 (73.2) | 101 (83.5) | 191 (78.3) | |
| ≤5 min | 33 (26.8) | 20 (16.5) | 53 (21.7) | |
Note. GED = General Equivalency Degree. Analyses of variance or chi-square tests were used to evaluate significant differences.
Primary Analyses
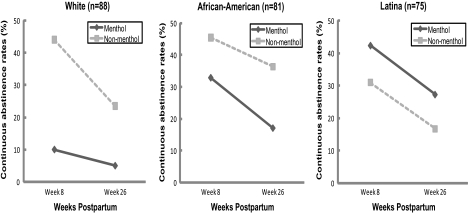
Menthol users had nonsignificantly lower rates of continuous abstinence than non-menthol users at both follow-up points. Longitudinal analyses indicated that menthol cigarette use did not significantly predict continuous abstinence from smoking through 26 weeks postpartum in analyses adjusted for treatment group and time (Model 1: β = −.24, SE = .23; χ2 = 1.05; p = .31; n [number of observations] = 331) or in analyses adjusted for age, race/ethnicity, partner status, income, and education, treatment group, cigarettes smoked per day, time to the first cigarette of the day, and time (Model 2: β = −.32, SE = .30; χ2 = 1.12; p = .29; n = 297). However, the menthol use status by race/ethnicity interaction was significant (Model 3: β = −.59, SE = .34; χ2 = 7.93; p = .02; n = 297). Follow-up racial/ethnic specific subgroup analyses indicated that menthol use status predicted abstinence among White women in adjusted analyses (β = −1.62, SE = .76; χ2 = 4.49; p = .03; n = 108, odds ratio = .19 [.04−.89]). White menthol users were less likely to maintain continuous abstinence than White non-menthol users. The relationships between menthol use and continuous smoking abstinence were not significant among the other racial/ethnic subgroups in adjusted analyses, although it approached significance among African Americans (African American: [β = −1.12, SE = .64; χ2 = 3.06; p = .08; n = 96]; Latina: [β = .46, SE = .50; χ2 = .86; p = .35; n = 93]). Specifically, there was a nonsignificant trend for African American menthol users to be less likely to maintain continuous abstinence than African American non-menthol users. Unadjusted continuous abstinence rates by menthol cigarette use status for each racial/ethnic group are displayed in Figure 1. Secondary analyses indicated that results were largely unchanged when missingness on income data was accounted for with the addition of a “refused to answer” category (Model 2: β = −.28, SE = .29; χ2 = .91; p = .34; n = 331; Model 3: β = −.56, SE = .33; χ2 = 9.07; p = .01; n = 331).
Figure 1.
Unadjusted continuous abstinence rates over time by menthol use status for White, African American, and Latina participants.
Discussion
This study was the first to examine the effect of prepartum menthol cigarette use on postpartum smoking abstinence. Results did not support a main effect of menthol use on cessation but did support a racial/ethnic interaction effect whereby White menthol users were less likely to maintain continuous postpartum smoking abstinence than were White non-menthol users. Specifically, abstinence rates were over 4 times as high at both follow-up assessments for White non-menthol versus White menthol users. The lack of a main effect of menthol use on cessation is consistent with a number of studies conducted among nonpregnant smokers (e.g., Fu et al., 2008; Hyland et al., 2002; Muscat et al., 2002). The significant relationship between menthol use and postpartum smoking relapse among White women in this sample was surprising, however, given that most previous studies found that the effect of menthol use on cessation was more salient among racial minority groups (e.g., Foulds et al., 2010; Gandhi et al., 2009; Gundersen et al., 2009; Stahre et al., 2010). However, it is notable that the effect of menthol use status on abstinence approached significance among the African American women in this sample. In this case, abstinence rates diverged over time between the groups and were over twice as high at Week 26 for Black non-menthol versus Black menthol users. Results suggest that White, and possibly African American, prepartum menthol users may require different or more intensive cessation services to aid in the maintenance of postpartum smoking abstinence. However, because some cell sizes in the interaction analyses were small (i.e., n = 20 White menthol users) and due to uneven distribution of non-menthol smokers within racial/ethnic subgroups (e.g., n = 70 among Whites vs n = 11 among African Americans), these results should be replicated with larger samples. In addition, research focused on the mechanisms underlying the relationship between prepartum menthol use and postpartum smoking relapse is needed to better understand racial/ethnic differences and to better inform treatment.
It was also interesting to note that, unlike the White and African American menthol users who had lower rates of continuous abstinence than their non-menthol using counterparts, Latina menthol users had nonsignificantly higher rates of continuous abstinence than Latina non-menthol users. This pattern is in need of replication but suggests that future studies should examine racial/ethnic interactions or conduct racial/ethnic subgroup analyses when examining the effects of prepartum menthol use on postpartum relapse.
Limitations of this study include the uneven distribution of menthol and non-menthol smokers among the African American and White participants. Future studies in this area might include equal proportions of menthol and non-menthol users within each racial/ethnic group. An additional limitation is that participants were treatment seeking and self-referred. Therefore, results may not generalize to nontreatment seeking pregnant/postpartum women or to pregnant/postpartum women who do not volunteer for relapse prevention studies. In this study, smokers had quit by the time of enrollment (30th to 33rd week of pregnancy). Therefore, results may not generalize to women who quit later in their pregnancies or postpartum. Participants were residents of the Houston, TX, metropolitan area and results may not generalize to pregnant/postpartum women from other locations, including rural areas. Finally, although analyses adjusted for several potential confounders, the degree to which the presence of unknown and unmeasured confounders might have influenced these results is unknown.
In conclusion, to our knowledge, this was the first study examining the effects of prepartum menthol use on postpartum smoking relapse. Although menthol use did not predict relapse among the racially/ethnically diverse sample of women as a whole, significant effects were found among the subgroup of White women. Results add to the literature that will inform the future legislative actions stemming from Act HR 1256 and are in need of future replication.
Funding
This work was supported by grants from the National Cancer Institute (R01CA89350 to D.W.W.), the Center for Tobacco Products of the Food and Drug Administration (to L.R.R.), and the National Institutes of Health through MD Anderson's Cancer Center Support Grant (CA016672). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Food and Drug Administration or any of the other project supporters.
Declaration of Interests
Authors would like to report that P. M. Cinciripini has served on the scientific advisory board of Pfizer Pharmaceuticals and has conducted educational talks sponsored by Pfizer on smoking cessation for physicians within the last 3 years.
References
- Agresti A. Categorical data analysis. 2nd ed. Hoboken, NJ: John Wiley & Sons, Inc; 2002. doi:10.2307/1269816. [Google Scholar]
- Ahijevych K, Garrett BE. Menthol pharmacology and its potential impact on cigarette smoking behavior. Nicotine & Tobacco Research. 2004;6(Suppl. 1):S17–S28. doi: 10.1080/14622200310001649469. doi:10.1080/14622200310001649469. [DOI] [PubMed] [Google Scholar]
- Bender R, Benner A. Calculating ordinal regression models in SAS and S-Plus. Biometrical Journal. 2000;42:677–699. doi:10.1002/1521-4036(200010)42:6<677::AID-BIMJ677>3.3.CO;2-F. [Google Scholar]
- Clark PI, Gardiner PS, Djordjevic MV, Leischow SJ, Robinson RG. Menthol cigarettes: Setting the research agenda. Nicotine & Tobacco Research. 2004;6(Suppl. 1):S5–S9. doi: 10.1080/14622200310001649441. doi:10.1080/14622200310001649441. [DOI] [PubMed] [Google Scholar]
- Fiore M, Jaen C, Baker T. Treating tobacco use and dependence: 2008 Update. Clinical practice guidelines. Rockville, MD: U.S. Department of Health and Human Services; 2008. Public Health Service. [Google Scholar]
- Foulds J, Hooper MW, Pletcher MJ, Okuyemi KS. Do smokers of menthol cigarettes find it harder to quit smoking? Nicotine & Tobacco Research. 2010;12(Suppl. 2):S102–S109. doi: 10.1093/ntr/ntq166. doi: 10.1093/ntr/ntq166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu SS, Okuyemi KS, Partin MR, Ahluwalia JS, Nelson DB, Clothier BA, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine & Tobacco Research. 2008;10:457–462. doi: 10.1080/14622200801901914. doi:10.1080/14622200801901914. [DOI] [PubMed] [Google Scholar]
- Gandhi KK, Foulds J, Steinberg MB, Lu SE, Williams JM. Lower quit rates among African American and Latino menthol cigarette smokers at a tobacco treatment clinic. International Journal of Clinical Practice. 2009;63:360–367. doi: 10.1111/j.1742-1241.2008.01969.x. doi:10.1111/j.1742-1241.2008.01969.x. [DOI] [PubMed] [Google Scholar]
- Gardiner P, Clark PI. Menthol cigarettes: Moving toward a broader definition of harm. Nicotine & Tobacco Research. 2010;12(Suppl. 2):S85–S93. doi: 10.1093/ntr/ntq176. doi: 10.1093/ntr/ntq176. [DOI] [PubMed] [Google Scholar]
- Gundersen DA, Delnevo CD, Wackowski O. Exploring the relationship between race/ethnicity, menthol smoking, and cessation, in a nationally representative sample of adults. Preventive Medicine. 2009;49:553–557. doi: 10.1016/j.ypmed.2009.10.003. doi:10.1016/j.ypmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Hajek P, West R, Lee A, Foulds J, Owen L, Eiser JR, et al. Randomized controlled trial of a midwife-delivered brief smoking cessation intervention in pregnancy. Addiction. 2001;96:485–494. doi: 10.1046/j.1360-0443.2001.96348511.x. doi:10.1046/j.1360-0443.2001.96348511.x. [DOI] [PubMed] [Google Scholar]
- Healton CG, Bullock AT, Robinson WS, Beck SE, Cartwright J, Eubanks SY. Why we should make menthol cigarettes history. Nicotine & Tobacco Research. 2010;12(Suppl. 2):S94–S97. doi: 10.1093/ntr/ntq177. doi: 10.1093/ntr/ntq177. [DOI] [PubMed] [Google Scholar]
- Hyland A, Garten S, Giovino GA, Cummings KM. Mentholated cigarettes and smoking cessation: Findings from COMMIT. Community Intervention Trial for Smoking Cessation. Tobacco Control. 2002;11:135–139. doi: 10.1136/tc.11.2.135. doi:10.1136/tc.11.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko RH, Ji L, Barnette P, Bostrom B, Hutchinson R, Raetz E, et al. Outcome of patients treated for relapsed or refractory acute lymphoblastic leukemia: A Therapeutic Advances in Childhood Leukemia Consortium study. Journal of Clinical Oncology. 2010;28:648–654. doi: 10.1200/JCO.2009.22.2950. doi:10.1200/JCO.2009.22.2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Curry SJ, Lando HA, Pirie PL, Grothaus LC, Nelson JC. Prevention of relapse in women who quit smoking during pregnancy. American Journal of Public Health. 1999;89:706–711. doi: 10.2105/ajph.89.5.706. doi:10.2105/AJPH.89.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan MJ. Ordinal outcomes with the continuation ratio model. 2000, September. . Paper presented at the Proceedings of the Northeast SAS Users Group Conference, Philadelphia, PA. [Google Scholar]
- Muscat JE, Richie JP, Jr., Stellman SD. Mentholated cigarettes and smoking habits in whites and blacks. Tobacco Control. 2002;11:368–371. doi: 10.1136/tc.11.4.368. doi:10.1136/tc.11.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuyemi KS, Ahluwalia JS, Ebersole-Robinson M, Catley D, Mayo MS, Resnicow K. Does menthol attenuate the effect of bupropion among African American smokers? Addiction. 2003;98:1387–1393. doi: 10.1046/j.1360-0443.2003.00443.x. doi:10.1046/j.1360-0443.2003.00443.x. [DOI] [PubMed] [Google Scholar]
- Okuyemi KS, Faseru B, Sanderson Cox L, Bronars CA, Ahluwalia JS. Relationship between menthol cigarettes and smoking cessation among African American light smokers. Addiction. 2007;102:1979–1986. doi: 10.1111/j.1360-0443.2007.02010.x. doi:10.1111/j.1360-0443.2007.02010.x. [DOI] [PubMed] [Google Scholar]
- Okuyemi KS, Lawrence D, Hammons G, Alexander LA. Use of mentholated cigarettes: What can we learn from national data sets? Addiction. 2010;105(Suppl. 1):1–4. doi: 10.1111/j.1360-0443.2010.03239.x. doi:10.1111/j.1360-0443.2010.03239.x. [DOI] [PubMed] [Google Scholar]
- Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S. Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Archives of Internal Medicine. 2006;166:1915–1922. doi: 10.1001/archinte.166.17.1915. doi:10.1001/archinte.166.17.1915. [DOI] [PubMed] [Google Scholar]
- Quach A, Ji L, Mishra V, Sznewajs A, Veatch J, Huberty J, et al. Thyroid and hepatic function after high-dose (131)I-metaiodobenzylguanidine ((131)I-MIBG) therapy for neuroblastoma. Pediatric Blood Cancer. 2011;56:191–201. doi: 10.1002/pbc.22767. doi:10.1002/pbc.22767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitzel LR, Vidrine JI, Businelle MS, Kendzor DE, Costello TJ, Li Y, et al. Preventing postpartum smoking relapse among diverse, low income women: A randomized clinical trial. Nicotine & Tobacco Research. 2010;12:326–335. doi: 10.1093/ntr/ntq001. doi:10.1093/ntr/ntq001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahre M, Okuyemi KS, Joseph AM, Fu SS. Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence-based tobacco cessation treatments. Addiction. 2010;105(Suppl. 1):75–83. doi: 10.1111/j.1360-0443.2010.03200.x. doi:10.1111/j.1360-0443.2010.03200.x. [DOI] [PubMed] [Google Scholar]
- Trinidad DR, Perez-Stable EJ, Messer K, White MM, Pierce JP. Menthol cigarettes and smoking cessation among racial/ethnic groups in the United States. Addiction. 2010;105(Suppl. 1):84–94. doi: 10.1111/j.1360-0443.2010.03187.x. doi:10.1111/j.1360-0443.2010.03187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Reitzel LR, Velasquez MM, Mazas CA, Cinciripini PM, Wetter DW. Motivation and Problem Solving (MAPS): Motivationally-based skills training for treating tobacco dependence. 2011 doi: 10.1016/j.cbpra.2011.11.001. Manuscript in preparation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JM, Gandhi KK, Steinberg ML, Foulds J, Ziedonis DM, Benowitz NL. Higher nicotine and carbon monoxide levels in menthol cigarette smokers with and without schizophrenia. Nicotine & Tobacco Research. 2007;9:873–881. doi: 10.1080/14622200701484995. doi:10.1080/14622200701484995. [DOI] [PubMed] [Google Scholar]