Abstract
Drug-induced esophageal injury is an under-recognized clinical problem, and is associated with antibiotic use in more than 50% of cases. The current report describes a teenage girl who presented with symptoms of pill-induced esophagitis following doxycycline use. Subsequent investigations identified a previously undiagnosed vascular ring. Although most patients who experience drug-induced esophageal injury have no underlying anatomical or functional disorder of the esophagus, the condition is more common in areas of esophageal narrowing. The present case illustrates the possibility of an occult esophageal obstruction representing a risk factor for pill esophagitis. The etiologies, mechanisms and management of drug-induced esophageal injury are reviewed, and aspects of vascular rings that are relevant to paediatricians are discussed.
Keywords: Blood vessels, Congenital abnormalities, Deglutition disorders, Esophagitis, Pharmaceutical preparations
Abstract
Les lésions œsophagiennes induites par les médicaments sont un problème clinique sous-diagnostiqué et, dans plus de 50 % des cas, elles s’associent à une antibiothérapie. Le présent article décrit le cas d’une adolescente qui a consulté en raison de symptômes d’œsophagite induite par l’utilisation de comprimés de doxycycline. Des examens subséquents ont révélé un anneau vasculaire jusque-là non diagnostiqué. Même si la plupart des patients qui présentent des lésions œsophagiennes induites par les médicaments n’ont pas de trouble anatomique ou fonctionnel sous-jacent de l’œsophage, ce problème est plus courant dans les zones de rétrécissement œsophagien. Le présent cas illustre la possibilité d’obstruction œsophagienne occulte comme facteur de risque d’œsophagite induite par des comprimés. Les chercheurs passent en revue les étiologies, les mécanismes et la prise en charge des lésions œsophagiennes induites par les médicaments et exposent les aspects des anneaux vasculaires pertinents pour les pédiatres.
A previously healthy 17-year-old girl presented to the emergency department with a five-day history of progressive odynophagia and dysphagia. Two days before the onset of symptoms, she began a course of oral doxycycline to treat acne. She now described discomfort localized to the sternal notch, both at rest and when swallowing liquids. Multiple swallows were required to pass solids due to the sensation of impaction in the esophagus. Over the preceding two days, she had developed subjective shortness of breath with exertion or deep inspiration.
The patient had no history of dysphagia, food bolus impaction, shortness of breath or stridor. She denied symptoms of gastroesophageal reflux, and had no history of oral lesions or Candida infections. Personal and family histories were negative for gastrointestinal, atopic or autoimmune conditions. Her only medication was doxycycline, which was reportedly swallowed in an upright position with ample fluids.
The patient’s physical examination was entirely unremarkable. A double-contrast barium swallow revealed a rounded posterior indentation of the esophagus at the level of the aortic arch, suggestive of a vascular ring (Figure 1). Computed tomography identified a right-sided aortic arch with an aberrant left subclavian artery and suggested an intact ligamentum arteriosum. The trachea was deviated leftward with narrowing to less than 50% of its original diameter at the level of the compression. Echocardiography did not reveal any intracardiac abnormalities.
Figure 1).
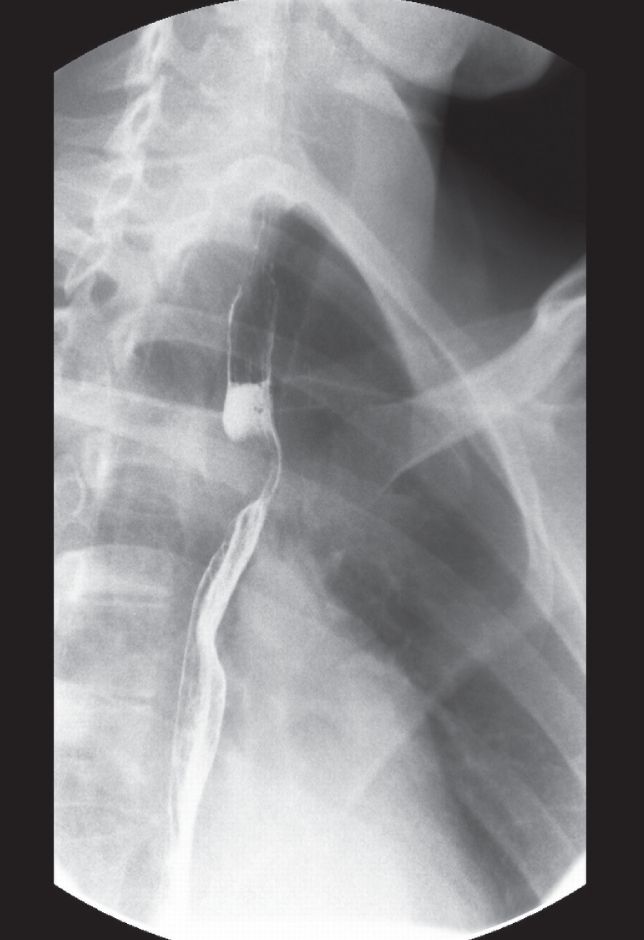
Barium esophogram demonstrating a posterior filling defect
The patient was advised to discontinue the doxycycline; no further therapy was initiated. Due to persistent dysphagia, upper endoscopy was performed two weeks after the initial presentation and revealed a narrowed area of the upper esophageal lumen through which the endoscope passed easily. There was no evidence of mucosal injury, and biopsies of the esophageal mucosa were histologically unremarkable. Because of persistent symptoms, the patient subsequently underwent successful thoracoscopic surgery to divide the vascular ring.
DISCUSSION
Drug-induced esophageal injury (DIEI) is a relatively common, although under-recognized, phenomenon. A comprehensive review in 1999 (1) identified nearly 1000 cases of this condition over 30 years, which likely underestimated the scope of DIEI. The true incidence of this condition is uncertain given the absence of noninvasive diagnostic testing, but one estimate suggested 10,000 cases/year in the United States alone (1). At least 20 paediatric cases have been reported, of which the youngest child was three years of age (1,2). DIEI is believed to be less common in children than in adults because they take fewer medications and these are less likely to be in tablet form.
Almost 80 different medications have been associated with DIEI, and the majority of cases involve either antibiotics or nonsteroidal anti-inflammatory drugs (NSAIDs) (1,3). Among antibiotics, tetracycline, doxycycline and clindamycin have been the causative agents in more than 50% of cases (3,4). Although all forms of NSAIDs can cause esophageal injury, the use of acetylsalicylic acid has been reported in most cases (1). Other medications commonly associated with DIEI include potassium chloride, quinidine, alendronate, ascorbic acid and ferrous sulphate (Table 1) (3,5).
TABLE 1.
Common drugs associated with drug-induced esophageal injury
| Antibiotics | Nonsteroidal anti-inflammatory agents | Other |
|---|---|---|
| Doxycycline | Acetylsalicylic acid | Potassium chloride |
| Tetracycline | Ibuprofen | Quinidine |
| Clindamycin | Naproxen | Alendronate |
| Amoxicillin | Ascorbic acid | |
| Ferrous sulphate | ||
| Glibenclamide (glyburide) | ||
| Captopril | ||
| Nifedipine |
Data from reference 3
Both pharmacological and patient factors may contribute to DIEI (Table 2). Patient-related factors include swallowing tablets with insufficient fluids, recumbence shortly after ingestion of medications, decreased saliva production (whether intrinsic or due to anticholinergic drugs) and, to a lesser extent, underlying esophageal disorders (3). Although the vast majority of patients with DIEI have no esophageal abnormality, the condition has been reported with increased frequency in association with abnormal esophageal structure and dysmotility (3). Among patients with normal esophageal anatomy, DIEI most commonly occurs where there is anatomical narrowing such as at the site of the aortic arch, the left mainstem bronchus or the gastroesophageal junction. DIEI has also been described in patients with esophageal compression due to left atrial enlargement from mitral valve disease (6). In addition, patients with hiatus hernia may be at greater risk for esophageal ulceration with NSAID use, likely due to a demonstrated delay in passing tablets into the stomach (7).
TABLE 2.
Factors contributing to drug-induced esophageal injury
| Patient | Pharmaceutical |
|---|---|
| Recumbence after ingestion of medication | Concentration of medication |
| Insufficient fluid taken with medication | pH of medication |
| Decreased saliva production | Slow-release format |
| Prolonged contact of medication with mucosa | Delivery method (capsule versus tablet) |
| Esophageal disorders | Tablet size |
Data from reference 3
The mechanism of mucosal injury in DIEI depends on several pharmacological factors. Prolonged mucosal contact with pill contents plays a significant role, and can be influenced by pill size and formulation (3,8). Large pills are more commonly retained in the esophagus than small pills (9). Sustained-release preparations are sometimes more damaging to the esophagus than standard preparations of the same medications (1). Gelatin capsules are hygroscopic and can become sticky, adhering to esophageal mucosa and delaying pill transit (3). For this reason, doxycycline capsules have been associated with esophageal injury more than the tablet form has (10). Doxycycline may accumulate in the basal layer of the squamous epithelium and cause cell toxicity by inhibiting protein synthesis, cell turnover and repair (11). Doxycycline, tetracycline, ascorbic acid and ferrous sulphate all produce a pH <3.0 when in contact with saliva, and may ‘burn’ the esophageal mucosa causing ulceration (1,8). NSAIDs are also acidic molecules that may cause injury by accumulating in toxic concentrations in esophageal tissues (3,12). While the inhibition of prostaglandins and subsequent decreased mucosal cytoprotection are known to be important in NSAID-associated gastritis, it is not clear whether this mechanism plays a significant role in DIEI (12,13).
In most cases of DIEI, esophageal injury consists of local inflammation or discrete ulceration, although rare cases of esophageal hemorrhage, perforation or stenosis have been reported (14–16). The majority of uncomplicated cases resolve spontaneously with supportive care and removal of the offending agent. There is little evidence to support the use of acid suppressive or antisecretory agents for the promotion of healing, although clinical practice may include trials of these drugs (3,8). A few studies have reported symptomatic improvement with topical anesthetic solutions or sucralfate (17).
In our patient, an underlying esophageal pathology was suspected because her symptoms arose despite using an ideal pill-taking technique. Investigations for abnormal esophageal anatomy identified the vascular ring that had contributed to her development of pill-induced dysphagia.
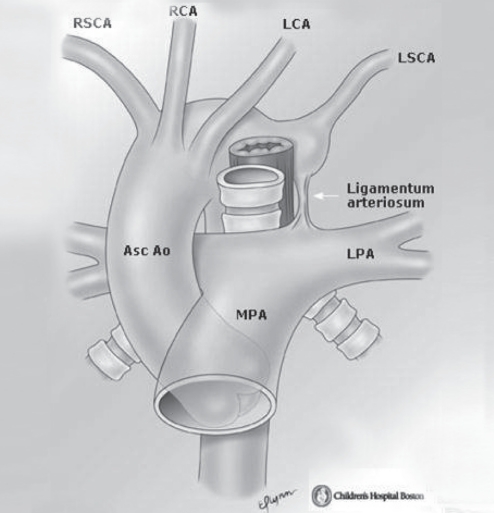
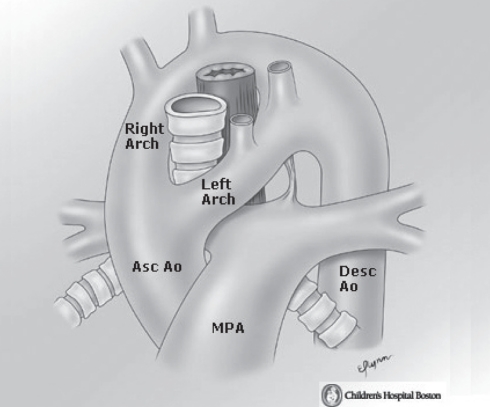
A vascular ring is a combination of blood vessels and ligamentous structures that encircle the intrathoracic trachea and esophagus because of abnormal regression of elements of the embryonic aortic arch. These structures can result in clinically significant symptoms due to varying degrees of tracheal and/or esophageal compression. Although their overall incidence is uncertain, these vascular anomalies are known to represent 1% to 2% of all congenital heart lesions (18). Two forms of vascular rings have been described: complete and incomplete – so named based on the degree of tracheoesophageal encirclement. The majority of patients have complete rings, of which the most common forms are a double aortic arch and a right aortic arch with an aberrant left subclavian artery (as in our patient) (18). In the second of these lesions, the normal left-sided orientation of the aortic arch is reversed and the vessel crosses over the right bronchus. The abnormal origin of the left subclavian artery results in its course posterior to the esophagus. The ring is completed by the presence of the ligamentum arteriosum, which is a nonfunctional vestige of the ductus arteriosus (Figures 2 and 3).
Figure 2).
Right aortic arch with aberrant origin of the left subclavian artery (LSCA). Asc Ao Ascending aorta; LCA Left carotid artery; LPA Left pulmonary artery; MPA Main pulmonary artery; RCA Right carotid artery; RSCA Right subclavian artery. Reproduced with permission from the multimedia library of Children’s Hospital Boston (Massachusetts, USA)
Figure 3).
Double aortic arch. Asc Ao Ascending aorta; Desc Ao Descending aorta, MPA Main pulmonary artery. Reproduced with permission from the multimedia library of Children’s Hospital Boston (Massachusetts, USA)
The degree to which a vascular ring causes symptoms and, therefore, the age at which patients present depend on the tightness of the encircling structures (19). Rings that cause little or no tracheoesophageal compression may be asymptomatic, although most patients with complete vascular rings demonstrate signs within the first few months of life (20). Children with a right aortic arch and an aberrant left subclavian artery generally present later in life than children with a double aortic arch (18). Symptoms in younger patients most commonly include stridor or noisy respirations, respiratory distress and wheezing (20). Feeding difficulties and choking episodes are also frequently reported once solid foods are introduced (18). Patients present less often with complaints of dysphagia, although this may be the only symptom of a vascular ring in an older child or adolescent (20).
The most useful imaging modality for the identification of a vascular ring is the barium esophogram, which may demonstrate a characteristic esophageal indentation(s) (20). A posterior filling defect (Figure 1) is usually caused by a retroesophageal subclavian artery, as in our patient (14). Chest radiography is often not contributory, although it may demonstrate tracheal narrowing or deviation on careful evaluation (13). Computed tomography or magnetic resonance imaging are important complementary studies for delineation of the tracheal and vascular anatomy (18,20). Echocardiography may be valuable in ruling out other concurrent cardiac anomalies (18).
The management of patients with symptomatic vascular rings involves surgery, generally via a left posterolateral thoracotomy (20). For a right-sided aortic arch with aberrant left subclavian artery, the procedure involves division of the left ligamentum arteriosum, and lysis of any adhesions around the esophagus and trachea (18). For patients with tracheal compression, resolution of symptoms may take weeks to months after surgery, particularly if the vascular ring has caused constriction deformities of the tracheal cartilage (20).
CONCLUSION
While the large majority of patients with DIEI have no underlying structural anomalies, the present case illustrates the possibility of an occult esophageal obstruction representing an unsuspected risk factor for pill esophagitis. When patients with a presentation suggestive of pill-induced esophageal injury have no risk factors or history of a suboptimal medication-taking technique, the present report suggests that investigation of a possible underlying esophageal pathology may be worthwhile.
Footnotes
NOTE: The patient described in this report was examined and treated at The Hospital for Sick Children in Toronto, Ontario. The authors have no conflicts of interest to declare, and no sources of funding to disclose.
REFERENCES
- 1.Kikendall J. Pill esophagitis. J Clin Gastroenterol. 1999;28:298–305. doi: 10.1097/00004836-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Kato S, Komatsu K, Harada Y. Medication-induced esophagitis in children. Gastroenterol Jpn. 1990;25:485–8. [PubMed] [Google Scholar]
- 3.Jaspersen D. Drug-induced oesophageal disorders. Pathogenesis, incidence, prevention and management. Drug Saf. 2000;22:237–49. doi: 10.2165/00002018-200022030-00007. [DOI] [PubMed] [Google Scholar]
- 4.Bott SJ, McCallum RW. Medication-induced oesophageal injury. Survey of the literature. Med Toxicol. 1986;1:449–57. doi: 10.1007/BF03259855. [DOI] [PubMed] [Google Scholar]
- 5.Levine M. Drug-induced disorders of the esophagus. Abdom Imaging. 1999;24:3–8. doi: 10.1007/s002619900431. [DOI] [PubMed] [Google Scholar]
- 6.Whitney B, Croxon R. Dysphagia caused by cardiac enlargement. Clin Radiol. 1972;23:147–52. doi: 10.1016/s0009-9260(72)80079-5. [DOI] [PubMed] [Google Scholar]
- 7.Shallcross TM, Wyatt JI, Rathbone BJ, Heatley RV. Non-steroidal anti-inflammatory drugs, hiatus hernia, and Helicobacter pylori, in patients with oesophageal ulceration. Br J Rheumatol. 1990;29:288–90. doi: 10.1093/rheumatology/29.4.288. [DOI] [PubMed] [Google Scholar]
- 8.Boyce H. Drug-induced esophageal damage: Diseases of medical progress. Gastrointest Endosc. 1998;47:547–50. doi: 10.1016/s0016-5107(98)70264-0. [DOI] [PubMed] [Google Scholar]
- 9.Hey H, Jorgensen F, Sorensen K, et al. Oesophageal transit of six commonly used tablets and capsules. BMJ. 1982;285:1717–9. doi: 10.1136/bmj.285.6356.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlborg B, Densert O, Lindqvist C. Tetracycline induced esophageal ulcers: A clinical and experimental study. Laryngoscope. 1983;93:184–7. doi: 10.1288/00005537-198302000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Leong RW, Chan FK. Drug-induced side effects affecting the gastrointestinal tract. Expert Opin Drug Saf. 2006;5:585–92. doi: 10.1517/14740338.5.4.585. [DOI] [PubMed] [Google Scholar]
- 12.Peterson KU, Jaspersen D. Medication-induced oesophageal disorders. Expert Opin Drug Saf. 2003;2:495–507. doi: 10.1517/14740338.2.5.495. [DOI] [PubMed] [Google Scholar]
- 13.Zografos GN, Georgiadou D, Thomas D, et al. Drug-induced esophagitis. Dis Esophagus. 2009;22:633–63. doi: 10.1111/j.1442-2050.2009.00972.x. [DOI] [PubMed] [Google Scholar]
- 14.Abid S, Mumtaz K, Jafri W, et al. Pill-induced esophageal injury: Endoscopic features and clinical outcomes. Endoscopy. 2005;37:740–4. doi: 10.1055/s-2005-870129. [DOI] [PubMed] [Google Scholar]
- 15.Kikendall JW, Friedman AC, Oyewole MA, Fleischer D, Johnson LF. Pill-induced esophageal injury. Case reports and review of the medical literature. Dig Dis Sci. 1983;28:174–82. doi: 10.1007/BF01315148. [DOI] [PubMed] [Google Scholar]
- 16.D’Agostino L, Manguso F, Bennato R, Scaramuzzo A. A life-threatening case of stenosing pill hypopharynx-oesophagitis caused by a tamsulosin capsule. Dig Liver Dis. 2004;36:632–4. doi: 10.1016/j.dld.2003.11.032. [DOI] [PubMed] [Google Scholar]
- 17.Pinos T, Figueras C, Mas R. Doxicycline-induced esophagitis: Treatment with liquid sucralphate. Am J Gastroenterol. 1990;85:902–3. [PubMed] [Google Scholar]
- 18.Devaney E, Ohye R, Bove E. Vascular rings and slings. In: Grosfeld J, O’Neill J, Fonkalsrud E, Coran A, editors. Pediatric Surgery. 6th edn. Philadelphia: Mosby Inc; 2006. pp. 1978–80. [Google Scholar]
- 19.Hernanz-Schulman M. Vascular rings: A practical approach to imaging diagnosis. Pediatr Radiol. 2005;35:961–79. doi: 10.1007/s00247-005-1529-0. [DOI] [PubMed] [Google Scholar]
- 20.Fakhoury K, Seilheimer D. Vascular rings. In: Garson A, Bricker J, Fisher D, Neish S, editors. The Science and Practice of Pediatric Cardiology. 2nd edn. Baltimore: Williams and Wilkins; 1998. pp. 2821–2. [Google Scholar]