Abstract
Objective
The aim of this study was to gather data from Canadian stakeholders to help construct a national strategy and agenda for lymphedema management.
Methods
The Canadian Lymphedema Framework, a collaboration of medical academics, lymphedema therapists, patient advocates, and others, used participatory action research and Open Space Technology to identify issues and build consensus at a national meeting of lymphedema stakeholders. Proceedings were videotaped and underwent content analysis. Existing Canadian documentation on lymphedema services was analyzed. Using those data sources, the Canadian Lymphedema Framework drafted a development strategy.
Results
Of 320 invited stakeholders (patients, therapists, physicians, industry representatives, and health policymakers), 108 participated in a day-long videotaped meeting discussing strategies to improve the management of lymphedema and related disorders in Canada. Participants identified barriers, challenges, and issues related to the need to raise awareness about lymphedema with patients, physicians, and the public. Five priority areas for development were articulated: education, standards, research, reimbursement and access to treatment, and advocacy. The main barrier to development was identified as the lack of clear responsibility within the health care system for lymphedema care.
Conclusions
Data from stakeholders was obtained to solidly define priority areas for lymphedema development at a national level. The Canadian Lymphedema Framework has created a working plan, an advisory board, and working groups to implement the strategy.
Keywords: Lymphedema, cancer rehabilitation, qualitative study, health policy, health education
1. INTRODUCTION
Lymphedema is an under-recognized and under-treated condition that affects many cancer survivors, but that lacks a national voice. In 2009, the Canadian Lymphedema Framework was formed to fill that need (Table I).
TABLE I.
Key points about lymphedema
| Lymphedema is a vastly under-recognized medical condition that affects patients treated for cancer, children, and people with comorbid conditions such as advanced venous stasis disease. Many patients do not receive timely diagnosis, adequate treatment, or risk reduction education. |
| The Canadian Lymphedema Framework is a collaboration of medical academics, lymphedema therapists, patient advocates, and interested others, part of an international initiative to promote research, best practice guidelines, and lymphedema clinical development worldwide. |
| Education about basic pathophysiology and about best practices in lymphedema diagnosis and treatment is needed in all health care programs—medical, nursing, physical therapy, occupational therapy, and kinesiology. |
With medical improvements in cancer treatment leading to increased rates of survival and longer survival times, cancer rehabilitation is needed to address the physical, emotional, and social consequences of treatment, and to improve overall quality of life 1. Lymphedema is reported to be the most debilitating complication of treatment for breast cancer, affecting body image and social, family, sexual, and work-related activities 2. In lower-limb lymphedema, mobility limitations may lead to loss of work, and treatment itself can impose an increased financial burden 3.
Lymphedema is the accumulation of a protein-rich fluid in the interstitial space because of reduced lymph transport capacity. Secondary lymphedema can occur after damage to lymph vessels or nodes from trauma, tumors, surgery, or radiation therapy. Primary lymphedema is a result of absent or malformed lymph vessels. Most cases of lymphedema in North America occur secondary to cancer treatment 4. The reported incidence varies depending on the definition of lymphedema, the length of follow-up, and the type of cancer treated. Breast cancer has been the most studied; in recent reports, its lymphedema incidence range is given as 3%–42% 5,6. Incidences from other cancer treatments vary with the malignancy—for example, 3%–50% in soft-tissue sarcoma, 19.6% in gynecologic malignancies, and 16.3% in melanoma 4,7.
2. BACKGROUND
The Canadian Lymphedema Framework is an academic and patient-stakeholder collaboration with charitable status that promotes research, education, and lymphedema management in Canada and worldwide. It is part of an international collaboration begun in 2002 when a British coalition of clinicians, researchers, patient support groups, and industry partners came together to make lymphedema a national health care priority. The result was a new U.K. tariff classification giving access, by prescription, to all products required for lymphedema treatment 8. In the United Kingdom, the International Lymphoedema Framework was established as a charity, and the creation of national frameworks was promoted in other countries. The Canadian Lymphedema Framework was formed in 2009, and with help from the International Lymphoedema Framework, initiated a national meeting of stakeholders to discuss the issues and to set the research and development agenda for lymphedema management in Canada. The present report summarizes that project.
3. METHODS
The Canadian Lymphedema Framework used Open Space Technology in a participatory action research framework. Participatory research is an interactive approach in which all participants are co-investigators, defining and implementing research goals 9. Open Space Technology allows for various constituencies to participate equally in consensus-building about priorities, barriers, and resource issues. It is an effective strategy that self-organizing groups with no designated meeting leader can use to address complex issues in a short space of time 10. The Open Space Technology format was successfully used by Frameworks in other countries 11. Participants receive all recorded documentation from the meeting in a Book of Proceedings 12.
3.1 Data Sources
The only Canadian report on community priorities for lymphedema located was the Lymph Listens report of the Lymphedema Association of Ontario 13. Funded through the Canadian Breast Cancer Foundation–Ontario Chapter, that project surveyed and interviewed lymphedema patients, health care providers, and other key stakeholder representatives 13. The report documented
a lack of standardized and comprehensive material for patient education.
limited knowledge among physicians about lymphedema, treatment options, and support services.
a need for more hospital-based lymphedema diagnosis and treatment centres.
a need for more certified lymphedema therapists.
Other data sources were the documents produced at the stakeholder meeting:
The Book of Proceedings
Raw videotape footage of the meeting
Pre-meeting correspondence
Field notes of one of the researchers (PH)
3.2 Ethics Approval
McGill University granted ethics approval to conduct the present study, which included videotaping the national stakeholder meeting held in Toronto, Ontario, November 6, 2009. All participants gave informed consent for the videotaping.
3.3 Sampling Procedures
With a diverse network of contacts across the country, the Canadian Lymphedema Framework used purposeful sampling to invite more than 300 key lymphedema stakeholders to the meeting. Invitations were sent to representatives in all territories and provinces, and across a spectrum of socio-economic and cultural groups.
3.4 Data Analysis
The national meeting proceeded to consensus building using large-group briefing and knowledge-transfer sessions before and after small group discussion periods. To construct themes and to congregate and confirm working group strategies and action plans, two of the researchers (PH, AT) separately read the Book of Proceedings and the pre-meeting correspondence. The two researchers independently analyzed videotaped and written proceedings, then conjointly discussed results.
4. RESULTS
The 108 attendees were representative of all key stakeholder groups: lymphedema therapists (25.9%), patient advocates (16.6%), industry representatives (14.8%), physicians (11%), nurses (9.25%), researchers (6.5%), government and policy representatives (4.6%), educators (3.7%), and interested others (7.4%). (Percentages add to more than 100% because of a few assignments to more than one category.)
During the day-long meeting, participants were totally engaged, passionate, and vocal, but also respectful listeners. Many patients told personal stories of difficulties getting diagnosed (or misdiagnosed) and finding appropriate treatment. Health professionals and patients shared equally in an atmosphere of mutual trust and commitment. One health care provider acknowledged the psychological difficulty patients face and said, “It is easy for clinicians to write a note that patient compliance is a problem. Patients try to pretend it is not happening. Sometimes it takes three to four years to accept [the lymphedema condition].” A patient commented, “We have been living so long with these problems, they are seeped into our genes” 12.
Data analysis of all sources was consistent. It revealed a lack of awareness, insufficient education and research, and limited access to treatment as the major issues.
4.1 Issues Identified
4.1.1 Global Lack of Awareness
The central problem identified was a global lack of awareness of lymphedema as a chronic medical condition. Participants articulated the ignorance that exists among health care professionals, policymakers, funders, and the public. One group termed it a “vicious circle of lacks”—lack of education affects lack of standards of care, and lack of research affects lack of funding, and so on 12.
4.1.2 Insufficient Education and Standards
Education about the lymphatic system, its disorders, and treatment of all types of lymphedema was identified as being needed in all health care programs. Health practitioners in the field need evidence-based information to diagnose lymphedema early, to provide guidance, and to refer patients for prompt and appropriate treatment to prevent morbidity. Government policymakers and funders need to be aware of the impact of lymphedema on patient work status and on health care costs accrued because of the complications of untreated lymphedema.
Insufficient education about lymphedema in undergraduate health care programs and lack of homogeneity of standards in definition, diagnosis, care models, and training for therapists and garment fitters mean that patients may not receive prompt and appropriate diagnosis and treatment. Patients are often not informed about risk reduction, self-care, and treatment. There is a need to make lymphedema, its impact, and its treatment better understood by the public.
4.1.3 Limited or No Access to Lymphedema Treatment
Many patients with lymphedema, especially those with non-cancer-related lymphedema and children with lymphedema, have limited or no access to treatment. This compromised access stems from a lack of hospital-based services and an insufficient number of private clinics or from the cost of treatment. Patients in rural areas may not have access to trained therapists or physicians who can properly diagnose the condition. Participants identified an urgent need for better provincial reimbursement policies.
4.1.4 Lack of Research
Stakeholders described a lack of research into the prevalence of lymphedema, effective treatment modalities, impact on quality of life, and cost analysis. Lack of research in these areas means that lymphedema advocacy with decision-makers and funders is often difficult and ineffective.
4.2 Barriers to Improved Care
Several major barriers to improved care were identified (Table II). The immensity of Canada’s geography and decentralized provincial responsibility for health care delivery present difficulties. How is a national policy to be achieved in a “regional” country? Importantly, the setting for lymphedema management in the health system is not clear. Secondary lymphedema is an issue for cancer survivors and should be included in cancer rehabilitation programs, but patients with primary lymphedema feel abandoned. Who is responsible for the lymphedema diagnosis? Where are the lymphology specialists? Who provides lymphedema care, and what training is required? Lack of funding sources affects access to treatment.
TABLE II.
Barriers to lymphedema care
| No defined medical domain responsible for lymphedema diagnosis and treatment |
| Lack of funding sources |
| Limited access to treatment in hospitals |
| Inequities in provincial health policies regarding lymphedema care |
| Insufficient access to trained therapists, particularly in rural areas |
At the conclusion of the meeting, the Canadian Lymphedema Framework undertook to analyze the recommendations and to create a process to move the agenda forward.
5. DISCUSSION AND CONCLUSIONS
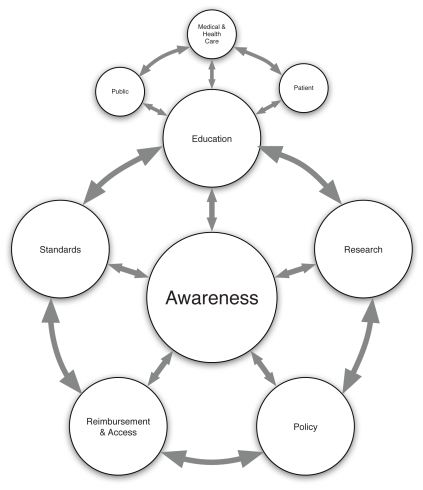
The Canadian Lymphedema Framework continued the strategic planning exercise by grouping the meeting themes into 5 major priority areas: education, research, reimbursement, standards, and advocacy (Figure 1).
FIGURE 1.
The lymphedema web of awareness.
Participants identified education as key to developing awareness, encouraging interest in research, and promoting best practices in clinical care. Implementing chronic disease or rehabilitation models, Web-based education programs, and current best practices were identified as possible solutions.
A need was identified for prevalence data, cost–benefit analyses of treatment, and trials on preventive strategies and the clinical effectiveness of decongestive therapy components. In preparing an update of the 2006 best practice guidelines, the American Lymphedema Framework Project and the International Lymphoedema Framework noted that the scarcity of clinical trials remains a difficulty 14.
The need for standardization in lymphedema terminology, diagnostics, measurements, and clinical trials is also widely acknowledged 11. The International Lymphoedema Framework created a minimal dataset so that common data could begin to be gathered using standard terminology. The Japanese and American frameworks unveiled new databases at the 3rd International Lymphedema Conference, co-hosted by the International Lymphoedema Framework, the Canadian Lymphedema Framework, and the Lymphedema Association of Ontario in Toronto, Ontario, in June 2011. Use of these databases will be reported at the 4th International Lymphedema Conference in Montpellier, France, in June 2012.
Funding for treatment was identified as a major issue. Drafting of reimbursement policy requires compilation of data from existing regional funding models and research into funding practices in other countries. Provincial patient advocacy groups have been effective in signalling lymphedema as an unrecognized medical condition and in advocating for treatment. Physicians and policymakers also need to become more active and to participate in developing effective lymphedema programs.
The national stakeholder meeting was an initial step in bringing together diverse stakeholders and soliciting their perspectives on lymphedema management in Canada. The identified priorities reflect the consensus achieved at the meeting and the urgent need for action. The Canadian Lymphedema Framework has now developed a 3-year strategic roadmap to
raise the profile of lymphedema in Canada,
develop a national coordinated patient advocacy strategy,
gain consensus and adoption of best practice guidelines, and
promote the development of research networks.
A volunteer Advisory Board and three volunteer working groups (Education, Research, and Partnership Development) are now working with the executive to identify key partners, to gather data, and to plan action to influence lymphedema practice, inform policy, and educate health professionals as the first priorities. A first lymphedema landscape study, undertaken in April 2010, has gathered important data on the current status of lymphedema management in Canada. Those data will inform the work of the committees, be used to measure progress, and be shared with government. The Education working group of educators and practitioners is now developing basic standards of education. Researchers representing medical, social, physical, and basic sciences have formed a core working group to lead the research agenda, prepare grant proposals, and establish relationships with international researchers to develop common projects. The partnership working group of patients, policymakers, and physicians is developing partnerships to support the Canadian Lymphedema The Lymphedema Web of Awareness Framework and its projects. Those individuals and other volunteers will be integral partners in establishing a long-term national strategy and a campaign for improved lymphedema management in Canada.
6. ACKNOWLEDGMENTS
The research reported here was supported by a grant from the Canadian Breast Cancer Research Alliance Knowledge Translation–Link Program, grant no. 020637. The Canadian Lymphedema Framework thanks all who participated in the National Lymphedema Stakeholder Meeting and all who have since volunteered.
Footnotes
7. CONFLICT OF INTEREST DISCLOSURES
AT is an instructor for the Dr. Vodder School International. JA is employed by 3M. The authors declare no financial conflicts of interest.
8. REFERENCES
- 1.Ristovski–Slijepcevic S, Nicoll I, Bennie F. Canadian Invitational Cancer Survivorship Workshop: creating an agenda for cancer survivorship. Toronto, ON: Canadian Partnership Against Cancer; 2008. [cited September 12, 2010]. [Available online at: http://www.partnershipagainstcancer.ca/wp-content/uploads/2.4.0.2.6-CPAC_CJ_Survivorship_0308_Final_E.pdf. [Google Scholar]
- 2.Towers A, Carnevale FA, Baker ME. The psychosocial effects of cancer-related lymphedema. J Palliat Care. 2008;24:134–43. [PubMed] [Google Scholar]
- 3.Ryan M, Stainton MC, Jaconelli C, Watts S, MacKenzie P, Mansberg T. The experience of lower limb lymphedema for women after treatment for gynecological cancer. Oncol Nurs Forum. 2003;30:417–23. doi: 10.1188/03.ONF.417-423. [DOI] [PubMed] [Google Scholar]
- 4.Cormier JN, Askew RL, Mungovan KS, Xing Y, Ross MI, Armer JM. Lymphedema beyond breast cancer: a systematic review and meta-analysis of cancer-related secondary lymphedema. Cancer. 2010;116:5138–49. doi: 10.1002/cncr.25458. [DOI] [PubMed] [Google Scholar]
- 5.McLaughlin SA, Wright MJ, Morris KT, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: patient perceptions and precautionary behaviors. J Clin Oncol. 2008;26:5220–6. doi: 10.1200/JCO.2008.16.3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Norman SA, Localio AR, Potashnik SL, et al. Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol. 2009;27:390–7. doi: 10.1200/JCO.2008.17.9291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N Y Acad Sci. 2008;1131:147–54. doi: 10.1196/annals.1413.014. [DOI] [PubMed] [Google Scholar]
- 8.International Lymphoedema Framework. Lymphedema Frameworks— The Way Forward. London, U.K.: International Lymphoedema Framework; 2010. [cited March 22, 2010]. [Available online at: http://www.lympho.org/mod_turbolead/upload/file/Focus%20Frameworks%20-%20protected.pdf. [Google Scholar]
- 9.Stringer ET. Action Research. 3rd ed. Los Angeles, CA: Sage Publications; 2007. [Google Scholar]
- 10.Owen H. Open Space Technology: A User’s Guide. 2nd ed. San Francisco, CA: Berrett–Koehler Publishers; 1997. [Google Scholar]
- 11.Armer J, Feldman J, Fu M, et al. alfp: identifying issues in lymphoedema in the US. J Lymphoedema. 2009;4:91. [Google Scholar]
- 12.Canadian Lymphedema Framework (CLF) Toronto, ON: CLF; 2009. [cited June 15, 2010]. Book of Proceedings. [Available online at: http://sites.google.com/site/canadalymph/national-stakeholder-meeting/post-meeting-documentation. [Google Scholar]
- 13.Kennedy A, Klein P. Lymph Listens: A Community Based Report on Living with Lymphedema in Ontario. Toronto, ON: The Lymphedema Association of Ontario; 2006. [cited June 12, 2010]. [Available online at: http://www.lymphovenous-canada.ca/lymphlistensfinalreport.pdf. [Google Scholar]
- 14.Cormier J, Feldman J, Askew R, et al. alfp to update the best practice document. J Lymphoedema. 2010;5:68–71. [Google Scholar]