Abstract
While emerging studies have demonstrated the benefit of exercise in early recovery from substance use disorders, recruitment and adherence to exercise interventions have been challenging. Tailoring interventions based on patient exercise preferences may address these concerns. Ninety-seven (N=97; age=41.6 years; 44% female) patients were recruited from an intensive substance abuse outpatient program and filled out questionnaires about their exercise preferences. Most (71%) patients were not currently engaged in an exercise program (i.e., exercising less than 20 minutes/day for 3 days/week over the last 6 months). The vast majority (95%) expressed an interest in engaging in an exercise program specifically designed for persons in substance use recovery and 89% reported wanting to initiate an exercise program within the first 3 months of sobriety. Specific exercise preferences regarding type of physical activity, exercise intervention components, and perceived benefits and barriers to exercise differed between males and females. These findings suggest low rates of regular exercise, high level of interest in engaging in exercise during early recovery, and point toward the need to tailor interventions to the unique preferences of individuals.
1. Introduction
Drug and alcohol dependence continue to be major public health concerns. Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) point toward high rates of substance use disorders (SUD) with 9.5% of the United States (US) population meeting DSM-IV criteria for either abuse or dependence within the last 12 months (Grant et al., 2004). The costs of SUDs in the US (in terms of treatment of the individual with a drug use disorder and his/her family) have been estimated between $150 and $200 billion annually (ONDCP, 2004). Not only are spontaneous remission rates from substance use disorders very low (Finney, Moos, & Timko, 1999)but relapse rates are high - ranging from 60–90% within the first year following treatment (Brownell, Marlatt, Lichtenstein, & Wilson, 1986; Hunt, Barnett, & Branch, 1971; Xie, McHugo, Fox, & Drake, 2005). Therefore, the development of interventions to decrease relapse rates and maintain treatment gains for substance abusing patients is critically important.
Relapse prevention models have included lifestyle modifications as a potentially important component of recovery (Marlatt & Donovan, 2005). For example, Larimer and colleagues (1999) describe the importance of helping the client develop “positive addictions” such as increased physical activity. Over the last decade there has been a growing body of literature examining the relationship and potential benefit of exercise in substance abusing populations. It has been argued that the benefits of exercise in early recovery may include increased self-efficacy for abstinence, improved mood states, decreased urges and cravings, and could function as a useful coping strategy (Read & Brown, 2003). Indeed, in one study moderate-intensity exercise was found to provide short-term relief from urges to drink alcohol (Ussher, Sampuran, Doshi, West, & Drummond, 2004). More recently, animal studies have shown that long-term physical activity decreases sensitivity to the positive-reinforcing effects of cocaine (Smith, Schmidt, Iordanou, & Mustroph, 2008)and that aerobic exercise during an abstinence period decreased subsequent cocaine seeking in rats (Lynch, Piehl, Acosta, Peterson, & Hemby, 2010).
While relatively few studies have been conducted to date, there have been efforts to examine exercise interventions for reducing problematic substance use and as an adjunct to substance abuse treatment (Brown et al., 2009; Brown et al., 2010; Collingwood, Sunderlin, Reynolds, & Kohl, 2000; Roessler, 2010; Sinyor, Brown, Rostant, & Seraganian, 1982). These studies provide preliminary evidence for the benefit of engaging in an exercise program during early recovery in terms of substance use outcomes, improved cardiorespiratory fitness, and acceptability of interventions. However, in addition to such methodological limitations as small sample sizes and lack of control groups, these studies also experienced challenges related to recruitment and retention of patients in the exercise interventions (Brown, et al., 2009; Brown, et al., 2010; Roessler, 2010; Weinstock, 2010).
Factors that limit exercise intervention recruitment and retention may be related to substance abusing patients' perceived benefits/barriers of exercise as well as specific exercise preferences. Utilizing a “patient-centered care” framework (Laine & Davidoff, 1996)may help address this issue. A patient-centered care approach consists of taking into account patient preferences, needs, and values when making treatment decisions (Institue of Medicine, 2001; Stewart et al., 2000). If these considerations are not included in treatment decision-making, patients may end up in a form of treatment that does not suit their needs, preferences or goals. This type of mismatch may result in decreased treatment adherence resulting from less commitment to staying in treatment or less efficacious outcomes even if patients stay in treatment (Battle et al., 2010). Similarly, this type of patient-centered care framework may be particularly helpful in informing the treatment development stage of designing new interventions for patient populations. As such, taking into account specific exercise preferences of substance abusing patients in early recovery may result in the development of interventions that are a better “fit” for this patient population.
For example, substance dependent patients in early recovery may be in a sensitive period of transition that can include attending numerous outpatient treatment sessions as well as 12-step meetings, rebuilding strained familial and personal relationships, finding new jobs, and addressing physical health problems that may have resulted from prolonged periods of substance use. They may have specific preferences regarding the timing, type, and structure of an exercise intervention that would influence adoption and maintenance of regular physical activity. As a result, consistent with the patient-centered care framework, focusing future research efforts on identifying exercise preferences among substance abusing populations may contribute to the development of exercise interventions that are not only effective but also more feasible to administer.
There has been relatively little work on examining exercise preferences in substance abusing populations. In one study, Read and colleagues (2001)examined the level of interest, preferred type of physical activity, and perceived barriers among alcohol dependent patients in substance abuse treatment. They found that the majority (75%) of participants expressed some interest in participating in an exercise program (Read, et al., 2001). Common barriers to exercise included: the cost of joining a gym, the cost of exercise equipment, lack of motivation, not having enough time, and transportation difficulties. Further, the most commonly endorsed type of physical activity participants would prefer to engage in was walking (66%). Finally, slightly more than half (51%) stated they preferred to exercise individually as opposed to in a group.
While the Read and colleagues (2001)study was an important first step, identification of specific exercise preferences can significantly optimize efforts to incorporate exercise as part of the recovery process for substance abusing patients. Future work in this area can be informed by the growing body of literature examining exercise preferences in other patient populations (e.g., cancer, depression, and diabetes). In these patient populations, concurrent examination of exercise preferences has been conducted in an effort to more effectively develop interventions that promote increased adherence, quality of life, and symptom reduction. Studies examining exercise preferences have often considered, but have not been limited to, interest for participating in a program, type of exercise, intensity of activity, location, company (i.e., alone or with others), extent of supervision, structure and duration of exercise (Karvinen, Courneya, Venner, & North, 2007; Lowe, Watanabe, Baracos, & Courneya, 2010; Rogers, Courneya, Verhulst, Markwell, & McAuley, 2008; Rogers et al., 2009; Stevinson et al., 2009; Vallance, Courneya, Jones, & Reiman, 2006). Results of these studies have shown specific associations between exercise preferences and demographic factors as well as disease-specific characteristics. For example, patients having undergone cancer treatment and particularly those in palliative care often prefer exercise that is home-based and conducted alone with family, friends or other cancer survivors (Karvinen et al., 2006; Stevinson, et al., 2009; Vallance, et al., 2006).
A demographic characteristic that consistently emerges as important in differentiating exercise preferences is gender. In a general population, Booth and colleagues (1997)found that more women than men reported walking and aerobics as their preferred form of physical activity whereas men preferred other activities such as swimming, team sports, racquet sports and jogging. Consistent with this finding, in a study of exercise preferences and barriers among urban African Americans with type 2 diabetes, more women than men indicated walking outdoors as their favorite form of physical activity (Wanko et al., 2004). The study also found that women exercised fewer days per week for shorter periods each time and were also more likely to report barriers to engaging in exercise. Similarly, in a physical activity cohort of HIV-positive and HIV-negative injection drug users, women had lower vigorous activity levels than men (Smit et al., 2006). With regard to the structure and extent of supervision, several studies indicate the potential need for additional assistance and support for women. In a survey of psychiatric patients in the United Kingdom, women had significantly lower self-efficacy for exercise compared to men (Ussher, Stanbury, Cheeseman, & Faulkner, 2007). Among non-Hodgkin's lymphoma survivors, more women than men reported preferring to be counseled about exercise and to engage in supervised exercise sessions (Vallance, et al., 2006).
The purpose of the present study is threefold. Our first objective is to investigate the extent to which substance dependent patients are interested in engaging in an exercise intervention as an adjunct to their substance abuse treatment. The second objective is to examine patients' preferences regarding the type, intensity, and timing of exercise interventions in relation to their ongoing substance abuse treatment. The third objective is to determine if there exist differences in exercise preferences across substance abuse treatment type (i.e., alcohol dependence only or drug dependence with or without alcohol dependence) and by gender. By tailoring physical activity interventions to patients' exercise preferences, the effectiveness of and adherence to the intervention may be increased.
2. Materials and methods
2.1. Participants and Procedures
Study participants were surveyed from an intensive day alcohol and drug treatment program of a private non-profit psychiatric and substance abuse hospital located in the Northeast United States. This project was reviewed and approved by the hospital's Institutional Review Board. Patients were eligible to participate if they were currently engaged in the alcohol and drug treatment program and were between the ages of 18 and 65 years. Individuals were excluded from the study if they had a current diagnosis of anorexia or bulimia nervosa, bipolar disorder, history of psychotic disorder or current psychotic symptoms, current suicidality or homicidality, marked organic impairment or significant physical disabilities or medical problems.
Trained research assistants reviewed medical records of patients enrolled in the hospital's Alcohol and Drug Treatment Programs. One hundred and sixty-five (N=165) patients were approached and presented with a description of the study. Of those patients, 33 (20%) were ineligible, 21 (12.7%) were discharged before the assessment could be completed, and 12 (7.3%) refused. Patients were ineligible because of current bipolar disorder (n=9), age (n=7), significant medical problems (n=6), current eating disorder (n=4), psychotic symptoms (n=4), no current substance use (n=2) and current suicidality (n=1). Written informed consent was obtained from all recruited participants (N=97). Of the 97 participants recruited in this study, 44.3% were female and the mean age of the sample was 41.6 (SD=12) years. A majority of the sample was Caucasian (91.7%) and had some college education (58.7%) while 44.4% were currently married or cohabitating with a partner and 43.3 % were currently employed.
All patients were receiving standard treatment in an abstinence-oriented program that focuses on substance abuse as a learned, maladaptive behavior pattern and on participation in 12-step recovery programs. Treatment was primarily group-based and included patients with any primary substance of abuse. Approximately half of the current sample (47.4%) was seeking treatment for alcohol dependence only (referred to the “Alcohol Dependence” group in this study) while the remainder of the sample (52.6%) had primary drug dependence only or with concomitant alcohol problems (referred to as the “Drug Dependence” group). In addition, over three-quarters (81.4%) of the sample had a comorbid mood and/or anxiety disorder. Table 1 lists demographic and clinical characteristics for the entire sample and for the Alcohol and Drug Dependence subsamples. Patients receiving treatment primarily for alcohol dependence, compared to those for drug dependence, were more likely to be older (45.3 vs. 38.3 years; t=3.02, df=95, p<.01), comprised of more females (60.5% vs. 39.5%; χ2=5.27, df=1, p<.05), less likely to be a smoker (50% vs. 78.4%; χ2 = 8.59, df=1, p<.01) and demonstrated a trend toward a higher prevalence of mood disorders (84.8% vs. 68.6%, χ2=3.49, df=1, p=.06).
Table 1.
Demographic and Clinical Characteristics
| Sample Characteristic | TOTAL Sample (N=97) | Alcohol Dependence Only (n=46) | Drug Dependence (n=51) |
|---|---|---|---|
| Age (mean years, SD)** | 41.6 (12.0) | 45.3(10.7) | 38.3(12.1) |
| Gender (% Female)* | 44.3% | 60.5% | 39.5% |
| Married/Cohabitating (%) | 44% | 47.8 | 41.1 |
| Ethnicity (% Caucasian) | 91.7% | 91.1 | 92.2 |
| Education (% with at least some college) | 58.7 | 63.0 | 54.9 |
| Currently employed (% part-, full-time)t | 43.3% | 52.2 | 35.3 |
| Current Smoker (%)** | 64.9% | 50 | 78.4 |
| Mood Disorder (e.g., Depression, Mood NOS, Dysthymia)t | 76.3 | 84.8 | 68.6 |
| Anxiety disorder | 21.6 | 28.3 | 15.6 |
Significant differences between Alcohol Dependence Only and Drug Dependence are indicated above by the following:
p<. 10
p<.05
p<.01
2.2. Measures
Demographic & Clinical Characteristics
Clinical records were screened for medical and psychiatric diagnoses. In addition, through self-report questionnaires, information was collected regarding participants' age, sex, level of education, marital status, employment status, and level of income. Participants were also asked to fill out a health questionnaire inquiring about the participants' health history and general health status, including medical conditions that might prevent or make it difficult to participate in a moderate intensity exercise program.
Engagement in current exercise program
To determine the current rates of substance abusing patients who were physically active, participants were queried on whether they regularly engage in an exercise program of moderate intensity activity for at least 20 uninterrupted minutes. Follow-up probes assessed the frequency (number of times per week) and length of time (weeks or months) that patients have been participating in exercise of this type. Participants were considered to be currently engaged in a regular exercise program if they were physically active for more than 20 minutes of moderate-intensity exercise, at least 3 times per week, over the course of the last 6 months. Individuals (with and without substance use problems) engaging in less than this level of physical activity have been considered sedentary in previous studies (Brown et al., 2009; Brown et al., 2010; Church, Earnest, Skinner, & Blair, 2007; Jakicic, Marcus, Gallagher, Napolitano, & Lang, 2003).
Exercise Preferences
Exercise preference items were adapted from items used with cancer patients (Karvinen, et al., 2006; Rogers, Malone, et al., 2009; Rogers, Markwell, Verhulst, McAuley, & Courneya, 2009; Vallance, et al., 2006). Participants in this study were asked their exercise preferences for the following: 1) type of activity (e.g., walking, running, gym equipment, swimming, organized sport), 2) timing of exercise initiation (early in drug treatment or several months after drug treatment participation), 3) company (alone, with others in drug treatment, with family), 4) location (home, community fitness center, at drug treatment setting), 5) intensity (low, moderate, vigorous), and 6) structure (supervised vs. self-paced, scheduled vs. spontaneous/flexible). In addition, participants were also asked whether they would have wanted to discuss how to incorporate physical activity into recovery during their current substance abuse treatment program as well as whether they would be interested in participating in an exercise program if it were offered to them.
Preferred Activity
Participants were provided with a list of 10 different types of physical activities (walking, running/jogging, strength/resistance training, sports, cycling, swimming, exercise videos, aerobic equipment at home, gym/YMCA, yoga/stretching) and were asked to rate their top three choices by indicating with “1” for their most preferred activity, followed by “2” and “3” for their next most preferred activities.
Exercise Program Scenarios
In an effort to determine the specific type of exercise program that could be developed for this substance abusing population, 3 types of exercise program “scenarios” were presented to the participants. They were asked to read them and rank them according to their preference. The 3 exercise program scenarios were presented as follows:
Program A: Do it Yourself – 1) Participate in a brief session with an exercise specialist to discuss the benefits of exercise and how to get started. 2) How, when and where you exercise will be solely determined by you.
Program B: Do it Yourself with Professional Guidance -- 1)be given fitness tools to help you monitor your progress (e.g., heart rate monitors, pedometers) OR a membership to a community fitness center where you could engage in exercise whenever it is convenient for you, 2) Exercise guidance and consultation will be provided by an exercise specialist. This will consist of an initial session and continued contact with the exercise specialist through brief phone calls and/or occasional visits to hospital's Fitness Facility. 3) How, when, and where you exercise will be determined by you, with guidance from the exercise specialist.
Program C: Relying on Professional Supervision -- 1) Attend the hospital's Fitness Facility at the same predetermined day and time each week for 12 weeks. At these weekly sessions, you will: a) Engage in aerobic exercise under the direction of an exercise specialist, and b) Participate in a group to learn about and discuss the benefits of physical activity. 2) How, when, and where you exercise during the week will be determined through discussions with the exercise specialist.
Perceived Benefits of Physical Activity
A modified version of the Motives for Physical Activity Measure (Frederick & Ryan, 1993)was used to assess motives (i.e., perceived benefits) for participating in physical activities. This measure was modified specifically for patients in substance abuse treatment. For example, additional items included “Be less likely to relapse”, “Experience less anxiety”, “Manage stress better”, “Feel stronger”, “Decrease my depression, “Increase my confidence to stay clean and sober”, “Decrease my urges and cravings to use alcohol and/or drugs”, and “Provide structure in my life”. All 21 statements of the measure were rated by the participant on a 7-point Likert scale ranging from 1 (not true at all for me) to 7 (very true for me).
Perceived Barriers to Physical Activity
Barriers to physical activity were assessed through an 18-item measure (Booth, et al., 1997)which classified barriers into five categories: (1) physical barriers, (2) emotional barriers, (3) motivational barriers, (4) time barriers, and (5) availability barriers. This instrument uses a 7-point Likert scale ranging from 1 (not true at all for me) to 7 (very true for me).
3. Results
3.1. Rates and Predictors of Exercise
A majority of participants (71%) were not currently engaged in a regular exercise program over the course of the six months prior to current substance abuse treatment engagement. That is, they did not participate in exercise of at least 20-minute bouts of moderate-intensity aerobic activity, 3 times per week. A number of demographic (age, gender, level of education, martial status, and ethnicity) and clinical characteristics (type of substance dependence, smoking status, mood and anxiety disorders) were examined as correlates of being engaged in a regular exercise program in the 6 months prior to substance abuse treatment. The only statistically significant finding that emerged involved those who were married or cohabiting being more likely to be engaged in a regular exercise program (χ2=4.28, df=1, p<.05).
3.2. Specific Exercise Preferences
Table 2 lists specific exercise preferences and responses for the overall sample, as well as highlights differences in preferences between men and women. While a majority (84.4%) of participants expressed openness (i.e., endorsed yes or maybe) to discussing exercise during their current substance abuse treatment program, women were significantly more likely than men to voice this interest (95.3% vs. 75.9%; χ2 = 6.68, df=1, p=.01). In addition, the level of interest in engaging in an exercise program significantly differed with respect of psychiatric comorbidity – 93.8% for those with both mood and anxiety, 69.4% for those with either disorder, and 44.4% for those without either disorder (χ2 = 18.37, df=4, p<.001). Interest in exercise was particularly strong for an exercise intervention if it was designed specifically for substance abusing patients receiving addiction treatment (94.8%; yes or maybe).
Table 2.
Overall and Gender-Specific Exercise Preferences of Patients in Substance Abuse Treatment(Significant associations are shaded. Refer to Results section for statistical parameters)
| Preference | Overall | Females | Males |
|---|---|---|---|
| 1. Would you have wanted to discuss how to develop your own exercise program at some point DURING your participation in the Hospital's Alcohol and Drug Treatment Services (ADTS) program? | |||
| YES | 50.0 | 66.7 | 37.0 |
| NO | 15.6 | 4.8 | 24.1 |
| MAYBE | 34.4 | 28.6 | 38.9 |
| 2. If an exercise program designed for persons in substance use recovery were offered to you, would you be interested in participating? | |||
| YES | 68.8 | 78.6 | 61.1 |
| NO | 5.2 | 2.4 | 7.4 |
| MAYBE | 26.0 | 19.0 | 34.5 |
| 3. With whom would you prefer to exercise? | |||
| Alone | 23.2 | 5.7 | 36.2 |
| With Others | 14.6 | 42.9 | 34.0 |
| No preference | 39.0 | 51.4 | 29.8 |
| 4. Where would you prefer to exercise? (More than one preference allowed) | |||
| Home | 34.4 | 30.9 | 37.0 |
| Gym/YMCA | 41.7 | 33.3 | 48.1 |
| Substance Abuse Treatment program | 9.4 | 16.6 | 3.7 |
| Outside | 41.7 | 50.0 | 35.2 |
| No preference | 26 | 30.9 | 22.2 |
| 5. When would you prefer to start an exercise program? | |||
| During substance use treatment | 50.5 | 53.7 | 48.1 |
| In the first 3 months of sobriety | 37.9 | 31.7 | 42.6 |
| 3–6 months after initiating sobriety | 9.5 | 12.2 | 7.4 |
| More than 6 months after initiating sobriety | 2.1 | 2.4 | 1.9 |
| 6. What intensity would you prefer your exercise program to be? | |||
| Low intensity (e.g., taking a leisurely stroll) | 11.7 | 9.8 | 13.2 |
| Moderate intensity (e.g., brisk walk) | 62.8 | 75.6 | 52.8 |
| High intensity (e.g., running) | 13.8 | 4.9 | 20.8 |
| No preference | 11.7 | 9.8 | 13.8 |
| 7. What type of activities would you like to perform ? | |||
| Same exercise each session | 25.5 | 41.9 | 11.8 |
| Different exercise each session | 74.5 | 58.1 | 88.2 |
| 8. How would you prefer to perform these exercises? | |||
| Supervised/instructed | 37.2 | 51.2 | 26.4 |
| Unsupervised/self-paced | 62.8 | 48.8 | 73.6 |
| 9. Would you be willing to wear a pedometer to keep track of your daily steps? | |||
| YES | 79.4 | 88.4 | 72.2 |
| NO | 5.2 | 0 | 9.3 |
| MAYBE | 15.5 | 11.6 | 18.5 |
| 10. Would you want to incorporate strength/resistance training into your exercise program? | |||
| YES | 70.5 | 65.8 | 74.1 |
| NO | 8.4 | 12.2 | 5.6 |
| MAYBE | 21.1 | 21.9 | 20.4 |
| 11. How would you prefer to engage in physical activity? | |||
| In one long bout of exercise (30–60 minutes) | 66.7 | 69.7 | 64.4 |
| In short bouts throughout the day when you can fit them in (10 minutes each time) | 20.5 | 27.3 | 15.6 |
| No preference | 12.8 | 3.0 | 20.0 |
In general, participants did not have a strong preference for the location of exercise: exercising outside, at a gym/YMCA, or at home were almost equally preferred. Men also did not have a preference regarding whether they exercised alone or with company; women, however, were less likely to prefer exercising alone compared to men (5.7% vs. 36.2%; χc2 = 10.85, df=2, p<.01). In terms of when to begin an exercise program relative to their substance abuse treatment, most participants expressed a preference to begin an exercise program early in their recovery (e.g. during their current treatment or first 3 months of recovery). While men and women reported similar preferences regarding the timing of an exercise program, patients receiving treatment for alcohol dependence only, compared to those for drug dependence, displayed a trend toward wanting to begin an exercise program earlier in their recovery (i.e., first 3 months of recovery versus later; χ2 = 3.60, df=1, p=.059).
In terms of the specific characteristics of an exercise program, most participants reported a preference for exercising at an intensity level that was moderate. Overall, participants wanted to engage in different exercises each session in a manner that was unsupervised, self-paced. However, this preference was primarily true for males; females reported approximately equal preferences for whether exercise was similar each session (χ2 = 11.11, df=1, p=.001) or whether it was supervised (χ2 = 6.09, df=1, p<.05). Most participants were interested in incorporating resistance/strength training and preferred to exercise in one long bout rather than multiple bouts throughout the day. Lastly, many participants reported a willingness to incorporate a pedometer in their exercise program. Pedometers were particularly appealing to women compared to men (χ2 = 4.20, df=1, p<.05), as well as to those receiving treatment for alcohol dependence only compared to drug dependence (χ2 = 4.76, df=1, p<.05).
Lastly, participants voiced a preference for receiving weekly information and support regarding their exercise program in the following formats: e-mail (46%), telephone calls (33%), and in-person sessions (37%).
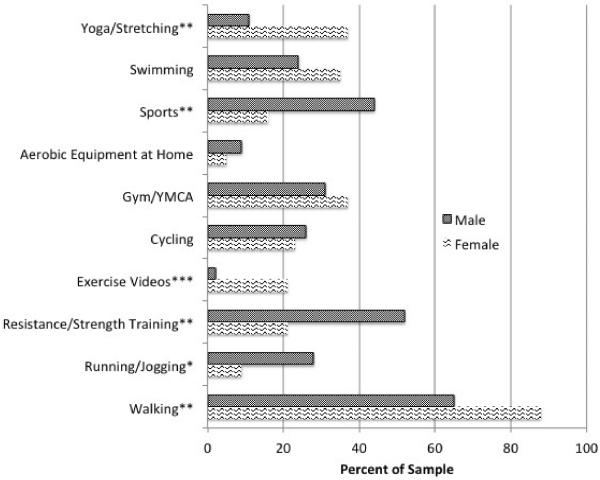
3.3. Preferred Type of Activity
When asked to rate their top three most preferred types of physical activity, walking (75%) emerged as the most preferred activity followed by strength/resistance training (37.1%), gym/YMCA (33%), sports (32%), swimming (27.8%), cycling (24.7%), yoga/stretching (21.6%), running (18.6%), exercise videos (9.3%), and utilizing home exercise equipment (7.2%). Few differences in preferred activity emerged between drug treatment type - alcohol dependent only patients were significantly more likely to prefer walking than the drug dependent individuals (84.8% vs. 66.7%; χ2 = 4.26, df=1, p<.039) and less likely to prefer sports (19.6% vs. 43.1%; χ2 = 6.18, df=1, p<.05). More differences, however, emerged when men and women were compared on their preferred activity (See Figure 1). Women, compared to men, were significantly more likely to prefer walking (88.4% vs. 64.8%; χ2 = 7.13, df=1, p<.01), use of exercise videos (20.9% vs. 0%; χ2 = 12.46, df=1, p<.001), and yoga (37.2% vs. 9.3%, χ2 = 11.03, df=1, p=.001) whereas they were significantly less likely to prefer running (9.3% vs. 25.9%, χ2 = 4.38, df=1, p<.05), strength/resistance training (20.9% vs. 50.0%; χ2 = 8.67, df=1, p<.01), and sports (16.3% vs. 44.4%; χ2 = 8.73, df=1, p<.01).
Figure 1.
Percentage of Males and Female Substance Abusing Patients who indicated the types of physical activity as their top 3 preferred choices.
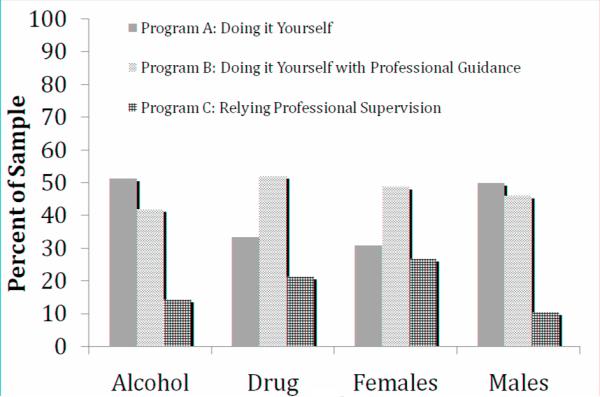
3.4. Exercise Program Type Preferences
Figure 2 displays the percent of the sample that ranked each program as their top choice by substance treatment type and sex. Program B: Do It Yourself with Profession Guidance was the most preferred program overall (47.3%) closely followed by Program A: Do It Yourself (41.8%). The least preferred program was Program C: Relying on Professional Supervision (18.0%). There were no statistically significant differences across program preferences between substance treatment type and sex.
Figure 2.
Exercise Program Scenarios: Percent of sample rated most preferred
3.5. Perceived Benefits and Barriers to Engaging in Exercise
The highest rated perceived benefits of engaging in exercise for the entire sample included (beginning with the highest): a sense of accomplishment, feeling stronger, improved health, becoming physically fit, and increased confidence in staying clean and sober. While there were no differences in the perceived benefits of substance treatment type, men and women differed in their perceptions of several benefits of exercise. Females rated the following perceived benefits significantly higher than males: manage stress better (6.28 vs. 5.70, t=2.26, df=80, p<.05), increased confidence to stay clean and sober (6.42 vs. 5.83, t=2.19, df=81, p<.05), and help me make new friends (5.14 vs. 4.19, t=2.26, df=92, p<.05).
The highest rated perceived barriers of engaging in exercise included (beginning with the highest): not being able to afford it, too lazy/not motivated/can't get started, not having the energy, would not be able to keep up, and not having anyone to do it with. There were no differences in the perceived barriers of substance treatment type and comparisons between males and females revealed only one difference regarding barriers related to health. Men were more likely than women to report having an injury or disability that would stop them from being able to exercise (2.94 vs. 1.95, t=2.29, df=95, p<.05).
4. Discussion
The findings from this study point toward high levels of interest in incorporating exercise into one's recovery from alcohol and other substance use disorders, yet low rates of involvement in exercise programs. Given that exercise interventions may provide an effective, low-cost adjunct to substance abuse treatment with numerous secondary health benefits (Penedo & Dahn, 2005), it is important to understand patients' preferences with regard to exercise program participation. Identification of these patient preferences can provide critical information needed to guide development of more tailored intervention programs; such programs may, in turn, be more successful at engaging and retaining participants. Our findings clarified a number of these preferences, as well as the benefits of and barriers to participation, as perceived by patients. In addition to elucidating general preferences for incorporating exercise into substance abuse treatment, we also explored whether differences existed between men and women, and between those seeking treatment for alcohol dependence only versus drug dependence with or without alcohol problems.
Overall, results suggest that individuals seeking substance abuse treatment are quite open to discussing exercise as part of their treatment regimen. Nearly 85% of respondents indicated that they would be amenable to talking about their exercise patterns during their substance abuse treatment, even early in recovery, and the majority of these indicated willingness to enroll in an exercise program tailored for patients in substance use recovery. This suggests that during the height of their addiction, when they were actively using alcohol and/or drugs, they may not have been able to prioritize or follow-through with an exercise program. However, given even a brief period of sobriety, participants were able to recognize and be interested in incorporating regular physical activity into their lives and as a potentially important part of their recovery.
Although a range of activities were rated to be of interest to survey respondents (ie., strength/resistance training, sports, jogging, yoga), walking emerged as the overwhelmingly preferred type of physical activity. This finding is consistent with exercise literature on activity preferences for adults. For example, Croteau(2004) examined self-selected strategies to increase physical activity in a lifestyle intervention and found that the primary strategy consisted of walking – during work, before and after work, during lunch, with the dog, to a store, and while traveling. Walking interventions have resulted in significant improvements in both physical and psychological well-being. For example, in a meta-analysis of 24 randomized controlled trials (Murphy, Nevill, Murtagh, & Holder, 2007), walking significantly increased aerobic fitness, decreased body weight, body mass index, percent body fat, and resting diastolic blood pressure. Other studies have found that walking decreases tension and anxiety(Murphy, Nevill, Neville, Biddle, & Hardman, 2002), reduces depressive symptomatology (Armstrong & Edwards, 2004) and improves mood disturbance (Osei-Tutu & Campagna, 2005). Importantly, walking and brief bouts of physical activity have also been associated with decreased urges to drink or smoke cigarettes (Taylor, Ussher, & Faulkner, 2007; Ussher, et al., 2004). These findings for walking interventions are comparable to those demonstrated with more structured, supervised exercise programs. Therefore, a walking intervention may be an effective approach for increasing physical activity and increasing physical and psychological health benefits among substance abusing patients in early recovery.
In terms of perceived barriers, lack of motivation was identified as one of the greatest barriers for involvement in exercise. Additionally, almost all participants, but particularly females were willing to wear a pedometer as part of their exercise program. Pedometers have been used to improve self-monitoring, facilitate goal setting, and enhance motivation in numerous exercise intervention studies (Croteau, 2004; Merom et al., 2007; Murphy, et al., 2007). The inclusion of pedometers in an exercise intervention for substance abusing patients may play an important role in increasing participant motivation and increase self-monitoring. In addition, the use of monetary incentives has been utilized in previous exercise intervention studies as a means of increasing motivation and adherence (Jeffery, Wing, Thorson, & Burton, 1998; Robison et al., 1992). Given that contingency management approaches have been efficacious in substance abusing populations (Higgins & Petry, 1999), utilizing a similar approach within exercise interventions for patients in substance abuse treatment may be an effective strategy for increasing motivation in this population.
While both male and female respondents voiced strong enthusiasm for exercise, it is notable that several key gender differences emerged with regard to the type of exercise that appeals to women vs. men, as well as the perceived benefits of engaging in an exercise-based intervention. For example, in comparison to men, women expressed greater interest in exercising with others as opposed to exercising alone. Women were also more open than their male counterparts in initiating involvement in an exercise program based in the same treatment facility as their substance abuse treatment program, and were more open to having the exercise program be supervised rather than unstructured. Men were most interested in exercise programs that included varied activities at each session; although many women also expressed this interest, a higher proportion of them preferred programs that repeated the same type of exercise activity at each session. More so than the men in our sample, women viewed exercise as a means of managing stress, staying sober, and connecting with others socially. Thus some of the perceived benefits for exercise participation also vary by gender.
In addition, perhaps some of the most striking gender differences that emerged were those with regard to preference for specific types of exercise activities. Whereas both males and females voiced strong interest in walking, this activity was particularly highly rated among women. Moreover, as noted previously, significantly more women indicated that they would be willing to wear a pedometer. Yoga, stretching and use of exercise videos were also significantly more appealing to women. Men, on the other hand, were more likely than women to endorse interest in sports, strength training and running. These findings are not surprising in that they generally mirror overall patterns of exercise choice among women vs. men (Booth, et al., 1997). However, these patterns are critical to keep in mind as new intervention programs are developed for individuals in substance use recovery. Such interventions may be most successful if they are either tailored directly for women vs. men -- or if they are flexibly designed so that appealing options are available for both gender groups.
In addition to gender differences in exercise preferences, a study examining the relationship between physical activity and alcohol use in a large, population-based sample in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), found that gender moderated this relationship (Lisha, Martens, & Leventhal, 2011). Males demonstrated a stronger relationship between physical activity and alcohol use, which the authors of the study posited could be due to the greater involvement of organized sports (in which alcohol consumption may be part of the sporting culture) by males than females. The results of the current study suggest that males are very interested in engaging in sports and therefore, exercise interventions that involve increasing sport participation should consider any risks associated with social drinking or drug use in that context. Another important gender difference related to physical activity involvement involves motives for exercise. Research studies have clearly demonstrated that men are motivated by the attainment of such positive outcomes related to increased physical activity as strength, endurance, social recognition, and feeling challenged(Kilpatrick, Hebert, & Bartholomew, 2005). On the other hand, women are more motivated by the avoidance of negative consequences such as weight gain (Kilpatrick, et al., 2005). Incorporating these unique motives in addition to helping substance abusing patients make the connection between increased physical activity and potentially better substance abuse treatment outcomes may result in increased motivation to adopt and adhere to a long-term exercise program.
Although less so than differences by gender, some differences were also observed between individuals seeking treatment for alcohol use only vs. those seeking treatment for other substance use disorders. Alcohol dependent patients voiced a stronger interest in starting an exercise intervention early in their recovery, and were also more open to wearing a pedometer. Patients seeking drug treatment were slightly more likely overall to voice interest in engaging in an exercise program as part of their recovery.
Interestingly, patients with mood and anxiety disorders were more likely to express an interest in engaging in an exercise program as a part of their substance abuse treatment. There is a large, growing body of evidence that aerobic exercise has beneficial effects on psychological functioning (see Taylor & Faulkner, 2008). Both cross-sectional and prospective correlational studies have demonstrated an inverse relationship between depression, anxiety, and physical activity. Further, aerobic exercise interventions have consistently been shown to be efficacious in improving mental health outcomes among patients diagnosed with depression and anxiety. Furthermore, exercise may be a particularly suitable intervention for individuals with depressive symptoms as it appears that depression has actually been associated with increased adherence to exercise in some studies (Patten, Vickers, Martin, & Williams, 2003). Given these mood-enhancing effects of exercise, interventions targeting increased physical activity among substance abusers may also demonstrate decreased mood and anxiety.
Given the exercise preferences, benefits, and barriers to physical activity identified in this study, the next logical step is to incorporate these findings into intervention development. There has been recent interest in the effectiveness of lifestyle physical activity (LPA) interventions (as opposed to supervised, structured exercise programs). Dunn, Andersen, &Jakicic(1998)define lifestyle physical activity as “daily accumulation of at least 30 minutes of self-selected activities, which include all leisure, occupational, or household activities that are at least moderate to vigorous in their intensity and could be planned or unplanned activities that are part of everyday life.” Bolstered by findings that prescribing short bouts of physical activity was associated with increased adherence (Jakicic, Wing, Butler, & Robertson, 1995), lifestyle physical activity interventions have consisted of utilizing behavioral strategies to guide individuals to engage in intermittent bouts of physical activity throughout the day (e.g, brisk walking, using the stairs, gardening, parking car farther away). As such LPAs have the potential to address common barriers to exercise and are sufficiently flexible to incorporate individual preferences thereby, promoting increased adherence. While, to date, there have not been any studies examining lifestyle physical activity interventions for substance abusing patients, LPA interventions may be a good “fit” and more generalizable for a substance abusing population experiencing the newfound demands of early recovery due to its flexibility, low cost, and easy integration into daily lives.Assessing whether such lifestyle interventions are efficacious in terms of assisting treatment for substance abuse should be a research priority.
Several study limitations should be noted. First, the sample size is relatively small (N=97) and participants were all currently engaged in substance abuse treatment. Although it is important to ascertain the preferences and barriers of patients who are actually motivated to seek some form of treatment for their addiction, it is unknown whether our findings can generalize to non-treatment seeking patients in the community. Further, the exercise preferences assessment was modified from the work conducted primarily with cancer patients. While attempts were made to modify existing questions for use with a substance abusing population, psychometric work with these measures will contribute to the quality of data obtained in future studies. In addition, the study sample was primarily Caucasian; racial and ethnic minority patients with substance abuse problems may have different treatment preferences and barriers. Finally, all data were obtained via chart review and administration of self-report questionnaires; diagnostic interviews were not conducted to clarify substance abuse and/ or other psychiatric diagnoses. While self-report surveys are regarded as a useful method for obtaining patient preferences (e.g., Vallance, et al., 2006) the lack of an interview format for obtaining preferences does have some limitations, such as lack of the ability to re-word questions that may be unclear.
Despite these limitations, working to develop acceptable and uniquely-tailored exercise interventions is a worthwhile endeavor given that increased physical activity during substance use treatment could provide some definite advantages. Increased physical activity offers the potential for improved health and wellness, as the physiological health benefits of physical activity have been well documented (Penedo & Dahn, 2005; USDHHS, 1996). Increasing physical activity also has the potential to be cost-effective, flexible, and accessible; many forms of lifestyle physical activity (e.g., walking, going up and down stairs, parking farther away, doing housework and gardening, exercise videos) may be conducted independently, either at home or outdoors, and associated costs are likely to be minimal. Finally, engaging in physical activity has minimal side effects (e.g., Broocks et al., 1998). With the use of proper precautions for prevention of injuries (American College of Sports Medicine, 2000), engaging in physical activity carries with it relatively low risk of adverse events. Given each of these benefits, if acceptable and efficacious exercise interventions can be established, substance dependent patients will be provided with a valuable adjunct to their ongoing substance abuse treatment.
In conclusion, these study findings underscore the importance of developing tailored approaches for incorporating exercise into substance use recovery. Patients voice strong interest in such programs, yet to date, such programs have noted difficulties with recruitment and retention of participants. Targeting specific groups of substance using individuals, e.g., programs for women or men only, or programs targeting individuals in recovery from alcohol vs. drug use – may allow programs to be more successful by meeting the unique needs of the population they are trying to serve.
Highlights
Patients in substance abuse treatment exhibit low rates of physical activity
There is high interest in beginning an exercise program in early recovery
Male and female substance abusing patients have different exercise preferences
Using preferences to tailor interventions may aid the effectiveness of future work
Acknowledgements
This research was supported by a NIDA-funded Mentored Patient-Oriented Career Development Award to Dr. Ana Abrantes (K23 DA019950-01)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American College of Sports Medicine . Guidelines for exercise testing and prescription. Lippincott, Williams and Wilkins; New York: 2000. [Google Scholar]
- Armstrong K, Edwards H. The effectiveness of a pram-walking exercise programme in reducing depressive symptomatology for postnatal women. International Journal of Nursing Practice. 2004;10:177–194. doi: 10.1111/j.1440-172X.2004.00478.x. [DOI] [PubMed] [Google Scholar]
- Battle CL, Uebelacker L, Friedman MA, Cardemil EV, Beevers CG, Miller IW. Treatment goals of depressed outpatients: a qualitative investigation of goals identified by participants in a depression treatment trial. Journal of Psychiatric Practice. 2010;16:425–430. doi: 10.1097/01.pra.0000390763.57946.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth ML, Bauman A, Owen N, Gore CJ. Physical activity preferences, preferred sources of assistance, and perceived barriers to increased activity among physically inactive Australians. Preventive Medicine. 1997;26:131–137. doi: 10.1006/pmed.1996.9982. [DOI] [PubMed] [Google Scholar]
- Broocks A, Bandelow B, Pekrun G, George A, Meyer T, Bartmann U, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. American Journal of Psychiatry. 1998;155:603–609. doi: 10.1176/ajp.155.5.603. [DOI] [PubMed] [Google Scholar]
- Brown RA, Abrantes AM, Read JP, Marcus BH, Jakicic J, Strong DR, et al. Aerobic exercise for alcohol recovery: Rationale, program description, and preliminary findings. Behavior Modification. 2009;33:220–249. doi: 10.1177/0145445508329112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Abrantes AM, Read JP, Marcus BH, Jakicic J, Strong DR, et al. A Pilot Study of Aerobic Exercise as an Adjunctive Treatment for Drug Dependence. Mental Health &Physical Activity. 2010;3:27–34. doi: 10.1016/j.mhpa.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownell KD, Marlatt GA, Lichtenstein E, Wilson GT. Understanding and preventing relapse. American Psychologist. 1986;41:765–782. doi: 10.1037//0003-066x.41.7.765. [DOI] [PubMed] [Google Scholar]
- Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure. JAMA: Journal of the American Medical Association. 2007;297:2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- Collingwood TR, Sunderlin J, Reynolds R, Kohl HW., 3rd. Physical training as a substance abuse prevention intervention for youth. Journal of Drug Education. 2000;30:435–451. doi: 10.2190/RVUE-9XW7-TYRQ-EJR8. [DOI] [PubMed] [Google Scholar]
- Croteau KA. Strategies used to increase lifestyle physical activity in a pedometer-based intervention. Journal of Allied Health. 2004;33:278–281. [PubMed] [Google Scholar]
- Dunn AL, Andersen RE, Jakicic JM. Lifestyle physical activity interventions. History, short- and long-term effects, and recommendations. American Journal of Preventive Medicine. 1998;15:398–412. doi: 10.1016/s0749-3797(98)00084-1. [DOI] [PubMed] [Google Scholar]
- Finney JW, Moos RH, Timko C. Addictions: A Comprehensive Guidebook. 1999. The course of treated and untreated substance use disorders: Remission and resolution, relapse and mortality; pp. 30–49. [Google Scholar]
- Frederick CM, Ryan RM. Differences in motivation for sport and exercise and their relationships with participation and mental health. Journal of Sport Behavior. 1993;16:125–145. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Petry NM. Contingency management. Incentives for sobriety. Alcohol research & health: The Journal of the National Institute on Alcohol Abuse and Alcoholism. 1999;23:122–127. [PMC free article] [PubMed] [Google Scholar]
- Hunt WA, Barnett LW, Branch LG. Relapse rates in addiction programs. Journal of Clinical Psychology. 1971;27:455–456. doi: 10.1002/1097-4679(197110)27:4<455::aid-jclp2270270412>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Institue of Medicine [accessed August 3, 2011];Crossing the quality chasm: A new health care system for the 21st century. 2001 (available at http://www.iom.edu/Reports/2001/Crossing-the-Quality-Chasm-ANew-Health-System-for-the-21st-Century.aspx,)
- Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women. JAMA: Journal of the American Medical Association. 2003;290:1323–1330. doi: 10.1001/jama.290.10.1323. [DOI] [PubMed] [Google Scholar]
- Jakicic JM, Wing RR, Butler BA, Robertson RJ. Prescribing exercise in multiple short bouts versus one continuous bout: effects on adherence, cardiorespiratory fitness, and weight loss in overweight women. International Journal of Obesity and Related Metabolic Disorders. 1995;19:893–901. [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Thorson C, Burton LR. Use of personal trainers and financial incentives to increase exercise in a behavioral weight-loss program. Journal of Consulting and Clinical Psychology. 1998;66:777–783. doi: 10.1037//0022-006x.66.5.777. [DOI] [PubMed] [Google Scholar]
- Karvinen KH, Courneya KS, Campbell KL, Pearcey RG, Dundas G, Capstick V, et al. Exercise preferences of endometrial cancer survivors: a population-based study. Cancer Nursing. 2006;29:259–265. doi: 10.1097/00002820-200607000-00001. [DOI] [PubMed] [Google Scholar]
- Karvinen KH, Courneya KS, Venner P, North S. Exercise programming and counseling preferences in bladder cancer survivors: a population-based study. Journal of Cancer Survivors. 2007;1:27–34. doi: 10.1007/s11764-007-0010-5. [DOI] [PubMed] [Google Scholar]
- Kilpatrick M, Hebert E, Bartholomew J. College students' motivation for physical activity: differentiating men's and women's motives for sport participation and exercise. Journal of American College Health. 2005;54:87–94. doi: 10.3200/JACH.54.2.87-94. [DOI] [PubMed] [Google Scholar]
- Laine C, Davidoff F. Patient-centered medicine. A professional evolution. JAMA: The Journal of the American Medical Association. 1996;275:152–156. [PubMed] [Google Scholar]
- Larimer ME, Palmer RS, Marlatt GA. Relapse prevention. An overview of Marlatt's cognitive-behavioral model. Alcohol Research and Health. 1999;23:151–160. [PMC free article] [PubMed] [Google Scholar]
- Lisha NE, Martens M, Leventhal AM. Age and gender as moderators of the relationship between physical activity and alcohol use. Addictive Behaviors. 2011;36:933–936. doi: 10.1016/j.addbeh.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe SS, Watanabe SM, Baracos VE, Courneya KS. Physical activity interests and preferences in palliative cancer patients. Supportive Care in Cancer. 2010;18:1469–1475. doi: 10.1007/s00520-009-0770-8. [DOI] [PubMed] [Google Scholar]
- Lynch WJ, Piehl KB, Acosta G, Peterson AB, Hemby SE. Aerobic exercise attenuates reinstatement of cocaine-seeking behavior and associated neuroadaptations in the prefrontal cortex. Biological Psychiatry. 2010;68:774–777. doi: 10.1016/j.biopsych.2010.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Donovan DM. Relapse Prevention: Maintenance strategies in the treatment of addictive behaviors. Second Edition Guildford Press; New York: 2005. [Google Scholar]
- Merom D, Rissel C, Phongsavan P, Smith BJ, Van Kemenade C, Brown WJ, et al. Promoting walking with pedometers in the community: the step-by-step trial. American Journal of Preventive Medicine. 2007;32:290–297. doi: 10.1016/j.amepre.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Murphy M, Nevill A, Neville C, Biddle S, Hardman A. Accumulating brisk walking for fitness, cardiovascular risk, and psychological health. Medicine and Science in Sports and Exercise. 2002;34:1468–1474. doi: 10.1097/00005768-200209000-00011. [DOI] [PubMed] [Google Scholar]
- Murphy MH, Nevill AM, Murtagh EM, Holder RL. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Preventive Medicine. 2007;44:377–385. doi: 10.1016/j.ypmed.2006.12.008. [DOI] [PubMed] [Google Scholar]
- ONDCP . The Economic Costs of Drug Abuse in the United States 1192–2002. 2004. [Google Scholar]
- Osei-Tutu KB, Campagna PD. The effects of short- vs. long-bout exercise on mood, VO2max, and percent body fat. Preventive Medicine. 2005;40:92–98. doi: 10.1016/j.ypmed.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Patten CA, Vickers KS, Martin JE, Williams CD. Exercise interventions for smokers with a history of alcoholism: exercise adherence rates and effect of depression on adherence. Addictive Behaviors. 2003;28:657–667. doi: 10.1016/s0306-4603(01)00280-5. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18:189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Read JP, Brown RA. The role of physical exercise in alcoholism treatment and recovery. Professional Psychology: Research and Practice. 2003;34:49–56. [Google Scholar]
- Read JP, Brown RA, Marcus BH, Kahler CW, Ramsey SE, Dubreuil ME, et al. Exercise attitudes and behaviors among persons in treatment for alcohol use disorders. Journal of Substance Abuse Treatment. 2001;21:199–206. doi: 10.1016/s0740-5472(01)00203-3. [DOI] [PubMed] [Google Scholar]
- Robison JI, Rogers MA, Carlson JJ, Mavis BE, Stachnik T, Stoffelmayr B, et al. Effects of a 6-month incentive-based exercise program on adherence and work capacity. Medicine and Science in Sports and Exercise. 1992;24:85–93. [PubMed] [Google Scholar]
- Roessler KK. Exercise treatment for drug abuse--a Danish pilot study. Scandanavian Journal of Public Health. 2010;38:664–669. doi: 10.1177/1403494810371249. [DOI] [PubMed] [Google Scholar]
- Rogers LQ, Courneya KS, Verhulst S, Markwell SJ, McAuley E. Factors associated with exercise counseling and program preferences among breast cancer survivors. Journal of Physical Activity and Health. 2008;5:688–705. doi: 10.1123/jpah.5.5.688. [DOI] [PubMed] [Google Scholar]
- Rogers LQ, Malone J, Rao K, Courneya KS, Fogleman A, Tippey A, et al. Exercise preferences among patients with head and neck cancer: prevalence and associations with quality of life, symptom severity, depression, and rural residence. Head& Neck. 2009;31:994–1005. doi: 10.1002/hed.21053. [DOI] [PubMed] [Google Scholar]
- Rogers LQ, Markwell SJ, Verhulst S, McAuley E, Courneya KS. Rural breast cancer survivors: exercise preferences and their determinants. Psychooncology. 2009;18:412–421. doi: 10.1002/pon.1497. [DOI] [PubMed] [Google Scholar]
- Sinyor D, Brown T, Rostant L, Seraganian P. The role of a physical fitness program in the treatment of alcoholism. Journal of Studies on Alcohol. 1982;43:380–386. doi: 10.15288/jsa.1982.43.380. [DOI] [PubMed] [Google Scholar]
- Smit E, Crespo CJ, Semba RD, Jaworowicz D, Vlahov D, Ricketts EP, et al. Physical activity in a cohort of HIV-positive and HIV-negative injection drug users. AIDS Care. 2006;18:1040–1045. doi: 10.1080/09540120600580926. [DOI] [PubMed] [Google Scholar]
- Smith MA, Schmidt KT, Iordanou JC, Mustroph ML. Aerobic exercise decreases the positive-reinforcing effects of cocaine. Drug and Alcohol Dependence. 2008;98:129–135. doi: 10.1016/j.drugalcdep.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevinson C, Capstick V, Schepansky A, Tonkin K, Vallance JK, Ladha AB, et al. Physical activity preferences of ovarian cancer survivors. Psychooncology. 2009;18:422–428. doi: 10.1002/pon.1396. [DOI] [PubMed] [Google Scholar]
- Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. The Journal of Family Practice. 2000;49:796–804. Clinical TrialRandomized Controlled TrialResearch Support, Non-U.S. Gov't. [PubMed] [Google Scholar]
- Taylor AH, Faulkner G. Inaugural editorial. Mental Health and Physical Activity. 2008;1:1–8. [Google Scholar]
- Taylor AH, Ussher MH, Faulkner G. The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect and smoking behaviour: a systematic review. Addiction. 2007;102:534–543. doi: 10.1111/j.1360-0443.2006.01739.x. [DOI] [PubMed] [Google Scholar]
- USDHHS . Physical Activity and Health: A Report of the Surgeon General. Centers for Disease Control and Prevention, National Center for Chronic Disease Control and Prevention; Atlanta, GA: 1996. [Google Scholar]
- Ussher M, Sampuran AK, Doshi R, West R, Drummond DC. Acute effect of a brief bout of exercise on alcohol urges. Addiction. 2004;99:1542–1547. doi: 10.1111/j.1360-0443.2004.00919.x. [DOI] [PubMed] [Google Scholar]
- Ussher M, Stanbury L, Cheeseman V, Faulkner G. Physical activity preferences and perceived barriers to activity among persons with severe mental illness in the United Kingdom. Psychiatric Services. 2007;58:405–408. doi: 10.1176/ps.2007.58.3.405. [DOI] [PubMed] [Google Scholar]
- Vallance JK, Courneya KS, Jones LW, Reiman T. Exercise preferences among a population-based sample of non-Hodgkin's lymphoma survivors. European Journal of Cancer Care (Engl) 2006;15:34–43. doi: 10.1111/j.1365-2354.2005.00617.x. [DOI] [PubMed] [Google Scholar]
- Wanko NS, Brazier CW, Young-Rogers D, Dunbar VG, Boyd B, George CD, et al. Exercise preferences and barriers in urban African Americans with type 2 diabetes. The Diabetes Educator. 2004;30:502–513. doi: 10.1177/014572170403000322. [DOI] [PubMed] [Google Scholar]
- Weinstock J. A review of exercise as intervention for sedentary hazardous drinking college students: rationale and issues. Journal of American College Health. 2010;58:539–544. doi: 10.1080/07448481003686034. Research Support, N.I.H., ExtramuralReview. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie H, McHugo GJ, Fox MB, Drake RE. Substance abuse relapse in a ten-year prospective follow-up of clients with mental and substance use disorders. Psychiatric Services. 2005;56:1282–1287. doi: 10.1176/appi.ps.56.10.1282. [DOI] [PubMed] [Google Scholar]