Abstract
We examined an at-risk population in China, money boys (MBs), to evaluate their potential role for transmitting HIV and sexually transmitted infections (STIs). Data were collected from 418 MBs selected by time-location cluster sampling, using a self-administered computerized questionnaire and testing a small blood sample for HIV/STIs. One-third (32.1%) of participants self-identified as homosexual, 25.4% heterosexual, 33.5% bisexual, and 9.1% uncertain. Consistent condom use by participants was 70–80% with commercial sex partners, 43.9% with girlfriends, and 60–70% with other non-commercial partners. HIV prevalence was 3.3%; syphilis, 10.5%; and HSV-2, 11.0%; overall prevalence for any was 20.3%. Factors significantly associated with HIV/STIs included being minority (OR = 4.82), having only male partners (OR = 1.92), having more male casual partners in the last 6 months (OR = 1.28), being younger at sexual debut (OR = 1.14), and being older (OR = 1.11). This study emphasizes the importance of developing targeted interventions for MBs, particularly those who are homosexual or minority.
Keywords: Money boys, Male sex workers, HIV, Sexually transmitted infections (STIs), Condom use, Risk factors, China
Introduction
China has been increasingly responsive to the social issue of HIV/STIs among MSM (men who have sex with men) and its consequences of transmitting the epidemic to other populations [1]. It is estimated that there are approximately 10–20 million MSM in China [2]. Many surveys have revealed that unprotected sexual activities are common among MSM [3–8].
As a subset of MSM, male sex workers (MSWs) have been studied internationally for over 20 years. Previous studies in several developing countries indicated that MSWs who have risky behaviors were vulnerable to HIV/STIs (sexually transmitted infections) [9–12]. A survey in Mumbai reported an HIV prevalence of 33% among MSWs [11]. A longitudinal study in Moscow reported an HIV prevalence of 16% at baseline and an incidence of 4.8 per 100 person years during a 6 month follow-up [10]. A 10 year follow-up study of MSWs in London reported 9% baseline HIV prevalence and an incidence rate of 3.7 per 100 person years [13]. The major factors reported to be associated with MSWs’ risk behaviors or HIV infection are age, education level, duration of sex work, migration patterns, financial status, drug and alcohol intake, sexual orientation, being receptive during anal intercourse, and having an STI history [9, 11, 14–17].
“Money boys (MBs)” (a sub-group of MSWs who sell sex to men instead of exclusively to women), who typically sell sex to MSM and sometimes to female clients as well, appear to be a core HIV transmitter group for MSM and the general population in China. Until recently, MBs have not been extensively studied in China. However, initial studies have shown that they may contribute to the growing HIV/STI epidemic among MSM, and may also act as a bridge to transmit HIV/STIs to the general population [13, 14, 18, 19].
Although commercial sex is illegal in China, it is rampant in many cities, especially in commercialized cities such as Shenzhen. MBs are a hidden and marginalized group, and are thus very hard to reach. Recently the Chinese government launched a large-scale counseling and testing program targeting MSM. This program involves participation of many MSM non-governmental organizations (NGOs). As a result, more MBs can now be reached for interventions and studies. Through a systematic search of the literature, we found four reported quantitative surveys and one qualitative focus group report about MBs in China [14, 18–22]. They report that MBs have limited knowledge of HIV/STIs, have sex partners of both genders, have a high prevalence of risky sexual behaviors, and are therefore in need of intervention activities.
In surveys asking sensitive questions, researchers are always concerned about the accuracy of self-reported data, because participants tend to conceal or under-report their risky behaviors, due to social desirability bias or concern about confidentiality [23–28], particularly those involved in illegal commercial sex. Their answers may also vary with different interviewers. Computer-assisted self-administered interviews (CASI) are a standard tool to reduce the variability between interviewers by using a prerecorded questionnaire [29–36].
This study was conducted from June to October, 2009 in Shenzhen, one of the highly developed and commercialized cities in southern China with a large migrant population. Shenzhen has many entertainment venues where MBs can be hired. The main types are dorm-based venues (providing only dormitories for MBs who are advertised on the internet, but leave to meet clients; called “dorms” herein), gay bars, and massage parlors.
Methods
This study used a cross-sectional design to survey MBs who were working at dorm-based venues, gay bars, and massage parlors. Participants were asked to self-administer a computer-based questionnaire and donate a 5 ml blood sample for testing for HIV, syphilis, and HSV-2 antibodies. To locate eligible participants, the research team compiled and continually updated a detailed list of all MB venues in Shenzhen, including location, phone numbers, and approximate numbers of MBs working in each venue. The list contained 30–40 dorm-based venues, six gay bars, and four massage parlors in Shenzhen.
Time-location cluster sampling was employed. Each month, 16 venues were randomly selected based on estimated workload, as well as two alternate venues for refusals. For each selected venue, a peak period in a 1 week timeframe was randomly selected. The research team arranged for site visits at the selected times for five consecutive months until the sample size was achieved. In total, we successfully completed data collection from 418 MBs in the selected study venues who reported being paid for sex within the past 30 days.
Both screening and confirmatory testing were done for HIV and syphilis, but only screening for HSV-2. Syphilis antibody was qualitatively screened for with Rapid Plasma Regain (Rongsheng Biotech Inc., Shanghai, China) and confirmed by Treponema Pallidum Particle Agglutination Assay (Fujirebio Inc., Japan). HIV antibody was detected using a rapid test (Abbott Laboratories, IL, USA) and the enzyme-linked immunosorbent assay (ELISA; Wantai Biotech Inc., Beijing, China), and confirmed by Western blot (Genlabs Diagnostics, Singapore). HSV-2 antibody was detected by ELISA (Trinity Biotech, USA).
This study was approved by the UCLA Institutional Review Board (#G08-11-030) and the Shenzhen Center for Disease Control.
Measurements and Data Analysis
Data collected in this survey included socio-demographic characteristics, level of HIV/AIDS knowledge, STI history, current HIV/STI sero-status, and sexual behaviors (including gender and numbers of different types of sex partners, condom use rates, position during anal intercourse, lubricant use, and condom breakage). Condom use rates were measured by an ordinal scale of “every time”, “often”, “occasionally”, and “never”, but recoded as a binary variable (1, consistent use: every time; 0: not consistent use) for logistic regression analyses. Numbers of casual partners and girlfriends were recoded into ordinal categorical variables.
SPSS 15.0 and STATA 9.2 were used for all statistical analyses. Pearson chi-square analysis was used to test for associations between sexual orientation and sexual behaviors. The Kruskal–Wallis non-parametric test was used to examine the associations of sexual orientation and count variables, such as the numbers of different partners and monthly sexual encounters. The Wilcoxon signed rank sum test was used to compare condom use by MBs with male clients and all other types of partners. Ordinal logistic regression analyses were attempted to identify potential factors associated with condom use rates by MBs with different types of partners, because the dependent variable, condom use, was ordinal. However, we found that the proportional odds assumption was violated in our regression models, so we recoded the condom use rates into binary variables and performed logistic regression analyses. Logistic regression analyses examined the associations between HIV/STIs and relevant factors. When performing logistic regression analyses, univariate analyses were first done to select variables for inclusion in models based on these results and the hypothesized relationships to outcomes. Other potential factors that might be associated with outcomes were also included in regression models, such as age, education level, income, duration of being MB, and level of HIV/AIDS knowledge. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were obtained from the results of logistic regression analyses.
Results
Socio-Demographic Characteristics
A total of 418 participants (after excluding four with poor data quality) were recruited; 246 (58.9%) were from 26 dorm-based venues, 122 (29.2%) from six gay bars, and 50 (12.0%) from two massage parlors. Four MBs refused to give blood samples and were excluded. Table 1 presents the socio-demographic characteristics of the participants.
Table 1.
Socio-demographic characteristics of venue-based MBs in Shenzhen, China
| Characteristics | Venue type n (%)
|
Average na (%) (N = 418) | χ2b | P-value | ||
|---|---|---|---|---|---|---|
| Dorms (N = 246) | Gay bars (N = 122) | Massage parlors (N = 50) | ||||
| Age (yrs), mean | 23.6 | 22.7 | 25.3 | 23.6 | 7.65c | 0.001 |
| Duration of being MB (yrs), mean | 0.9 | 0.8 | 1.0 | 0.9 | 0.46c | 0.630 |
| Hometown location | 5.87 | 0.053 | ||||
| Urban | 92 (37.4) | 39 (32.0) | 10 (20.0) | 141 (33.7) | ||
| Rural | 154 (62.6) | 83 (68.0) | 40 (80.0) | 277 (66.3) | ||
| Migration status | 6.05 | 0.048 | ||||
| Local resident | 19 (7.7) | 2 (1.6) | 2 (4.0) | 23 (5.7) | ||
| Migrant | 227 (92.3) | 120 (98.4) | 48 (96.0) | 395 (94.3) | ||
| Residence in Shenzhen | 40.97d | 0.000 | ||||
| < 1 month | 63 (26.6) | 15 (12.5) | 1 (2.0) | 79 (19.4) | ||
| 1–3 months | 55 (23.2) | 27 (22.5) | 5 (10.0) | 87 (21.4) | ||
| 3–6 months | 37 (15.6) | 13 (10.8) | 5 (10.0) | 55 (13.5) | ||
| 7–12 month | 15 (6.3) | 9 (7.5) | 6 (12.0) | 30 (7.4) | ||
| 1–2 years | 23 (9.7) | 24 (20.0) | 6 (12.0) | 53 (13.0) | ||
| > 2 year | 44 (18.6) | 32 (26.7) | 27 (54.0) | 103 (25.3) | ||
| Ethnicity | 0.91 | 0.633 | ||||
| Han | 205 (96.2) | 105 (98.1) | 48 (96.0) | 358 (96.8) | ||
| Minority | 8 (3.8) | 2 (1.9) | 2 (4.0) | 12 (3.2) | ||
| Education level | 3.48d | 0.176 | ||||
| Elementary school | 8 (3.8) | 2 (1.9) | 2 (4.0) | 12 (3.2) | ||
| Middle school | 65 (30.5) | 22 (20.6) | 15 (30.0) | 102 (27.6) | ||
| High school | 99 (46.5) | 65 (60.7) | 29 (58.0) | 193 (52.2) | ||
| Vocational school, college, or above | 41 (19.2) | 18 (16.8) | 4 (8.0) | 63 (17.0) | ||
| Monthly income (CNY [1USD = 6.8 CNY]) | 14.37d | 0.001 | ||||
| ≤2000 | 53 (21.5) | 22 (18.0) | 12 (24.0) | 87 (20.8) | ||
| 2001–3000 | 44 (17.9) | 28 (22.9) | 23 (46.0) | 95 (22.7) | ||
| 3001–4000 | 46 (18.7) | 30 (24.6) | 10 (20.0) | 86 (20.6) | ||
| 4001–7000 | 65 (26.4) | 29 (23.8) | 4 (8.0) | 98 (23.4) | ||
| ≥7001 | 38 (15.5) | 13 (10.7) | 1 (2.0) | 52 (12.4) | ||
| Living situation | 14.05 | 0.080 | ||||
| Alone | 66 (26.8) | 46 (37.7) | 22 (44.0) | 134 (32.1) | ||
| Boyfriend | 21 (8.5) | 14 (11.5) | 0 (0) | 35 (8.4) | ||
| Girlfriend | 11 (4.5) | 5 (4.1) | 2 (4.0) | 18 (4.3) | ||
| General friends or other MBs | 140 (56.9) | 54 (44.2) | 25 (50.0) | 219 (52.4) | ||
| Family members | 8 (3.3) | 3 (2.5) | 1 (2.0) | 12 (2.9) | ||
| Marital status | 16.73 | 0.002 | ||||
| Never married | 216 (87.8) | 120 (98.4) | 42 (84.0) | 378 (90.4) | ||
| Married | 14 (5.7) | 2 (1.6) | 6 (12.0) | 22 (5.3) | ||
| Other (divorced, widowed, etc.) | 16 (6.5) | 0 (0) | 2 (4.0) | 18 (4.3) | ||
| Willing to marry a woman in future | 12.96 | 0.011 | ||||
| Yes | 155 (71.8) | 82 (68.3) | 21 (50.0) | 258 (68.3) | ||
| No | 21 (9.7) | 14 (11.7) | 3 (7.1) | 38 (10.1) | ||
| Not sure | 40 (18.5) | 24 (20.0) | 18 (42.9) | 82 (21.7) | ||
| Self-identified sexual orientation | 12.03 | 0.061 | ||||
| Homosexual | 89 (36.2) | 32 (26.2) | 13 (26.0) | 134 (32.1) | ||
| Heterosexual | 66 (26.8) | 33 (27.1) | 7 (14.0) | 106 (25.4) | ||
| Bisexual | 72 (29.3) | 45 (36.9) | 23 (46.0) | 140 (33.5) | ||
| Uncertain | 19 (7.7) | 12 (9.8) | 7 (14.0) | 38 (9.1) | ||
The numbers do not necessarily reach total sample size because of missing values
Pearson Chi-square test unless otherwise indicated
One-way analysis of variance
Kruskal–Wallis nonparametric test
Among all participants, 32.1% self-identified as homosexual, 25.4% heterosexual, 33.5% bisexual, and 9.1% were uncertain. Mean age was 23.6 years. Average duration of being a MB was 0.9 years, ranging from 1 month to 8 years. Two-thirds (66.3%) were from rural regions, almost all (94.3%) were migrants, 69.2% had completed high school or higher, and most (90.4%) had never married. Those participants from massage parlors were older, more likely to be from rural areas, and had lower income.
STI History
Fifty (12.0%) participants reported that they had at least one STI symptom in the last year. Ten (2.4%) reported being diagnosed with gonorrhea, seven (1.7%) with syphilis, five (1.2%) with herpes, and three (0.7%) with genital warts.
For treating STI symptoms, 77.3% would choose public hospitals, 32.5% STI specialty clinics, 8.1% pharmacies, and 1.7% private clinics (overlap due to more than one choice).
Sexual Behaviors
Table 2 presents information on the participants’ sexual behaviors. In the past 6 months, 55.7% had sex with both genders, but for self-identified heterosexual and bisexual MBs, this rate was 82.1 and 70.0%, respectively, which was significantly higher than for homosexuals (15.7%). Anal intercourse encounters with males averaged once in the past week for all participants, but were more frequent among self-identified homosexuals. During anal intercourse, 27.0% were insertive only, 14.8% receptive only, and 58.2% both (varied proportions). Several (16.1%) reported condom breakage during anal intercourse on average twice in the past 6 months; this rate was 23.7% among self-identified homosexuals.
Table 2.
Sexual behaviors of venue-based money boys by self-identified sexual orientation
| Characteristics | Self-identified sexual orientation, n (%)
|
Average, n (%) (N = 418) | χ2c | P-value | |||
|---|---|---|---|---|---|---|---|
| Homosexual (N = 134) | Heterosexual (N = 106) | Bisexual (N = 140) | Uncertain (N = 38) | ||||
| Gender of first sexual partner | 180.54 | 0.000 | |||||
| Male | 97 (72.4) | 4 (3.8) | 15 (10.7) | 6 (15.8) | 122 (29.2) | ||
| Female | 37 (27.6) | 102 (96.2) | 125 (89.3) | 32 (84.2) | 296 (70.8) | ||
| Mean age at sexual debut (yrs) | 19.4 | 18.3 | 19.0 | 18.8 | 19.0 | 4.03d | 0.008 |
| Mean age at sexual debut with a male (yrs) | 20.0 | 21.4 | 21.6 | 21.5 | 21.0 | 8.42d | 0.000 |
| Gender of all sexual partners in the past 6 months | 132.15 | 0.000 | |||||
| Male only | 113 (84.3) | 19 (17.9) | 42 (30.0) | 11 (28.9) | 185 (44.3) | ||
| Male and female | 21 (15.7) | 87 (82.1) | 98 (70.0) | 27 (71.1) | 233 (55.7) | ||
| Sexual activities in the past 6 monthsb | |||||||
| Anal intercourse | 132 (98.5) | 95 (89.6) | 133 (95.0) | 34 (89.5) | 394 (94.3) | 10.43 | 0.015 |
| Oral sex | 111 (82.8) | 80 (75.5) | 106 (75.7) | 29 (76.3) | 326 (78.0) | 2.71 | 0.439 |
| Sadomasochism (SM) | 6 (4.5) | 5 (4.7) | 5 (3.6) | 2 (5.3) | 18 (4.3) | 0.32 | 0.956 |
| Group sex | 4 (3.0) | 7 (6.6) | 9 (6.4) | 4 (10.5) | 24 (5.7) | 3.76 | 0.289 |
| Number of anal intercourse encounters with males in the past week: median (Q1, Q3a) | 1 (1, 3) | 1 (0, 2) | 1 (0, 2) | 1 (0, 2) | 1 (0, 2) | 12.32e | 0.006 |
| Anal intercourse | |||||||
| Insertive only | 29 (23.4) | 22 (26.2) | 37 (29.8) | 9 (33.3) | 97 (27.0) | 1.36 | 0.714 |
| Receptive only | 15 (12.1) | 17 (20.2) | 17 (13.7) | 4 (14.8) | 53 (14.8) | 1.54 | 0.673 |
| Both, but mainly insertive | 15 (12.1) | 11 (13.1) | 26 (21.0) | 4 (14.8) | 56 (15.6) | 4.89 | 0.180 |
| Both, but mainly receptive | 20 (16.1) | 14 (16.7) | 15 (12.1) | 3 (11.1) | 52 (14.5) | 1.92 | 0.589 |
| Both, equally insertive & receptive | 45 (36.3) | 20 (23.8) | 29 (23.4) | 7 (25.9) | 101 (28.1) | 9.70 | 0.021 |
| Lubricant use during anal intercourse in the past 6 months | 4.10f | 0.213 | |||||
| Yes | 124 (100.0) | 83 (98.8) | 120 (96.8) | 27 (100.0) | 354 (98.6) | ||
| No | 0 (0) | 1 (1.2) | 4 (3.2) | 0 (0) | 5 (1.4) | ||
| Condom breakage during anal intercourse | 23.53 | 0.001 | |||||
| Yes | 31 (23.7) | 12 (11.5) | 17 (12.4) | 6 (16.2) | 66 (16.1) | ||
| No | 61 (46.6) | 79 (76.0) | 86 (62.8) | 21 (56.8) | 247 (60.4) | ||
| Uncertain | 39 (29.8) | 13 (12.5) | 34 (24.8) | 10 (27.0) | 96 (23.5) | ||
| Number of condom breakages during anal intercourse in the past 6 months: median (Q1, Q3) | 3 (2, 5) | 1 (1, 2) | 2 (1, 3) | 1 (1, 3) | 2 (1, 3) | 9.67e | 0.022 |
Q1, Q3 25th percentile and 75th percentile
Proportions don’t add up to 100% because of multiple choices
Pearson Chi-square analysis unless otherwise indicated
One-way analysis of variance
Kruskal–Wallis nonparametric test
Fisher’s exact test
In the past month, the median number of male clients was three, but was zero for female clients. In the past 6 months, 30.4% had paid for sex with other MBs, and 21.5% had paid for sex with female sex workers (FSWs). Of the 36.2% who reported having anal intercourse with boyfriends, the average was three per month. Many (40.9%) reported having girlfriends, with a monthly average of eight sexual intercourse encounters with them. In addition, 41.8% had had casual male partners, and 31.8% had had female casual partners. There were no significant differences between MBs of different sexual orientations for numbers of clients or casual partners of either gender.
Condom Use with Different Types of Sexual Partners
Reported condom use rates of participants with different types of sexual partners are presented in Table 3. Consistent condom use rates in our study population were 70–80% with commercial sex partners, 43.9% with girlfriends, and 60–70% with other non-commercial partners. The rates for never using condoms were 1–5% with commercial sex partners, 21.1% with girlfriends, and 5–10% with other non-commercial sex partners. Condom use with male clients was significantly more consistent than with female clients, FSWs, boyfriends, girlfriends, and female casual partners, and did not significantly differ from condom use rates with paid MBs and male casual partners.
Table 3.
Condom use with different types of sexual partners by venue-based MBs
| Condom use with different types of partners | Condom use rates, n (%)
|
za | P-value | |||
|---|---|---|---|---|---|---|
| Every time (100%) | Often (>50%) | Occasionally (<50%) | Never (0%) | |||
| Male clients (N = 414) | 341 (82.4) | 37 (8.9) | 31 (7.5) | 5 (1.2) | –b | – |
| Female clients (N = 110) | 76 (69.1) | 9 (8.2) | 20 (18.2) | 5 (4.5) | 3.89 | 0.000 |
| Paid MBs (N = 127) | 98 (77.2) | 11 (8.7) | 10 (7.9) | 8 (6.3) | 0.43 | 0.671 |
| Female sex workers (N = 88) | 62 (70.5) | 9 (10.2) | 14 (15.9) | 3 (3.4) | 2.29 | 0.022 |
| Boyfriends (N = 134) | 85 (63.4) | 12 (9.0) | 22 (16.4) | 15 (11.2) | 4.16 | 0.000 |
| Girlfriends (N = 171) | 75 (43.9) | 17 (9.9) | 43 (25.1) | 36 (21.1) | 8.46 | 0.000 |
| Male casual partners (N = 168) | 117 (69.6) | 18 (10.7) | 24 (14.3) | 9 (5.4) | 0.90 | 0.366 |
| Female casual partners (N = 133) | 78 (58.6) | 12 (9.0) | 30 (22.6) | 13 (9.8) | 5.68 | 0.000 |
Wilcoxon signed rank sum test
Condom use by MBs with male clients was the reference
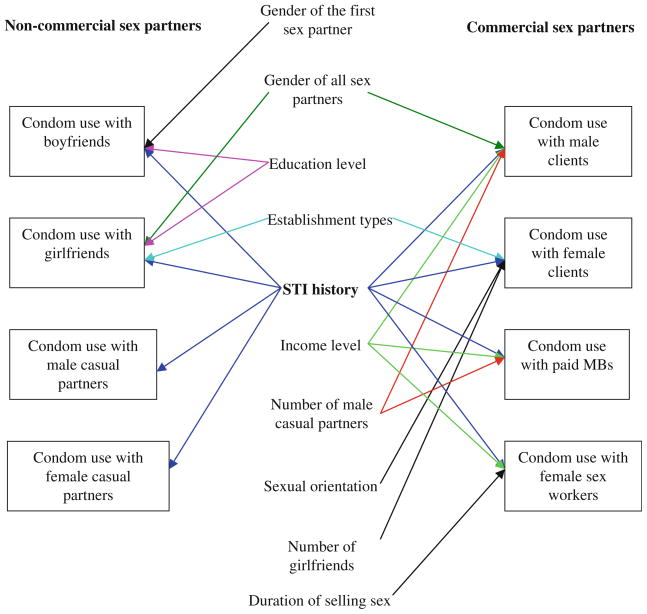
Logistic regression analyses were used to examine factors associated with consistent condom use with different types of partners (Table 4). Figure 1 summarizes these associations. A lower likelihood of consistent condom use with all types of sexual partners was typically seen for those who had an STI history. MBs with higher income were more likely to consistently use condoms with commercial partners (male clients OR = 1.31, other paid MBs OR = 1.71, FSWs OR = 1.58). The more male casual partners, the less likely MBs were to consistently use condoms with their male clients (OR = 0.67) and other paid MBs (OR = 0.57). Education level was found to be associated only with condom use with regular partners, and higher education level predicted more consistent condom use with boyfriends (OR = 2.62) and girlfriends (OR = 1.73). Compared to dorm-based MBs, those working at bars were less likely to use condoms with female clients (OR = 0.34), but were more likely to with girlfriends (OR = 2.17).
Table 4.
Factors significantly associated with MBs’ consistent condom use with different types of partners
| Types of partners | Factors | Consistent condom use
|
Unadjusted
|
Multiple logistic regressiona |
||||
|---|---|---|---|---|---|---|---|---|
| Use (n) | Total (N) | n/N (%) | OR (95% CI) | P-value | OR (95% CI) | P-value | ||
| Male clients (N = 414) | Gender of sex partners in the last six months | |||||||
| Male only | 143 | 182 | 78.6 | 1.00 | – | 1.00 | – | |
| Both | 198 | 232 | 85.3 | 1.59 (0.96,2.64) | 0.074 | 1.77 (1.01, 3.11) | 0.046 | |
| Monthly income (CNY) | 1.32 (1.08, 1.61) | 0.006 | 1.31 (1.05, 1.62) | 0.014 | ||||
| ≤2000 | 60 | 85 | 70.6 | |||||
| 2001–3000 | 78 | 95 | 82.1 | |||||
| 3001–4000 | 72 | 86 | 83.7 | |||||
| 4001–7000 | 89 | 96 | 92.7 | |||||
| ≥7001 | 42 | 52 | 80.7 | |||||
| STI history | ||||||||
| No | 314 | 365 | 86.0 | 1.00 | – | 1.00 | – | |
| Yes | 27 | 49 | 55.1 | 0.20 (0.11, 0.38) | 0.000 | 0.15 (0.08, 0.31) | 0.000 | |
| Number of male casual partners in the past 6 months | 0.88 (0.70, 1.11) | 0.275 | 0.67 (0.53, 0.85) | 0.001 | ||||
| 0 | 214 | 239 | 89.5 | |||||
| 1–2 | 48 | 67 | 71.6 | |||||
| 3–5 | 37 | 47 | 78.7 | |||||
| ≥6 | 40 | 57 | 70.2 | |||||
| Female clients (N = 110) | Self-identified sexual orientation | |||||||
| Homosexual | 13 | 23 | 56.5 | 1.00 | – | 1.00 | – | |
| Heterosexual | 19 | 30 | 63.3 | 1.33 (0.44, 4.03) | 0.616 | 2.32 (0.67,8.02) | 0.185 | |
| Bisexual | 36 | 45 | 80.0 | 3.08 (1.02, 9.26) | 0.046 | 10.81 (2.51,46.49) | 0.001 | |
| Uncertain | 8 | 12 | 66.7 | 1.54 (0.36, 6.60) | 0.562 | 3.20 (0.65,15.81) | 0.154 | |
| Venue type | ||||||||
| Dorm | 39 | 53 | 73.6 | 1.00 | – | 1.00 | – | |
| Gay bar | 28 | 45 | 62.2 | 0.59 (0.25, 1.39) | 0.230 | 0.34 (0.12, 0.95) | 0.040 | |
| Massage parlor | 9 | 12 | 75.0 | 1.08 (0.25, 4.56) | 0.920 | 1.52 (0.29,7.93) | 0.619 | |
| STI history | ||||||||
| No | 70 | 95 | 73.7 | 1.00 | – | 1.00 | – | |
| Yes | 6 | 15 | 40.0 | 0.24 (0.08, 0.74) | 0.013 | 0.13 (0.04, 0.50) | 0.003 | |
| Number of girlfriends in the past 6 months | 0.78 (0.53, 1.13) | 0.188 | 0.55 (0.35, 0.88) | 0.012 | ||||
| 0 | 29 | 42 | 69.1 | |||||
| 1 | 29 | 36 | 80.6 | |||||
| 2 | 9 | 15 | 60.0 | |||||
| ≥3 | 9 | 17 | 52.9 | |||||
| Paid MBs (N = 127) | STI history | |||||||
| No | 93 | 111 | 83.8 | 1.00 | – | 1.00 | – | |
| Yes | 5 | 16 | 31.3 | 0.09 (0.03, 0.28) | 0.000 | 0.09 (0.02, 0.33) | 0.000 | |
| Monthly income (CNY) | 1.69 (1.19, 2.40) | 0.004 | 1.71 (1.15, 2.54) | 0.008 | ||||
| ≤2000 | 19 | 31 | 61.3 | |||||
| 2001–3000 | 20 | 27 | 74.1 | |||||
| 3001–4000 | 15 | 21 | 71.4 | |||||
| 4001–7000 | 36 | 39 | 92.3 | |||||
| ≥7001 | 8 | 9 | 88.9 | |||||
| Number of male casual partners in the last 6 months | 0.58 (0.41, 0.84) | 0.004 | 0.57 (0.37, 0.88) | 0.011 | ||||
| 0 | 63 | 71 | 88.7 | |||||
| 1–2 | 17 | 27 | 63.0 | |||||
| 3–5 | 7 | 11 | 63.6 | |||||
| ≥6 | 11 | 18 | 61.1 | |||||
| Female sex workers (N = 88) | STI history | |||||||
| No | 54 | 70 | 77.1 | 1.00 | – | 1.00 | – | |
| Yes | 8 | 18 | 44.4 | 0.24 (0.08, 0.70) | 0.009 | 0.17 (0.05, 0.56) | 0.004 | |
| Duration of selling sex (yrs) | 0.78 (0.54, 1.13) | 0.189 | 0.69 (0.46, 1.02) | 0.065 | ||||
| Monthly income (CNY) | 1.27 (0.91, 1.77) | 0.163 | 1.58 (1.06, 2.33) | 0.023 | ||||
| ≤2000 | 9 | 17 | 52.9 | |||||
| 2001–3000 | 11 | 15 | 73.3 | |||||
| 3001–4000 | 16 | 21 | 76.2 | |||||
| 4001–7000 | 11 | 16 | 68.8 | |||||
| ≥7001 | 15 | 19 | 79.0 | |||||
| Boyfriends (N = 134) | Gender of first sexual partner | |||||||
| Female | 56 | 76 | 73.7 | 1.00 | – | 1.00 | – | |
| Male | 29 | 58 | 50.0 | 0.36 (0.17, 0.74) | 0.005 | 0.25 (0.10, 0.61) | 0.003 | |
| STI history | ||||||||
| No | 78 | 111 | 70.3 | 1.00 | – | 1.00 | – | |
| Yes | 7 | 23 | 30.4 | 0.19 (0.07, 0.49) | 0.001 | 0.20 (0.06, 0.70) | 0.012 | |
| Education level | 2.26 (1.26, 4.05) | 0.006 | 2.62 (1.36, 5.02) | 0.004 | ||||
| Elementary school | 0 | 1 | 0.0 | |||||
| Middle school | 19 | 36 | 52.8 | |||||
| High school | 40 | 56 | 71.4 | |||||
| Vocational school, college, or above | 20 | 24 | 83.3 | |||||
| Girlfriends (N = 171) | Gender of sex partners in the past 6 months | |||||||
| Male only | 15 | 19 | 79.0 | 1.00 | – | 1.00 | – | |
| Male and female | 60 | 152 | 39.5 | 0.17 (0.06, 0.55) | 0.003 | 0.15 (0.04, 0.59) | 0.007 | |
| STI history | ||||||||
| No | 73 | 150 | 48.7 | 1.00 | – | 1.00 | – | |
| Yes | 2 | 21 | 9.5 | 0.11 (0.02, 0.49) | 0.004 | 0.05 (0.01, 0.44) | 0.007 | |
| Venue types | ||||||||
| Dorm | 33 | 92 | 35.9 | 1.00 | – | 1.00 | – | |
| Gay bar | 26 | 52 | 50.0 | 1.79 (0.90, 3.57) | 0.099 | 2.17 (0.94, 5.01) | 0.068 | |
| Massage parlor | 16 | 27 | 59.3 | 2.60 (1.08, 6.26) | 0.033 | 2.89 (1.09, 7.64) | 0.032 | |
| Education level | 1.84 (1.15, 2.95) | 0.012 | 1.73 (1.02, 2.94) | 0.042 | ||||
| Elementary school | 3 | 4 | 75.0 | |||||
| Middle school | 12 | 48 | 25.0 | |||||
| High school | 40 | 79 | 50.6 | |||||
| Vocational school, college, or above | 14 | 22 | 63.6 | |||||
| Male casual partners (N = 168) | STI history | |||||||
| No | 15 | 51 | 29.4 | 1.00 | – | 1.00 | – | |
| Yes | 9 | 117 | 7.7 | 0.20 (0.08, 0.50) | 0.001 | 0.20(0.08, 0.50) | 0.001 | |
| Female casual partners (N = 133) | STI history | |||||||
| No | 20 | 55 | 36.4 | 1.00 | – | 1.00 | – | |
| Yes | 4 | 78 | 5.1 | 0.09 (0.03, 0.30) | 0.000 | 0.09 (0.03, 0.30) | 0.000 | |
Attempted to control for potential confounders such as age, education level, income, duration of being MB, HIV/AIDS knowledge
Fig. 1.
Factors associated with MBs’ condom use with different types of sexual partners
HIV/STIs and Associated Factors
Fourteen participants were HIV-positive (an overall prevalence of 3.3%), but this rate was much higher among self-identified homosexuals, 7.5% (1.4%; unadjusted OR = 5.65, 95% CI 1.74–18.35). Prevalence among dorm-based MBs was 4.1%, 4.0% among massage parlor-based MBs, and 1.6% among gay bar-based MBs. Forty-four (10.5%) were syphilis antibody-positive, and 46 (11.0%) were HSV-2 antibody-positive. Eighty-five (20.3%) had at least one pathogen antibody-positive test. Positivity was 50.0% among minorities and 20.1% among Hans (the largest ethnic group in China) (unadjusted OR = 3.97, 95% CI 1.24–12.68). For those who had only male partners in the past 6 months, 26.5% were antibody-positive, compared to 15.5% among all participants (unadjusted OR = 1.97, 95% CI 1.22–3.19). Of the 14 HIV antibody-positive, eight were also syphilis antibody-positive (including three positives for all three agents). Among the 44 syphilis antibody-positive, 11 were also HSV-2 antibody-positive (including three positives for all three agents).
In logistic regression analysis for HIV infection, we found that after controlling for ethnicity, the gender of sex partners in the past six months was associated with HIV infection. Those who had only male partners had HIV prevalence of 6.5%, which was much higher than those with sexual partners of both genders (0.9%; OR = 14.32, 95% CI 1.83–112.22) (see Table 5).
Table 5.
Factors associated with HIV and other STIs among venue-based MBs (N = 418)
| Dependent variable | Factors | Positive (n) | Total N | n/N (%) | Unadjusted
|
Multiple logistic regressiona |
||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |||||
| HIV-positive | Gender of sexual partners in the past 6 months | |||||||
| Both male and female | 2 | 233 | 0.9 | 1.00 | – | 1.00 | – | |
| Male only | 12 | 185 | 6.5 | 8.01 (1.77, 36.26) | 0.007 | 14.32 (1.83, 112.22) | 0.011 | |
| Minority | ||||||||
| No | 11 | 358 | 3.1 | 1.00 | – | 1.00 | – | |
| Yes | 1 | 12 | 8.3 | 2.87(0.34, 24.21) | 0.333 | 2.71(0.30, 24.55) | 0.375 | |
| Self-identified sexual orientation | ||||||||
| Homosexual | 10 | 134 | 7.5 | 1.00 | – | |||
| Heterosexual | 0 | 106 | 0.0 | – | – | |||
| Bisexual | 3 | 140 | 2.1 | 0.53(0.15, 1.94) | 0.338 | |||
| Uncertain | 1 | 38 | 2.6 | 0.76(0.10, 6.00) | 0.797 | |||
| Venue type | ||||||||
| Gay bar | 2 | 122 | 1.6 | 1.00 | – | |||
| Dorm | 10 | 246 | 4.1 | 2.54(0.55, 11.79) | 0.233 | |||
| Massage parlor | 2 | 50 | 4.0 | 2.50(0.34, 18.26) | 0.366 | |||
| Positive for HIV or any STI | Age | 1.08 (1.02, 1.13) | 0.008 | 1.11 (1.04, 1.19) | 0.003 | |||
| Minority | ||||||||
| No | 72 | 358 | 20.1 | 1.00 | – | 1.00 | – | |
| Yes | 6 | 12 | 50.0 | 3.97 (1.24, 12.68) | 0.020 | 4.82 (1.46, 15.88) | 0.010 | |
| Age at sexual debut, yrs | 0.98 (0.89, 1.07) | 0.653 | 0.88 (0.79, 0.98) | 0.020 | ||||
| Gender of sexual partners in the past 6 months | ||||||||
| Male and female | 36 | 233 | 15.5 | 1.00 | – | 1.00 | – | |
| Male only | 49 | 185 | 26.5 | 1.97 (1.22, 3.19) | 0.006 | 1.92 (1.12, 3.30) | 0.018 | |
| Number of male casual partners in the last 6 months | 1.20 (0.97, 1.47) | 0.095 | 1.28 (1.01, 1.61) | 0.040 | ||||
| 0 | 44 | 241 | 18.3 | |||||
| 1–2 | 13 | 69 | 18.8 | |||||
| 3–5 | 9 | 47 | 19.2 | |||||
| ≥6 | 17 | 57 | 29.8 | |||||
Attempted to control for potential confounders such as age, education level, income, duration of being MB, HIV/AIDS knowledge, and condom use rates with different types of partners
Regression analysis of participants who were positive for at least one STI or HIV indicated that being older (OR = 1.11, 95% CI 1.04–1.19), minority (OR = 4.82, 95% CI 1.46–15.88), younger at sexual debut (OR = 1.14, 95% CI 1.02–1.27), having only male sexual partners (OR = 1.92, 95% CI 1.12–3.30), and having more male casual partners in the past 6 months (OR = 1.28, 95% CI 1.01–1.61) were factors significantly associated with HIV/STIs (see Table 5).
Discussion
We found that consistent condom use among MBs is relatively high compared to other risk populations in China, such as non-commercial MSM and FSWs [1, 4, 37]. This may explain why HIV prevalence was not higher in our study population. However, consistent condom use rates were still not high enough to prevent the risk of HIV/STI transmission to their sexual partners. Intervention activities need to be increased among MBs to encourage higher levels of consistent condom use with all types of partners, especially females.
We also found that the HIV prevalence rate in our study population (3.3%) is close to that of the general MSM population in Shenzhen (3.6–4.2%) [38]. An average HIV prevalence of 2.9% was reported in a recent large-scale survey among MSM in seven provinces in China [39]. In another nationwide survey among MSM in 61 cities in China, the average prevalence of HIV was 4.9% (Chinese Center for Disease Control and Prevention, 2008). On the other hand, we found that HIV prevalence was much higher among self-identified homosexuals (7.5% vs. 1.4% among those of other sexual orientations) and those who had only male sex partners (6.5% vs. 0.9% of those who had both male and female partners). While there was a higher prevalence of HIV/STIs in the self-identified homosexuals in our study population, HIV/STIs were also prevalent in the heterosexuals, and this has the greatest potential to spread to other populations in China through heterosexual contact. Of the 14 HIV-positive MBs in our study, three (21%) did not consistently use condoms with male clients, three (21%) did not with casual male partners, two (14%) did not with paid MBs, and one (7%) did not with girlfriends. Among those who tested positive for other STI pathogens, inconsistent condom use was 67.9% with girl-friends and 20–40% with other types of partners. These HIV/STI-positive MBs are therefore putting their partners at high risk for becoming infected.
It is commonly believed that sex work is a risk factor for HIV/STIs. However, a 10 year follow-up study among MSWs in London reported that their risk of HIV/STIs did not appear to be linked to sex work [13]. The results from our study are consistent with this finding, probably due to very high rates of consistent condom use with male clients. We found that MBs’ current HIV/STI status was not related to their numbers of male clients; rather, it was related to the number of male casual partners, with whom condom use was lower.
Another finding is that due to their higher prevalence of HIV/STIs, ethnic minorities (non-Hans) should be targeted for intervention activities, since they are at particularly high risk for HIV/STIs.
MBs with a STI history should especially be targeted for condom promotion, as STI history was associated with low condom use with all types of sexual partners. Our findings also imply that those who had prior infectious with STIs did not appear to increase their subsequent condom use. Better prevention counseling should be offered at STI clinics.
Higher income was found to be associated with more consistent condom use with commercial partners (either paying or being paid), but not with non-commercial partners. More intervention efforts need to be focused on low-income MBs and those having sex with non-commercial partners.
Study Limitations
This is the first study in China using the CASI technique to survey MBs. Many studies using CASI have reported obtaining more reliable data on sensitive topics in surveys [29–31, 33, 34, 36]. We therefore assumed that we had good data validity, although we did not confirm reported responses. However, data from CASI still need to be scrutinized. There were about 150 questions in our questionnaire, and it took an average of 22 min to complete. Because we did not supervise the participants completing the questionnaire, we found obvious fabrications, and therefore deleted four cases from our dataset. We found that some self-identified heterosexuals reported having boyfriends. Some might be due to misreporting, but some MBs who were “kept” by clients might have considered them to be boyfriends. For some multiple choice questions, it was especially hard to use logic to determine whether the answers were valid. Therefore, researchers should carefully consider strategies to confirm reported activities, especially for sensitive topics.
There may be other limitations in our study. The data collected from self-reporting were not free of social desirability bias, so there might have been under-reporting of risky behaviors or over-reporting of condom use. We noticed that sometimes respondents were sitting very close to each other, which might have influenced their responses. The representativeness of our study population is uncertain. Some MBs did not show up for their interviews. Our sample size seems large, considering our study population was hard to reach. However, when we conducted categorized analyses, such as those who had different types of partners and sexual orientations, the sample size became insufficient, yielding broad confidence intervals. In addition, antibody-positivity for HIV/STIs might have been from prior infections, so we cannot establish a causal relationship between HIV/STI sero-status and current or recent risk factors.
Nonetheless, this study provides relevant information to assist public health workers and researchers to better understand venue-based MBs and their role in transmitting HIV/STIs. It confirms the findings of other studies, in that MBs have sex with both genders, both as clients and otherwise, within both high- and low-risk populations, and have both short- and long-term relationships [14, 18, 19]. The complexity of their sexual activities presents a challenge for controlling transmission of the HIV/STI epidemic from them to the general population.
The accurate number of MBs in China is difficult to obtain. However, their impact on the HIV/STI epidemic needs to be further studied and assessed. Our study shows that this population has a significant prevalence of HIV/STIs, and may be a core group for transmitting HIV/STIs in sexually active populations. Intervention activities need to be conducted to reduce unprotected sexual activities with all types of partners. More effective counseling, readily available condoms, and early testing and treatment for HIV/STIs should be delivered to this population, especially minority MBs, as soon as possible.
Acknowledgments
This study was supported by the Fogarty/UCLA AIDS International Training and Research Program (D43 TW000013). The authors thank Shenzhen 258 Rainbow Workgroup and its staff for their help recruiting study participants. The authors also thank Wendy Aft and Sam Guo for editing assistance.
Contributor Information
Shusen Liu, National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, China.
Jin Zhao, Shenzhen Center for Disease Control and Prevention, Shenzhen, China.
Keming Rou, National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, China.
Lin Chen, Shenzhen Center for Disease Control and Prevention, Shenzhen, China.
Wende Cai, Shenzhen Center for Disease Control and Prevention, Shenzhen, China.
Li Li, School of Public Health, University of California, Los Angeles, 630 South Charles Young Drive, 71-269 CHS, Los Angeles, CA 90095-1772, USA.
Zunyou Wu, National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, China.
Roger Detels, Email: detels@ucla.edu, School of Public Health, University of California, Los Angeles, 630 South Charles Young Drive, 71-269 CHS, Los Angeles, CA 90095-1772, USA.
References
- 1.Chinese State Council AIDS Working Committee and United Nations Theme Group on AIDS. A Joint Assessment of HIV/AIDS Prevention, Treatment and Care in China. 2007. [Google Scholar]
- 2.Zhang B, Li X, Shi T. A primary estimation of the number of population and HIV prevalence in homosexual and bisexual men in China. J China AIDS/STD Prevent Control. 2002;8:197. [Google Scholar]
- 3.Zhong F, Lin P, Xu H, et al. Possible increase in HIV and syphilis prevalence among men who have sex with men in Guangzhou, China: results from a respondent-driven sampling survey. AIDS Behav. 2009;36(10):647–56. doi: 10.1007/s10461-009-9619-x. [DOI] [PubMed] [Google Scholar]
- 4.Wong FY, Huang ZJ, Wang W, et al. STIs and HIV among men having sex with men in China: a ticking time bomb? AIDS Educ Prev. 2009;21(5):430–46. doi: 10.1521/aeap.2009.21.5.430. [DOI] [PubMed] [Google Scholar]
- 5.Lau JT, Wang M, Wong HN, et al. Prevalence of bisexual behaviors among men who have sex with men (MSM) in China and associations between condom use in MSM and heterosexual behaviors. Sex Transm Dis. 2008;35(4):406–13. doi: 10.1097/OLQ.0b013e318164467f. [DOI] [PubMed] [Google Scholar]
- 6.Ma X, Zhang Q, He X, et al. Trends in prevalence of HIV, syphilis, hepatitis C, hepatitis B, sexual risk behavior among men who have sex with men. Results of 3 consecutive respondent-driven sampling surveys in Beijing, 2004 through 2006. J Acquir Immune Defic Syndr. 2007;45(5):581–7. doi: 10.1097/QAI.0b013e31811eadbc. [DOI] [PubMed] [Google Scholar]
- 7.Jiang J, Cao N, Zhang J, et al. High prevalence of sexually transmitted diseases among men who have sex with men in Jiangsu Province, China. Sex Transm Dis. 2006;33(2):118–23. doi: 10.1097/01.olq.0000199763.14766.2b. [DOI] [PubMed] [Google Scholar]
- 8.Zhang D, Bi P, Lv F, Zhang J, Hiller JE. Changes in HIV prevalence and sexual behavior among men who have sex with men in a northern Chinese city: 2002–2006. J Infect. 2007;55(5):456–63. doi: 10.1016/j.jinf.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Chemnasiri T, Netwong T, Visarutratana S, et al. Inconsistent condom use among young men who have sex with men, male sex workers, and transgenders in Thailand. AIDS Educ Prev. 2010;22(2):100–9. doi: 10.1521/aeap.2010.22.2.100. [DOI] [PubMed] [Google Scholar]
- 10.Baral S, Kizub D, Masenior NF, et al. Male sex workers in Moscow, Russia: a pilot study of demographics, substance use patterns, and prevalence of HIV-1 and sexually transmitted infections. AIDS Care. 2010;22(1):112–8. doi: 10.1080/09540120903012551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shinde S, Setia MS, Row-Kavi A, Anand V, Jerajani H. Male sex workers: are we ignoring a risk group in Mumbai, India? Indian J Dermatol Venereol Leprol. 2009;75(1):41–6. doi: 10.4103/0378-6323.45219. [DOI] [PubMed] [Google Scholar]
- 12.Tun W, de Mello M, Pinho A, Chinaglia M, Diaz J. Sexual risk behaviours and HIV seroprevalence among male sex workers who have sex with men and non-sex workers in Campinas, Brazil. Sex Transm Infect. 2008;84(6):455–7. doi: 10.1136/sti.2008.031336. [DOI] [PubMed] [Google Scholar]
- 13.Sethi G, Holden BM, Gaffney J, Greene L, Ghani AC, Ward H. HIV, sexually transmitted infections, and risk behaviours in male sex workers in London over a 10 year period. Sex Transm Infect. 2006;82(5):359–63. doi: 10.1136/sti.2005.019257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cai WD, Zhao J, Zhao JK, et al. HIV prevalence and related risk factors among male sex workers in Shenzhen, China: results from a time-location sampling survey. Sex Transm Infect. 2010;86(1):15–20. doi: 10.1136/sti.2009.037440. [DOI] [PubMed] [Google Scholar]
- 15.Lau JT, Cai WD, Tsui HY, Chen L, Cheng JQ. Psychosocial factors in association with condom use during commercial sex among migrant male sex workers living in Shenzhen, mainland China who serve cross-border Hong Kong male clients. AIDS Behav. 2009;13(5):939–48. doi: 10.1007/s10461-009-9591-5. [DOI] [PubMed] [Google Scholar]
- 16.Geibel S, Luchters S, King’Ola N, Esu-Williams E, Rinyiru A, Tun W. Factors associated with self-reported unprotected anal sex among male sex workers in Mombasa, Kenya. Sex Transm Dis. 2008;35(8):746–52. doi: 10.1097/OLQ.0b013e318170589d. [DOI] [PubMed] [Google Scholar]
- 17.Kong TS. Risk factors affecting condom use among male sex workers who serve men in China: a qualitative study. Sex Transm Infect. 2008;84(6):444–8. doi: 10.1136/sti.2008.030650. [DOI] [PubMed] [Google Scholar]
- 18.Wong FY, Huang ZJ, He N, et al. HIV risks among gay- and non-gay-identified migrant money boys in Shanghai, China. AIDS Care. 2008;20(2):170–80. doi: 10.1080/09540120701534707. [DOI] [PubMed] [Google Scholar]
- 19.Liu H, Liu H, Cai Y, Rhodes AG, Hong F. Money boys, HIV risks, and the associations between norms and safer sex: a respondent-driven sampling study in Shenzhen, China. AIDS Behav. 2009;13(4):652–62. doi: 10.1007/s10461-008-9475-0. [DOI] [PubMed] [Google Scholar]
- 20.He N, Wong FY, Huang ZJ, Thompson EE, Fu C. Substance use and HIV risks among male heterosexual and ‘money boy’ migrants in Shanghai, China. AIDS Care. 2007;19(1):109–15. doi: 10.1080/09540120600888394. [DOI] [PubMed] [Google Scholar]
- 21.He N, Wong FY, Huang ZJ, et al. HIV risks among two types of male migrants in Shanghai, China: money boys vs. general male migrants. AIDS. 2007;21(Suppl 8):S73–9. doi: 10.1097/01.aids.0000304700.85379.f3. [DOI] [PubMed] [Google Scholar]
- 22.Mi G, Wu Z, Zhang B, Zhang H. Survey on HIV/AIDS-related high risk behaviors among male sex workers in two cities in China. AIDS. 2007;21(Suppl 8):S67–72. doi: 10.1097/01.aids.0000304699.85379.32. [DOI] [PubMed] [Google Scholar]
- 23.Dare OO, Cleland JG. Reliability and validity of survey data on sexual behaviour. Hlth Transit Rev. 1994;4(Suppl):93–110. [PubMed] [Google Scholar]
- 24.Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull. 2007;133(5):859–83. doi: 10.1037/0033-2909.133.5.859. [DOI] [PubMed] [Google Scholar]
- 25.Geary C, Tchupo J, Johnson L, Cheta C, Nyiama T. Respondent perspectives on self-report measures of condom use. AIDS Educ Prev. 2003;15(6):499–515. doi: 10.1521/aeap.15.7.499.24044. [DOI] [PubMed] [Google Scholar]
- 26.Paulhus D. Measures of personality and social psychological attitudes. In: Robinson J, Shaver P, Wrightsman L, editors. Measurement and control of response bias. New York: Academic Press; 1991. pp. 17–59. [Google Scholar]
- 27.Guest G, Bunce A, Johnson L, Akumatey B, Adeokun L. Fear, hope and social desirability bias among women at high risk for HIV in West Africa. J Fam Plan Reprod Health Care. 2005;31(4):285–7. doi: 10.1783/jfp.31.2.285. [DOI] [PubMed] [Google Scholar]
- 28.Schopper D, Doussantousse S, Orav J. Sexual behaviours relevant to HIV transmission in a rural African population: How much can a KAP survey tell us? Soc Sci Med. 1993;37:401–12. doi: 10.1016/0277-9536(93)90270-e. [DOI] [PubMed] [Google Scholar]
- 29.Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353(9165):1657–61. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 30.Kissinger P, Rice J, Farley T, et al. Application of computer-assisted interviews to sexual behavior research. Am J Epidemiol. 1999;149(10):950–4. doi: 10.1093/oxfordjournals.aje.a009739. [DOI] [PubMed] [Google Scholar]
- 31.Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Educ Prev. 2002;14(5):367–78. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- 32.Navaline HA, Snider EC, Petro CJ, et al. Preparations for AIDS vaccine trials. An automated version of the risk assessment battery (RAB): enhancing the assessment of risk behaviors. AIDS Res Hum Retroviruses. 1994;10(Suppl 2):S281–3. [PubMed] [Google Scholar]
- 33.Reichmann WM, Losina E, Seage GR, et al. Does modality of survey administration impact data quality: audio computer assisted self interview (ACASI) versus self-administered pen and paper? PLoS One. 2010;5(1):e8728. doi: 10.1371/journal.pone.0008728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rogers SM, Willis G, Al-Tayyib A, et al. Audio computer assisted interviewing to measure HIV risk behaviours in a clinic population. Sex Transm Infect. 2005;81(6):501–7. doi: 10.1136/sti.2004.014266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van der Elst EM, Okuku HS, Nakamya P, et al. Is audio computer-assisted self-interview (ACASI) useful in risk behaviour assessment of female and male sex workers, Mombasa, Kenya? PLoS One. 2009;4(5):e5340. doi: 10.1371/journal.pone.0005340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams ML, Freeman RC, Bowen AM, et al. A comparison of the reliability of self-reported drug use and sexual behaviors using computer-assisted versus face-to-face interviewing. AIDS Educ Prev. 2000;12(3):199–213. [PubMed] [Google Scholar]
- 37.Wang L, Ding ZW, Ding GW, et al. Data analysis of national HIV comprehensive surveillance sites among female sex workers from 2004 to 2008. Zhonghua Yu Fang Yi Xue Za Zhi. 2009;43(11):1009–15. [PubMed] [Google Scholar]
- 38.Hong FC, Zhou H, Cai YM, et al. Prevalence of syphilis and HIV infections among men who have sex with men from different settings in Shenzhen, China: implications for HIV/STD surveillance. Sex Transm Infect. 2009;85(1):42–4. doi: 10.1136/sti.2008.031682. [DOI] [PubMed] [Google Scholar]
- 39.Xiao Y, Sun J, Li C, et al. Prevalence and correlates of HIV and syphilis infections among men who have sex with men in seven provinces in China with historically low HIV prevalence. J Acquir Immune Defic Syndr. 2010;53(Suppl 1):S66–73. doi: 10.1097/QAI.0b013e3181c7db43. [DOI] [PubMed] [Google Scholar]