Abstract
Evidence is emerging that obesity-associated cardiovascular disorders (CVD) show variations across regions and ethnicities. However, it is unclear if there are distinctive patterns of abdominal obesity contributing to an increased CVD risk in South Asians. Also, potential underlying mechanistic pathways of such unique patterns are not comprehensively reported in South Asians. This review sets out to examine both. A comprehensive database search strategy was undertaken, namely, PubMed, Embase and Cochrane Library, applying specific search terms for potentially relevant published literature in English language. Grey literature, including scientific meeting abstracts, expert consultations, text books and government/non-government publications were also retrieved. South Asians have 3-5% higher body fat than whites, at any given body mass index. Additional distinctive features, such as South Asian phenotype, low adipokine production, lower lean body mass, ethno-specific socio-cultural and economic factors, were considered as potential contributors to an early age-onset of obesity-linked CVD risk in South Asians. Proven cost-effective anti-obesity strategies, including the development of ethno-specific clinical risk assessment tools, should be adopted early in the life-course to prevent premature CVD deaths and morbidity in South Asians.
Keywords: Abdominal obesity, cardiovascular risk, cardiovascular diseases, diabetes mellitus, South Asians
INTRODUCTION
Increased health risks of obesity have been documented for centuries in Charaka Samhita[1] and writings attributed to Hippocrates.[2] Such observations are no less relevant now. Evidence is emerging that obesity-associated illnesses, specifically cardiovascular disorders (CVD) show variations across regions and ethnicities.[3,4] One of the strongest phenomena in support of such observations is the recent redefinition of the body-mass-index (BMI) criteria, to specific populations, for example, the Asia-Pacific criterion for obesity.[5] In this review, distinct patterns in obesity, mainly abdominal obesity, and its associated illnesses are discussed from a South Asian perspective. South Asians comprise individuals who belong to heterogeneous ethnicities and trace their origin from various countries in the Indian subcontinent (India, Pakistan, Nepal Sri Lanka and Bangladesh). There are two main focus areas of this review. First, what are the distinctive features of adult obesity in South Asians compared to Caucasian populations? Such an approach might help identify the uniqueness of clinical patterns of obesity-related illnesses in the South Asians and also help towards better clinical diagnosis and tailored management. Secondly, the underlying mechanistic pathways that contribute to such distinct patterns among the South Asians. This second aspect is vital for adopting a strategic approach to prevent and control obesity-related disease burden among the South Asians. In addition, this review discusses related topics, such as the need for new and revised cut-off points of BMI for specific ethnicities, the burden of obesity in specific population sub-groups, and main differences underlying abdominal obesity compared to general obesity.
DEFINITIONS
Obesity, is defined as a body fat content of more than 20% in average adult males and over 30% in females.[6] However, obese individuals vary in the amount of excess fat that they store, the regional distribution of that fat within the body, and the related health consequences differ noticeably amongst these obese persons.[6,7] It is therefore essential to make a distinction between those at augmented risk as a result of abdominal obesity from those with generalized obesity.[8] Even though most epidemiological studies have only used BMI as a predictor of disease, there is substantiation that subjects with abdominal obesity, as assessed by measurement of waist circumference or waist-hip ratio, are at a greater risk of cardio metabolic risk, independently of risk associated with a raised BMI.[9–11] Further, waist circumference beyond 90 cm in males and over 80 cm in females is an effectual clinical predictor of the metabolic risk like other clinical, biochemical and imaging variables.[5,12] Such clinico-epidemiological observations are clearly important to redefine the occurrence of obesity-associated cardiovascular risks in a population where both obesity and CVD are recent phenomena. South Asians, in particular, have shown a different pattern of cardiovascular risks, both, in indigenous populations, and also those who migrated to the West.[13,14]
MATERIALS AND METHODS
This review attempts a comprehensive database search strategy more akin to a systematic review approach; however, falls short of the scientific rigor involved in a systematic review. Nevertheless, the evidence drawn should add to the existing body of literature showing similar observations and conclusions.[14] We abstracted the most significant published literature on the electronic databases, namely, Pub Med, Embase and the Cochrane Library applying specific search terms such as “South Asians”;“ Asian Indians”; “obesity”; “overweight”; “cardiovascular risk factors”; “childhood obesity”; cardiovascular disorders - “CVD”; Coronary heart disease - “CHD”; “physical inactivity”; “metabolic syndrome”; “ethnicity” etc. We have also gone through articles unpublished on Pub Med; abstracts of conference/meetings; consulting authors/experts in the field; text books; and, publications of governmental/non-governmental organization. Articles only in English language were considered.
Globalization, epidemiological transition and obesity
Recent data of mounting burden of noncommunicable diseases synchronizing with globalization can be understood in the context of epidemiological, nutritional, demographic and socioeconomic transition across the globe.[15–17] It has been hypothesized that obesity and type-2 diabetes had their lineage in a natural choice of early humans, favoring a “thrifty genotype”,[18] which enabled very well-organized storage of energy during periods of food abundance. Similarly, the ‘thrifty phenotype’[19] explains how low-birth-weight babies, who have been exposed to a chronic energy-deprived state, accumulate energy stores and go on to develop type-2 diabetes in adulthood. These genetic or phenotypic adaptations that were supportive in times of famine, have become detrimental with increasing nutritional availability and decreasing physical activity due to modern lifestyle [Figure 1].
Figure 1.
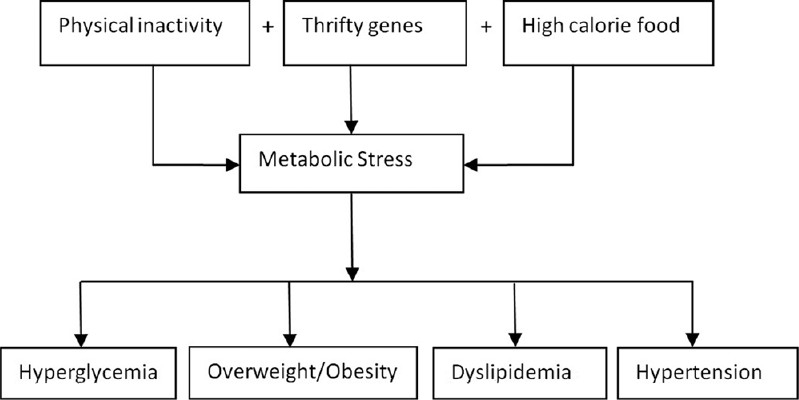
Thrifty genotype and epidemiological transition, modern lifestyle-metabolic stress with thrifty genes
Overweight and obesity in South Asians
Though South Asians have a very high prevalence of abdominal obesity, there is paucity of country wide accurate data and statistics related to this..[20–22] Obesity in childhood and adolescence is attaining an alarming and epidemic proportion in India with about 15–20% of the population being affected.[23] Similarly, about 30-65% of adult urban Indians are either overweight, obese or have abdominal obesity.[24] Though the prevalence of obesity in South Asians is lower than whites, blacks and Hispanics, the health risks related with obesity crop up at a lower BMI in South Asians.[25,26] These observations put forth the fact that the current World Health Organization (WHO) criteria to define overweight and obesity may not be suitable for Asian populace in general, and South Asians in particular.[5,27] Thus, a new criteria to define overweight and obesity in the Asia-Pacific and South Asian Region has been proposed.[24,28] The BMI and waist circumferences included in this criteria for the Asians has been[5] summarized in Table 1.
Table 1.
Co-morbidities risk associated with different levels of body mass index and suggested waist circumference in adult Asians
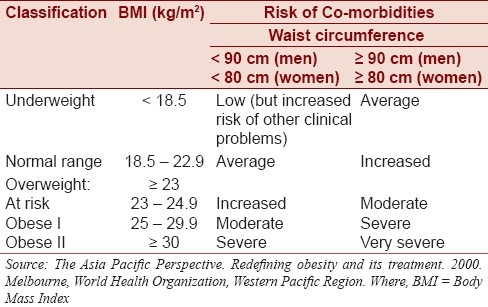
World Health Organization Asia Pacific criteria for obesity
On an average, in adult males the desirable body fat content is about 15-20%, and in females it is higher at about 25-30%.[6] Women have more fat than men for a given BMI. An analogous situation is seen for Asians as compared to whites and blacks. Asian populations have 3% to 5% higher body fat than others at an identical BMI.[8] Similarly, for a given amount of body fat, the BMI is 2 to 3 units lower in Asians than in whites. This observable fact is ascribed to the smaller body frame of Asians. Hence, the usual cut-points of obesity may not be suitable for Asians in general, and South Asians in particular.[8] The WHO recommends different cut off points for obesity in Asians.[5] A BMI more than 25 is considered obese for Asians in variation to 30 for other populations.[8] Furthermore, blacks have a lower body fat and different metabolic abnormalities for a given BMI. The optimum BMI appears to be below 23 for Asians, 23 to 25 for whites and 23 to 30 for blacks.[8] However, existing data does not essentially specify a clear BMI cut-off point for all Asians for overweight or obesity.[27]
General obesity versus abdominal obesity
Even as the relative importance of general and abdominal obesity is still debated, abdominal obesity is particularly considered of the atherogenic variety of adiposity, because it appears to promote a cluster of atherogenic risk factors asso-ciated with insulin resistance.[29,30] Abdominal obesity as represented by the waist circumference or the waist-hip ratio, has been shown to be a strong predictor of CHD, independent of the general level of obesity, although the BMI also influences CHD risk.[31] Furthermore, the markers of obesity, namely, BMI, waist size and waist hip ratio have a positive relationship with major cardiovascular risk factors like hypertension, metabolic diseases like diabetes; while, the waist hip ratio also correlates with dyslipidemia.[32]
Abdominal obesity is more common amongst South Asians than general adiposity, which is in contrast to whites, who have only a slightly higher rate of abdominal adiposity, and blacks who actually have a lower rate of abdominal obesity than general obesity.[8,14] Abdominal adiposity accumulates in three places:(i) subcutaneous fat, (ii) retro-peritoneal fat, and (iii) visceral fat. However, the visceral fat is considered to be most atherogenic, diabetogenic and hypertensiogenic fat depot of the human body.[14] Visceral fat is particularly deleterious because of its anatomical location and the resultant increased supply of free fatty acids to the liver via portal venous drainage.[14]
Specific features of South Asian thin-fat phenotype
‘Thin fat’ phenotype or muscle thin but adipose body composition is defined as a relatively low body mass index but increased total, subcutaneous and central (truncal and abdominal) body fat.[33,34] These features appear to be present from birth as Indian neonates tend to have increased body fat compared to their Caucasians despite lower birth weights.[33–35] These unique features led to the coining of the term ‘Thin-Fat phenotype’[33] or ‘Asian Indian Phenotype′.[35]
Excess body fat: South Asians have higher percentage of body fat for a given BMI as compared to Caucasians and Blacks.[8,14]
Abdominal obesity: Is seen with increased prevalence in South Asians even amongst those who have a BMI < 25 kg/m2.[8,14]
Truncal subcutaneous fat: It is a particular distinctive feature and an important correlate of insulin resistance in this ethnic group.[8,14]
Metabolic obesity: This can lead to numerous metabolic derangements like insulin resistance, dyslipidemias and hyperglycemia in conjunction with proinflammatory and prothrombotic factors even though they are non obese by usual BMI values.[23,36]
Pathophysiological effects of abdominal adiposity and increased cardiovascular risk in South Asians
For a better understanding of the clinico-epidemiological observations around obesity-associated cardiovascular risks, an insight into the underlying pathogenesis is useful. It is now well established that the insulin resistant, dyslipidemic, proinflammatory and prothrombotic state of abdominal obesity has been implicated as an important contributor in the pathogenesis of glucose intolerance and atherosclerotic CVD.[6] Obesity involves uneven increases in the amount of adipose tissue relative to other tissues, and Adipose tissue free fatty acids (FFA) turnover is also increased and the inhibition of lipolysis by insulin is decreased. The adipose tissue is the source of proinflammatory adipokines like tumor necrosis factor-alpha,interleukin-6, leptin, plasminogen activator inhibitor-1,angiotensiongen, resistin and C-reactive protein (CRP) that may play a role in metabolic and cardiovascular complications of obesity.[6] It is also the source of anti inflammatory and anti atherosclerotic adipokines i.e. Adiponectin. The same are depicted in the flow chart [Figure 2].
Figure 2.
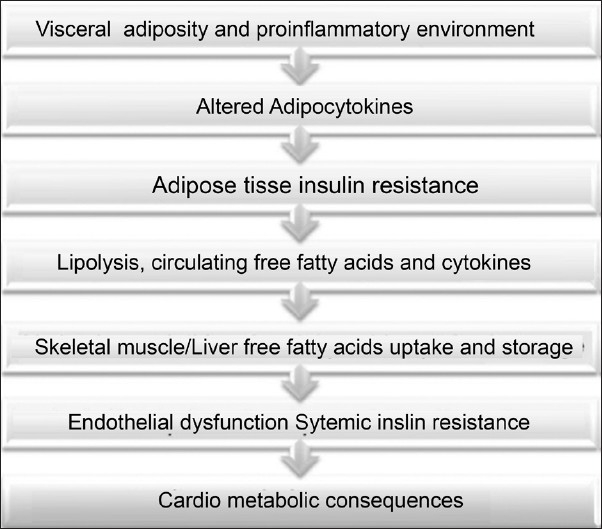
Pathophysiological effects of abdominal adiposity
Increased vascular risk observed in South Asians may be attributed to altered adipokine production or action.[37] Further, derangements in the adiponectin - insulin sensitivity axis may be an important biomarker linking visceral adiposity to atherogenesis in South Asians.[38] Insulin resistance, impaired fibrinolysis and endothelial dysfunction also occur as a result of lower Adiponectin. These lower levels of Adiponectin also predispose them to increased susceptibility to vascular and diabetic risk.[39,40] Further, they have higher plasma concentrations of leptin, (an adipose tissue metabolite) and nonesterified free fatty acids. Further, Leptin receptor gene polymorphism has been shown to have a role in obesity and Type 2 Diabetes mellitus.[41,42] Hence, there is likelihood of unique anthropometric, biochemical and genetic risk factors that cause for an increased cardiometabolic risk in South Asians.[14]
Determinants of obesity and cardiovascular disorders in South Asians
Role of body composition, Frame size / proportions
Evidence is emerging that proportion of fat free mass varies between populace of diverse ethnicities/racial backgrounds.[6] Body compositions of Asians in general and south Asians in particular, have consistently revealed a lower lean mass and a higher proportion of body fat than Caucasians.[8,43] Much of the ethnic variation in the relationship between BMI and body fatness is explained by differing body proportions and frame sizes.[6]
Role of body fat distribution
The risk imposed by central obesity is independent of BMI, and was found to be an important factor in those who would not be classified as obese based on their BMI alone. The correlation between increased abdominal adiposity and amplified levels of metabolic risk factors is strong and graded in South Asians, and appears to explain a proportion of the augmented risk of ill health at lower ΒMI.[4,43]
Role of ethnicity
The first clue that people of Asian origin were more prone to visceral obesity and CVD at low levels of BMI came from studies involving migrants from South Asia.[44] As stated earlier, Asians have 3 to 5% higher body fat than whites, at any given BMI.[8,25] Among Asians who have the same BMI, Chinese have the lowest percentage of body fat, while Indians have the highest.[25,45] At a given waist size, Asians have greater body fat and metabolic abnormalities.[8,46]
Rate of weight gain and duration
Evidence is emerging about importance of weight gain and duration as vital determinants of CVD risk than BMI alone.[6] Further, the association of weight gain, duration of adiposity and CVD risk is of importance in South Asians as they are showing rapid weight gain in their populace due to changing lifestyle.[14,47] However, the most alarming aspect of epidemiological transition in South Asia is the rapid increase in number of children who are overweight and affected by obesity.[23]
Rapid changes in diet and physical activity
As a consequence of globalization, increased urbanization and mechanization, dietary habits are changing and physical activity levels are reducing, resulting in a rapid increase in the mean body weight of the population in the South Asian region.[48,49] Further, South Asians are changing from the consumption of traditional frugal diets to energy rich imbalanced foods along with sedentary lifestyle.
Low birth weight and fetal under nutrition
Widespread prevalence of maternal malnutrition in South Asia resulting in low birth weight and fetal under nutrition, can have lasting undesirable effects on cardiometabolic risk factors in growing children.[47,50] Further as under nutrition coexists with over nutrition in South Asia, focusing on efforts to improve the nutrition during pregnancy, while simultaneously avoiding excessive weight gain needs consideration.
Socioeconomic factors
There is reversal of social gradient in cardiovascular risk factors in South Asians, and the disease burden shifts towards lower socioeconomic strata.[51] Further, the obstacles to control non communicable diseases in South Asia include extreme poverty and inadequate health infrastructure.[52]
Sociocultural factors
Lack of disease awareness, lack of health-seeking behavior, delayed diagnosis, language barriers, and religious and sociocultural factors are important in South Asia.[4] Illiteracy, ignorance and blind beliefs amongst women lead to maternal malnutrition, and mothers tend to feed their children with ghee, butter and other fats for growth and strength. Moreover women in certain communities are not allowed to leave their homes, thereby leading to physical inactivity.
Prevention and Control
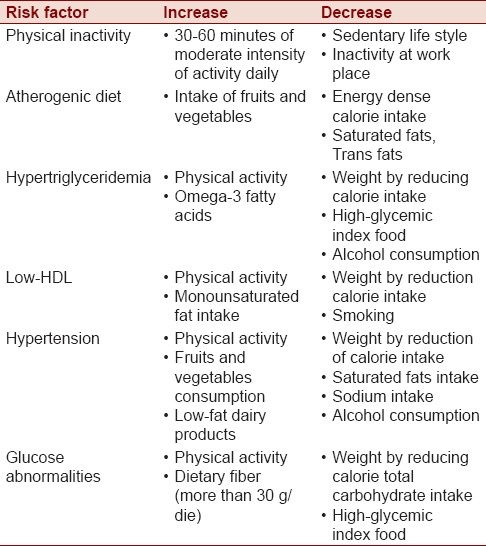
Prevention and control of noncommunicable diseases is a global priority for the WHO and obesity management is an important part of the strategy being employed.[5] The prevalence of obesity in children and adolescents is rapidly growing as well. The presence of obesity at this age appears to program adult obesity and CVD. The importance of early intervention for obesity in childhood, for future prevention of adult CVD, need to be emphasized.[53] The proper risk stratification for adolescents could direct clinicians in identifying overweight youth who are at an increased risk of developing pre-diabetes, diabetes, or CVD, and lead to a timely intervention. In this regard, life style changes that are beneficial for obesity related cardiovascular risk factors are listed in Table 2.
Table 2.
Life style intervention for cardiovascular disease risk factors associated with abdominal obesity
Obesity management should incorporate a broad range of long term strategies ranging from prevention, weight maintenance and management of obesity related comorbidities to weight loss.[54] It also necessitates both population approach and an individual approach. The population based effort should focus on the community, including schools and media; and, the individual approach should consist of a multidisciplinary strategy involving physicians, exercise specialists, dieticians, nurses and other health care personnel.[55] Further, it is imperative to stress that strategies should be cost effective, culturally sensitive, adoptable to local practices, and messages conveyed should be straightforward and implementable with meager health resources, omnipresent illiteracy, blind beliefs and ignorance in South Asian nations.
CONCLUSION
South Asians have a distinct obesity pattern in the form of increased fat mass and low lean mass than Whites for the same level of BMI. More importantly, the review indicates that the early onset of CVD risk among South Asians may be related to insulin resistant, dyslipidemic, proinflammatory, prothrombotic state of abdominal obesity. However, an altered adipokine production can also be linked to increased vascular risk, as observed among the South Asians. Evidence is emerging to suggest that there is a likelihood of unique anthropometric, biochemical and genetic risk factors for cardiometabolic risk in South Asians. Thus, a distinct clinical diagnostic tool for South Asians, as well as a tailored obesity management is warranted.
Moreover socio-cultural factors, economic factors, low birth weight status, and ethnicity, as an independent non-modifiable risk factor, can all contribute to increased obesity-associated CVD risk in South Asians. Such ethnic-specific determinants of obesity are crucial for prevention and control of obesity-associated illness in South Asians. In addition, the application of Asia-Pacific BMI cut-off point rather than the universal WHO BMI cut-off levels would be more scientific and accurate for estimating obesity-associated CVD risk burden in South Asians. Thus, we would like to conclude on a rather cautious note that anti-obesity management should be encouraged earlier in the life trajectory of South Asian populations. Though the escalating number of childhood obesity and overweight cases could be a challenge for the governments and healthcare providers, it would certainly contribute to positive health gains in the foreseeable future. Nevertheless, cost-effective interventions in reducing weight gain should be undertaken in local populations in real-life situations for further evidence in support of reducing CVD risk, not only in South Asians but also in similar populations elsewhere.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Valithan MS. Chennai, India: Orient Longman; 2003. The Legacy of Charaka. [Google Scholar]
- 2.Chadwick J, Mann WN. Boston MA: Blackwell Scientific; 1950. Medical Works of Hippocrates. [Google Scholar]
- 3.Razak F, Anand SS, Shannon H, Vuksan V, Davis B, Jacobs R, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115:2111–8. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- 4.Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes. 2011;35:167–87. doi: 10.1038/ijo.2010.135. [DOI] [PubMed] [Google Scholar]
- 5.Melbourne: World Health Organization, Western Pacific Region; 2000. The AsiaPacific perspective. Redefining obesity and its treatment. World Health Organization. International associaton for the study of obesity and International obesity task force. International Diabetes Institute. [Google Scholar]
- 6.Kopelman PG, Caterson ID, Dietz WH. New Delhi: Blackwell Publishing; 2006. Clinical Obesity in Adults and Children. First Indian Reprint. [Google Scholar]
- 7.Geneva: World Health Organization; 2000. World Health Organization. Technical report series 894: Obesity: Preventing and managing the global epidemic. (PDF) [PubMed] [Google Scholar]
- 8.Enas EA, Kannan S. 1st ed. Downers Grove, IL: Advanced Heart Lipid Clinic; 2008. How to Beat the Heart Disease Epidemic among South Asians. [Google Scholar]
- 9.Obesity in Asia Collaboration. Waist circumference thresholds provide an accurate and widely applicable method for the discrimination of diabetes. Diabetes Care. 2007;30:3116–8. doi: 10.2337/dc07-1455. [DOI] [PubMed] [Google Scholar]
- 10.Mohan V, Deepa M. Measuring obesity to assess cardiovascular risk-inch tape,weighing machine, or both? J Assoc Physicians India. 2007;55:617–9. [PubMed] [Google Scholar]
- 11.Arambepolaab C, Fernandob D, Ekanayakec R. A simple valid tool for measuring obesity-related-CHD risk in Sri Lankan adults. Prev Control. 2008;3:11–9. [Google Scholar]
- 12.Chopra HK, Kaur S, Sambi RS. Potbelly-The most powerful predictor of metabolic syndrome and premature morbidity and mortality. Indian Heart J. 2007;59:56–63. [PubMed] [Google Scholar]
- 13.Patel KC, Bhopal RS. Birmingham, UK: The South Asian Health Foundation; 2004. The epidemic of coronary heart disease in South Asian populations: Causes and consequences. [Google Scholar]
- 14.Mohan V, Rao GH. 1st ed. New Delhi: South Asian Society on Atherosclerosis and Thrombosis; 2007. Type 2 Diabetes in South Asians. [Google Scholar]
- 15.Omran A. The Epidemiologic Transition: A theory of epidemiology of population change. Millibank Q. 1971;49:509–38. [PubMed] [Google Scholar]
- 16.Ounpuu S, Negassa A, Yusuf S. INTER-HEART: A global study of risk factors for acute myocardial infarction. Am Heart J. 2001;141:711–21. doi: 10.1067/mhj.2001.114974. [DOI] [PubMed] [Google Scholar]
- 17.Prasad DS, Zubair K, Dash AK, Das BC. Cardiovascular risk factors in developing countries: A review of clinico-epidemiological evidence. CVD Prev Control. 2010;5:115–23. [Google Scholar]
- 18.Neel JV. Diabetes Mellitus: A “Thrifty” Genotype Rendered Detrimental by “Progress”. Am J Hum Genet. 1962;4:353–62. [PMC free article] [PubMed] [Google Scholar]
- 19.Hales CN, Barker DJ. Type 2 (non-insulin-dependent) diabetes mellitus: The thrifty phenotype hypothesis. Diabetologia. 1992;35:595–601. doi: 10.1007/BF00400248. [DOI] [PubMed] [Google Scholar]
- 20.Balkau B, Deanfield JE, Despres JP, Bassand JP, Fox KA, Smith SC, Jr, et al. International day for the evaluation of abdominal obesity (IDEA): A study of waist circumference, cardiovascular disease, and diabetes mellitus in 168 000 primary care patients in 63 countries. Circulation. 2007;116:1942–51. doi: 10.1161/CIRCULATIONAHA.106.676379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prasad DS, Kabir Z, Dash AK, Das BC. Coronary risk factors in South Asians: A prevalence study in an urban populace of Eastern India. CVD Prev Control. 2010;5:125–32. [Google Scholar]
- 22.Vaidya A, Shakya S, Krettek A. Obesity prevalence in Nepal: Public health challenges in a low-income nation during an alarming worldwide trend. Int J Environ Res Public Health. 2010;7:2726–44. doi: 10.3390/ijerph7062726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manoria PC, Manoria P, Manoria P. Metabolic obesity: A new therapeutic target for cardio-metabolic risk reduction. CVD Prev Control. 2010;5:39–44. [Google Scholar]
- 24.Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70. [PubMed] [Google Scholar]
- 25.Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–6. doi: 10.1046/j.1467-789x.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 26.Deurenberg-Yap M, Chew SK, Deurenberg P. Elevated body fat percentage and cardiovascular risks at low body mass index levels among Singaporean Chinese, Malays and Indians. Obes Rev. 2002;3:209–15. doi: 10.1046/j.1467-789x.2002.00069.x. [DOI] [PubMed] [Google Scholar]
- 27.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 28.Brussels, editor. Belgium: International Diabetes Federation; 2006. The IDF consensus worldwide definition of the Metabolic Syndrome. IDF Communications. [Google Scholar]
- 29.Kannel WB, Cupples LA, Ramaswamy R, Stokes JI, Kreger BE, Higgins MW. Regional obesity and risk of cardiovascular disease; the Framingham Study. J Clin Epidemiol. 1991;44:183–90. doi: 10.1016/0895-4356(91)90265-b. [DOI] [PubMed] [Google Scholar]
- 30.Despres J. Targeting abdominal obesity and the metabolic syndrome to manage cardiovascular disease risk. Heart. 2009;95:1118–24. doi: 10.1136/hrt.2008.151274. [DOI] [PubMed] [Google Scholar]
- 31.Asia Pacific Cohort Studies Collaboration. Central obesity and risk of cardiovascular disease in the Asia Pacific Region. Asia Pac J Clin Nutr. 2006;15:287–92. [PubMed] [Google Scholar]
- 32.Gupta R, Rastogi P, Sarna M, Gupta VP, Sharma SK, Kothari K. Body-mass index, waist-size, waist-hip ratio and cardiovascular risk factors in urban subejcts. J Assoc Physicians India. 2007;55:621–7. [PubMed] [Google Scholar]
- 33.Kulkarni ML, Mythri HP, Kulakarni AM. ‘Thinfat’ Phenotype in Newborns. Indian J Pediatr. 2009;76:369–73. doi: 10.1007/s12098-009-0010-8. [DOI] [PubMed] [Google Scholar]
- 34.Krishnaveni GV, Veena SR, Chachyamma KJ. Truncal adiposity is present at birth and in early childhood in South Indian children. Indian Pediatr. 2005;42:527–38. [PubMed] [Google Scholar]
- 35.Mohan V, Deepa R. Adipocytokines and The Expanding ‘Asian Indian Phenotype’. J Assoc Physicians India. 2006;54:685–6. [PubMed] [Google Scholar]
- 36.Ruderman N, Chisholm D, Pi-Sunyer X, Schneider S. The metabolically obese, normal-weight individual revisited. Diabetes. 1998;47:699–713. doi: 10.2337/diabetes.47.5.699. [DOI] [PubMed] [Google Scholar]
- 37.Gupta M, Brister S. Is South Asian ethnicity an independent cardiovascular risk factor? Can J Cardiol. 2006;22:193–7. doi: 10.1016/s0828-282x(06)70895-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gupta M, Singh N, Verma S. South Asians and cardiovascular risk: What clinicians should know. Circulation. 2006;113:e924–29. doi: 10.1161/CIRCULATIONAHA.105.583815. [DOI] [PubMed] [Google Scholar]
- 39.Raji A, Gerhard-Herman MD, Warren M, Silverman SG, Raptopoulos V, Mantzoros CS, et al. Insulin resistance and vascular dysfunction in nondiabetic Asian Indians. J Clin Endocrinol Metab. 2004;89:3965–72. doi: 10.1210/jc.2004-0087. [DOI] [PubMed] [Google Scholar]
- 40.Snehalatha C, Mukesh B, Simon M, Viswanathan V, Haffner SM, Ramachandran A. Plasma adiponectin is an independent predictor of type 2 diabetes in Asian Indians. Diabetes Care. 2003;26:3226–9. doi: 10.2337/diacare.26.12.3226. [DOI] [PubMed] [Google Scholar]
- 41.Abate N, Chandalia M, Snell PG, Grundy SM. Adipose tissue metabolites and insulin resistance in nondiabetic Asian Indian men. J Clin Endocrinol Metab. 2004;89:2750–5. doi: 10.1210/jc.2003-031843. [DOI] [PubMed] [Google Scholar]
- 42.Murugesan D, Arunachalam T, Ramamurthy V, Subramanian S. Association of polymorphisms in leptin receptor gene with obesity and type 2 diabetes in the local population of Coimbatore. Indian J Hum Genet. 2010;16:72–7. doi: 10.4103/0971-6866.69350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Misra A, Khurana L. The metabolic syndrome in South Asians: Epidemiology, determinants, and prevention. Metab Syndr Relat Disord. 2009;7:497–514. doi: 10.1089/met.2009.0024. [DOI] [PubMed] [Google Scholar]
- 44.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991;337:382–6. doi: 10.1016/0140-6736(91)91164-p. [DOI] [PubMed] [Google Scholar]
- 45.Deurenberg-Yap M, Schmidt G, van Staveren WA, Deurenberg P. The paradox of low body mass index and high body fat percentage among Chinese, Malays and Indians in Singapore. Int J Obes Relat Metab Disord. 2000;24:1011–7. doi: 10.1038/sj.ijo.0801353. [DOI] [PubMed] [Google Scholar]
- 46.Razak F, Anand S, Vuksan V, Davis B, Jacobs R, Teo KK, et al. Ethnic differences in the relationships between obesity and glucose-metabolic abnormalities: A cross-sectional population-based study. Int J Obes. 2005;29:656–67. doi: 10.1038/sj.ijo.0802937. [DOI] [PubMed] [Google Scholar]
- 47.Yajnik CS. Early life origins of insulin resistance and type 2 diabetes in India and other Asian countries. J Nutr. 2004;134:205–10. doi: 10.1093/jn/134.1.205. [DOI] [PubMed] [Google Scholar]
- 48.New Delhi: World Health Organization, Country Office, India and Ministry of Health and Family Welfare, Government of India; 2006. Recommendations for a National Plan of Action for the Implementation of WHO's Global strategy on Diet, Physical Activity and Health in India. [Google Scholar]
- 49.Prasad DS, Das BC. Physical inactivity: A cardiovascular risk factor. Indian J Med Sci. 2009;63:33–42. [PubMed] [Google Scholar]
- 50.Nair MK, Nair L, Chacko DS, Zulfikar AM, George B, Sarma PS. Markers of fetal onset adult diseases: A comparison among low birth weight and normal birth weight adolescents. Indian Pediatr. 2009;46:S43–7. [PubMed] [Google Scholar]
- 51.Gupta R, Gupta VP, Sarna M, Prakash H, Rastogi S, Gupta KD. Serial epidemiological surveys in an urban Indian population demonstrate increasing coronary risk factors among the lower socioeconomic strata. J Assoc Physicians India. 2003;51:470–7. [PubMed] [Google Scholar]
- 52.Ghaffar A, Reddy KS, Singh M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328:807–10. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS. Childhood adiposity as a predictor of cardiac mass in adulthood: The Bogalusa heart study. Circulation. 2004;110:3488–92. doi: 10.1161/01.CIR.0000149713.48317.27. [DOI] [PubMed] [Google Scholar]
- 54.Macdonald IA, Atkinson R. Public health initiatives in obesity prevention: The need for evidence-based policy. Int J Obes. 2011;35:463. doi: 10.1038/ijo.2011.14. [DOI] [PubMed] [Google Scholar]
- 55.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93:s9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]


