Abstract
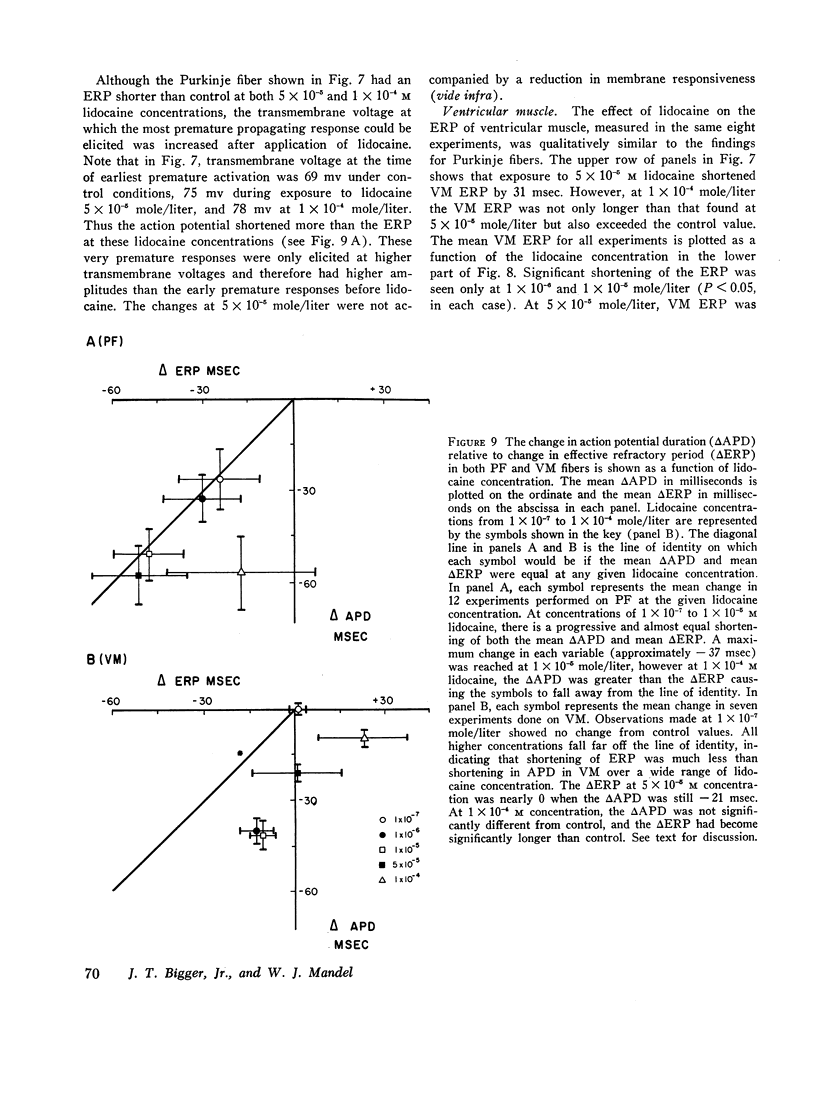
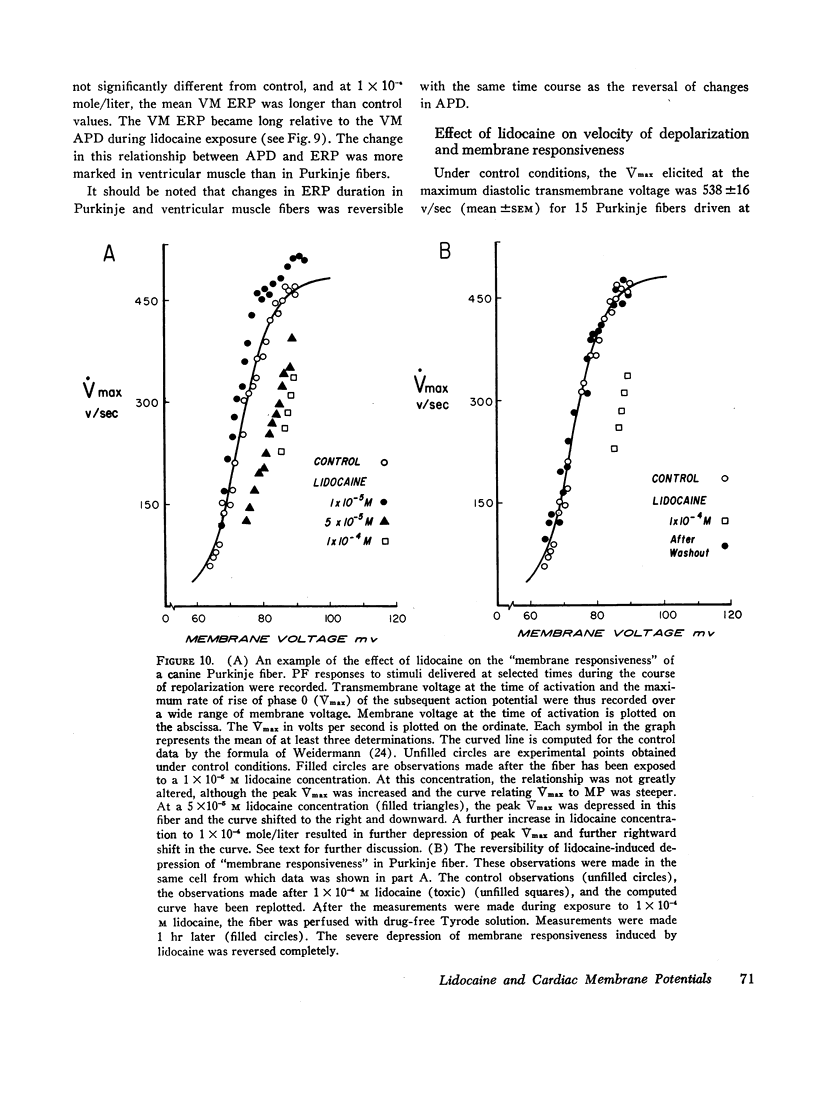
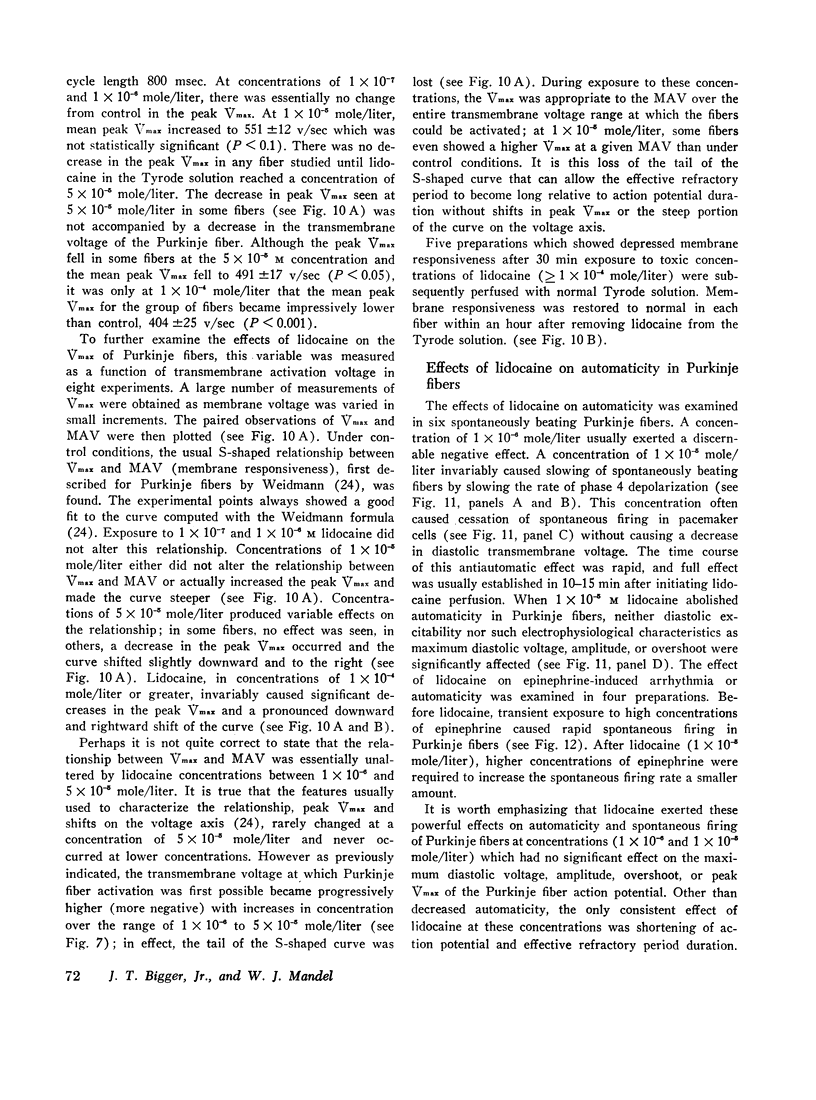
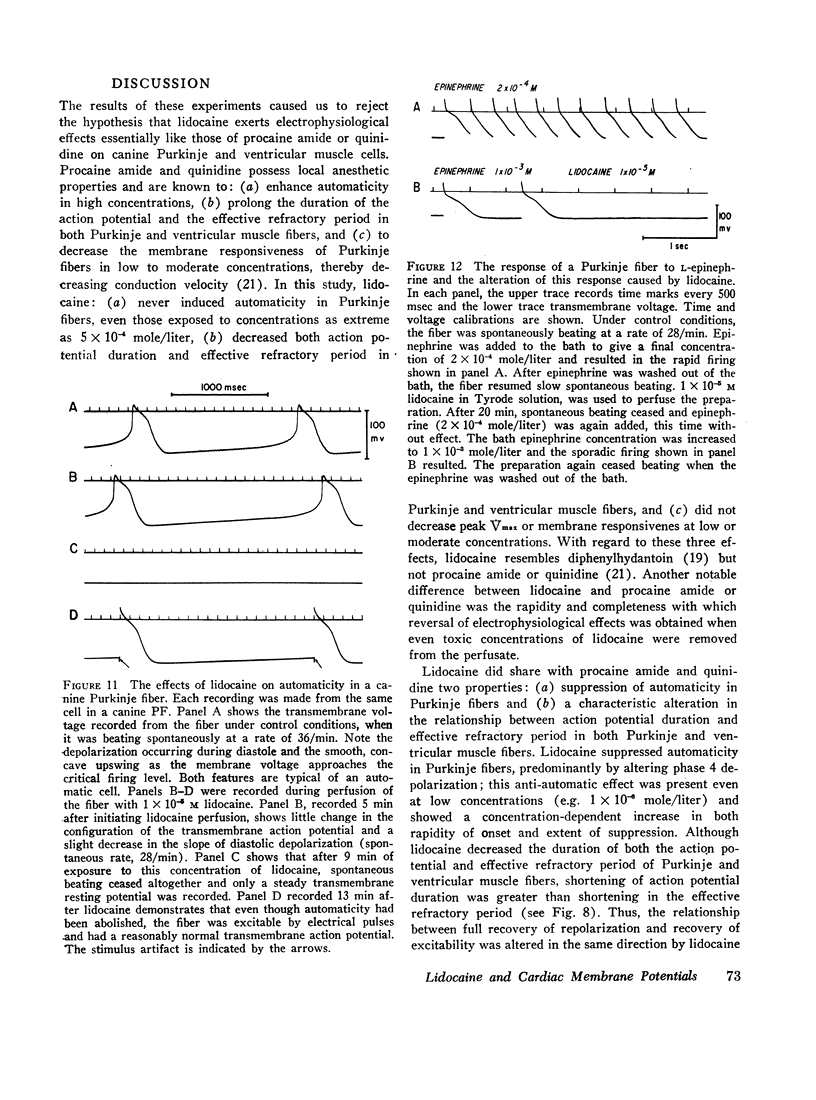
Preparations of right ventricular papillary muscle and false tendon (Purkinje fiber) were obtained from dog hearts, placed in a bath perfused with Tyrode solution, and observed both under control conditions and during exposure to lidocaine in concentrations from 1 × 10-7 to 5 × 10-4 mole/liter. Transmembrane voltages were recorded from both ventricular muscle (VM) and Purkinje fibers (PF) of spontaneously beating and electrically driven preparations. Low concentrations (1 × 10-6 and 1 × 10-5 mole/liter) attenuated or abolished phase 4 (diastolic) depolarization and spontaneous firing in PF without decreasing their diastolic excitability. Concentrations of 1 × 10-5 mole/liter produced maximal shortening of both action potential duration (APD) and effective refractory period (ERP) and made the ERP long relative to APD; the latter alteration was more prominent in VM. At concentrations ≤ 1 × 10-5 mole/liter, lidocaine either caused a slight increase or no change in peak maximum rate of phase 0 depolarization (Vmax) and membrane responsiveness, the relationship between transmembrane activation voltage (MAV) and Vmax of the resultant action potential; these concentrations had no significant effect on resting potential (RP) in VM, maximal diastolic transmembrane voltage (DTMVmax) in PF, or action potential amplitude in either fiber type.
High (toxic) concentrations (≥ 1 × 10-4 mole/liter) did not cause further shortening of APD or ERP in either VM or PF but did produce a decrease in peak Vmax of phase 0 and membrane responsiveness. In most cases, these concentrations also caused a decrease in RP or DTMVmax and action potential amplitude, with progression to bizarre action potential depolarization and inexcitability. These properties of lidocaine are strikingly different from those of quinidine or procaine amide. The mechanisms responsible for lidocaine's in vivo antiarrhythmic action are discussed.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Austen W. G., Moran J. M. Cardiac and peripheral vascular effects of lidocaine and procainamide. Am J Cardiol. 1965 Nov;16(5):701–707. doi: 10.1016/0002-9149(65)90054-8. [DOI] [PubMed] [Google Scholar]
- Bianchi C. P., Bolton T. C. Action of local anesthetics on coupling systems in muscle. J Pharmacol Exp Ther. 1967 Aug;157(2):388–405. [PubMed] [Google Scholar]
- Bigger J. T., Jr, Bassett A. L., Hoffman B. F. Electrophysiological effects of diphenylhydantoin on canine purkinje fibers. Circ Res. 1968 Feb;22(2):221–236. doi: 10.1161/01.res.22.2.221. [DOI] [PubMed] [Google Scholar]
- Bigger J. T., Jr, Heissenbuttel R. H. The use of procaine amide and lidocaine in the treatment of cardiac arrhythmias. Prog Cardiovasc Dis. 1969 May;11(6):515–534. doi: 10.1016/0033-0620(69)90004-8. [DOI] [PubMed] [Google Scholar]
- Dudel J., Peper K., Rüdel R., Trautwein W. The dynamic chloride component of membrane current in Purkinje fibers. Pflugers Arch Gesamte Physiol Menschen Tiere. 1967;295(3):197–212. doi: 10.1007/BF01844100. [DOI] [PubMed] [Google Scholar]
- Dudel J., Peper K., Rüdel R., Trautwein W. The potassium component of membrane current in Purkinje fibers. Pflugers Arch Gesamte Physiol Menschen Tiere. 1967;296(4):308–327. doi: 10.1007/BF00362531. [DOI] [PubMed] [Google Scholar]
- FEINSTEIN M. B. REACTION OF LOCAL ANESTHETICS WITH PHOSPHOLIPIDS. A POSSIBLE CHEMICAL BASIS FOR ANESTHESIA. J Gen Physiol. 1964 Nov;48:357–374. doi: 10.1085/jgp.48.2.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frieden J. Antiarrhythmic drugs. VII. Lidocaine as an antiarrhythmic agent. Am Heart J. 1965 Nov;70(5):713–715. doi: 10.1016/0002-8703(65)90399-6. [DOI] [PubMed] [Google Scholar]
- Gianelly R., von der Groeben J. O., Spivack A. P., Harrison D. C. Effect of lidocaine on ventricular arrhythmias in patients with coronary heart disease. N Engl J Med. 1967 Dec 7;277(23):1215–1219. doi: 10.1056/NEJM196712072772301. [DOI] [PubMed] [Google Scholar]
- HARRISON D. C., SPROUSE J. H., MORROW A. G. THE ANTIARRHYTHMIC PROPERTIES OF LIDOCAINE AND PROCAINE AMIDE. CLINICAL AND PHYSIOLOGIC STUDIES OF THEIR CARDIOVASCULAR EFFECTS IN MAN. Circulation. 1963 Oct;28:486–491. doi: 10.1161/01.cir.28.4.486. [DOI] [PubMed] [Google Scholar]
- HITCHCOCK P., KEOWN K. K. The management of cardiac arrhythmias during cardiac surgery. South Med J. 1959 Jun;52(6):702–706. doi: 10.1097/00007611-195906000-00015. [DOI] [PubMed] [Google Scholar]
- HOFFMAN B. F., CRANEFIELD P. F. THE PHYSIOLOGICAL BASIS OF CARDIAC ARRHYTHMIAS. Am J Med. 1964 Nov;37:670–684. doi: 10.1016/0002-9343(64)90017-8. [DOI] [PubMed] [Google Scholar]
- Hilmi K. I., Regan T. J. Relative effectiveness of antiarrhythmic drugs in treatment of digitalis-induced ventricular tachycardia. Am Heart J. 1968 Sep;76(3):365–369. doi: 10.1016/0002-8703(68)90232-9. [DOI] [PubMed] [Google Scholar]
- Hoffman B. F. The genesis of cardiac arrhythmias. Prog Cardiovasc Dis. 1966 Jan;8(4):319–329. doi: 10.1016/s0033-0620(66)80009-9. [DOI] [PubMed] [Google Scholar]
- KAO C. Y., HOFFMAN B. F. Graded and decremental response in heart muscle fibers. Am J Physiol. 1958 Jul;194(1):187–196. doi: 10.1152/ajplegacy.1958.194.1.187. [DOI] [PubMed] [Google Scholar]
- Katz M. J., Zitnik R. S. Direct current shock and lidocaine in the treatment of digitalis-induced ventricular tachycardia. Am J Cardiol. 1966 Oct;18(4):552–556. doi: 10.1016/0002-9149(66)90010-5. [DOI] [PubMed] [Google Scholar]
- Keenaghan J. B. The determination of lidocaine and prilocaine in whole blood by gas chromatography. Anesthesiology. 1968 Jan-Feb;29(1):110–112. doi: 10.1097/00000542-196801000-00029. [DOI] [PubMed] [Google Scholar]
- LIKOFF W. Cardiac arrhythmias complicating surgery. Am J Cardiol. 1959 Apr;3(4):427–429. doi: 10.1016/0002-9149(59)90362-5. [DOI] [PubMed] [Google Scholar]
- Lieberman N. A., Harris R. S., Katz R. I., Lipschutz H. M., Dolgin M., Fisher V. J. The effects of lidocaine on the electrical and mechanical activity of the heart. Am J Cardiol. 1968 Sep;22(3):375–380. doi: 10.1016/0002-9149(68)90122-7. [DOI] [PubMed] [Google Scholar]
- Lown B., Fakhro A. M., Hood W. B., Jr, Thorn G. W. The coronary care unit. New perspectives and directions. JAMA. 1967 Jan 16;199(3):188–198. [PubMed] [Google Scholar]
- McAllister R. E., Noble D. The time and voltage dependence of the slow outward current in cardiac Purkinje fibres. J Physiol. 1966 Oct;186(3):632–662. doi: 10.1113/jphysiol.1966.sp008060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narahashi T., Moore J. W. Neuroactive agents and nerve membrane conductances. J Gen Physiol. 1968 May;51(5 Suppl):93S+–93S+. [PubMed] [Google Scholar]
- Noble D., Tsien R. W. The kinetics and rectifier properties of the slow potassium current in cardiac Purkinje fibres. J Physiol. 1968 Mar;195(1):185–214. doi: 10.1113/jphysiol.1968.sp008454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peper K., Trautwein W. A membrane current related to the plateau of the action potential of Purkinje fibers. Pflugers Arch. 1968;303(2):108–123. doi: 10.1007/BF00592629. [DOI] [PubMed] [Google Scholar]
- Reuter H. The dependence of slow inward current in Purkinje fibres on the extracellular calcium-concentration. J Physiol. 1967 Sep;192(2):479–492. doi: 10.1113/jphysiol.1967.sp008310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie J. M., Greengard P. On the mode of action of local anesthetics. Annu Rev Pharmacol. 1966;6:405–430. doi: 10.1146/annurev.pa.06.040166.002201. [DOI] [PubMed] [Google Scholar]
- Ritchie J. M., Ritchie B. R. Local anesthetics: effect of pH on activity. Science. 1968 Dec 20;162(3860):1394–1395. doi: 10.1126/science.162.3860.1394. [DOI] [PubMed] [Google Scholar]
- SOUTHWORTH J. L., McKUSICK V. A., PIERCE E. C., 2nd, RAWSON F. L., Jr Ventricular fibrillation precipitated by cardiac catheterization; complete recovery of the patient after 45 minutes. J Am Med Assoc. 1950 Jun 24;143(8):717–720. doi: 10.1001/jama.1950.02910430009003. [DOI] [PubMed] [Google Scholar]
- SUNG C. Y., TRUANT A. P. The physiological disposition of lidocaine and its comparison in some respects with procaine. J Pharmacol Exp Ther. 1954 Dec;112(4):432–443. [PubMed] [Google Scholar]
- Schumacher R. R., Lieberson A. D., Childress R. H., Williams J. F., Jr Hemodynamic effects of lidocaine in patients with heart disease. Circulation. 1968 Jun;37(6):965–972. doi: 10.1161/01.cir.37.6.965. [DOI] [PubMed] [Google Scholar]
- Singer D. H., Lazzara R., Hoffman B. F. Interrelationship between automaticity and conduction in Purkinje fibers. Circ Res. 1967 Oct;21(4):537–558. doi: 10.1161/01.res.21.4.537. [DOI] [PubMed] [Google Scholar]
- Spracklen F. H., Kimerling J. J., Besterman E. M., Litchfield J. W. Use of lignocaine in treatment of cardiac arrhythmias. Br Med J. 1968 Jan 13;1(5584):89–91. doi: 10.1136/bmj.1.5584.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss H. C., Bigger J. T., Jr, Bassett A. L., Hoffman B. F. Actions of diphenylhydatoin on the electrical properties of isolated rabbit and canine atria. Circ Res. 1968 Sep;23(3):463–477. doi: 10.1161/01.res.23.3.463. [DOI] [PubMed] [Google Scholar]
- TAYLOR R. E. Effect of procaine on electrical properties of squid axon membrane. Am J Physiol. 1959 May;196(5):1071–1078. doi: 10.1152/ajplegacy.1959.196.5.1071. [DOI] [PubMed] [Google Scholar]
- TRUANT A. P., TAKMAN B. Differential physical-chemical and neuropharmacologic properties of local anesthetic agents. Anesth Analg. 1959 Nov-Dec;38:478–484. [PubMed] [Google Scholar]
- WEIDMANN S. Effects of calcium ions and local anesthetics on electrical properties of Purkinje fibres. J Physiol. 1955 Sep 28;129(3):568–582. doi: 10.1113/jphysiol.1955.sp005379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WEIDMANN S. The effect of the cardiac membrane potential on the rapid availability of the sodium-carrying system. J Physiol. 1955 Jan 28;127(1):213–224. doi: 10.1113/jphysiol.1955.sp005250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WEISS W. A. Intravenous use of lidocaine for ventricular arrhythmias. Anesth Analg. 1960 Jul-Aug;39:369–381. [PubMed] [Google Scholar]