Abstract
In the evidence-based medicine era, objective treatment guidelines have been laid down for pulmonary tuberculosis, but the same is not true for osteoarticular tuberculosis. This has led to demands for standardising the treatment protocol and to a lack of consensus between doctors regarding the composition and duration of treatment. Twenty-five patients with extraspinal osteoarticular tuberculosis were evaluated prospectively. Following the diagnosis, patients were given standard directly observed treatment short course (DOTS) regimen and were monitored for disease activity at zero, three and six months with the help of technetium-99m-labelled ciprofloxacin (99m Tc) scan. Tracer activity at the site was recorded and compared on sequential scans. Clinical and radiological profile of all the patients were also recorded at regular intervals and compared. All 25 cases had a positive 99mTc bone scan initially. Four patients (16%) converted to negative scans at three months, whereas the remaining 21 patients (84%) showed negative scans at six months. The end of six months therapy also coincided with resolution of clinical and radiological parameters in all cases. In conclusion, 99mTc scan is a promising tool for monitoring drug response in osteoarticular tuberculosis; however, due to the small sample size, studies with a large number of patients might be of help.
Introduction
Tuberculosis has been declared a global emergency by the World Health Organisation (WHO) [1, 2]. Though osteoarticular tuberculosis constitutes only 1–3% of all tubercular cases, it is an important cause of morbidity in developing countries because of its high prevalence [3]. High index of suspicion and meticulous clinicoradiological evaluation remains the mainstay of diagnosis in these cases. Whereas objective criteria have been established for pulmonary tuberculosis, such as sputum microscopy for both initiating and ceasing treatment, the same is not true for skeletal tuberculosis, as it is a paucibacillary disease [4]. Imaging modalities such as magnetic resonance imaging (MRI) are useful in monitoring disease status, but there is no modality to date that has been able to exactly pinpoint the time of disease activity cessation in skeletal tuberculosis that can guide the clinician to stop the chemotherapy at the earliest opportunity, thereby ensuring cure as well as avoiding chemotherapy side effects and minimising treatment cost.
Chemotherapy duration for treating osteoarticular tuberculosis is also under considerable debate. Presumably, poor penetration of skeletal tubercular foci by antitubercular drugs has led to the long duration of treatment regimens for the condition. There is an apprehension among surgeons that the standard six month short-course chemotherapy currently being advocated by the World Health Organisation (WHO) [5] may not be an adequate period of treatment. Infections in bones have always been difficult to eradicate, which is why prolonged antitubercular therapy (nine–18 months) is still routinely prescribed in endemic countries such as India.
Recently, ciprofloxacin labelled with technetium-99m (99mTc) has been shown to be a highly sensitive and specific marker for diagnosing osteoarticular infections. So we decided to study the course of osteoarticular tuberculosis after starting chemotherapy and to assess the adequacy of a short-course regimen by monitoring disease activity with the help of sequential 99mTc-labelled ciprofloxacin scan.
Materials and methods
This prospective study was conducted in the Department of Orthopaedics, Maulana Azad Medical College and Lok Nayak Hospital in association with the Department of Nuclear Medicine, Institute of Medical Allied Science (INMAS), Timarpur, New Dehli, India from 1 October 2006 to 31 January 2008. The study consisted of 25 newly diagnosed cases of extra-spinal osteoarticular tuberculosis (Table 1), aged in the range of 3–65 (mean 21) years. The purpose of the study was explained to each patient, and a written informed consent was obtained.
Table 1.
Patient information
| Patient no. | Age (years)/Sex | Site of Involvement | First scan | Second scan | Third scan |
|---|---|---|---|---|---|
| 1 | 56/M | Hip | + | + | - |
| 2 | 4/F | Carpal bones | + | - | - |
| 3 | 28/F | Hip | + | + | - |
| 4 | 19/F | Knee | + | + | - |
| 5 | 25/F | Tibia | + | + | - |
| 6 | 17/F | SI joint | + | + | - |
| 7 | 30/F | Ankle | + | + | - |
| 8 | 4/M | Elbow | + | + | - |
| 9 | 26/M | Foot | + | + | - |
| 10 | 20/F | Ankle | + | - | - |
| 11 | 9/F | Hip | + | + | - |
| 12 | 21/M | Hip | + | + | - |
| 13 | 25/F | Knee | + | + | - |
| 14 | 47/M | Olecranon | + | - | - |
| 15 | 65/F | Hip | + | + | - |
| 16 | 16/M | Elbow | + | + | - |
| 17 | 3/M | Fibula | + | - | - |
| 18 | 16/F | Elbow | + | + | - |
| 19 | 13/M | Foot | + | + | - |
| 20 | 35/F | Hip | + | + | - |
| 21 | 18/F | Elbow | + | + | - |
| 22 | 24/M | Hip | + | + | - |
| 23 | 19/M | Foot | + | + | - |
| 24 | 23/F | Elbow | + | + | - |
| 25 | 12/F | Hip | + | + | - |
Patients suspected of having extra-spinal osteoarticular tuberculosis were evaluated thoroughly to establish a clinicoradiological diagnosis. Patients were classified as definite or probable cases [6]. Patients who had already taken chemotherapy for more than one week, and pregnant and lactating women, were excluded. All patients were investigated for estimation of haemoglobin level (Hb), total leukocyte count (TLC), differential leukocyte count (DLC), erythrocyte sedimentation rate (ESR) and chest X-ray. Histopathological diagnosis was established in five cases. In six cases of tubercular arthritis, joint fluid was aspirated and the polymerase chain reaction (PCR) test for Mycobacterium tuberculosis was positive. In four cases, MRI of the affected region was done and was used as the corroborative evidence for tuberculosis. The remaining ten cases had typical clinicoradiological features of tuberculosis. Patients thus diagnosed as having extraspinal skeletal tuberculosis were then subjected to 99mTc-ciprofloxacin-labelled bone scan. Each cold ciprofloxacin kit vial contained 2 mg of lyophilised powder and 180 mg of stannous chloride. For reconstitution, the rubber cap of the vial was disinfected, and about 25.0 mCi radioactivity of pertechnetate (99mTc) was injected into the vial. The contents of the vial were shaken and incubated for ten minutes at room temperature. The radioligand (99mTc ciprofloxacin) from the vial was syringed through a 0.22-μm Millipore filter. An intravenous injection of approximately 20 mCi (740 MBq) radioactivity of the radiopharmaceutical (99mTc ciprofloxacin) was given to each patient. Anterior and posterior isotime (five minutes each) images of the suspected site were acquired under the dual-headed gamma camera in 256 x 256 matrix at one, four and 24 hours following radiopharmaceutical administration. The anterior and posterior images were subjected to a quantitative analysis to calculate the lesion-to-background ratio of the radiotracer accumulating at infection site and were evaluated by specialists blinded to clinical data. The imaging was considered positive if there was a distinct positive uptake of tracer at the suspected site.
All cases were then started on antitubercular therapy according to directly observed treatment short course (DOTS) regimen, as per the Revised National Tuberculosis Control Programme (RNTCP) of India. Follow-up was done at weekly intervals during the intensive phase and monthly thereafter until 24 months after completion of therapy. During every visit, all patients were assessed for four quantitative (weight, ESR, pain, tenderness) and two qualitative parameters (fever and anorexia). Pain and tenderness were graded according to the system given in Table 2. Constitutional symptoms were described as either present or absent. The results were analysed using standard statistical tests.
Table 2.
Pain and tenderness grading scale
| Grade | Criteria |
|---|---|
| Pain | |
| Grade 1 | No pain/minimal pain (patient has pain but can continue daily activities normally). |
| Grade 2 | Moderate pain (patient can carry out daily activities but with difficulty) |
| Grade 3 | Moderately severe pain (patient has to modify activities due to pain) |
| Grade 4 | Severe pain (patient cannot perform day to day activities) |
| Tenderness | |
| Grade 1 | No/minimal tenderness (patient complains of pain but does not wince on palpation) |
| Grade 2 | Patient complains of pain and winces on palpation. |
| Grade 3 | Patient winces and withdraws the affected limb on palpation. |
| Grade 4 | Patient does not allow examination. |
Results
All patients had pain and tenderness at the initial presentation, and all of them showed progressive improvement following treatment. The mean scores for pain and tenderness decreased from 3.46 and 3.29, respectively, at the time of the first scan to 1.00 at the third scan after six months of short-course chemotherapy. Statistical analysis of sequential pain and tenderness scores using z test revealed significant improvement in scores (p <0.05). All (100%) patients gained weight during the course of the treatment. Mean body weight was 40.3 kg before starting the therapy and rose to 42.80 kg after three months of therapy and 45.50 kg after completion of six months therapy, and all showed consistent improvement in ESR during the course of chemotherapy, with the mean values decreasing from 53.03 to 10.53 mm in the first hour. The majority (83%) of patients had constitutional symptoms of tuberculosis in the form of anorexia and low-grade fever at the time of diagnosis. All showed marked improvement in these symptoms within two to three months of starting treatment. Constitutional symptoms were the earliest parameter to improve with chemotherapy.
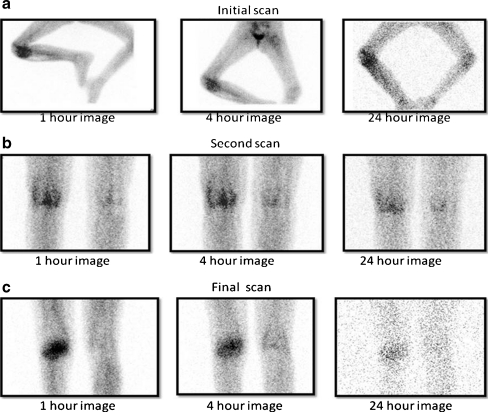
All 25 patients with extraspinal skeletal tuberculosis showed a positive scan (Table 1) before starting treatment. Of these, four patients (16%) converted to negative scans at the end of three months therapy. The scan at the completion of chemotherapy was negative in all these patients. Though only qualitative analysis of scan results was done in this study, progressive diminution in scan activity was observed during the sequential scanning (Fig. 1a–c).
Fig. 1.
a–c Sequential diminution of tracer uptake in a case of tuberculosis of the knee
Discussion
With the introduction of rifampicin and pyrazinamide, it is possible to reduce the duration of treatment for osteoarticular tuberculosis to six or eight months [7]. The occurrence of various side effects is significantly reduced using the same drugs twice or thrice a week [8]. A study in Korea, as well as the Fourteenth Report of the Medical Research Council showed that six and nine months regimen of isoniazid and rifampicin was comparable to the previously established regimen of 12–18 months [9, 10]. The Netherlands Tuberculosis Registry (NTR) data reported that the relapse rate following short-course chemotherapy is much lower and almost equivalent to reinfection rate [11].
Various parameters have been used over a period of years to help the clinician make the diagnosis and follow-up the course of osteoarticular tuberculosis in the absence of any objective criteria. Among all the haematological parameters, increased ESR has been observed to be a consistent finding in these cases [12, 13]. Various other serological investigations, such as enzyme-linked immunosorbent assay (ELISA) for antibody to mycobacterial antigen-6 [14] and polymerase chain reaction (PCR) [15–17] have shown good sensitivity and specificity in diagnosing skeletal tuberculosis, but they are not useful for following the disease course or defining the end point of treatment. Even recent imaging modalities such as MRI cannot differentiate between residual infection and postinfection reparative process once treatment is completed [18, 19].
Recently, 99mTC-labeled ciprofloxacin scan has been used to detect bone infections specifically. This scan has high sensitivity and specificity in detecting skeletal infection [20–22], but no study has been performed to investigate its role in tubercular infection. Ciprofloxacin is a potent broad-spectrum antibiotic that is active against most gram-positive and gram-negative bacteria and mycobacteria by virtue of binding to the DNA-gyrase enzyme in living bacteria. The therapeutic property of the drug has been exploited for diagnostic use. The complex formed by chelation of 99mTc with ciprofloxacin is strong, as indicated by in vitro serum stability and in vivo biodistribution experiments. The in vitro and in vivo study results have shown satisfactory labelling of ciprofloxacin with 99mTc, which is stable for up to 24 hours and has both hepatobiliary and renal routes of excretion [23]. No bone marrow uptake or blood-pool activity (visible cardiac cavities) on one, four and 24-hour image was seen. Initial in vitro and animal studies showed that 99mTc ciprofloxacin localises in lesions caused by living bacteria but does not localise in areas of sterile inflammation or abscess with dead bacteria [20, 21, 24]. Most false-positive images seen at four hours in chronic noninfective inflammatory disorders become negative when imaged at 24 hours; thus, 24-hour imaging is mandatory for evaluating chronic infections such as tuberculosis [21]. The main factor of 99mTc-ciprofloxacin imaging is considered to be tracer uptake by bacteria, which is distinct from its antibacterial activity, as bacteria resistant to ciprofloxacin can still take up 99mTc ciprofloxacin if their resistance is mediated only through DNA-gyrase alteration.
In a recent study, 99mTc ciprofloxacin was employed to detect tuberculosis in patients clinically suspected as having the disease. These patients were later subjected to various tests to establish or refute the diagnosis of skeletal tuberculosis, and a high degree of correlation was found with the scan [25]. In all of the above-mentioned studies using 99mTc ciprofloxacin, no patient was reported to have had any adverse reactions to the radiopharmaceutical agent. In our study, we found that 99mTc scan is a promising tool for monitoring drug response in cases of extra-spinal osteoarticular tuberculosis, almost akin to sputum microscopy for pulmonary tuberculosis. All 25 patients with extraspinal osteoarticular tuberculosis showed positive scan before treatment began. All patients achieved clinical, haematological and radiological cure after six months of short-course chemotherapy. The 99mTc ciprofloxacin scan done at this time was also negative in all patients. Though only qualitative analysis of scan results was done in this study, progressive diminution in scan activity was observed during the sequential scanning, which can be logically be assumed to be a reflection of decreasing bacterial load and disease activity at the site of infection. Four patients became scan negative after three months of chemotherapy, and, interestingly, all had involvement of small peripheral joints and presented relatively earlier than the other patients. None of the eight hip or two knee cases converted to negative scan after three months. Among five cases of tubercular arthritis of the elbow, only one converted to negative scan after three months of chemotherapy. In comparison with the other four patients with tuberculosis of the elbow joint, this patient had shorter disease duration before starting chemotherapy. This could possibly be because the patient was harbouring a decreased bacterial load and hence the early sterilisation of the lesions. However, as the sample size in this study is not large, a larger study with more cohorts may further clarify these trends.
All cases of osteoarticular tuberculosis responded adequately to short-course chemotherapy, and therapy duration did not need to be extended in any patient. At the two year follow-up, there was no recrudescence of the infection in any patient. Thus, it can be concluded that short-course chemotherapy as advised by the WHO is adequate treatment for all forms of extraspinal osteoarticular tuberculosis and that 99mTc ciprofloxacin scan is a novel and reliable marker to monitor drug response and define the end point of disease activity in these cases. A similar study with more patients may also be conducted to identify slow responders using 99mTc ciprofloxacin scan, which could then be considered for prolonged chemotherapy for nine months or beyond.
Acknowledgments
Conflict of Interest None
References
- 1.Dye C, Garnett GP, Sleeman K, Williams BG. Prospects for worldwide tuberculosis control under the WHO DOTS strategy. Lancet. 1998;352:1886–1891. doi: 10.1016/S0140-6736(98)03199-7. [DOI] [PubMed] [Google Scholar]
- 2.Nakajima H. Tuberculosis a global emergency. World Health. 1993;46(4):3. [Google Scholar]
- 3.Tuli SM (2004) Tuberculosis of the Skeletal System, (third ed); 3-4
- 4.Masood S. Diagnosis of tuberculosis of the bone and soft tissue by fine-needle aspiration biopsy. Diagn Cytopathol. 1992;8:451–455. doi: 10.1002/dc.2840080505. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization: treatment of tuberculosis. Guidelines for national programs Ed 2, Geneva, World Health Organization 1997
- 6.Glassroth J. Clinical considerations in designing trials of vaccines for tuberculosis. Clin Infect Dis. 2000;30(Suppl 3):S229–S232. doi: 10.1086/313866. [DOI] [PubMed] [Google Scholar]
- 7.Mitchison DA, Ellard GA, Fox W. Studies on the treatment of tuberculosis undertaken by the British Medical Research Council Tuberculosis Unit between 1946-86. Int J Tuberc Lung Dis. 1999;10:231–279. [PubMed] [Google Scholar]
- 8.Balasubramanian R. Fully intermittent six-month treatment regimen for pulmonary tuberculosis in south India. Ind J Tuberc. 1991;38:51–53. [Google Scholar]
- 9.MRC Working Party on Tuberculosis of the Spine Controlled trial of short-course regimens of chemotherapy in the ambulatory treatment of spinal tuberculosis results at three years of a study in Korea twelfth report of the medical research council working party on tuberculosis of the spine. J Bone Joint Surg Br. 1993;75:240–248. doi: 10.1302/0301-620X.75B2.8444944. [DOI] [PubMed] [Google Scholar]
- 10.MRC Working Party on Tuberculosis of the Spine Five-year assessment of controlled trials of short-course chemotherapy regimens of 6, 9 or 18 months’ duration for spinal tuberculosis in patients ambulatory from the start or undergoing radical surgery Fourteenth report of the Medical Research Council Working Party on Tuberculosis of the Spin. Int Orthop. 1999;23(2):73–81. doi: 10.1007/s002640050311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramachandran S, Clifton IJ, Collyns TA, Watson JP SB. 6-month treatment for bone tuberculosis. Int J Tuberc Lung Dis. 2006;10(9):1063–1065. [PubMed] [Google Scholar]
- 12.Yoon HJ, Song YG, Park WI, Choi JP, Chang KH, Kim JM. Clinical manifestations and diagnosis of extrapulmonary tuberculosis. Yonsei Med J. 2004;45(3):453–461. doi: 10.3349/ymj.2004.45.3.453. [DOI] [PubMed] [Google Scholar]
- 13.Martini M, Cuahes M. Bone and joint tuberculosis: a review of 652 cases. Orthopedics. 1988;11:861–866. doi: 10.3928/0147-7447-19880601-04. [DOI] [PubMed] [Google Scholar]
- 14.Maekura R, Nakagawa M, Nakamura Y, Hiraga T, Yamamura Y, Ito M, Ueda E, Yano S, He H, Oka S, et al. Clinical evaluation of rapid serodiagnosis of pulmonary tuberculosis by ELISA with cord factor (trehalose-6,6'-dimycolate) as antigen purified from Mycobacterium tuberculosis. Am Rev Respir Dis. 1993;148:997–1001. doi: 10.1164/ajrccm/148.4_Pt_1.997. [DOI] [PubMed] [Google Scholar]
- 15.Chiac P, Yen TSB, You JB, Maa JS, Fiss EH, Chang CH. Detection and identification of Mycobacterium tuberculosis by DNA amplification. J Clin Microb. 1990;28:1877–1880. doi: 10.1128/jcm.28.9.1877-1880.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noel AB, Lecossier D, Nassif X, Birgite G, Frebault VL, Hance AJ. Rapid diagnosis of tuberculosis by amplification of mycobacterial DNA in clinical samples. Lancet. 1989;2(8671):1069–1071. doi: 10.1016/S0140-6736(89)91082-9. [DOI] [PubMed] [Google Scholar]
- 17.Pandey V, Chawla K, Acharya K, Rao S, Rao S. The role of polymerase chain reaction in the management of osteoarticular tuberculosis. Int Orthop. 2009;33(3):801–805. doi: 10.1007/s00264-007-0485-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soler R, Rodriguez E, Remuinan C, Santos M. MRI of musculoskeletal extraspinal tuberculosis. J Computer Assisted Tomography. 2001;25(2):177–183. doi: 10.1097/00004728-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Vuyst D, Vanhoenacker F, Gielen J, Bernaerts A, De Schepper AM (2003) Imaging features of musculoskeletal tuberculosis. European Radiology.; 13:1809-1819 [DOI] [PubMed]
- 20.Britton KE, Vinjamuri S, Hall AV, et al. Clinical evaluation of technetium-99 m Infecton for the localization of bacterial infection. Eur J Nucl Med. 1997;24:553–556. doi: 10.1007/BF01267688. [DOI] [PubMed] [Google Scholar]
- 21.Hall AV, Solanki KK, Vinjamuri S, Britton KE, Das SS. Evaluation of the efficacy of 99mTc-Infecton, a novel agent for detecting sites of infection. J Clin Pathol. 1998;51:215–219. doi: 10.1136/jcp.51.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Britton KE, Wareham DW, Das SS, Solanki KK, Amaral H, Bhatnagar A, Katamihardja AHS, Malamitsi J, Moustafa HM, Soroa VE, Sundram FX, Padhy AK. Imaging bacterial infection with 99mTc-ciprofloxacin (Infecton) J Clin Path. 2002;55:817–823. doi: 10.1136/jcp.55.11.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vinjamuri S, Hall AV, Solanki KK, et al. Comparison of 99mTc Infecton imaging with radiolabeled white-cell imaging in the evaluation of bacterial infection. Lancet. 1996;347:233–235. doi: 10.1016/S0140-6736(96)90407-9. [DOI] [PubMed] [Google Scholar]
- 24.Easmon CSF, Crane JP, Browers A. Effect of ciprofloxacin on intracellular organism in-vitro and in-vivo studies. J of Antimicrob Chemotherapy. 1986;18(suppl):46–48. doi: 10.1093/jac/18.supplement_d.43. [DOI] [PubMed] [Google Scholar]
- 25.Sharma R, Tewari KN, Bhatnagar A, Mondal A, Mishra AK, Singh AK, Chopra MK, Rawat H, Kashyap R, Tripathi RP. Tc-99 m ciprofloxacin scans for detection of tubercular bone infection. Clin Nucl Med. 2007;32(5):367–370. doi: 10.1097/01.rlu.0000259322.31974.e8. [DOI] [PubMed] [Google Scholar]