Abstract
Purpose
The aim of this study was to report normal values of the tibial tuberosity–trochlear groove distance (TTTG) in males and females and assess the reliability of MRI in measuring TTTG.
Methods
Patients presenting with a suspected meniscus injury without any patellofemoral or ligamentous instability, and arthroscopically normal cruciate ligaments and patellofemoral joints were included in the study. K-PACS© was used for MRI analysis and was performed by three observers blinded to each others’ measurements.
Results
One hundred patients (57 males, 43 females) were recruited from 2006–2010. The mean TTTG in males was 9.91 mm (95% CI 8.9–10.8 mm) and in females 10.04 mm (95% CI 8.9–11.1). The coefficient of variation was <10% for both intra and inter-observer analysis.
Conclusions
The normal TTTG distance is 10 ± 1 mm with MRI being a reliable method of measurement. Literature supports a high degree of variability in reporting TTTG. This study establishes normal TTTG values, which will help in the assessment and treatment of patellofemoral disorders.
Introduction
Tibial tuberosity–trochlear groove distance (TTTG) is important in the assessment and treatment of patellofemoral disorders [1–3]. Dejour et al. [1] found that the TTTG in their control group was 12.7 ± 3.4 mm with a value of >20 mm being pathological. Alemparte et al. [4] studied healthy volunteers and found that normal values for TTTG were 13.6 ± 8.8 mm, indicating a large variation. Wittstein et al. [3], using MRI, found that the TTTG in their control group was 9.4 ± 0.6 mm. These studies suggest that literature supports a high degree of variability in reporting normal values for TTTG and some methods of measurement are complicated with significant intra and inter-observer measurement errors [5, 6].
New software packages have given us a way of standardising the measurement of TTTG. The aim of this study was to assess the reliability of using MRI in evaluating TTTG and report normal TTTG values for males and females.
Methods
Patients
Patients recruited in this study presented with a suspected meniscus injury (knee problem pain, mechanical symptoms). On clinical examination, they demonstrated no patellofemoral instability, no malalignment or ligamentous laxity. All patients had an MRI scan and a knee arthroscopy for their presenting problem. The knee arthroscopy in all the recruited patients demonstrated a normal patellofemoral joint and excluded a cruciate injury. Those with an arthroscopically abnormal patellofemoral joint or a ligamentous injury were excluded from the study. One hundred patients were recruited from 2006–2010 (57 males, 43 females; mean age 44 years).
Imaging
MRI images were obtained using a 1.5-Tesla MR scanner with the following parameters: TR 4000, TE 70, and slice thickness 4 mm. Images were performed with the knee in full extension and the quadriceps relaxed. The scans were analysed on a K-PACS© workstation (K-PACS ©), which is freely downloadable software with user-friendly measurement tools.
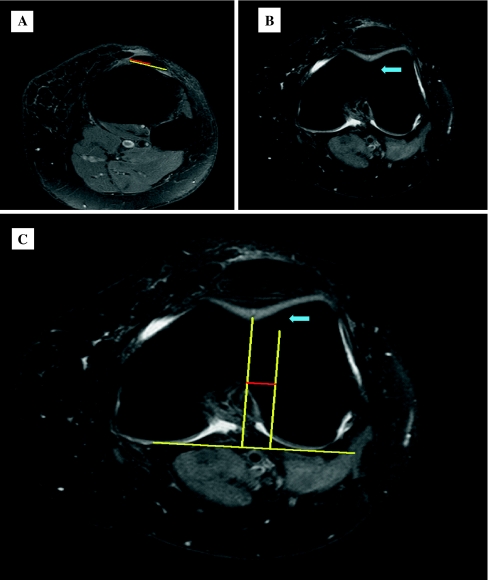
Fat suppressed proton density turbo-spin echo axial sequences were used to determine the TTTG. The technique we used is very similar to the one described by Wittstein et al. [7] (Fig. 1). The midpoint of the distal insertion of the patellar tendon at the tibial tuberosity was obtained using measurement tools (Fig. 1a). The cursor was then placed at this point and images were scrolled proximally to the first image that depicted a complete cartilaginous trochlear grove. The position of the cursor was marked on this new image (Fig. 1b). A reference line was drawn along the posterior femoral condyles and a second line was drawn from the deepest point of the trochlear groove perpendicular to this reference line. A line perpendicular to the reference line was also drawn from the point marked by the cursor. The distance between these two perpendicular lines is the TTTG (Fig 1c; line in red is the TTTG).
Fig. 1.
a The mid-point of the insertion of the patellar tendon is identified. The cursor is placed at this point and the images are scrolled proximally to the first image which depicts a complete continuous cartilaginous trochlear grove. b The position of the cursor is marked on this new image (blue arrow). A reference line is drawn across the posterior femoral condyles (c) and a second line was drawn from the deepest point of the trochlear groove perpendicular to this reference line. A line perpendicular to the reference line was also drawn from the point marked by the cursor. The distance between these two perpendicular lines is the tibial tuberosity–trochlear groove distance (TTTG) (depicted by the red line)
All the scans were double-read on two different occasions by each of the three observers. The observers were blinded to their first read and the results of the other observers.
Statistics
Mean values of TTTG of males and females were calculated with 95% confidence intervals; an independent t-test was used to detect any significant difference between the two values.
Intra and inter-observer reliability of the TTTG measurements was assessed by calculating the variation attributable to each source and these are represented using the coefficient of variation expressed as a percentage, whereby a coefficient of variation <10% represents very good reliability [8].
Scatter plots representing measurements of each pair of observers were created to depict the inter-observer reliability. All analyses were undertaken using SPSS v17.
Results
One hundred patients were recruited in the study from 2006–2010 (57 males, 43 females; mean age 44 years). Clinically, patients had no patellofemoral or cruciate instability and no varus, valgus or rotational malalignment. All patients had arthroscopically normal patellofemoral joint and cruciate ligaments. Imaging and arthroscopy confirmed no evidence of trochlear dysplasia, patella alta or a substantial patellar tilt.
The mean TTTG for males was 9.91 mm (95% CI 8.9–10.8 mm). The mean TTTG for females was 10.04 mm (95% CI 8.9–11.1). There was no significant difference between the two mean values (p = 0.849).
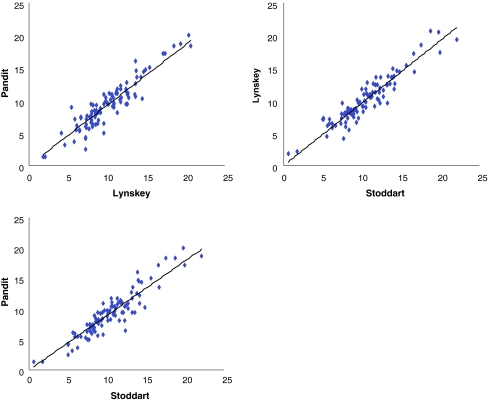
The intra-observer coefficient of variation (CV%) was 9.04% and the inter-observer CV% was 9.35%, representing very good reliability in measurements. Figure 2 demonstrates good inter-observer reliability on scatter plots.
Fig. 2.
Graphs representing good inter-observer reliability between the three observes
Discussion
Goutallier et al. [9] in 1978 first described TTTG using a plain X-ray on an axial image with the knee flexed 30°. A recent study has shown that conventional radiography was associated with large measurement errors when used in the assessment of TTTG [10]. The clinical measurement of TTTG is also unreliable [11], and it is generally agreed that CT or MRI scans most reliably assess TTTG.
Dejour et al. described the use of CT [1, 12] to increase the precision of measurement of TTTG. The technique superimposed two slices, one through the middle of the tibial tuberosity and the other through the bottom of the trochlear grove. A systematic review and meta-analysis showed good intra and inter-observer reliability for CT measurements of TTTG [13]. Some studies however have shown that CT measurements are complicated by poor inter-observer reliability [5, 6], mainly related to errors in obtaining the deepest point of the trochlear groove in patients with trochlear dysplasia. Additionally, CT only assesses bony structures and is associated with a high dose of radiation.
Schoettle et al. [14] demonstrated a high correlation between CT scan and MRI measurements of TTTG with no significant difference between the two. In their study, MRI scans had very good inter-observer and inter-period reliability. In our study, we also saw a very good level of intra and inter-observer agreement using MRI, indicating that MRI is a reliable way of assessing TTTG.
MRI scans have several advantages over CT for assessment and treatment of patellofemoral disorders. MRI offers better visualisation of the articular cartilage and soft tissue structures and has been shown to accurately distinguish the surface geometry of the articular cartilage from the subchondral osseous anatomy of the patellofemoral joint [15]. MRI is therefore helpful in planning surgical procedures aimed at reducing compressive stresses in the patellofemoral joint by visualising defective cartilaginous surfaces, which may need to be offloaded [16]. In patients with severe trochlear dysplasia requiring trochleoplasty, assessment of the cartilage is pivotal as pre-operative cartilaginous degeneration has been associated with inferior results. MRI is therefore helpful in patient selection and pre-operative planning for trochleoplasty [17–19]. The MRI also minimises exposure to radiation and new software has made it very user-friendly in measuring TTTG.
Defining the centre of the patellar tendon on an MRI as opposed to the most anterior part of the tibial tuberosity on a CT is a more anatomical measurement of TTTG and better represents the direction of forces on the patellar tendon [16, 20]. We therefore used this reference point for the centre of the patellar tendon insertion as done by Wittstein et al. and Shoettle et al. [7, 14]. Like Schoettle et al. [14], we also used the deepest cartilaginous point of the trochlear grove on the first image that depicted a complete cartilaginous trochlea as a reference on the trochlear grove. Such a point of reference would prove useful in a knee with trochlear dysplasia, where CT referencing is difficult when the trochlea is flat.
There has been a high degree of variability in normal values of TTTG. Dejour et al. [1] found that the TTTG was 12.7 ± 3.4 mm in their control group, and a value of greater than 20 mm was pathological. Alemparte et al. [4] found a great variation in normal values with TTTG being 13.6 ± 8.8 mm. Wittstein et al. [3] found that the TTTG in their control group was 9.4 ± 0.6 mm, and those with anterior knee pain had significantly greater lateral tibial tubercle deviation of 12.6 ± 1.1 mm.
We present a series of patients with clinically and arthroscopically normal patellofemoral joints in reporting our normal values for TTTG. Our results demonstrate no significant differences between males and females. We found that the normal TTTG is 10 ± 1 mm. These values would be useful in the assessment and treatment of patients with patellofemoral disorders.
Conclusion
This study shows that MRI is a reliable method in the assessment of TTTG. The normal TTTG value for both males and females is 10 ± 1 mm.
Acknowledgments
Conflict of Interest Authors declare that they have no conflict of interest.
References
- 1.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 2.Nagamine R, Miura H, Inoue Y, Tanaka K, Urabe K, Okamoto Y, Nishizawa M, Iwamoto Y. Malposition of the tibial tubercle during flexion in knees with patellofemoral arthritis. Skeletal Radiol. 1997;26(10):597–601. doi: 10.1007/s002560050292. [DOI] [PubMed] [Google Scholar]
- 3.Wittstein JR, Bartlett EC, Easterbrook J, Byrd JC. Magnetic resonance imaging evaluation of patellofemoral malalignment. Arthroscopy. 2006;22(6):643–649. doi: 10.1016/j.arthro.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Alemparte J, Ekdahl M, Burnier L, Hernández R, Cardemil A, Cielo R, Danilla S. Patellofemoral evaluation with radiographs and computed tomography scans in 60 knees of asymptomatic subjects. Arthroscopy. 2007;23(2):170–177. doi: 10.1016/j.arthro.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 5.Lustig S, Servien E, Aït Si Selmi T, Neyret P. Factors affecting reliability of TT-TG measurements before and after medialization: A CT-scan study. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(5):429–436. doi: 10.1016/S0035-1040(06)75829-9. [DOI] [PubMed] [Google Scholar]
- 6.Saudan M, Fritschy D. AT-TG (anterior tuberosity-trochlear groove): interobserver variability in CT measurements in subjects with patellar instability. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(3):250–255. [PubMed] [Google Scholar]
- 7.Wittstein JR, O’Brien SD, Vinson EN, Garrett WE., Jr MRI evaluation of anterior knee pain: predicting response to nonoperative treatment. Skeletal Radiol. 2009;38(9):895–901. doi: 10.1007/s00256-009-0698-6. [DOI] [PubMed] [Google Scholar]
- 8.Hendricks WA, Robey KW (Ann.91936) The sampling distribution of the coefficient of variation. Math Statist 129–132
- 9.Goutallier D, Bernageau J, Lecudonnec B. The measurement of the tibial tuberosity. Patella groove distanced technique and results (author’s transl) Rev Chir Orthop Reparatrice Appar Mot. 1978;64(5):423–428. [PubMed] [Google Scholar]
- 10.Wagenaar FC, Koëter S, Anderson PG, Wymenga AB. Conventional radiography cannot replace CT scanning in detecting tibial tubercle lateralisation. Knee. 2007;14(1):51–54. doi: 10.1016/j.knee.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 11.Shakespeare D, Fick D. Patellar instability-can the TT-TG distance be measured clinically? Knee. 2005;12(3):201–204. doi: 10.1016/j.knee.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Dejour H, Walch G, Neyret P, Adeleine P. La dysplasie de la trochlee femorale. Rev Chir Orthop. 1990;76:45–54. [PubMed] [Google Scholar]
- 13.Smith TO, Davies L, Toms AP, Hing CB, Donell ST (2010) The reliability and validity of radiological assessment for patellar instability. A systematic review and meta-analysis. Skeletal Radiol [Epub ahead of print] [DOI] [PubMed]
- 14.Schöttle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31. doi: 10.1016/j.knee.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Stäubli HU, Dürrenmatt U, Porcellini B, Rauschning W. Anatomy and surface geometry of the patellofemoral joint in the axial plane. J Bone Joint Surg Br. 1999;81(3):452–458. doi: 10.1302/0301-620X.81B3.8758. [DOI] [PubMed] [Google Scholar]
- 16.Maquet P. Advancement of the tibial tuberosity. Clin Orthop Relat Res. 1976;115:225–230. [PubMed] [Google Scholar]
- 17.Utting MR, Mulford JS, Eldridge JD. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg Br. 2008;90(2):180–185. doi: 10.1302/0301-620X.90B2.20017. [DOI] [PubMed] [Google Scholar]
- 18.Schöttle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J. Trochleaplasty for patellar instability due to trochlear dysplasia: A minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop. 2005;76(5):693–698. doi: 10.1080/17453670510041781. [DOI] [PubMed] [Google Scholar]
- 19.DeJour D, Saggin P. The sulcus deepening trochleoplasty—the Lyon’s procedure. Int Orthop. 2010;34:311–316. doi: 10.1007/s00264-009-0933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM. Surgical biomechanics of the patellofemoral joint. Arthroscopy. 2007;23(5):542–553. doi: 10.1016/j.arthro.2007.03.006. [DOI] [PubMed] [Google Scholar]