Abstract
Purpose
The purpose of this study was to compare femoral head placement, rates of reoperation and cephalic implant cut-out of a screw versus a blade for patients over age 60 with low energy trochanteric fractures (AO/OTA 31-A1, A2, and A3) treated either with sliding hip screw or cephalomedullary nail.
Methods
After surgeon selection of either hip screw or nail, hip screw patients were randomised to either a DHS (dynamic hip system screw) or DHS blade (dynamic hip system blade), while nail patients were randomised to either a Gamma3 Trochanteric Nail or a PFNA (proximal femoral nail antirotation). This resulted in a screw group (DHS and Gamma nail), and a blade group (DHS blade and PFNA). Outcome measures included tip-apex distance and zone location of the cephalic implant, as well as reoperation and implant cut-out within the first postoperative year.
Results
A total of 335 patients were randomised, 172 to a screw and 163 to a blade. There was no significant difference concerning mean tip-apex distance, percentage of patients with a tip-apex distance >25 mm, and patients with a centre–centre position of the cephalic implant. There were 137 patients in the screw group and 132 in the blade group available for follow-up. They did not differ regarding rates of reoperation or cut-out (screw group = 2.9%; blade group = 1.5%).
Conclusions
Both a screw and a blade performed equally well in terms of implant placement in the femoral head and outcome.
Introduction
It is well known that accurate positioning of the cephalic screw of a sliding hip screw (SHS) or intramedullary (IM) nail in the femoral head determines the outcome following open reduction internal fixation of trochanteric fractures [1–10]. The most common mode of failure of fixation is cut-out of the lag screw from the femoral head [11], and it has been shown [1, 2, 4, 10, 12] that the tip-apex distance (TAD) is the most valuable factor in determining the likelihood of lag screw cut-out, with a distance >25 mm an indicator of unsatisfactory screw placement and a statistically increased rate of cut-out. In earlier studies lag screw cut-out was reported to range from 8 to 23% [12, 13], but with improved surgical technique and awareness of the importance of the TAD, failures of fixation have been reported to be as low as 1.6–3% [1, 14, 15]. In addition to TAD the position of the cephalic screw in one of nine zones in the head has been described [16]. The ideal position is centre–centre, but a short screw which is centre–centre may still allow for a TAD >25 mm. Thus, it is both the correct length of the screw within the head, as well as the central position of the screw, that will help to prevent cut-out of the cephalic implant. Since the position of the implant in the head is dependent upon the initial guide wire, and since the position of the guide wire is solely under the control of the surgeon, proper placement of any of these implants is the best way to ensure a satisfactory outcome [17, 18].
However, even with a very low rate of fixation failure and lag screw cut-out there has been a shift in the type of cephalic implant that is used with either a SHS or IM nail. A helical blade has been introduced for use with either of the two implants, with the idea that there will be an improved hold in the femoral head and a reduced rate of cut-out. Although there are biomechanical studies [19–22] which give support to this idea, it has not been confirmed by clinical studies. Additionally, there is no information in the literature concerning any difference between a helical blade and screw with respect to placement of the implant within the femoral head. Thus, the primary objective of our study was to compare femoral head placement of a screw versus a blade for all low-energy trochanteric fractures in patients over the age of 60 years. Secondary objectives were to interpret rates of reoperation and cut-out within the first postoperative year as it related to implant position. Our hypothesis was that there would be no difference in placement of the cephalic implant within the femoral head, and no difference in rates of reoperation and cut-out between a cephalic screw and helical blade.
Materials and methods
Patients
We conducted a prospective randomised trial including all patients with extra-capsular hip fractures classified according to AO/OTA [23] as 31-A1 and A2 (pertrochanteric fractures), and 31-A3 (intertrochanteric fractures), in persons over the age of 60 years caused by a low-energy injury. Exclusion criteria included pathological fractures, patients with previous ipsilateral hip or femur surgery, or patients who refused to participate in the study. Since it has clearly been shown [1, 18, 24–27] that there is no difference in functional outcome or rates of cut-out between a SHS or IM nail for fractures classified as 31-A1 and A2, and a nail is the preferred implant biomechanically and clinically for all fractures classified as 31-A3 [18, 28, 29], this was not an intramedullary nail versus SHS study design. The choice between nail and SHS was left to the discretion of the operating surgeon. Once the choice was made between the two, patients selected for a SHS were randomised to a DHS screw (Dynamic Hip System Screw; Synthes, Solothurn, Switzerland) or DHS blade (Dynamic Hip System Blade; Synthes, Solothurn, Switzerland), while those selected for a nail were randomised to either a Gamma3 Trochanteric Nail (Stryker Osteosynthesis, Geneva, Switzerland) or a PFNA (Proximal Femoral Nail Antirotation; Synthes, Solothurn, Switzerland). Thus two groups were created: (1) a screw group consisting of those patients who received either a DHS screw or Gamma nail (Fig. 1); and (2) a blade group composed of those patients treated with a DHS blade or PFNA (Fig. 2). Randomisation to one of these two groups was performed by means of computer-generated random numbers placed in sealed opaque envelopes which were opened at the time the patient was included in the study to allow for appropriate preoperative planning. This study was performed at a university teaching hospital and the operations were performed by a large number of surgeons with varying levels of experience. Approval for this study was obtained from our Hospital Ethics Committee.
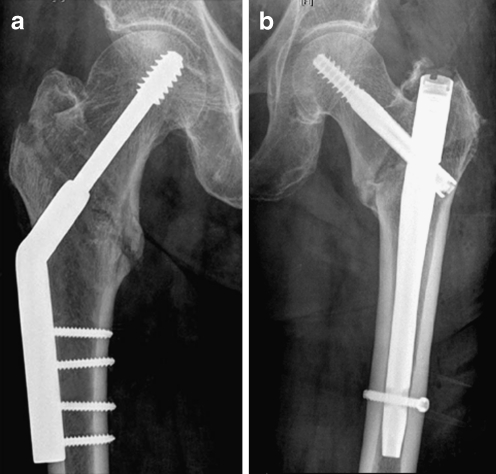
Fig. 1.
Implants for the screw group. a Dynamic hip system (DHS) screw. b Gamma nail
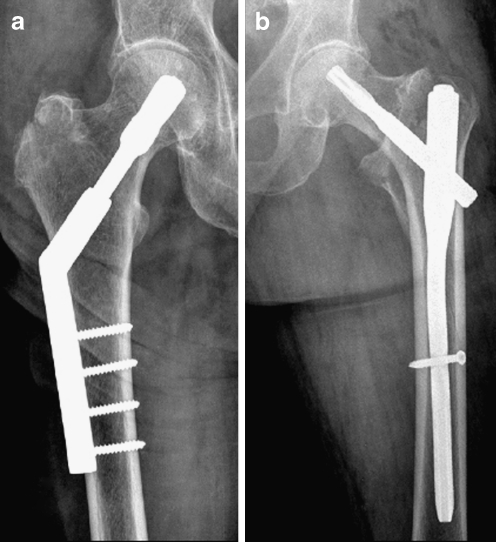
Fig. 2.
Implants for the blade group. a Dynamic hip system (DHS) blade. b Proximal femoral nail antirotation (PFNA)
Outcomes
The primary outcome was the position of the cephalic implant in the femoral head. Secondary outcomes were reoperation rates within the first year and correlation of implant position with cut-out of the screw or helical blade. Radiographic examination was performed on all patients prior to hospital discharge. Anterior-posterior and lateral radiographs were evaluated for TAD and the zone position of the cephalic implant within the femoral head. The measurement of TAD and the location of the implant in the femoral head zone were determined directly from digitised images (PACS; picture archiving and communications systems) by one surgeon not involved in any of the operations using specific measuring tools. We did not use the intraoperative fluoroscopic images, but anteroposterior and lateral radiographs performed at an average of three days after operation. For the TAD we noted the distance from the tip of the screw or blade to the apex of the femoral head on both views. Since the actual width of the stem portion of the lag screw or blade is easily known from the manufacturer, we were able to design a simple program that then calculated the magnification error and gave us the true TAD. A similar method of achieving the TAD from digitised images has been previously described [30].
All patients were managed in the same fashion postoperatively, regardless of chosen implant. They were mobilised out of bed and started on a physical therapy program of weight-bearing as tolerated within the first few days. Based upon the nature of the health care delivery system in our city, virtually all patients initially operated upon at our institution who underwent a reoperation for their hip fracture for any reason would be treated again at our institution. It is well-recognised [1, 31] that elderly patients represent a difficult patient population to return for routine follow-up. Since our only outcome measures were the immediate postoperative position of the screw or blade and reoperation and cut-out rates within the first year, we did not see the value of routine clinical assessment and additional follow-up radiographs. Based upon the concept of the “Functional Recovery Score” established by Zuckerman et al. [31, 32], a trained medical secretary contacted each patient, family member, or other health care-giver to ascertain any change in the patient’s ability to ambulate or degree of pain that might signal a failure of implant fixation. If there was any evidence of such an untoward event the patient was requested to return for evaluation and follow-up radiographs.
Statistical analysis
To compare differences in cephalic implant position (outcome 1) between the two groups we calculated relative risks (RR) and their 95% confidence intervals (CI) for categorical variables and mean differences and their 95% CIs for continuous variables. To compare reoperation rates (outcome 2) we calculated RRs and corresponding 95% CIs.
Sample size calculation was performed to determine the sample size necessary to detect a difference in mean tip-apex distance between the screw and the helical blade group based on previously published data. Assuming a mean tip-apex distance of 24 mm and a standard deviation of 5 mm, and with the objective of being able to detect a 1.5-mm difference in tip-apex distance (power of 0.80 and an alpha error of less than 0.05) we calculated that 175 patients in each arm would be needed.
Results
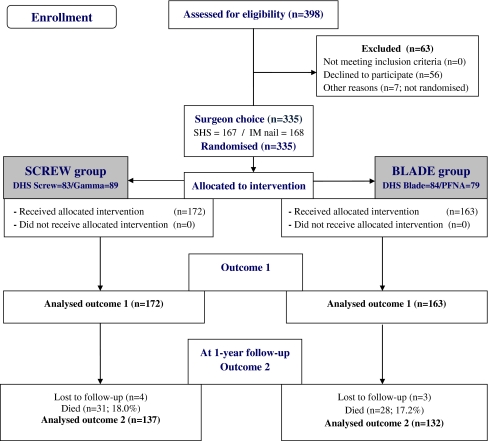
Between October 2006 and July 2009 (33 months) 398 patients were enrolled in the study (Fig. 3). After elimination of those who declined to participate or were inadvertently not randomised, surgeons first chose between a SHS and an IM nail. This resulted in 167 patients being selected for a SHS and 168 for a nail. Randomisation was then performed resulting in 172 randomised to the screw group (DHS screw = 83; Gamma = 89) and 163 to the blade group (DHS blade = 84; PFNA = 79). There were no differences between patients in the two groups as far as baseline characteristics were concerned (Table 1). As noted in Table 2 there was no significant difference on the immediate postoperative radiographs between the two groups concerning mean TAD, the percentage of those with a TAD >25 mm, and those with a centre–centre position of the cephalic implant. Overall, 82–86% of the cephalic implants had a TAD <25 mm, and the ideal zone position of “centre–centre” was achieved in almost 80% of patients. There was no difference in TAD between each of the four implants.
Fig. 3.
CONSORT 2010 flow diagram
Table 1.
Baseline characteristics
| Characteristics | Screw, n = 172 | Blade, n = 163 |
|---|---|---|
| Female (%) | 133 (77.3) | 124 (76.1) |
| Male (%) | 39 (22.7) | 39 (23.9) |
| Age (mean ± SD) | 85.9 ± 9.3 | 86.8 ± 8.7 |
| ASA | ||
| 2 | 51 (29.7) | 50 (30.7%) |
| 3 | 117 (68.0%) | 107 (65.6%) |
| 4 | 4 (2.3%) | 6 (3.7%) |
| AO/OTA classification | ||
| A1 (%) | 59 (34.3) | 61 (37.4) |
| A2 (%) | 96 (55.8) | 88 (54.0) |
| A3 (%) | 17 (9.9) | 14 (8.6) |
Table 2.
Radiographic analysis
| Measurements | Screw, n = 172 | Blade, n = 163 | Relative risk or mean difference* (95% CI) |
|---|---|---|---|
| Tip-apex distance (mm) (mean ± SD) | 22.1 ± 6.1 | 22.0 ± 5.5 | 0.1 (−1.2; 1.3)* |
| DHS Screw | 22.5 ± 5.6 | ||
| Gamma | 21.7 ± 6.6 | ||
| DHS Blade | 22.3 ± 5.3 | ||
| PFNA | 21.8 ± 5.8 | ||
| Tip-apex distance >25 mm (%) | 31 (18.0) | 23 (14.1) | 1.3 (0.8; 2.1) |
| Centre–centre position (%) | 133 (77.3) | 127 (77.9) | 1.0 (0.9; 1.1) |
At the one-year follow-up, there were 137 patients available in the screw group and 132 patients in the blade group. Table 3 shows those patients who required a revision within the first year. The reoperation rate did not differ between the two groups (screw group = 5.1%, blade group = 4.5%). There were four (2.9%) cut-outs in the screw group and two (1.5%) in the blade group (RR 1.9; 95% CI 0.4–10.3); the difference was not statistically significant. In the screw group, cut-outs occurred in one A1.1, one A3.3, and two A2.2 fractures. In the blade group there was one cut-out in an A2.3 fracture and one in an A3.2 fracture. All patients with cut-out had a TAD >25 mm; the mean TAD in the cut-out group was 29.4 mm (±2.0) compared to 21.9 mm (±5.8 mm) in those patients without cut-out (mean difference 7.5 mm; 95% CI 5.4–9.5). This was statistically significant. In two patients with a DHS blade there was complete sliding of the helical blade in the barrel, thus creating a fixed-angle device, and with further impaction of the fracture the blade perforated the femoral head. This was not considered cut-out or medial migration of the blade.
Table 3.
Reoperations
| Reoperations | Screw, n = 137 | Blade, n = 132 | Relative risk (95% CI) |
|---|---|---|---|
| Total reoperations | 7 (5.1%) | 6 (4.5%) | 1.1 (0.4; 3.3) |
| Cut-out | 4 (2.9%) | 2 (1.5%) | 1.9 (0.4; 10.3) |
| DHS screw | 2 | ||
| Gamma | 2 | ||
| DHS blade | 1 | ||
| PFNA | 1 | ||
| Nonunion | 2 | 1 | |
| Implant perforation of heada | 0 | 2 | |
| Superficial wound infection | 1 | 1 |
a Full slide of helical blade in barrel of plate with resultant perforation of the femoral head (not cut-out; not medial migration of blade)
Telephone contact with all patients, family members, or other care-givers resulted in 14 patients (screw group = 8; blade group = 6) seen in consultation due to increased pain and/or decreased ability to ambulate. None of the patients had radiographs that demonstrated failure of fixation or cut-out.
Discussion
For decades, whether one favoured a SHS or IM nail for stabilisation of fractures of the hip, the cephalic portion of the implant was a screw. More recent implant design has replaced the cephalic screw with a blade, and while there are biomechanical studies [19–22] that show advantages of the blade as compared to screw, this has yet to be demonstrated clinically. The objectives of our study were to determine the degree of accuracy in placement of either device into the femoral head, and additionally report on rates of reoperation and cut-out for the two implants.
We found no substantial difference in position of the cephalic implant between the two groups in terms of TAD and zone location within the femoral head. And we found no significant difference in the rates of cut-out and reoperation for any reason between the two groups as a factor of lag screw or blade position. While the number of patients with a TAD <25 mm might be considered satisfactory, it is not as good as the most recent reports in the literature [1]. Additionally, we achieved the ideal zone position of “centre–centre” in only 80% of patients. We acknowledge that both these radiographic results could be improved. The vast majority of our patients were operated upon by less senior staff, and although we encouraged the concept of “dead centre and very deep,” it was not always achieved. However, our overall mean TAD of 22 mm, and our overall cut-out rate of 2.2%, is consistent with many other recent reports in the literature [1, 4, 10, 15, 33, 34].
To the best of our knowledge this is the first randomised study in the literature that compares cephalic screw versus cephalic helical blade position in the femoral head as a predictor for cut-out in the treatment of low-energy trochanteric fractures. There are only three reports in the literature [35–37] that have specifically focussed on the difference between these two cephalic implants. One study [36] compared treatment outcomes in patients who received one of two IM nails, one with two screws as the cephalic implant (PFN; Proximal Femoral Nail, Synthes, Solothurn) and the other with a PFNA. There were 40 patients in total who were enrolled (17 screw group; 23 helical blade group), but there was no mention of the number who died within their follow-up period of 1.5 years. There was no report of TAD, zone position of the cephalic implants, or the number of cut-out failures, if any. The study noted some improved social function and mobility scores in the helical blade group, but the numbers appear too small to draw any meaningful conclusions. The second study [37] reported on 107 patients randomised to PFNA or Gamma nail, 91 of whom were available at final follow-up. There was no calculation of TAD. The authors reported a very low mortality rate with only 5/107 (4.6%) patients having died at a mean follow-up of 17.5 months. There were 23 intraoperative complications, six of which included fractures of the femoral shaft, with no difference between the two implants. There were no cut-outs in either group, but they noted a statistically significant shorter operative time and intraoperative blood loss with the PFNA. No explanation is given for these differences. The third study [35] compared four different IM nails, three with a blade and one with two screws for fixation into the femoral head. No randomisation was performed. The three devices with a blade included a Gleitnagel-GN® (Smith&Nephew), a Trochanteric Fixation Nail-TFN® (Synthes), and a PFNA. The screw device, a PFN, was evaluated retrospectively. There were 375 patients enrolled and the focus of the study was specifically cut-out of the cephalic device with the four implants. The PFN had on average a 1.5 times worse TAD than the three blade devices. The cut-out rate for the PFN was 14%, the GN 7%, the PFNA 5.7%, and the TFN 2.5%. These cut-out rates are higher than recently published studies [1, 4, 10, 15, 33, 34], and specifically as regards the PFN substantially higher than even earlier reports [27].
A recent study [4] retrospectively reviewed all hip fracture patients treated with IM nails over a seven-year period. The objective was to determine which factors, specifically TAD, correlated with a successful clinical outcome. While they included patients treated with two different nails, one with a cephalic screw and the other with a blade, a comparison between these two implants was not a specific objective of the study. There were 192 patients initially collected, of whom only 82 met the inclusion criteria, and only 46 fractures were classified as intertrochanteric fractures (the remaining were subtrochanteric). Minimum follow-up was three months. Overall mean TAD for the two nails was 20 mm ± 9 mm, but there was no calculation made specifically between the two different nails. The overall cut-out rate was 8.5% with no statistically significant difference between the two nails. As with our study and many others, no patient with a TAD <25 mm experienced cut-out.
Our study has several strengths. First, to the best of our knowledge it is the first randomised study in the literature that specifically evaluates cephalic implant position with a nail or SHS comparing a screw with a helical blade. Second, there are a sufficient number of patients to make a meaningful comparison with regards to implant position. And third, it is the largest series to date that looks at reoperations within the first postoperative year, and specifically implant cut-out, between patients receiving either a screw or blade. However, given the low incidence of cut-out a substantially larger sample size would have been needed to detect a clinically relevant difference between the two groups with adequate statistical power. As far as other limitations are concerned, we did not actually see the majority of patients at the one-year follow-up and hence did not have actual radiographs to assess healing and possible cephalic implant cut-out. While we endeavoured to make contact with each patient or care-giver it is possible that we missed identifying patients with minimum symptomatology who might have had radiographic evidence of implant cut-out.
In conclusion, our clinical study found that both a screw and a blade performed equally well with a SHS or IM nail for stabilisation of trochanteric fractures in the elderly. It remains that the most important factor in achieving a good result and avoiding cephalic implant cut-out in hip fracture surgery is careful technique respecting accurate tip-apex distance.
Acknowledgments
Funding No funding was received for this work.
Footnotes
This investigation was performed at the Division of Orthopaedics and Trauma Surgery, University Hospitals of Geneva, Geneva, Switzerland. Approval for this study was obtained from our Hospital Ethics Committee.
References
- 1.Barton TM, Gleeson R, Topliss C, Greenwood R, Harries WJ, Chesser TJ. A comparison of the long gamma nail with the sliding hip screw for the treatment of AO/OTA 31-A2 fractures of the proximal part of the femur: a prospective randomized trial. J Bone Joint Surg Am. 2010;92:792–798. doi: 10.2106/JBJS.I.00508. [DOI] [PubMed] [Google Scholar]
- 2.Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997;79:969–971. doi: 10.1302/0301-620X.79B6.7949. [DOI] [PubMed] [Google Scholar]
- 3.Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990;72:26–31. doi: 10.1302/0301-620X.72B1.2298790. [DOI] [PubMed] [Google Scholar]
- 4.Geller JA, Saifi C, Morrison TA, Macaulay W. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int Orthop. 2010;34:719–722. doi: 10.1007/s00264-009-0837-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gundle R, Gargan MF, Simpson AH. How to minimize failure of fixation of unstable intertrochanteric fractures. Injury. 1995;26:611–614. doi: 10.1016/0020-1383(95)00125-S. [DOI] [PubMed] [Google Scholar]
- 6.Hsueh KK, Fang CK, Chen CM, Su YP, Wu HF, Chiu FY. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int Orthop. 2010;34:1273–1276. doi: 10.1007/s00264-009-0866-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lobo-Escolar A, Joven E, Iglesias D, Herrera A. Predictive factors for cutting-out in femoral intramedullary nailing. Injury. 2010;41:1312–1316. doi: 10.1016/j.injury.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Kyle RF. Fractures of the proximal part of the femur. J Bone Joint Surg Am. 1994;76:924–950. [Google Scholar]
- 9.Parker MJ. Cutting-out of the dynamic hip screw related to its position. J Bone Joint Surg Br. 1992;74:625. doi: 10.1302/0301-620X.74B4.1624529. [DOI] [PubMed] [Google Scholar]
- 10.Walton M, Barnett A, Jackson M. Tip-apex distance as a predictor of failure following cephalo-medullary fixation for unstable fractures of the proximal femur. Eur J Trauma Emerg S. 2008;34:273–276. doi: 10.1007/s00068-008-7075-3. [DOI] [PubMed] [Google Scholar]
- 11.Pervez H, Parker MJ, Vowler S. Prediction of fixation failure after sliding hip screw fixation. Injury. 2004;35:994–998. doi: 10.1016/j.injury.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 12.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Bannister GC, Gibson AG, Ackroyd CE, Newman JH. The fixation and prognosis of trochanteric fractures. A randomized prospective controlled trial. Clin Orthop Relat Res. 1990;254:242–246. [PubMed] [Google Scholar]
- 14.Chirodian N, Arch B, Parker MJ. Sliding hip screw fixation of trochanteric hip fractures: outcome of 1024 procedures. Injury. 2005;36:793–800. doi: 10.1016/j.injury.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Lenich A, Mayr E, Ruter A, Mockl C, Fuchtmeier B. First results with the trochanter fixation nail (TFN): a report on 120 cases. Arch Orthop Trauma Surg. 2006;126:706–712. doi: 10.1007/s00402-006-0117-6. [DOI] [PubMed] [Google Scholar]
- 16.Cleveland M, Bosworth DM, Thompson FR, Wilson HJ, Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41:1399–1408. [PubMed] [Google Scholar]
- 17.Sahni V, Sureen S, Shetty V (2001) Who is responsible for failure of a dynamic hip screw by cutout, the patient or the surgeon? In: Proceedings of the 68th annual meeting of the American Academy of Orthopaedic Surgeons, vol 2, p 385
- 18.Stern R. Are there advances in the treatment of extracapsular hip fractures in the elderly? Injury. 2007;38(Suppl 3):S77–S87. doi: 10.1016/j.injury.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 19.Al-Munajjed AA, Hammer J, Mayr E, Nerlich M, Lenich A. Biomechanical characterisation of osteosyntheses for proximal femur fractures: helical blade versus screw. Stud Health Technol Inform. 2008;133:1–10. [PubMed] [Google Scholar]
- 20.Sommers MB, Roth C, Hall H, Kam BC, Ehmke LW, Krieg JC, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004;18:361–368. doi: 10.1097/00005131-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006;37:984–989. doi: 10.1016/j.injury.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 22.Windolf M, Braunstein V, Dutoit C, Schwieger K. Is a helical shaped implant a superior alternative to the dynamic hip screw for unstable femoral neck fractures? A biomechanical investigation. Clin Biomech (Bristol, Avon) 2009;24:59–64. doi: 10.1016/j.clinbiomech.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 24.Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008;90:700–707. doi: 10.2106/JBJS.G.00517. [DOI] [PubMed] [Google Scholar]
- 25.Forte ML, Virnig BA, Eberly LE, Swiontkowski MF, Feldman R, Bhandari M, et al. Provider factors associated with intramedullary nail use for intertrochanteric hip fractures. J Bone Joint Surg Am. 2010;92:1105–1114. doi: 10.2106/JBJS.I.00295. [DOI] [PubMed] [Google Scholar]
- 26.Parker MJ, Handoll HH (2008) Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev 3:CD000093 [DOI] [PubMed]
- 27.Saudan M, Lubbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002;16:386–393. doi: 10.1097/00005131-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Kuzyk PR, Lobo J, Whelan D, Zdero R, McKee MD, Schemitsch EH. Biomechanical evaluation of extramedullary versus intramedullary fixation for reverse obliquity intertrochanteric fractures. J Orthop Trauma. 2009;23:31–38. doi: 10.1097/BOT.0b013e318190ea7d. [DOI] [PubMed] [Google Scholar]
- 29.Park SY, Yang KH, Yoo JH, Yoon HK, Park HW. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J Trauma. 2008;65:852–857. doi: 10.1097/TA.0b013e31802b9559. [DOI] [PubMed] [Google Scholar]
- 30.Johnson LJ, Cope MR, Shahrokhi S, Tamblyn P. Measuring tip-apex distance using a picture archiving and communication system (PACS) Injury. 2008;39:786–790. doi: 10.1016/j.injury.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 31.Zuckerman JD, Koval KJ, Aharonoff GB, Hiebert R, Skovron ML. A functional recovery score for elderly hip fracture patients: I. Development. J Orthop Trauma. 2000;14:20–25. doi: 10.1097/00005131-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Zuckerman JD, Koval KJ, Aharonoff GB, Skovron ML. A functional recovery score for elderly hip fracture patients: II. Validity and reliability. J Orthop Trauma. 2000;14:26–30. doi: 10.1097/00005131-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Lindsey RW, Ahmed S, Overturf S, Tan A, Gugala Z. Accuracy of lag screw placement for the dynamic hip screw and the cephalomedullary nail. Orthopedics. 2009;32:488. doi: 10.3928/01477447-20090527-15. [DOI] [PubMed] [Google Scholar]
- 34.Simmermacher RK, Ljungqvist J, Bail H, Hockertz T, Vochteloo AJ, Ochs U, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury. 2008;39:932–939. doi: 10.1016/j.injury.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Lenich A, Vester H, Nerlich M, Mayr E, Stockle U, Fuchtmeier B. Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip-blade vs screw. Injury. 2010;41:1292–1296. doi: 10.1016/j.injury.2010.07.499. [DOI] [PubMed] [Google Scholar]
- 36.Park JH, Lee YS, Park JW, Wang JH, Kim JG. A comparative study of screw and helical proximal femoral nails for the treatment of intertrochanteric fractures. Orthopedics. 2010;33:81–85. doi: 10.3928/01477447-20100104-11. [DOI] [PubMed] [Google Scholar]
- 37.Yaozeng X, Dechun G, Huilin Y, Guangming Z, Xianbin W. Comparative study of trochanteric fracture treated with the proximal femoral nail anti-rotation and the third generation of gamma nail. Injury. 2010;41:1234–1238. doi: 10.1016/j.injury.2010.03.005. [DOI] [PubMed] [Google Scholar]