Abstract
Purpose
The aim of this prospective study was to evaluate the patellar height in 90° knee flexion.
Methods
A total of 85 patients with 95 knee joints were included in the study. Patellar height was measured according to the Blackburne-Peel, Labelle-Laurin, Insall-Salvati, Linclau, and Caton-Deschamps methods in the whole group and in subgroups based on age, gender, and side.
Results
The BP-ratio showed a patella norma in 45 cases, and in 25 cases a patella alta and infera, respectively. The Labelle-Laurin method determined a patella norma in eight knees, in 35 a patella alta and in 52 a patella infera. The IS-ratio revealed a patella norma in 52 patients, a patella alta in six and in 37 a patella infera. The Linclau method demonstrated in 52 cases a patella norma, in 17 a patella alta and in 26 a patella infera. The CD-ratio showed the highest values of a patella norma among all tested methods in 67 knees, whereas a patella alta was evident in 13 and a patella infera in 15 cases. In the subgroups, discrepancies depended on the subgroup and method used.
Conclusions
Our results demonstrate a method-dependent discrepancy in the measurement of patellar height. A future study should evaluate this effect in a direct comparison between 30° and 90° knee flexion.
Introduction
The patella position is one of the most important factors for normal knee joint function. The patella height, shift and tilt describe the patella position in relation to the tibiofemoral joint, and their values act as guidelines in several orthopaedic reconstructive procedures.
The patellar height is usually determined from lateral X-rays with the knee joint being flexed at approximately 20–30°. This range of knee flexion ensures the right tension of the patellar tendon for the correct height calculation. Several methods have been described for the estimation of the patellar height [1–7]. All these methods have pros and cons and possess different values of inter- and intraobserver variability, reliability and reproducibility [8–12]. Despite numerous proposals, there is still no method which precisely describes the true patellar height in relation to the tibiofemoral joint, with high values of reliability and reproducibility and low values of inter- and intraobserver variability.
Several orthopaedic knee operations include a postoperative treatment protocol with limitation of the joint flexion to 90° during the first six weeks after surgery. When estimating the patellar height, 90° flexion is an easier optical limit compared to the 20–30°, and might help the surgeon to determine the patellar height more quickly intraoperatively and correct it, if necessary. However, no literature has been published on this topic. Hence, the aim of our prospective study was to determine the patellar height in knees at 90° flexion according to five different commonly used methods.
Patients and methods
Between June 1, 2007 and December 1, 2007, all ambulatory patients in our department with symptomatic knees who needed a radiological examination of their joints were considered to be candidates for our study. Due to the possible influence of orthopaedic disorders or previous operations on the patellar height, the following exclusion criteria were determined: known osteoarthritis, knee flexion < 90°, prior rupture of the quadriceps tendon or known insufficiency, known neurological disorders, prior patellar fracture, prior patellar tendon rupture, prior patellar dislocation(s) and prior knee operations with a known decrease on the patellar height, involving anterior cruciate reconstruction (ACL) surgery, high tibial osteotomy, and uni- or total joint arthroplasty.
A total of 85 patients (42 male, 43 female, mean age of 57 [range, 15–76] years) with 95 knee joints (49 left, 46 right) fulfilled the criteria. In all cases, the lateral X-ray of the particular knee joint was done in 90° flexion instead of 20–30°. Because there was no additional radiation exposure to the patients, no specific approval from our institutional review board was necessary for the study. The correct angle was determined by a goniometer in all cases. For a standardised lateral joint view, the criteria as set by Berg et al. [9] were respected.
After completion of the study, all X-rays were evaluated by the same person (S.R.) once according to the following methods (Figs. 1, 2, 3, 4, 5): Insall-Salvati (IS) [5], Blackburne-Peel (BP) [1], Caton-Deschamps (CD) [2, 3], Labelle-Laurin (LL) [6] , and Linclau (LI) [7]. The patellar height was classified as alta, norma or infera according to the values shown in Table 1. These values are not always identical to those originally published, because over the years it has become evident that adjustments in the range of values had to be made. In addition, a problem for the Labelle-Laurin ratio was the definition of the infera values because it was not described in the original publication. Therefore, a patella infera was reported if the distance between the proximal patellar pole and the tangent of the ventral cortical line exceeded 5 mm.
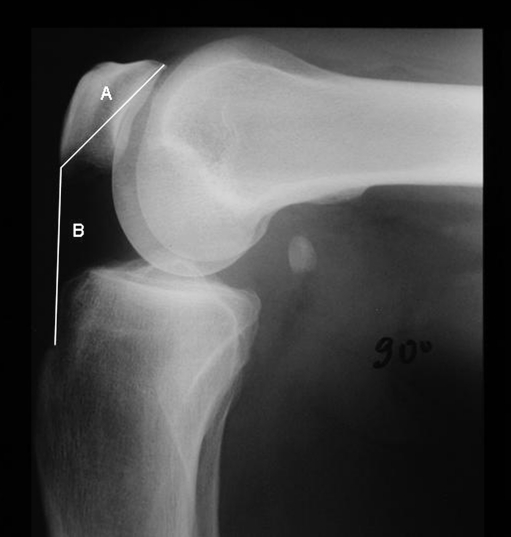
Fig. 1.
The Insall-Salvati ratio determines the diagonal length of the patella (a) in relation to the length of the patellar tendon (b)
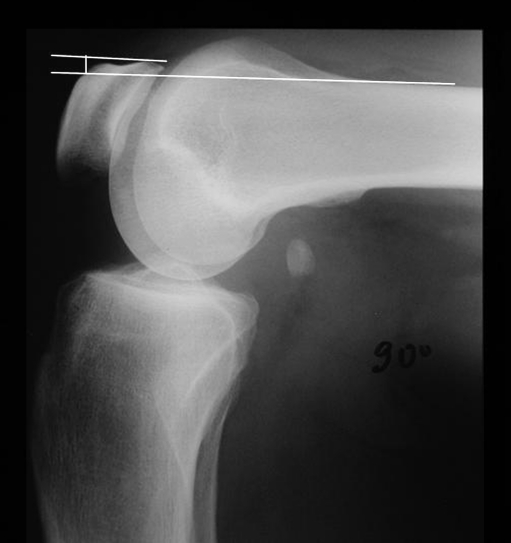
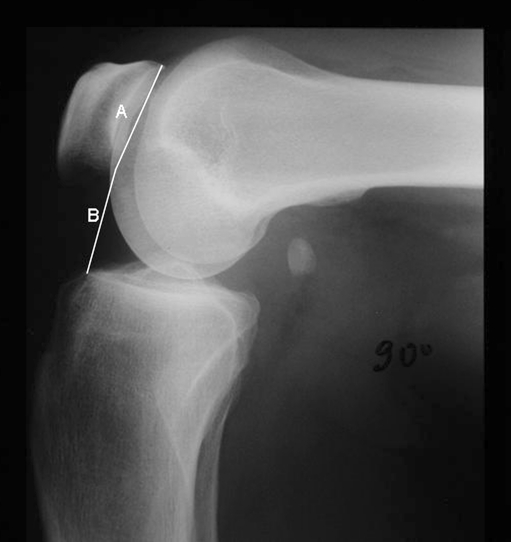
Fig. 2.
The Blackburne-Peel method measures the ratio of the articular surface length of the patella (a) to the height of the lower pole of the articular surface above a tibial plateau line (b)
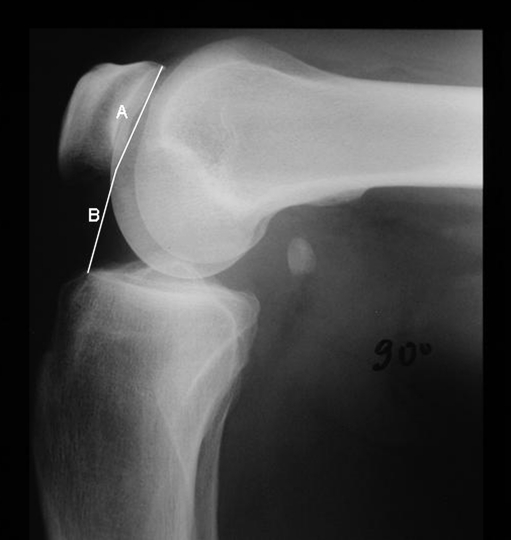
Fig. 3.
The Caton-Deschamps ratio measures the distance between the distal point of the patellar articular surface and the anterosuperior border of the tibia (b) divided by the length of the articular surface of the patella (a)
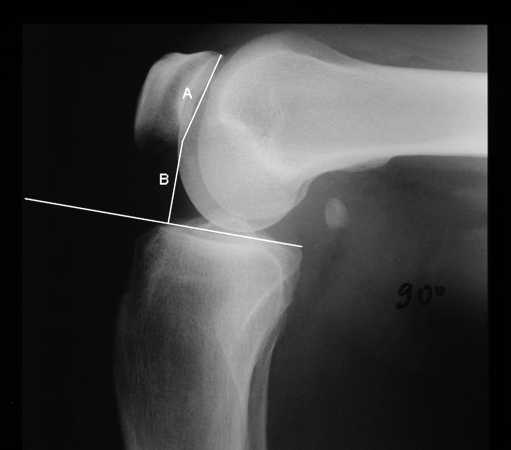
Fig. 4.
The Labelle-Laurin method defines a patella as alta if its proximal pole lies above the tangent of the ventral cortical line of the femur on a lateral X-ray in 90° of knee flexion
Fig. 5.
The Linclau method measures the same distances as the Caton-Deschamps ratio, however, the ratio is not B/A, but A/B
Table 1.
Patellar height ratios and their values for classification of a patella norma, alta and infera
| Method | Alta | Norma | Infera |
|---|---|---|---|
| Blackburne-Peel | > 1.0 | 0.8-1.0 | < 0.8 |
| Insall-Salvati | > 1.0 | 0.75-0.99 | < 0.75 |
| Caton-Deschamps | > 1.2 | 0.8-1.2 | < 0.8 |
| Linclau | > 1.2 | 0.9-1.2 | < 0.9 |
| Labelle-Laurin | See footnote | See footnote | See footnote |
For Labelle-Laurin, a patella alta is defined when the proximal patella pole is beyond the tangent of the ventral cortical line; a patella norma is defined when the tangent of the ventral cortical line contacts exactly the proximal patellar pole; a patella infera is defined if the distance between the proximal patellar pole and the tangent of the ventral cortical line exceeds 5 mm
Data were collected for the whole group and for subgroups with regard to side, gender, and age (≤55 y vs. >55 y). Due to the solely descriptive study design, no statistical analysis was performed regarding the validity or reliability of the values.
Results
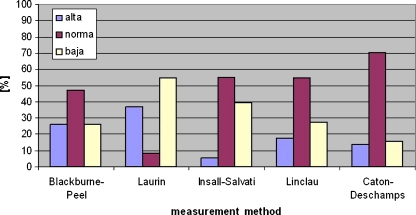
The BP ratio showed a patella norma in 45 cases (mean 0.9 [range, 0.8–0.97]), and in 25 cases a patella alta (mean 1.10 [range, 1.0–1.94]) and infera (mean 0.66 [range, 0.37–0.79]), respectively. The Labelle-Laurin method determined a patella norma in eight knees, a patella alta in 35 [+5 mm to + 13 mm] and a patella infera in 52 [−6 mm to −28 mm]. The IS ratio revealed a patella norma in 52 patients (mean 0.83 [range 0.75–0.99]), a patella alta in six (mean 1.02 [range, 1.0–1.17]) and a patella infera in 37 (mean 0.66 [range, 0.48–0.74]). The Linclau method demonstrated a patella norma in 52 cases (mean 1.00 [range, 0.9–1.19]), a patella alta in 17 (mean 1.36 [range, 1.21–2.3]) and a patella infera in 26 (mean 0.83 [range, 0.5–0.89]). The CD ratio showed the highest values of a patella norma among all tested methods in 67 knees (mean 1.00 [range, 0.81–1.19]), whereas a patella alta was evident in 13 (mean 1.30 [range, 1.21–2.00]) and a patella infera in 15 cases (mean 0.65 [range 0.43–0.78]) (Fig. 6).
Fig. 6.
Comparison of five methods for patellar height measurement in 90°-flexed knees
The evaluation of the determined values with regard to gender, age, and side showed great discrepancies depending on the method used. For example, the BP ratio showed similar values of a patella norma in both age subgroups (23 vs. 22), whereas the younger patients had an alta in 16 cases and an infera in nine cases. On the contrary, the elderly patients showed a patella alta in nine cases and a patella infera in nine cases. Similar discrepancies regarding the age subgroups were seen also in the values determined by the CD ratio, where the percentage of the patellae alta in the younger group was more than three times higher than in the elderly group. In the side subgroup, great discrepancies were seen regarding the patella norma, as measured by the BP ratio (58.7% for the right knees vs. 36.73% for the left knees). All values regarding the whole group as well as the subgroups are demonstrated in Table 2.
Table 2.
Patellar height values determined in 90°-flexed knees according to five different methods
| Method | Description | Absolute values | Relative values | |||||
|---|---|---|---|---|---|---|---|---|
| BP | Group | Alta | Infera | Norma | Total | % Alta | % Infera | % Norma |
| Total | 25 | 25 | 45 | 95 | 26.32 | 26.32 | 47.37 | |
| Male | 14 | 14 | 21 | 49 | 28.57 | 28.57 | 42.86 | |
| Female | 11 | 11 | 24 | 46 | 23.91 | 23.91 | 52.17 | |
| <55 y | 16 | 9 | 23 | 48 | 33.33 | 18.75 | 47.92 | |
| >55 y | 9 | 16 | 22 | 47 | 19.15 | 34.04 | 46.81 | |
| Right | 10 | 9 | 27 | 46 | 21.74 | 19.57 | 58.70 | |
| Left | 15 | 16 | 18 | 49 | 30.61 | 32.65 | 36.73 | |
| LL | Total | 35 | 52 | 8 | 95 | 36.84 | 54.74 | 8.42 |
| Male | 16 | 28 | 5 | 49 | 32.65 | 57.14 | 10.20 | |
| Female | 19 | 24 | 3 | 46 | 41.30 | 52.18 | 6.52 | |
| <55 y | 16 | 29 | 3 | 48 | 33.33 | 60.42 | 6.25 | |
| >55 y | 19 | 23 | 5 | 47 | 40.43 | 48.94 | 10.64 | |
| Right | 15 | 29 | 2 | 46 | 32.61 | 63.04 | 4.35 | |
| Left | 20 | 23 | 6 | 49 | 40.82 | 46.94 | 12.24 | |
| IS | Total | 6 | 37 | 52 | 95 | 6.31 | 39.36 | 55.32 |
| Male | 2 | 18 | 29 | 49 | 4.08 | 36.73 | 59.18 | |
| Female | 4 | 19 | 23 | 46 | 8.69 | 42.22 | 51.11 | |
| <55 y | 3 | 15 | 30 | 48 | 6.25 | 31.91 | 63.83 | |
| >55 y | 3 | 22 | 22 | 47 | 6.38 | 46.81 | 46.81 | |
| Right | 3 | 20 | 23 | 46 | 6.52 | 44.44 | 51.11 | |
| Left | 3 | 17 | 29 | 49 | 6.12 | 34.69 | 59.18 | |
| LI | Total | 17 | 26 | 52 | 95 | 17.89 | 27,.7 | 54.74 |
| Male | 7 | 13 | 29 | 49 | 14.29 | 26.53 | 61.22 | |
| Female | 10 | 13 | 23 | 46 | 21.74 | 28.26 | 50.00 | |
| <55 y | 6 | 19 | 23 | 48 | 12.50 | 39.58 | 47.92 | |
| >55 y | 11 | 7 | 29 | 47 | 23.40 | 14.89 | 61.70 | |
| Right | 7 | 13 | 26 | 46 | 15.22 | 28.26 | 56.52 | |
| Left | 10 | 13 | 26 | 49 | 20.41 | 26.53 | 53.06 | |
| CD | Total | 13 | 15 | 67 | 95 | 13.68 | 15.79 | 70.53 |
| Male | 8 | 7 | 34 | 49 | 16.33 | 14.29 | 69.39 | |
| Female | 5 | 8 | 33 | 46 | 10.87 | 17.39 | 71.74 | |
| <55 y | 10 | 5 | 33 | 48 | 20.83 | 10.42 | 68.75 | |
| >55 y | 3 | 10 | 34 | 47 | 6.38 | 21.28 | 72.34 | |
| Right | 5 | 6 | 35 | 46 | 10.87 | 13.04 | 76.09 | |
| Left | 8 | 9 | 32 | 49 | 16.33 | 18.37 | 65.31 | |
BP Blackburne-Peel, LL Labelle-Laurin, IS Insall-Salvati, LI Linclau, CD Caton-Deschamps
Discussion
Alterations in the patellar height have been described after several operations or at the site of numerous orthopaedic disorders and might be associated with decreased range of motion or symptoms. Generally, patella infera has been described after total [13–16] and unicompartmental knee replacement [17], high tibial osteotomy [11, 18–20], and anterior cruciate ligament reconstruction [21]. Whereas, patella alta has been described in neurological disorders [22], in association with anterior knee pain [23], and femoropatellar instability [24].
The exact aetiology is not completely clear for either entity and may vary depending on the presence of a patella infera or alta. The cause of patella infera has been ascribed to biological adaptation of the extensor mechanism, shrinking of scar tissue, scarring, formation of new bone, immobilisation, patellofemoral fibrosis, intra-articular fibrous bands, ischaemia and trauma to the patellar tendon [2, 17, 25, 26]. In total knee arthroplasty, some authors suggest that the eversion of the patella leads to ischaemia and trauma of the tendon and, hence, to a postoperative patella infera [17]. On the other hand, a patella alta may be idiopathic [27], associated with neurological disorders [22] and be the cause of or a complication after patellar dislocations [28].
Even the smallest alterations of the normal patellar height may be associated with altered joint motion and symptoms. Calculations have shown that 1 mm of shortening of the patellar tendon would be expected to cause loss of flexion of about 1° [17]. In a geometrical knee model, it has been demonstrated that when there is a short patellar tendon, the patella contacts the femur at a smaller angle of flexion than occurs when the tendon is of normal length [29]. Patella infera after TKR may be associated with a limited range of movement [17].
However, not every method is suitable for a universal measurement of the patellar height, regardless of the particular orthopaedic disorder. Some methods may be affected by changes in the patellar (Insall-Salvati [5], modified Insall-Salvati (MIS) [4]) or proximal tibia morphology (Insall-Salvati) [5]. Other ratios, such as the Blackburne-Peel [1], are affected by the position of the joint line, since they require the precise identification of the proximal joint surface of the tibia for their assessment, and, therefore, do not accurately correlate with true patellar height after unicompartmental or total knee arthroplasty. Similarly, this method is also inappropriate for patellar height measurement after high tibial osteotomy, because a change in the angle of inclination of the tibial plateau adversely affects the reproducibility of this measurement. Seil et al. have demonstrated paradoxical cases of patellar height in normal anatomy, where in the same knee the IS ratio showed a patella alta, the LL and MIS methods a patella norma and the BP and CD ratio a patella infera [12]. Orthopaedic surgeons should be aware of these facts and decide for themselves the most appropriate method to use.
Furthermore, factors such as the inter- and intraobserver variability, reliability and reproducibility may also play an important role in the assessment of the true patellar height. Berg et al. showed among three observers that the Blackburne-Peel method was relatively reproducible [9]. Seil et al. demonstrated for this ratio the lowest interobserver variability in a study of symptomatic knees [12]. Aparicio et al. found out that the Caton-Deschamps method was more reliable and reproducible than the Blackburne-Peel ratio in children [8]. Scuderi et al. showed differences in the incidence of patella infera after high tibial osteotomy, depending on whether the Insall-Salvati or the Blackburne-Peel ratio was used (89% vs. 73%) [11]. After TKR, Rogers et al. found out that the interobserver difference was reduced using both the Caton-Deschamps and the Blackburne-Peel method compared with the IS and the MIS ratio [10].
Taking the aforementioned literature data into consideration, we decided to conduct a study for measurement of the patellar height in 90° knee flexion which could be easily measured intraoperatively if these methods proved to be applicable. Our first aim was to investigate the value distribution in a symptomatic population because we could not predict if all methods could be used in this flexion position. A further aim was to verify whether the distribution of the height values into norma, alta and infera would be similar to those as reported in other studies where the patellar height was determined in the usual 20–30° knee flexion.
To some extent, our study showed a similar distribution of patellae norma, alta and infera as reported in the literature at the site of different surgical indications [12, 30–32]. In some cases, our results demonstrated great variations in the determined values. Regarding the Labelle-Laurin method, it might be the case that our “false” definitions of a patella norma and infera, respectively, could have led to a false classification. However, great discrepancies with regard to the particular classified height could be observed among the other ratios tested. The CD ratio revealed a patella norma in over 70% of cases, whereas this rate was approximately 47% for the BP and 55% for the IS ratio. Similarly, the fraction of a patella infera varied strongly among the tested methods, from 15% in the CD group to 39% in the IS group.
These data are extremely important in clinical practice. Although we cannot state categorically which method more accurately describes the true patellar height, a tendency is evident that some methods are more prone to determine a patella norma, infera or alta, respectively. For example, in the case of a tibial tuberosity transfer in the treatment of recurrent patellar dislocations, there is a higher possibility for the CD ratio to show a patella norma, whereas the possibility that the IS ratio would demonstrate a patella alta is extremely low. Based on our results, we cannot reliably interpret these findings and more information is required in the comparison of healthy, non-healthy and operated knees.
Moreover, we consider that the differentiation in relation to age, gender, and side is also important in such a descriptive study. It is well known that the female knee has a different anatomy from the male knee [33, 34]. Moreover, differences in the quadriceps muscle strength between right and left sides might also result in different patellar heights. Yiannakopoulos et al. have recently shown that quadriceps contraction has an influence on the patellar height, as measured by four different methods [35]. Furthermore, it seems logical that with increasing age the tension of the extensor mechanism might decrease, thus yielding a higher percentage of patella infera. In our opinion, all these differentiations are essential for the clinical use and have to be taken into consideration.
Despite the prospective design and the strict exclusion criteria, our study has some limitations. The patellar height was classified as norma, alta or infera depending on values which have been determined and defined in a different degree of knee flexion with the exception of the LL method. It is unknown whether these values also account for a 90° flexion, and this might be a systematic mistake of our study; however, some values have to act as guidelines, and unfortunately the literature does not provide any values in 90°-flexed knees. In addition, all radiographs were evaluated only once by a single person, so that no statements can be made regarding inter- and intraobserver variability. Methods where an anatomical landmark cannot always be identified easily (e.g. tuberositas tibiae for the IS ratio), a high inter- and intraobserver variability might be expected. Moreover, we did not have a control group with patellar height values measured in 20–30° knee flexion so that no correlation between this flexion grade and the 90° can be made. Furthermore, this fact also makes a direct comparison with literature data difficult, since our study is the first to evaluated these five methods in 90° knee flexion. Last but not least, our study included only healthy but symptomatic knee joints, which does not always correspond to clinical practice where many patients have osteoarthritic changes or are awaiting operation.
In conclusion, our study is the first to report on the comparison of five different patellar height measurement methods in 90° knee flexion. Our results demonstrate that all aforementioned methods are applicable in this degree of flexion, whereas adjustments of the scale values possibly have to be made for the correct classification of a patella norma, alta and infera. The differences between the results of the different ratios measuring patellar height are dependent on the value of the patella alta or infera as described by each author, and the normal value is different for each method of these different ratios. Future studies should investigate the value distribution for normal knees with each different method, and whether the 90° knee flexion provides more advantages compared with the 30° flexion. Moreover, it should be determined whether these methods can be also used in osteoarthritic or pre-operative knees in 90° joint flexion. Here, it should be remembered that 90° is the upper flexion limit because the more the knee is flexed the more the patella becomes infera.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59-B:241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 2.Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. Patella infera: apropos 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68:317–325. [PubMed] [Google Scholar]
- 3.Caton J. Method of measuring the height of the patella. Acta Orthop Belg. 1989;55:385–386. [PubMed] [Google Scholar]
- 4.Grelsamer RP, Meadows S. The modified Insall-Salvati-ratio for patellar height. Clin Orthop Relat Res. 1992;282:170–176. [PubMed] [Google Scholar]
- 5.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 6.Laurin CA. The investigation of the patellofemoral joint. J Bone Joint Surg Br. 1977;59-B:107. [Google Scholar]
- 7.Linclau L. Measuring patellar height. Acta Orthop Belg. 1984;50:70–74. [PubMed] [Google Scholar]
- 8.Aparicio G, Abril JC, Albinana J, Rodriguez-Salvanes F. Patellar height ratios in children: an interobserver study of three methods. J Pediatr Orthop B. 1999;8:29–32. doi: 10.1097/00009957-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Berg EE, Mason SL, Lucas MJ. Patellar height ratios: a comparison of four measurements methods. Am J Sports Med. 1996;24:218–221. doi: 10.1177/036354659602400218. [DOI] [PubMed] [Google Scholar]
- 10.Rogers BA, Thornton-Bott P, Cannon SR, Briggs TWR. Interobserver variation in the measurement of patellar height after total knee arthroplasty. J Bone Joint Surg Br. 2006;88-B:484–488. doi: 10.1302/0301-620X.88B4.16407. [DOI] [PubMed] [Google Scholar]
- 11.Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989;71-A:245–248. [PubMed] [Google Scholar]
- 12.Seil R, Müller B, Georg T, Kohn D, Rupp S. Reliability and interobserver variability in radiological patellar height ratios. Knee Surg Sports Traumatol Arthrosc. 2000;8:231–236. doi: 10.1007/s001670000121. [DOI] [PubMed] [Google Scholar]
- 13.Aglietti P, Buzzi R, Gaudenzi A. Patello-femoral functional results and complications with the posterior-stabilised total condylar knee prosthesis. J Arthroplasty. 1988;3:17–25. doi: 10.1016/S0883-5403(88)80049-4. [DOI] [PubMed] [Google Scholar]
- 14.Fern ED, Winson IG, Getty CJM. Anterior knee pain in rheumatoid patients after total knee replacement: possible selection criteria for patellar resurfacing. J Bone Joint Surg Br. 1992;74-B:745–748. doi: 10.1302/0301-620X.74B5.1527126. [DOI] [PubMed] [Google Scholar]
- 15.Figgie HE, 3rd, Goldberg VM, Heiple KG, Moller HS, III, Gordon NH. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior-stabilised condylar knee prosthesis. J Bone Joint Surg Am. 1986;68-A:1035–1040. [PubMed] [Google Scholar]
- 16.Koshino T, Ejima M, Okamoto R, Orii T. Gradual lowriding of the patella during postoperative course after total knee arthroplasty in osteoarthritis and rheumatoid arthritis. J Arthroplasty. 1990;5:323–327. doi: 10.1016/S0883-5403(08)80091-5. [DOI] [PubMed] [Google Scholar]
- 17.Weale AE, Murray DW, Newman JH, Ackroyd CE. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br. 1999;81-B:790–795. doi: 10.1302/0301-620X.81B5.9590. [DOI] [PubMed] [Google Scholar]
- 18.Tigani D, Ferrari D, Trentani P, Barbanti-Brodano G, Trentani F. Patellar height after high tibial osteotomy. Int Orthop. 2001;24:331–333. doi: 10.1007/s002640000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gasbeek RD, Nicolaas L, Rijnberg WJ, Loon CJ, Kampen A. Correction accuracy and collateral laxity in open versus closed wedge high tibial osteotomy. A one-year randomised controlled study. Int Orthop. 2010;34:201–207. doi: 10.1007/s00264-009-0861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raaij TM, Waal MJ. Anterior opening wedge osteotomy of the proximal tibia for anterior knee pain in idiopathic hyperextension knees. Int Orthop. 2006;30:248–252. doi: 10.1007/s00264-005-0063-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tria AJ, Jr, Alicea JA, Cody RP. Patella baja in anterior cruciate ligament reconstruction of the knee. Clin Orthop Relat Res. 1994;299:229–234. [PubMed] [Google Scholar]
- 22.Senaran H, Holden C, Dabney KW, Miller F. Anterior knee pain in children with cerebral palsy. J Pediatr Orthop B. 2007;27:12–16. doi: 10.1097/BPO.0b013e31802b715c. [DOI] [PubMed] [Google Scholar]
- 23.Luyckx T, Didden K, Vandenneucker H, Labey L, Innocenti B, Bellemans J. Is there a biomechanical explanation for anterior knee pain in patients with patella alta? Influence of patellar height on patellofemoral contact force, contact area and contact pressure. J Bone Joint Surg Br. 2009;91-B:344–350. doi: 10.1302/0301-620X.91B3.21592. [DOI] [PubMed] [Google Scholar]
- 24.Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34:305–309. doi: 10.1007/s00264-009-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kayler DE, Lyttle D. Surgical interruption of the patellar blood supply by total knee arthroplasty. Clin Orthop Relat Res. 1988;229:221–227. [PubMed] [Google Scholar]
- 26.Noyes FR, Wostys E, Marshall MT. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop Relat Res. 1991;265:241–252. [PubMed] [Google Scholar]
- 27.Caton J, Mirroneau A, Walch G, Levigne C, Michel CR. Idiopathic high patella in adolescents. Apropos 61 surgical cases. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:253–260. [PubMed] [Google Scholar]
- 28.Thaunat M, Erasmus PJ. Recurrent patellar dislocation after medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:40–43. doi: 10.1007/s00167-007-0418-5. [DOI] [PubMed] [Google Scholar]
- 29.Eijden TM, Kouwenhoven E, Weijs WA. Mechanics of the patellar articulation: effects of patellar ligament length studied with a mathematical model. Acta Orthop Scand. 1987;58:560–566. doi: 10.3109/17453678709146400. [DOI] [PubMed] [Google Scholar]
- 30.Brouwer RW, Bierma-Zeinstra SM, Koeveringe AJ, Verhaar JA. Patellar height and the inclination of the tibial plateau after height tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br. 2005;87-B:1227–1232. doi: 10.1302/0301-620X.87B9.15972. [DOI] [PubMed] [Google Scholar]
- 31.Kesmezacar H, Erginer R, Ogut T, Seyahi A, Babacan M, Tenekecioglu Y. Evaluation of patellar height and measurement methods after valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2005;13:539–544. doi: 10.1007/s00167-004-0572-y. [DOI] [PubMed] [Google Scholar]
- 32.Lin CF, Wu JJ, Chen TS, Huang TF. Comparison of the Insall-Salvati ratio of the patella in patients with and without an ACL tear. Knee Surg Sports Traumatol Arthrosc. 2005;13:8–11. doi: 10.1007/s00167-004-0515-7. [DOI] [PubMed] [Google Scholar]
- 33.Conley S, Rosenberg A, Crowninshield R. The female knee: anatomic variations. J Am Acad Orthop Surg. 2007;15:S31–36. doi: 10.5435/00124635-200700001-00009. [DOI] [PubMed] [Google Scholar]
- 34.Hovinga KR, Lerner AL. Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J Orthop Res. 2009;27:1191–1196. doi: 10.1002/jor.20858. [DOI] [PubMed] [Google Scholar]
- 35.Yiannakopoulos CK, Mataragas E, Antonogiannakis E. The effect of quadriceps contraction during weight-bearing on four patellar height indices. J Bone Joint Surg Br. 2008;90-B:870–873. doi: 10.1302/0301-620X.90B7.20111. [DOI] [PubMed] [Google Scholar]