Abstract
Purpose
The purpose of this study was to evaluate the functional impairments during gait after Legg-Calvé-Perthes Disease (LCPD) and to correlate these data with the clinical and radiographic outcome.
Methods
In 13 individuals with LCPD in recovery or final stage (mean age 9.5 ± 3.5 years) with unilateral hip involvement the clinical result was graded according to Tönnis and the radiographic outcome according to Heyman and Herndon; the functional impairment during gait was compared to a group of healthy children (n = 30, mean age 8.1 ± 1.2 years). All children underwent computerised three-dimensional gait analysis.
Results
The standard physical examination resulted in 69.2% normal range of movement according to Tönnis, but overall analysis of gait revealed that only 30.7% had a normal gait pattern. All children with an excellent or good radiographic (n = 6) outcome walked normally or showed minor deviations.
Conclusions
The results of the standard clinical examination do not reflect the function of the hip joint during gait. Additional information is revealed from gait analysis and should be part of outcome studies in LCPD.
Introduction
Current follow-up and outcome evaluations of Legg-Calvé-Perthes disease (LCPD) are based on subjective measures of function, clinical parameters and radiological changes [1–7]. The mechanisms influencing the final configuration of the femoral head are poorly understood. Until now the functional effects on gait have almost been neglected. Besides our analysis of the movement patterns in the frontal plane [8] there is only one study evaluating the abductor function during gait after LCPD [9].
The purpose of this study was to evaluate and describe the functional impairments during gait after LCPD and to correlate these data with the clinical and radiographic outcome.
Patients and methods
Thirteen children with LCPD were included in the study. Inclusion criteria were radiographically confirmed LCPD in the final stage according to the Waldenström classification [10]. In addition only patients with unilateral involvement and with non-operative treatment were included. Patients were excluded if they had a history of previous lower extremity surgery or other disorders altering gait.
For comparison a group of 30 healthy children six to ten years of age was recruited as volunteers to define physiological gait and to serve as a control group. Exclusion criteria were previous surgery on the lower extremities and disorders leading to gait abnormalities (Table 1).
Table 1.
Study population characteristics
| Control | LCPD | |
|---|---|---|
| n | 30 | 13 |
| Male | 14 | 9 |
| Female | 16 | 4 |
| Age, years (SD) | 8.1 (1.2) | 9.5 (3.5) |
All children underwent a standard physical examination. The pain level was measured by the visual analogue scale defined from 0 to 10 (0 = no pain, 10 = maximum pain). This is a reliable and valid measure of pain in paediatric populations [11]. The limitations in range of movement were classified according to Tönnis [12] (Table 2).
Table 2.
Classification of limitations in range of movement (ROM) of the hip joint according to Tönnis [12]
| Criteria | |
|---|---|
| Grade 0 | No limitation in ROM, flexion > 120°, ab-/adduction and internal/external rotation > 40°, extension at least 0° |
| Grade 1 | Flexion 110°, extension 0°, ab-/adduction and internal/external rotation 20–30° |
| Grade 2 | Flexion 100°, lack of extension 10–15°, internal rotation 0–20°, abduction 0–10° |
| Grade 3 | Flexion < 100°, external rotation contracture 10–20°, add- or abduction contracture 10–20° |
| Grade 4 | Contracture more pronounced than in grade 3 |
In case of doubt the amount of the flexion-extension movement takes precedence over the other movement directions
For analysing the functional impairments during gait all children underwent computerised three-dimensional gait analysis. Gait analysis was performed using a VICON 512 gait system (Oxford Metrics Ltd., Oxford, UK) with eight 50-Hz cameras and two AMTI force plates (AMTI OR6, Advanced Mechanical Technology Inc., Watertown, MA, USA). All subjects walked barefoot at a self-selected speed along a ten metre walkway. Fifteen small (2.5 cm diameter) retroreflective markers were placed on the lower extremity according to a standardised protocol [13]. For each subject the data of five trials with a clear foot-force plate contact were collected and averaged. The data of the control group were collected side-independently (left–right).
In addition all LCPD patients had a standard anteroposterior (AP) radiograph of the pelvis in standing position and a Lauenstein lateral view of the involved hip. The radiographic outcome was classified according to Heyman and Herndon [14]. This index summarises the results of the epiphyseal ratio, the head to neck ratio, the acetabular ratio and the acetabulum to head ratio. The total index is rated as follows: excellent 90–100%, good 80–89%, moderate 70–79% and poor < 70%.
The parents of the children included in this study were informed about the study and gave their written informed consent. The study was approved by the local Ethics Committee.
Data analysis
For the quantitative description of gait spatio-temporal parameters, kinematic and kinetic data were analysed. The kinematic evaluation consisted of the analysis of the pelvis and the hip, knee and ankle joints in the sagittal, frontal and transverse planes. The maximum and minimum values and the range of movement during a gait cycle were analysed. The kinetic evaluation consisted of the analysis of the power generation and absorption in the sagittal plane at the level of the hip, the knee and the ankle. Power generation and absorption were analysed as areas under the power curve.
The global hip function in the sagittal plane was analysed by the hip flexor index (HFISchwartz) according to Schwartz et al. [15]. A modified hip flexor index (HFIDuesseldorf) was also applied by repeating principal component analysis with the data of our normal population. The modified HFI was computed as HFIDuesseldorf = 0.50 * Zsubj MPT + 0.48 * ZsubjPTR + 0.54 * ZsubjHEST – 0.45 * ZsubjH3 [normalised values “maximum pelvic tilt” (MPT), “pelvic tilt range” (PTR), “maximum hip extension in stance” (HEST) and “late stance power burst H3” (H3)]. The results were compared.
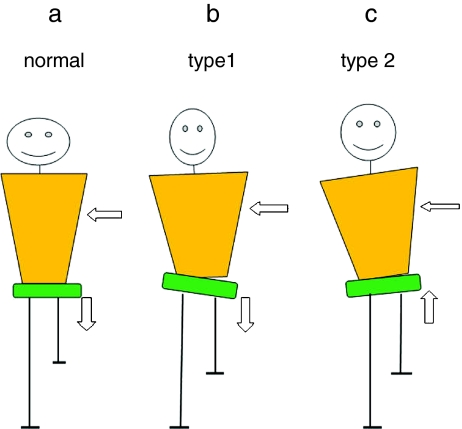
The global hip function in the frontal plane was classified during single stance according to the patterns previously defined quantitatively; the 2 SD range was defined as normal (Fig. 1) [8]:
Normal: slight drop of the pelvis to the swinging limb (−1 to 4°) and slight adduction of the hip (1–9°); the trunk leans toward the stance limb in relation to the pelvis (−5 to 1°) and stays almost horizontal in relation to the global coordinate system (−3 to 1°)
Type 1 (Trendelenburg-like): increased pelvic drop to the swinging limb > 4° and/or maximum pelvic drop > 8°, increased hip adduction > 9° and/or maximum hip adduction > 11° and a trunk lean in relation to the pelvis toward the stance limb > 5°
Type 2 (Duchenne-like): trunk lean toward the affected stance limb > 3° with the pelvis stable or elevated on the swinging limb
Fig. 1.
a–c Movement patterns in the frontal plane during single stance: a demonstrates the physiological movement pattern, b type 1 and c type 2
Statistical analysis was performed by the Wilcoxon test. A two-sided p value of less than or equal to 0.05 was considered to indicate statistical significance.
Results
The early clinical outcome after LCPD was generally positive: the pain level according to the visual analogue scale was 0.7 (SD 1.6, range 0–6). The standard physical examination of the involved hip joint graded according to Tönnis resulted in 69.2% (9/13 patients) normal range of movement (grade 0), in 23.1% (3/13 patients) slight limitations (grade 1) and in 7.7% (1/13 patients) moderate limitations (grade 2).
The gait analysis revealed no statistically significant deviations affecting the temporal spatial parameters (gait velocity, step length, duration of double and single support stance phase) compared to the control group. The kinematic evaluation showed—despite an increased maximum anteversion of the pelvis (17 vs 11° in the control group, p = 0.028)—no significant changes.
The kinetic analysis revealed a significantly reduced power generation at the level of the involved hip joint compared to the control group (11.21 vs 14.87 J/kg, p = 0.019).
The analysis of the global hip function in the sagittal plane showed for both indices—the HFISchwartz and the HFIDuesseldorf—a statistically significant elevation compared to the control group: HFISchwartz 2.45 (SD 1.7) compared to 0.55 (SD 1.36), p = 0.011 and HFIDuesseldorf 2.05 (SD 1.9) compared to 0.0 (SD 1.17), p = 0.01. For 53.8% (7/13) of the LCPD children a HFIDuesseldorf outside the range of 2 SDs could be calculated, indicating an impaired hip flexor function.
The analysis of the gait pattern in the frontal plane showed in 46.2% (6/13) a physiological type pattern. In one patient (7.7%) a type 1 and in three patients (23.1%) a type 2 pattern could be identified. Three patients (23.1%) did not fulfil the criteria of type1 or type 2 (“not classifiable”): two subjects showed a pelvic drop to the swinging limb outside the 2 SD range without any other abnormalities, and one subject had only an increased hip adduction in single stance.
Analysing gait function of the sagittal and frontal planes combined revealed that only four (30.7%) LCPD patients had a normal gait pattern (Table 3).
Table 3.
Gait deviations in sagittal and frontal planes
| n = 13 (100%) | |
|---|---|
| Normal sagittal and frontal | 4 (30.7%) |
| Only sagittal pathological | 2 (15.4%) |
| Only frontal pathological | 2 (15.4%) |
| Sagittal and frontal pathological | 5 (38.5%) |
“Normal” is defined in the sagittal plane as HFIDuesseldorf < 2 SD and in the frontal plane a gait pattern during single stance within the 2 SD range
The correlation of the standard clinical examination measurements classified according to Tönnis and the results of the gait analysis revealed that in children with a physiological range of movement (n = 9) only three (33.3%) also had a normal gait pattern in the sagittal and frontal planes; a further three patients showed a pronounced impairment of gait with pathology in the sagittal as well as in the frontal plane (Table 4).
Table 4.
Correlation of standard clinical examination and gait analysis
| n = 13 | Clinical examination | Gait analysis | |
|---|---|---|---|
| Range of movement | Sagittal plane | Frontal plane | |
| Tönnis | HFIDuesseldorf | ||
| M.W. | Grade 0 | Normal | Normal |
| S.B. | Grade 0 | Normal | Normal |
| S.A. | Grade 0 | Normal | Normal |
| K.W. | Grade 0 | Normal | Type 2 |
| L.P. | Grade 0 | Normal | Not classifiable |
| S.E. | Grade 0 | 3.8 | Normal |
| S.K. | Grade 0 | 5.1 | Type 2 |
| F.S. | Grade 0 | 2.5 | Not classifiable |
| F.M. | Grade 0 | 2.7 | Not classifiable |
| F.W. | Grade 1 | Normal | Normal |
| M.M. | Grade 1 | 2.99 | Normal |
| N.X. | Grade 1 | 4.99 | Type 1 |
| C.O. | Grade 2 | 2.6 | Type 2 |
“Normal” is defined in the sagittal plane as HFIDuesseldorf < 2 SD (HFIDuesseldorf < 2.34) and in the frontal plane a gait pattern during single stance within the 2 SD range
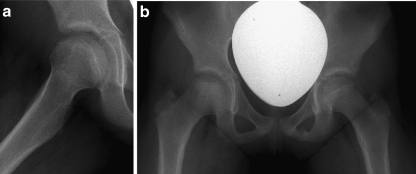
The radiographic evaluation revealed on average an index of 80.8% (SD 11.16%, range 61.85–103.06%). The correlation of the radiographic results and the results of the gait analysis showed that all children (n = 7) with a moderate or poor radiographic outcome had a pathological gait pattern (Fig. 2); four of them had deviations in the sagittal as well as in the frontal plane. Children with an excellent or good radiographic outcome (n = 6) walked normally (n = 4) or showed minor deviations (n = 2) (Table 5)
Fig. 2.
a, b Example of a 9-year-old girl after LCPD with subjectively no complaints: the radiological result was classified as moderate according to Heyman and Herndon mainly due to an impaired epiphyseal ratio. Gait analysis revealed a Duchenne-like gait pattern in the frontal plane and a physiological pattern in the sagittal plane
Table 5.
Correlation of radiographic outcome and gait analysis
| n = 13 | Radiographic outcome | Gait analysis | |
|---|---|---|---|
| Heyman and Herndon | Sagittal plane | Frontal plane | |
| HFIDuesseldorf | |||
| M.W. | Excellent | Normal | Normal |
| S.B. | Excellent | Normal | Normal |
| F.S. | Excellent | 2.5 | Not classifiable |
| F.W. | Good | Normal | Normal |
| S.A. | Good | Normal | Normal |
| L.P. | Good | Normal | Not classifiable |
| S.E. | Moderate | 3.8 | Normal |
| K.W. | Moderate | Normal | Type 2 |
| C.O. | Moderate | 2.6 | Type 2 |
| S.K. | Moderate | 5.1 | Type 2 |
| F.M. | Moderate | 2.7 | Not classifiable |
| N.X. | Moderate | 4.99 | Type 1 |
| M.M. | Poor | 2.9 | Normal |
“Normal” is defined in the sagittal plane as HFIDuesseldorf < 2 SD (HFIDuesseldorf < 2.34) and in the frontal plane a gait pattern during single stance within the 2 SD range
Discussion
The aetiology, pathogenetic mechanisms and treatment principles in LCPD are still controversial [2, 16]. Follow-up and outcome evaluations only analyse subjective results, standard clinical examination parameters including range of motion measurements and radiological changes [1–7]. This is the first study to use objective criteria to evaluate the functional impairments during gait as the outcome measure after LCPD and to compare these results with one of the standard clinical examinations and the radiographic analysis.
Even though physical examination after LCPD revealed limitation in range of movement in only 30.8% (Tönnis grade 1 or 2) gait analysis showed a pathological gait pattern in 69.3% of the patients: the pathological gait pattern consisted of either an impaired hip flexor function or an impaired hip function in the frontal plane or a combination of both. This indicates that in spite of favourable results in the standard clinical examination the hip joint does not function adequately during gait. That means in conclusion that the results of the standard range of movement measurements do not reflect the function of the hip joint during gait and that instrumented gait analysis gives additional information to describe the functionality of the involved joint.
Similar observations were made in patients with cerebral palsy: there were only some fair, but predominantly no correlations between clinical examination parameters (range of movement measurement, spasticity, muscle force, selective motor control) and gait parameters [17].
The comparison of the radiographic and functional results from gait analysis revealed a good correlation: LCPD children with a moderate or poor radiographic outcome had a pathological gait pattern in at least one plane, and LCPD children with an excellent or good radiographic outcome walked normally or showed minor deviations. This functional impairment might be explained by the changed geometry of the hip joint.
Plasschaert et al. studied the hip abductor function in adults treated for Perthes disease by investigating the peak abduction moment of the hip during maximal contraction in isokinetic dynamometry, the net adduction moment around the hip during gait by inverse dynamics and the moment of the hip abductors during gait by quantified and calibrated electromyography [8]. They found that poor clinical outcomes are correlated with inefficient hip abductor function and pain in these patients might be an additional intra-articular cause due to overload of the weak abductors.
Further long-term studies are needed to show whether the gait deviations correlate with the development of osteoarthritis. A further aspect will be whether the gait deviations can be positively influenced by conservative or surgical procedures and whether these therapeutic means will improve the long-term outcome after LCPD.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Herring JA, Kim HT, Browne RH. Legg-Calvé-Perthes disease. Part II: prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86-A:2121–2134. [PubMed] [Google Scholar]
- 2.Sharma S, Shewale S, Sibinski M, Sherlock DA. Legg-Calvé-Perthes disease affecting children less than eight years of age: a paired outcome study. Int Orthop. 2009;33:231–235. doi: 10.1007/s00264-007-0500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vukasinovic Z, Spasovski D, Vucetic C, Cobelijc G, Zivkovic Z, Matanovic D. Triple pelvic osteotomy in the treatment of Legg-Calve-Perthes disease. Int Orthop. 2009;33:1377–1383. doi: 10.1007/s00264-009-0745-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aksoy MC, Cankus MC, Alanay A, Yazici M, Caglar O, Alpaslan AM. Radiological outcome of proximal femoral varus osteotomy for the treatment of lateral pillar group-C Legg-Calvé-Perthes disease. J Pediatr Orthop B. 2005;14:88–91. doi: 10.1097/01202412-200503000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Kitakoji T, Hattori T, Kitoh H, Katho M, Ishiguro N. Which is a better method for Perthes’ disease: femoral varus or Salter osteotomy? Clin Orthop. 2005;430:163–170. doi: 10.1097/01.blo.0000137549.60694.63. [DOI] [PubMed] [Google Scholar]
- 6.Joseph B, Rao N, Mulpuri K, Varghese G, Nair S. How does a femoral varus osteotomy alter the natural evolution of Perthes’ disease. J Pediatr Orthop B. 2005;14:10–15. doi: 10.1097/01202412-200501000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Ishida A, Kuwajima SS, Laredo Filho J, Milani C. Salter innominate osteotomy in the treatment of severe Legg-Calvé-Perthes disease: clinical and radiographic results in 32 patients (37 hips) at skeletal maturity. J Pediatr Orthop. 2004;24:257–264. doi: 10.1097/01241398-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Westhoff B, Petermann A, Hirsch MA, Willers R, Krauspe R. Computerized gait analysis in Legg Calvé Perthes disease—analysis of the frontal plane. Gait Posture. 2006;24:196–202. doi: 10.1016/j.gaitpost.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Plasschaert VF, Horemans HL, Boer LM, Harlaar J, Diepstraten AF, Roebroeck ME. Hip abductor function in adults treated for Perthes disease. J Pediatr Orthop B. 2006;15:183–189. doi: 10.1097/01.bpb.0000186645.76697.7a. [DOI] [PubMed] [Google Scholar]
- 10.Waldenström H. Coxa plana, osteochondritis deformans coxae. Zentralbl Chir. 1920;47:539. [Google Scholar]
- 11.McGrath PA. Evaluating a child’s pain. J Pain Symptom Manage. 1989;4:198–214. doi: 10.1016/0885-3924(89)90044-4. [DOI] [PubMed] [Google Scholar]
- 12.Tönnis D (1984) Die angeborene Hüftdysplasie und Hüftluxation im Kindes- und Erwachsenenalter. Springer, Berlin
- 13.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 14.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–778. [PubMed] [Google Scholar]
- 15.Schwartz M, Novacheck TF, Trost J. A tool for quantifying hip flexor function during gait. Gait Posture. 2000;12:122–127. doi: 10.1016/S0966-6362(00)00064-3. [DOI] [PubMed] [Google Scholar]
- 16.Kamegaya M, Saisu T, Ochiai N, Hisamitsu J, Moriya H. A paired study of Perthes’ disease comparing conservative and surgical treatment. J Bone Joint Surg Br. 2004;86:1176–1181. doi: 10.1302/0301-620X.86B8.14458. [DOI] [PubMed] [Google Scholar]
- 17.Desloovere K, Molenaers G, Fey H, Huenaerts C, Callewaert B, Walle P. Do dynamic and static clinical measurements correlate with gait analysis parameters in children with cerebral palsy? Gait Posture. 2006;24:302–313. doi: 10.1016/j.gaitpost.2005.10.008. [DOI] [PubMed] [Google Scholar]