Abstract
Bleeding is the most important complication of oral anticoagulation (OAC) with vitamin K-antagonists. Whilst bleeding is unavoidably related to OAC, it may have a great impact on the prognosis of treated subjects by leading to discontinuation of treatment, permanent disability or death. The yearly incidence of bleeding during OAC is 2%-5% for major bleeding, 0.5%-1% for fatal bleeding, and 0.2%-0.4% for intracranial bleeding. While OAC interruption and/or antagonism, as well as administration of coagulation factors, represent the necessary measures for the management of bleeding, proper stratification of the individual risk of bleeding prior to start OAC is of paramount importance. Several factors, including advanced age, female gender, poor control and higher intensity of OAC, associated diseases and medications, as well as genetic factors, have been proven to be associated with an increased risk of bleeding. Most of these factors have been included in the development of bleeding prediction scores, which should now be used by clinicians when prescribing and monitoring OAC. Owing to the many limitations of OAC, including a narrow therapeutic window, cumbersome management, and wide inter- and intra-individual variability, novel oral anticoagulants, such as factor Xa inhibitors and direct thrombin inhibitors, have been recently developed. These agents can be given in fixed doses, have little interaction with foods and drugs, and do not require regular monitoring of anticoagulation. While the novel oral anticoagulants show promise for effective thromboprophylaxis in atrial fibrillation and venous thromboembolism, definitive data on their safety and efficacy are awaited.
Keywords: Bleeding, Oral anticoagulation, Vitamin K antagonists, Dabigatran, Apixaban, Rivaroxaban
INTRODUCTION
The purpose of oral anticoagulation (OAC) therapy is to induce a controlled depression of blood coagulability in order to reduce the risk of thromboembolic complications in clinical conditions such as atrial fibrillation, mechanical heart valves, deep vein thrombosis and pulmonary embolism, and cardiogenic stroke. While newer oral anticoagulants, such as direct thrombin inhibitors (i.e., dabigatran) and direct factor Xa inhibitors (i.e., apixaban, rivaroxaban), have been recently evaluated in the clinical setting[1-5], vitamin K antagonists (VKAs), such as warfarin, acenocoumarol, and phenprocoumon, currently represent the standard drugs for OAC therapy.
The anticoagulant effect of VKAs is a consequence of their interference with the cyclic interconversion of vitamin K and its epoxide, by means of the inhibition of the vitamin K epoxide reductase enzyme (VKORC1), which in turn, is essential for the gamma-carboxylation of vitamin K-dependent coagulation factors, including factor II, VII, IX and X[6] (Figure 1). While acenocoumarol and phenprocoumon are preferred in some countries, warfarin is the VKA most commonly used in clinical practice[6]. Warfarin is a racemic mixture of two optically active isomers, the R and S enantiomers[6]. It is rapidly absorbed from the gastrointestinal tract, has high bioavailability, and reaches its maximal blood concentration about 90 min after oral administration[6]. Racemic warfarin has a half-life of 36-42 h, as compared to 8-24 h for acenocoumarol, and 80-270 h for phenprocoumon, circulates bound to plasma proteins, and accumulates in the liver, where the two enantiomers are metabolized by different pathways[6]. The S enantiomer, which is about three times more potent than the R enantiomer, is primarily metabolized by the CYP2C9 enzyme of the cytochrome P450 system, whereas the R enantiomer is metabolized by the CYP1A2 and CYP3A4 enzymes[6].
Figure 1.
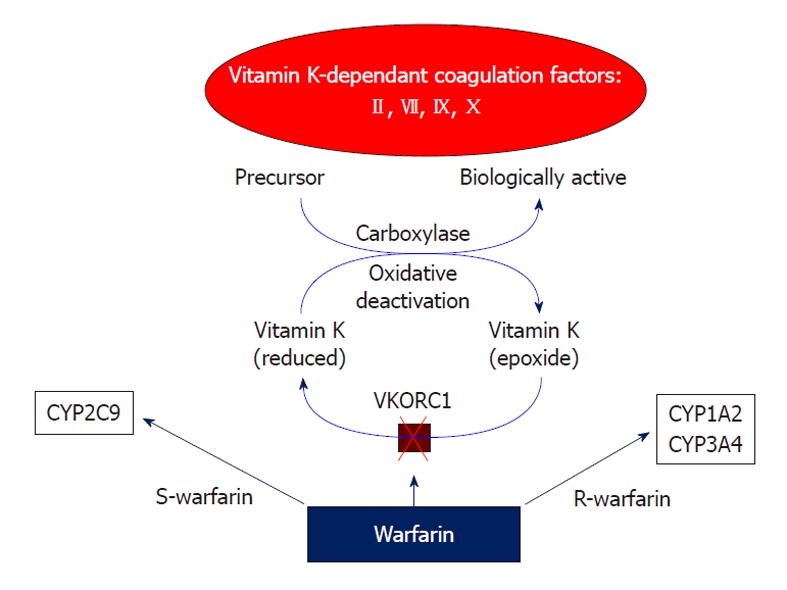
Mechanism of action and metabolism of warfarin. VKORC1: Vitamin K epoxide reductase enzyme.
In order to maximize protection against thromboembolic complications while minimizing the risk of bleeding associated with VKA therapy, the intensity of OAC should be maintained within a narrow therapeutic range (TTR). Apart from non-bileaflet mechanical heart valves and mechanical heart valves in the mitral position, where a higher intensity of OAC therapy is required, an international normalized ratio (INR) of 2.0-3.0 has long been identified as the optimal TTR for most clinical conditions at risk for thromboembolic events[6]. Nonetheless, bleeding represents the major complication of OAC therapy, even when OAC is properly prescribed[7].
INCIDENCE OF BLEEDING
The reported incidence of bleeding during OAC therapy with VKAs is highly variable in published studies. This variability may be accounted for by the differences in the definition and classification of bleeding (Table 1). More importantly however, the differences in the reported hemorrhagic rates are more likely to be attributed to differences in study design and patient population. In randomized clinical trials, where highly selected patients are enrolled, rates of bleeding are expected to be lower than in observational studies, where patients commonly encountered in clinical practice, including those with individual risk factors for bleeding, are included. As an example, in six pivotal trials evaluating the effect of warfarin compared to placebo in patients with atrial fibrillation, only 12.6% out of the 28 787 patients screened were finally included[8]. Whether or not monitoring of OAC therapy is carried out in specialized services, where a better and more stable control of the INR is generally achieved, may also have an impact on the occurrence of bleeding complications[9].
Table 1.
Different definitions of major bleeding in various studies
| Ref. | Clinical setting | Definition |
| Landefeld et al[53] | Various | Fatal, life-threatening, potentially life-threatening, causing severe blood loss, leading to surgical treatment or moderate acute/subacute blood loss not explained by surgery/trauma |
| Palareti et al[32] | Various | Fatal intracranial (documented by imaging); ocular (with blindness); articular; retroperitoneal; requiring surgery/angiographic intervention; associated to Hb decrease ≥ 2 g/dL or need for ≥ 2 blood units transfusion |
| Beyth et al[54] | Various | Overt bleeding leading to ≥ 2 blood units loss in ≤ 7 d, or life-threatening |
| Gage et al[55] | AF | ICD-9CM codes for bleed in any location |
| Shireman et al[56] | AF | Hospitalization for “major acute bleeding” (including gastrointestinal or intracranial hemorrhage) |
AF: Atrial fibrillation; Hb: Hemoglobin.
The expected incidence of bleeding during long-term VKA therapy is about 10%-17% per year for all events, 2%-5% per year for major bleeding, and 0.5%-1% per year for fatal bleeding[10]. The reported occurrence of intracranial hemorrhage (ICH), which represents the mostly feared bleeding complication of VKA therapy because of its high disability and/or fatality rate, is in the range of 0.2%-0.4% per year[7,11].
CLINICAL IMPACT AND MANAGEMENT OF BLEEDING
The occurrence of bleeding during OAC therapy with VKAs has relevant prognostic and management implications. Major bleeding can be life-threatening, such as when occurring at critical sites like the head, the pericardium or the pleura, or when leading to the development of hemorrhagic shock. Also, major bleeding complications are generally associated with VKA discontinuation, which in turn, contributes to adverse outcomes by leaving the patient exposed to an increased risk of thromboembolism. In a recent meta-analysis of clinical trials reporting on OAC therapy with VKAs for venous thromboembolism, a case-fatality rate of major bleeding of 13.4% (95% CI: 9.4%-17.4%) has been reported in all patients, with a rate of ICH of 1.15% per year (95% CI: 2.5%-21.7%)[12]. Regardless of the severity however, hemorrhagic complications of OAC therapy with VKAs may be important for the related inconvenience to the patients. The perceived higher risk of bleeding of VKA therapy limits its more widespread use, therefore excluding many patients from the benefits of such therapy. It has been shown that the occurrence of VKA-associated adverse events has an impact on the prescribing of this treatment, since physicians are less likely to prescribe VKAs after observing a bleeding complication during VKA treatment in their patients[13].
Management of bleeding occurring during OAC therapy with VKAs generally consists of discontinuation and/or antagonism of VKAs, as well as of local measures (i.e. endoscopic treatment and/or surgical hemostasis) and proper transfusion procedures. Discontinuation of VKAs allows for subsequent normalization of INR, which may require several hours owing to the prolonged half-life of VKAs. According to available data, temporary interruption of VKA therapy because of major bleeding or trauma appears not to be associated with an increased risk of subsequent thromboembolic complications[14,15]. In a population of 28 patients with prosthetic heart valves receiving warfarin and hospitalized for major hemorrhage who were retrospectively evaluated, discontinuation of OAC therapy for 1 d to > 3 wk (mean duration 15 ± 4 d) was not associated with thromboembolic complications at 6-mo follow-up[14]. In a retrospective, population-based, cohort study evaluating 8450 patients aged > 65 years on warfarin for various reasons and surviving a major trauma, the incidence of stroke at a mean follow-up of 3.3 years did not differ between patients who discontinued warfarin as compared to those who continued warfarin [hazard ratio (HR), 0.99; 95% CI: 0.82-1.21], while the incidence of major hemorrhages was significantly lower (HR, 0.69; 95% CI: 0.54-0.88) and that of venous thromboembolism was significantly higher (HR, 1.59; 95% CI: 1.07-2.36)[15]. Antagonism of the VKA anticoagulation effect is obtained by directly administering vitamin K[16]. Vitamin K can be given orally or intravenously, with the parenteral route having the advantage of a more rapid onset of action[17]. After intravenous administration of vitamin K, the INR will start to drop within 2 h and will be normalized within 12-16 h[18], whereas after oral administration it will take up to 24 h to normalize the INR[19]. While low (1-2.5 mg) to moderate (2.5-5 mg) doses of vitamin K given orally are indicated for the management of non-emergency bleeding, slow intravenous infusion of 10 mg vitamin K should be given in emergency situations[6]. Higher doses of vitamin K are equally effective but may induce resistance to VKAs for more than 1 wk[20], and are therefore not recommended. In emergency situations, immediate correction of high INR should be pursued also by the administration of vitamin K-dependent coagulation factors. These factors are present in fresh frozen plasma, which however is inconvenient to use owing to the very large amount needed, the prolonged time required for administration, and the associated risk of fluid overload[21]. Therefore, prothrombin complex concentrates, most of which contain all vitamin K-dependent coagulation factors, are more useful and should be administered either according to fixed dose schemes or, preferably, by individualized dosing regimens based on INR value and body weight[22].
RISK FACTORS FOR BLEEDING
Numerous factors, including individual characteristics, intensity, timing and quality of OAC therapy, and use of concomitant medications, have been established as impacting on the risk of bleeding during VKA treatment (Table 2).
Table 2.
Factors associated with an increased risk of bleeding
| Author |
| Age > 65-70 yr |
| Female gender |
| CYP2C9 and/or VKORC1 gene polymorphism |
| Higher intensity of anticoagulation (i.e., INR > 4.5) |
| Labile INR (i.e., TTR < 60%) |
| Early 90 d of anticoagulation |
| History of bleeding |
| Comorbidities (i.e., hypertension, malignancy, liver and/or renal and/or cardiac failure) |
| Comedications (i.e., antiplatelet agents, non-steroidal anti-inflammatory drugs) |
INR: International normalized ratio; TTR: Time within the therapeutic range.
Age
In most studies, older age has consistently shown to increase the risk of bleeding[11]. As compared to younger patients, elderly patients have about a 5-fold higher incidence of major and fatal bleeding (3.2% and 0.64% per year vs 0.6% and 0.12% per year, respectively)[23]. Importantly, the risk of ICH is particularly increased in subjects of advanced age[24]. In patients aged ≥ 85 years an adjusted odds ratio of 2.5 (95% CI: 2.3-9.4) for ICH has been recently reported in comparison to a reference group of patients of 70-74 years[25]. Elderly patients are at higher risk of bleeding for several reasons, including the lower dose of anticoagulant required for effective anticoagulation (mainly because of reduced metabolic clearance)[26], the higher frequency of pathological changes in cerebral vessels, such as leukoaraiosis and amyloid angiopathy, which may increase the risk of ICH[27,28], and the increased prevalence of diverticulosis, malignancy, angiodysplasias, and ischemic colitis, which in turn may predispose to gastrointestinal bleeding. Additionally, elderly patients have a higher prevalence of comorbid conditions and are more likely to take interacting drugs[29]. Non-compliance to VKAs and lack of a clear understanding of their purpose and actions by older patients[30], who are also prone to mental impairment, are additional factors which may influence the bleeding rate.
Gender
Female gender has been found to be associated with a greater risk of bleeding during OAC therapy with VKAs for atrial fibrillation[31,32], but such an association has not been found in another study which enrolled patients with various indications for VKA anticoagulation[33].
Intensity and quality of anticoagulation
Although bleeding complications are not always related to a high intensity of anticoagulation and may occur even with INR values lower than 2.0, the target intensity of anticoagulation, and especially the actually achieved intensity, have long been recognized as major determinants of anticoagulation-related hemorrhages[11]. The increase in bleeding becomes exponential for INR values > 4.5, while the lowest rate is observed with INR values between 2.0 and 3.0[32]. The risk of death is also related to INR values with a minimum risk at INR 2.2[34]. High INR values are associated with an excess in mortality as well with a 2-fold increase in risk for one unit increase in INR above 2.5[34].
The initiation phase of anticoagulation, and especially the first 90 d of treatment, are associated with a higher incidence of bleeding[32,35]. Factors including the unmasking of occult lesions at the beginning of anticoagulation and/or less adequacy of dose adjustments in that period may account for this finding.
The quality of anticoagulation, as expressed by the time spent within the TTR, is another important variable influencing the likelihood of hemorrhagic complications. A strong relationship between TTR and bleeding, as well as thromboembolic complications, has consistently been reported in different patient populations and different intensity ranges[6]. Both major bleeding and mortality rates have been reported to be significantly higher in patients with TTR < 60% (3.85% and 4.20%, respectively) compared to those with TTR > 75% (1.58% and 1.69%, respectively)[36]. Apart from the application of general measures, like patient information and education and use of coumarin derivatives with a longer half-life, such as warfarin and phenprocoumon[37-39], achievement of good anticoagulation control may be better obtained by monitoring the treatment at specialized coagulation services or by patients themselves[6,40].
Comorbid conditions and comedications
Both as a marker of increased patient frailty and cause of concomitant use of other medications, the presence of comorbidities represents another factor potentially increasing the risk of bleeding during OAC therapy with VKAs. Apart from previous bleeding (especially in the gastrointestinal tract), which is the most potent predictor of recurrent hemorrhagic complications, congestive heart failure, hepatic or renal failure and diabetes have been identified as conditions associated with major bleeding[41,42]. Blood pressure control is also a critical factor for hemorrhagic complications during VKAs therapy. Among anticoagulated patients experiencing bleeding complications, a higher prevalence of history of hypertension has been frequently reported compared to patients with no previous bleeding[43]. Therefore, strict monitoring and control of blood pressure is warranted to reduce the risk of major hemorrhagic complications. More time spent above the intended intensity of OAC and wide and unpredictable fluctuations of the INR have been observed in patients with malignancies, which should also be regarded as risk factors for bleeding during VKA anticoagulation[44].
Among concomitant drugs frequently taken by patients on OAC therapy, antiplatelet agents are the most important because of the additional inhibitory effect on the anticoagulation system. Such an effect is of high clinical relevance because of the frequent coexistence, especially in elderly patients, of conditions such as atrial fibrillation or venous thromboembolism and coronary artery disease, where both VKAs and antiplatelet agents are indicated. Indeed, a relative risk of major bleeding of 2.5 (95% CI: 1.7-3.7) has been reported for the association of VKAs and aspirin[45]. An increasingly important subset of OAC patients potentially at increased bleeding risk is represented by those with an acute coronary syndrome and/or undergoing percutaneous coronary intervention with stent implantation, in whom a course of dual antiplatelet therapy with aspirin and clopidogrel is necessary to prevent stent thrombosis and/or ischemic recurrences. These patients represent 5%-10% of the whole population undergoing percutaneous coronary revascularization and appear exposed to a higher risk of major bleeding, which apparently increases with prolongation of treatment[46,47]. While waiting for solid data on drug combinations, such as VKAs plus clopidogrel[48], in patients on triple therapy of VKA, aspirin and clopidogrel, meticulous care should be exerted (1) to prolong this regimen for as short as possible (therefore avoiding the implantation of drug-eluting stents for which a duration of 6-12 mo of clopidogrel therapy is recommended)[49]; (2) to target an INR at the lower end (i.e., between 2.0 and 2.5) of the TTR; (3) to frequently review the patient and test the INR; and (4) to extensively use gastric protective agents[46,47].
Genetic factors
Recent advances in the pharmacogenetics of VKAs have greatly increased the understanding of their mechanism of action and of the known broad inter-individual variability in VKA response. It is now known that at least 30 genes are involved in the metabolism and action of warfarin, and some polymorphism of genes encoding for VKORC1 and CYP2C9 enzymes is present[6,50]. While mutations of VKORC1 are associated with different sensitivities to VKA, polymorphism of CYP2C9 can cause a delayed stabilization of VKA treatment[11]. Indeed, CYP2C9 variants are significantly more frequent among patients with an unstable response to VKAs[30] who achieve a stable dose significantly later, spend significantly more time above the therapeutic INR range in the initial phase of treatment, and have higher risk of having INR values > 5.0 as compared to non-carrier patients[50]. Owing to the reported association between gene variants and risk of bleeding and dose requirements in the initial phase of anticoagulation[51], several dosing algorithms based on VKORC1 and CYP2C9 genotypes have been proposed, although not integrated yet in clinical practice, to assist initiation of VKA treatment[52].
BLEEDING RISK SCORES
Stratification of the individual bleeding risk prior to initiation of OAC therapy with VKAs is another important measure to adopt for prevention of hemorrhagic complications[53]. To assist clinicians in this task, several schemes have been developed (Table 3).
Table 3.
Most popular bleeding risk prediction scores
| Author | Ref. | Calculation | Risk classification |
| mOBRI | [54] | Age ≥ 65 yr, previous stroke, GI bleed in the last 2 wk, ≥ 1 of the following: recent MI, hematocrit < 30%, creatinine > 1.5 mg/dL, diabetes) | Low: 0 points |
| Intermediate: 1-2 points | |||
| 1 point each | High: ≥ 3 points | ||
| HEMORR2HAGES | [55] | Hepatic or renal disease, ethanol abuse, malignancy, older, reduced platelet count/function, re-bleeding, uncontrolled hypertension, anemia, genetic factors, excessive fall risk, and stroke | Low: 0-1 points |
| Intermediate: 2-3 points | |||
| 1 point each and 2 points for previous bleed | High: ≥ 4 points | ||
| Shireman et al | [56] | (0.49 × age ≥ 70 yr) + (0.32 × female gender) + (0.58 × remote bleed) + (0.62 × recent bleed) + (0.71 × alcohol/drug abuse) + (0.27 × diabetes) + (0.86 × anemia) + (0.32 × antiplatelet therapy) | Low: ≤ 1.07 points |
| Intermediate: < 1.07 to < 2.19 points | |||
| 1 point each | High: ≥ 2.19 points | ||
| HAS-BLED | [57] | Hypertension (SBP > 160 mmHg), abnormal renal/liver function, stroke, history of bleeding, labile INR, elderly age (> 65 yr), drugs (antiplatelets/NSAIDs/alcohol) | Low: 0-1 points |
| Intermediate: 1-2 points | |||
| 1 point each | High: ≥ 3 points |
GI: Gastrointestinal; MI: Myocardial infarction; SBP: Systolic blood pressure; NSAIDs: Non-steroidal antiinflammatory drugs.
The modified outpatient bleeding risk index (mOBRI) has been prospectively derived and extensively validated in patients with different indications for VKAs[54]. Also, the mOBRI was evaluated in a “real-life” setting of anticoagulation monitoring (i.e., primary care physicians or pharmacist-run anticoagulation clinic) and the assessment of bleeding was blinded[54]. The hepatic or renal disease, ethanol abuse, malignancy, older, reduced platelet count/function, re-bleeding, uncontrolled hypertension, anemia, genetic factors, excessive fall risk, and stroke score has been derived from a retrospective chart review of nationwide registry data of patients with atrial fibrillation[55]. The retrospective design, the inclusion of genetic factors (which are rarely investigated in common practice), and of anemia and platelet data (also infrequently available), limit the usefulness of this score, as well as the lack of inclusion of important factors such as the concomitant use of antiplatelet agents and/or other drugs. The schema by Shireman et al[56] is also derived from a retrospective evaluation of nationwide registry data, and incorporates eight risk factors for bleeding. As regards limitations, the follow-up period was relatively short (i.e. 90 d), the outcome assessment was not blinded, and the quality of anticoagulation control and the use of comedications were not reported[56]. Finally, the individual determination of this score requires a complex mathematical calculation, which makes it rather impractical[56]. The hypertension, abnormal liver or renal function, stroke, bleeding, labile INRs, elderly, drugs or alcohol (HAS-BLED) score has been recently developed for patients with atrial fibrillation, based on the prospective Euro Heart Survey on atrial fibrillation[57]. Compared with the previous three scores, the HAS-BLED score was recently demonstrated to have better predictive ability for bleeding among all patients enrolled in the SPORTIF III and V trials, as well as among warfarin-naïve patients and patients treated with warfarin and aspirin[58]. The HAS-BLED score appears easy and user-friendly for everyday application, owing to the small number of variables to memorize and the common availability of all the information required for risk calculation. Finally, the HAS-BLED score allows for periodical re-assessment of a patient’s bleeding risk as it also takes into account the quality of INR control.
When applying the different bleeding scores, a wide variability in the prevalence of patients determined to be at low-, moderate-, and high-risk is observed because of differences in the risk factors comprising each schema, the various definitions of major bleeding, the different lengths of follow-up in the cohorts, and the different populations evaluated in the studies. Furthermore, no data on the impact of these scores on patient outcomes are currently available, so that none of the proposed bleeding risk scores can currently be recommended for widespread clinical use. Nonetheless, it must be emphasized that bleeding risk stratification should represent an integral part of the management of OAC therapy, and application of these scores may assist clinicians in their decision-making in everyday clinical practice.
NOVEL ORAL ANTICOAGULANTS
While VKAs are the standard drugs for OAC therapy, they have several major limitations, including the narrow therapeutic window, the cumbersome management, and the wide inter- and intra-individual variability. Therefore, more effective and/or safer and/or easier to use oral anticoagulants have long been sought. Recently, two main classes of new non-VKA oral anticoagulants (i.e. factor Xa-inhibitors and direct thrombin inhibitors) have been developed. These agents can be given in fixed doses, have little interaction with foods and drugs, and do not require regular monitoring of anticoagulation[59].
Apixaban, rivaroxaban and edoxaban are orally active, direct inhibitors of factor Xa. While being currently evaluated in several large, double-blind trials in patients with atrial fibrillation or venous thromboembolism, some evidence about the efficacy and safety of these drugs has already been reported. In the EINSTEIN-DVT and EINSTEIN-Extension studies[1], 3449 patients with acute deep vein thrombosis received, in an open-label manner, rivaroxaban or standard treatment (i.e. initial course of enoxaparin followed by VKAs) for 3, 6 or 12 mo. The 602 patients who had completed 6 to 12 mo of treatment then entered a double-blind study with randomization to rivaroxaban or placebo for an additional 6 or 12 mo. In the whole population, the efficacy of rivaroxaban on recurrent venous thromboembolism was non-inferior to the enoxaparin/VKA regimen (2.1% vs 3.0%, P < 0.001). The safety, as expressed by the on-treatment occurrence of major bleeding, was identical (8.1% in both groups). In the extended-treatment group, rivaroxaban was significantly more effective (1.3% vs 7.1%, P < 0.001), however, there was an increased, albeit non significant, incidence of major bleeding (0.7% vs 0%). In the AVERROES trial[2] 5599 patients with atrial fibrillation, who were unsuitable for or who were not willing to receive VKAs were randomized to apixaban or aspirin. At the 1.1-year follow-up, the treatment with apixaban was significantly more effective on the incidence of stroke/systemic embolism (1.6% vs 3.7%, P < 0.001). No differences in the rates of major bleeding were observed between the apixaban and aspirin groups (1.4% vs 1.2%, P = 0.57). In the double-blind ROCKET-AF trial[3], which enrolled > 14 000 atrial fibrillation patients, and investigated the efficacy (incidence of stroke/systemic embolism) and safety (incidence of bleeding) of rivaroxaban compared to warfarin, rivaroxaban was more effective (1.71% vs 2.16%, P < 0.001 for non-inferiority), without no significant difference in the rate of major bleeding (3.60% vs 3.45%).
Dabigatran is an orally active, direct thrombin inhibitor, which has been tested for the long-term treatment of patients with nonvalvular atrial fibrillation and venous thromboembolism. In the RE-LY trial, 18 113 patients with atrial fibrillation were randomized to two blinded doses of dabigatran against open-label warfarin[4]. At 2-year follow up, the primary outcome of stroke and systemic embolism was lower both with low-dose and high-dose dabigatran compared to warfarin (1.53% and 1.11% vs 1.69%, P < 0.001 for non-inferiority and P < 0.001 for superiority, respectively). The incidence of major bleeding was lower in the low-dose group (2.71% vs 3.36%, P = 0.03) and similar to warfarin in the high-dose group (3.11% vs 3.36%, P = 0.31). Among the 2564 patients with acute venous thromboembolism enrolled in the double-blind RE-COVER study, dabigatran was as effective as warfarin for secondary prevention of recurrent venous thromboembolism at 6-mo follow-up (2.4% vs 2.1%). The incidence of major bleeding was also comparable in the two groups (1.6% vs 1.9%)[5].
In the light of the promising outcomes, as well as of the superior ease of use, the novel non-VKA oral anticoagulants represent an attractive alternative to VKAs for OAC therapy. Nonetheless, additional data on the impact of the lack of a method to monitor the intensity of anticoagulation, lack of a specific antidote, and little information regarding the risk/benefit ratio of their combination with more potent antiplatelet agents, such as the increasingly used prasugrel or ticagrelor, are necessarily awaited before these drugs can be truly considered substitutes for VKAs.
CONCLUSION
OAC therapy with VKAs is the most effective available treatment for prevention of thromboembolic complications in frequent clinical conditions, such as atrial fibrillation, venous thromboembolism, prosthetic heart valves, and cardiogenic stroke. Such efficacy comes at the price of an increased risk of overall, major and ICH bleeding. While novel, non-VKA oral anticoagulants, such as direct thrombin inhibitors and direct factor Xa inhibitors, have been showing promise in the setting of atrial fibrillation and venous thromboembolism, VKA treatment should currently be offered to all patients at high risk of arterial/venous thromboembolism because of the established benefit outweighing the risk. However, meticulous care should be directed towards accurate bleeding risk stratification and minimization and/or control of all the numerous factors known to influence the risk of hemorrhagic complications.
Footnotes
Peer reviewer: Shinji Satoh, MD, PhD, Department of Cardiology and Clinical Research Institute, NationalHospital Organization Kyushu Medical Center, 1-8-1 Jigyohama, Chuo-ku, Fukuoka 810-8563, Japan
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
References
- 1.Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, Gallus AS, Lensing AW, Misselwitz F, Prins MH, Raskob GE, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363:2499–2510. doi: 10.1056/NEJMoa1007903. [DOI] [PubMed] [Google Scholar]
- 2.Connolly SJ, Eikelboom J, Joyner C, Diener HC, Hart R, Golitsyn S, Flaker G, Avezum A, Hohnloser SH, Diaz R, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364:806–817. doi: 10.1056/NEJMoa1007432. [DOI] [PubMed] [Google Scholar]
- 3.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 4.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 5.Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, Baanstra D, Schnee J, Goldhaber SZ. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361:2342–2352. doi: 10.1056/NEJMoa0906598. [DOI] [PubMed] [Google Scholar]
- 6.Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133:160S–198S. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 7.Schulman S, Beyth RJ, Kearon C, Levine MN. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133:257S–298S. doi: 10.1378/chest.08-0674. [DOI] [PubMed] [Google Scholar]
- 8.Levi M, Hovingh GK, Cannegieter SC, Vermeulen M, Büller HR, Rosendaal FR. Bleeding in patients receiving vitamin K antagonists who would have been excluded from trials on which the indication for anticoagulation was based. Blood. 2008;111:4471–4476. doi: 10.1182/blood-2007-11-123711. [DOI] [PubMed] [Google Scholar]
- 9.Fanikos J, Grasso-Correnti N, Shah R, Kucher N, Goldhaber SZ. Major bleeding complications in a specialized anticoagulation service. Am J Cardiol. 2005;96:595–598. doi: 10.1016/j.amjcard.2005.03.104. [DOI] [PubMed] [Google Scholar]
- 10.Stehle S, Kirchheiner J, Lazar A, Fuhr U. Pharmacogenetics of oral anticoagulants: a basis for dose individualization. Clin Pharmacokinet. 2008;47:565–594. doi: 10.2165/00003088-200847090-00002. [DOI] [PubMed] [Google Scholar]
- 11.Palareti G, Cosmi B. Bleeding with anticoagulation therapy - who is at risk, and how best to identify such patients. Thromb Haemost. 2009;102:268–278. doi: 10.1160/TH08-11-0730. [DOI] [PubMed] [Google Scholar]
- 12.Linkins LA, Choi PT, Douketis JD. Clinical impact of bleeding in patients taking oral anticoagulant therapy for venous thromboembolism: a meta-analysis. Ann Intern Med. 2003;139:893–900. doi: 10.7326/0003-4819-139-11-200312020-00007. [DOI] [PubMed] [Google Scholar]
- 13.Choudhry NK, Anderson GM, Laupacis A, Ross-Degnan D, Normand SL, Soumerai SB. Impact of adverse events on prescribing warfarin in patients with atrial fibrillation: matched pair analysis. BMJ. 2006;332:141–145. doi: 10.1136/bmj.38698.709572.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ananthasubramaniam K, Beattie JN, Rosman HS, Jayam V, Borzak S. How safely and for how long can warfarin therapy be withheld in prosthetic heart valve patients hospitalized with a major hemorrhage? Chest. 2001;119:478–484. doi: 10.1378/chest.119.2.478. [DOI] [PubMed] [Google Scholar]
- 15.Hackam DG, Kopp A, Redelmeier DA. Prognostic implications of warfarin cessation after major trauma: a population-based cohort analysis. Circulation. 2005;111:2250–2256. doi: 10.1161/01.CIR.0000163548.38396.E7. [DOI] [PubMed] [Google Scholar]
- 16.Dentali F, Ageno W, Crowther M. Treatment of coumarin-associated coagulopathy: a systematic review and proposed treatment algorithms. J Thromb Haemost. 2006;4:1853–1863. doi: 10.1111/j.1538-7836.2006.01986.x. [DOI] [PubMed] [Google Scholar]
- 17.Crowther MA, Douketis JD, Schnurr T, Steidl L, Mera V, Ultori C, Venco A, Ageno W. Oral vitamin K lowers the international normalized ratio more rapidly than subcutaneous vitamin K in the treatment of warfarin-associated coagulopathy. A randomized, controlled trial. Ann Intern Med. 2002;137:251–254. doi: 10.7326/0003-4819-137-4-200208200-00009. [DOI] [PubMed] [Google Scholar]
- 18.Lubetsky A, Yonath H, Olchovsky D, Loebstein R, Halkin H, Ezra D. Comparison of oral vs intravenous phytonadione (vitamin K1) in patients with excessive anticoagulation: a prospective randomized controlled study. Arch Intern Med. 2003;163:2469–2473. doi: 10.1001/archinte.163.20.2469. [DOI] [PubMed] [Google Scholar]
- 19.Singer DE, Chang Y, Fang MC, Borowsky LH, Pomernacki NK, Udaltsova N, Go AS. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann Intern Med. 2009;151:297–305. doi: 10.7326/0003-4819-151-5-200909010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Geest-Daalderop JH, Hutten BA, Péquériaux NC, de Vries-Goldschmeding HJ, Räkers E, Levi M. Invasive procedures in the outpatient setting: managing the short-acting acenocoumarol and the long-acting phenprocoumon. Thromb Haemost. 2007;98:747–755. [PubMed] [Google Scholar]
- 21.Aguilar MI, Hart RG, Kase CS, Freeman WD, Hoeben BJ, García RC, Ansell JE, Mayer SA, Norrving B, Rosand J, et al. Treatment of warfarin-associated intracerebral hemorrhage: literature review and expert opinion. Mayo Clin Proc. 2007;82:82–92. doi: 10.4065/82.1.82. [DOI] [PubMed] [Google Scholar]
- 22.van Aart L, Eijkhout HW, Kamphuis JS, Dam M, Schattenkerk ME, Schouten TJ, Ploeger B, Strengers PF. Individualized dosing regimen for prothrombin complex concentrate more effective than standard treatment in the reversal of oral anticoagulant therapy: an open, prospective randomized controlled trial. Thromb Res. 2006;118:313–320. doi: 10.1016/j.thromres.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 23.Keeling D. Duration of anticoagulation: decision making based on absolute risk. Blood Rev. 2006;20:173–178. doi: 10.1016/j.blre.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med. 1994;120:897–902. doi: 10.7326/0003-4819-120-11-199406010-00001. [DOI] [PubMed] [Google Scholar]
- 25.Fang MC, Chang Y, Hylek EM, Rosand J, Greenberg SM, Go AS, Singer DE. Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for atrial fibrillation. Ann Intern Med. 2004;141:745–752. doi: 10.7326/0003-4819-141-10-200411160-00005. [DOI] [PubMed] [Google Scholar]
- 26.Russmann S, Gohlke-Bärwolf C, Jähnchen E, Trenk D, Roskamm H. Age-dependent differences in the anticoagulant effect of phenprocoumon in patients after heart valve surgery. Eur J Clin Pharmacol. 1997;52:31–35. doi: 10.1007/s002280050245. [DOI] [PubMed] [Google Scholar]
- 27.Rosand J, Hylek EM, O’Donnell HC, Greenberg SM. Warfarin-associated hemorrhage and cerebral amyloid angiopathy: a genetic and pathologic study. Neurology. 2000;55:947–951. doi: 10.1212/wnl.55.7.947. [DOI] [PubMed] [Google Scholar]
- 28.Smith EE, Rosand J, Knudsen KA, Hylek EM, Greenberg SM. Leukoaraiosis is associated with warfarin-related hemorrhage following ischemic stroke. Neurology. 2002;59:193–197. doi: 10.1212/wnl.59.2.193. [DOI] [PubMed] [Google Scholar]
- 29.Shorr RI, Ray WA, Daugherty JR, Griffin MR. Concurrent use of nonsteroidal anti-inflammatory drugs and oral anticoagulants places elderly persons at high risk for hemorrhagic peptic ulcer disease. Arch Intern Med. 1993;153:1665–1670. [PubMed] [Google Scholar]
- 30.Palareti G, Legnani C, Guazzaloca G, Lelia V, Cosmi B, Lunghi B, Marchetti G, Poli D, Pengo V. Risks factors for highly unstable response to oral anticoagulation: a case-control study. Br J Haematol. 2005;129:72–78. doi: 10.1111/j.1365-2141.2005.05417.x. [DOI] [PubMed] [Google Scholar]
- 31.Sam C, Massaro JM, D’Agostino RB, Levy D, Lambert JW, Wolf PA, Benjamin EJ. Warfarin and aspirin use and the predictors of major bleeding complications in atrial fibrillation (the Framingham Heart Study) Am J Cardiol. 2004;94:947–951. doi: 10.1016/j.amjcard.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 32.Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D’Angelo A, Pengo V, Erba N, Moia M, Ciavarella N, et al. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Italian Study on Complications of Oral Anticoagulant Therapy. Lancet. 1996;348:423–428. doi: 10.1016/s0140-6736(96)01109-9. [DOI] [PubMed] [Google Scholar]
- 33.Pengo V, Legnani C, Noventa F, Palareti G. Oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and risk of bleeding. A Multicenter Inception Cohort Study. Thromb Haemost. 2001;85:418–422. [PubMed] [Google Scholar]
- 34.Odén A, Fahlén M. Oral anticoagulation and risk of death: a medical record linkage study. BMJ. 2002;325:1073–1075. doi: 10.1136/bmj.325.7372.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation. 2007;115:2689–2696. doi: 10.1161/CIRCULATIONAHA.106.653048. [DOI] [PubMed] [Google Scholar]
- 36.White HD, Gruber M, Feyzi J, Kaatz S, Tse HF, Husted S, Albers GW. Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V. Arch Intern Med. 2007;167:239–245. doi: 10.1001/archinte.167.3.239. [DOI] [PubMed] [Google Scholar]
- 37.Pattacini C, Manotti C, Pini M, Quintavalla R, Dettori AG. A comparative study on the quality of oral anticoagulant therapy (warfarin versus acenocoumarol) Thromb Haemost. 1994;71:188–191. [PubMed] [Google Scholar]
- 38.Fihn SD, Gadisseur AA, Pasterkamp E, van der Meer FJ, Breukink-Engbers WG, Geven-Boere LM, van Meegen E, de Vries-Goldschmeding H, Antheunissen-Anneveld I, van’t Hoff AR, et al. Comparison of control and stability of oral anticoagulant therapy using acenocoumarol versus phenprocoumon. Thromb Haemost. 2003;90:260–266. doi: 10.1160/TH02-10-0179. [DOI] [PubMed] [Google Scholar]
- 39.Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med. 2004;164:2044–2050. doi: 10.1001/archinte.164.18.2044. [DOI] [PubMed] [Google Scholar]
- 40.Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P. Self-monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet. 2006;367:404–411. doi: 10.1016/S0140-6736(06)68139-7. [DOI] [PubMed] [Google Scholar]
- 41.DiMarco JP, Flaker G, Waldo AL, Corley SD, Greene HL, Safford RE, Rosenfeld LE, Mitrani G, Nemeth M. Factors affecting bleeding risk during anticoagulant therapy in patients with atrial fibrillation: observations from the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study. Am Heart J. 2005;149:650–656. doi: 10.1016/j.ahj.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 42.McMahan DA, Smith DM, Carey MA, Zhou XH. Risk of major hemorrhage for outpatients treated with warfarin. J Gen Intern Med. 1998;13:311–316. doi: 10.1046/j.1525-1497.1998.00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abdelhafiz AH, Wheeldon NM. Results of an open-label, prospective study of anticoagulant therapy for atrial fibrillation in an outpatient anticoagulation clinic. Clin Ther. 2004;26:1470–1478. doi: 10.1016/j.clinthera.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 44.Palareti G, Legnani C, Lee A, Manotti C, Hirsh J, D’Angelo A, Pengo V, Moia M, Coccheri S. A comparison of the safety and efficacy of oral anticoagulation for the treatment of venous thromboembolic disease in patients with or without malignancy. Thromb Haemost. 2000;84:805–810. [PubMed] [Google Scholar]
- 45.Rothberg MB, Celestin C, Fiore LD, Lawler E, Cook JR. Warfarin plus aspirin after myocardial infarction or the acute coronary syndrome: meta-analysis with estimates of risk and benefit. Ann Intern Med. 2005;143:241–250. doi: 10.7326/0003-4819-143-4-200508160-00005. [DOI] [PubMed] [Google Scholar]
- 46.Rubboli A, Halperin JL, Airaksinen KE, Buerke M, Eeckhout E, Freedman SB, Gershlick AH, Schlitt A, Tse HF, Verheugt FW, et al. Antithrombotic therapy in patients treated with oral anticoagulation undergoing coronary artery stenting. An expert consensus document with focus on atrial fibrillation. Ann Med. 2008;40:428–436. doi: 10.1080/07853890802089786. [DOI] [PubMed] [Google Scholar]
- 47.Lip GY, Huber K, Andreotti F, Arnesen H, Airaksinen KJ, Cuisset T, Kirchhof P, Marín F. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary intervention/ stenting. Thromb Haemost. 2010;103:13–28. doi: 10.1160/TH09-08-0580. [DOI] [PubMed] [Google Scholar]
- 48.Dewilde W, Berg JT. Design and rationale of the WOEST trial: What is the Optimal antiplatElet and anticoagulant therapy in patients with oral anticoagulation and coronary StenTing (WOEST) Am Heart J. 2009;158:713–718. doi: 10.1016/j.ahj.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 49.Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501–2555. doi: 10.1093/eurheartj/ehq277. [DOI] [PubMed] [Google Scholar]
- 50.Vecsler M, Loebstein R, Almog S, Kurnik D, Goldman B, Halkin H, Gak E. Combined genetic profiles of components and regulators of the vitamin K-dependent gamma-carboxylation system affect individual sensitivity to warfarin. Thromb Haemost. 2006;95:205–211. doi: 10.1160/TH05-06-0446. [DOI] [PubMed] [Google Scholar]
- 51.Meckley LM, Wittkowsky AK, Rieder MJ, Rettie AE, Veenstra DL. An analysis of the relative effects of VKORC1 and CYP2C9 variants on anticoagulation related outcomes in warfarin-treated patients. Thromb Haemost. 2008;100:229–239. [PubMed] [Google Scholar]
- 52.Sconce EA, Khan TI, Wynne HA, Avery P, Monkhouse L, King BP, Wood P, Kesteven P, Daly AK, Kamali F. The impact of CYP2C9 and VKORC1 genetic polymorphism and patient characteristics upon warfarin dose requirements: proposal for a new dosing regimen. Blood. 2005;106:2329–2333. doi: 10.1182/blood-2005-03-1108. [DOI] [PubMed] [Google Scholar]
- 53.Landefeld CS, Goldman L. Major bleeding in outpatients treated with warfarin: incidence and prediction by factors known at the start of outpatient therapy. Am J Med. 1989;87:144–152. doi: 10.1016/s0002-9343(89)80689-8. [DOI] [PubMed] [Google Scholar]
- 54.Beyth RJ, Quinn LM, Landefeld CS. Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin. Am J Med. 1998;105:91–99. doi: 10.1016/s0002-9343(98)00198-3. [DOI] [PubMed] [Google Scholar]
- 55.Gage BF, Yan Y, Milligan PE, Waterman AD, Culverhouse R, Rich MW, Radford MJ. Clinical classification schemes for predicting hemorrhage: results from the National Registry of Atrial Fibrillation (NRAF) Am Heart J. 2006;151:713–719. doi: 10.1016/j.ahj.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 56.Shireman TI, Mahnken JD, Howard PA, Kresowik TF, Hou Q, Ellerbeck EF. Development of a contemporary bleeding risk model for elderly warfarin recipients. Chest. 2006;130:1390–1396. doi: 10.1378/chest.130.5.1390. [DOI] [PubMed] [Google Scholar]
- 57.Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–1100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 58.Lip GY, Frison L, Halperin JL, Lane DA. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. J Am Coll Cardiol. 2011;57:173–180. doi: 10.1016/j.jacc.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 59.Ahrens I, Lip GY, Peter K. New oral anticoagulant drugs in cardiovascular disease. Thromb Haemost. 2010;104:49–60. doi: 10.1160/TH09-05-0327. [DOI] [PubMed] [Google Scholar]


