Summary
The ability to control the growth of new blood vessels would be an extraordinary therapeutic tool for many disease processes. Too often, the promises of discoveries in the basic science arena fail to translate to clinical success. While several anti angiogenic therapeutics are now FDA approved, the envisioned clinical benefits have yet to be seen. The ability to clinically non-invasively image angiogenesis would potentially be used to identify patients who may benefit from anti-angiogenic treatments, prognostication/risk stratification and therapy monitoring. This article reviews the current and future prospects of implementing angiogenesis imaging in the clinic.
Keywords: Molecular Imaging, Targeted Imaging, Angiogenesis, Oncology, Cardiac Disease, PET/CT, MR, DCE MR, US, microbubbles, bevicizumab, VEFG, integrins, Nuclear medicine, [18F]galacto-RGD, [18F]fluciclitide, [18F]AH111585
The Angiogenic Switch
The hypothesis that tumor growth is dependent on the development of new blood vessels and that the tumor cells themselves direct this process was proposed by Folkman in 1971. (1)As tumors increase in size, they begin to exceed the ~1 mm oxygen diffusion limit, whereupon they must also increase their blood supply in order to continue growing. Mechanisms by which they accomplish this includes angiogenesis—developing new blood vessels from existing blood vessels. Tumors unable to undergo angiogenesis either die or arrest growth and remain in a dormant state that is typically <2 mm in diameter, resulting in large reservoirs of occult disease that potentially can activate under certain conditions, such as inhibition of the immune system or provocation by excess growth factors(1–2). Angiogenesis plays a critical role in a tumor’s continued growth. The proliferative rate of many dormant tumors is equal to that of angiogenic tumors; however the apoptosis rate is significantly decreased in the latter. Thus, dormant tumors are poised for progression. While increased cellular proliferation and decreased apoptosis are necessary for tumor growth, they are not sufficient for sustained tumor growth. The evolution of an avascular “dormant” tumor to an aggressive metastatic cancer is believed to occur after an “angiogenic switch” has been thrown, giving the tumor the resources to obtain oxygen and nutrients through increased blood supply. (3)It is projected that only ~1 in 600 “dormant” tumors switch to an angiogenic phenotype. (4)While the underlying trigger for the switch is not yet known and may differ according to tumor type, the process is directly regulated by oncogenes, tumor suppressor genes, and indirectly controlled by the microenvironment (i.e. hypoxia, glucose concentration, pH). Udagawa et al. demonstrated that after transducing non-angiogenic osteogenic sarcoma cells with the Ras oncogene, the expression of the pro-angiogenic mediator, vascular endothelial growth factor (VEGF), increased by 38%, and that of the anti-angiogenic factor thrombospondin-1 (tsp-1) decreased by 50%. (5). In a mouse model, animals with Ras transduction lived only a few weeks, while those without the Ras oncogene lived for ~ 1 year. In general, activation of oncogenes often results in increased endothelial cell proliferation, migration and increase the rate of tumor cell apoptosis.
Indirect control of angiogenesis by the microenvironment is illustrated by the the ability of a low oxygen environment to activate Hypoxia-inducible factor alpha(HIF-1a), which in turn, activates pathways which, among other things, controls angiogenesisis. HIF-1a is a transcription factor which upregulates VEGF, and other pro-angiogenic genes. HIF-1a is degraded in the presence of oxygen, thus regulating angiogenesis under normal circumstances. If HIF-1a is allowed to accumulate in the cell (either by increased production or decreased degradation), the cell will transcribe pro-angiogenic genes, resulting in angiogenesis
The Players
Often lost in the discussion of angiogenesis is that it is a normal physiologic process and becomes pathologic only when it is no longer regulated. The biological process of angiogenesis is complex and involves activation of inflammatory cells (macrophages, monocytes, lymphocytes), the migration of endothelial or progenitor cells and the proliferation of existing endothelial cells. (6)Angiogenesis plays a role in wound healing, the menstrual cycle and pregnancy. There are a multitude of regulatory molecules and pathways involved in angiogenesis, making therapeutic manipulation of the process challenging. These regulatory molecules may arise from within the extracellular matrix (ECM) or be produced by tumor, stromal or immune cells. For the most part, normal mature tissue is at steady state: pro-angiogenic effectors balance anti-angiogenic effectors, resulting in no net increase in vascularity. Physiologically, under appropriate circumstances (tissue growth damage or repair), the balance is tipped resulting in angiogenesis.
While a complete description of the molecular pathways which play a role in angiogenesis is beyond the scope of this article (interested reader’s are referred to an excellent text on angiogenesis edited by Marme and Fusenig (7))Selected well studied endogenous pro-angiogenic molecules are discussed briefly here: VEGF, Fibroblast Growth Factor (FGF), and αvβ3 integrin.
VEGF
VEGF is a 45 kD homodimeric glycoprotein secreted by tumor cells released and activated by heparinase, plasmin, urokinase, and plasminogen activator. Its interaction with VEGF receptor A (VEGF-A) on endothelial cells results in the mobilization of circulating endothelial precursors (CEP), decreased apoptosis, increased vascular permeability and actin reorganization. Up-regulated by the oncogene Ras, VEGF is secreted from tumors, binds to VEGFR-1 and -2 on endothelial cells (ECs) and bone marrow derived cells. Therapeutic modulation of the VEGF system has been shown to potentiate chemotherapy and radiation effects.
FGF
Associated with the extracellular matrix (ECM), protected from degradation by binding to heparin sulfate proteoglycans, FGF is released by heparinase. FGF induces cell proliferation, migration and production of proteases in endothelial cells. Interactions with Fibroblast Growth Factor receptors (FGFRs) and Heparin-Like glycosaminoglycans (HLGAG) result in FGFR dimerization or oligomerization and activation of the receptor tyrosine kinase. This activates multiple transduction pathways including sustained activation of Ras. (8)One of the first angiogenesis inhibitors used in humans was low dose interferon(INF)-α. A patient with progressive hemangiomatosis of both lungs leading to intractable hemoptysis was successfully treated with very low dose INF-α. (9)At these low doses (below that needed for a cytotoxic or immunosuppressive effect), angiogenesis was inhibited by suppression of FGF. (10)
αvβ3 integrins
Integrins are a family of receptors within the extracellular matrix (ECM) which span the cellular membrane, passing signals from the ECM to the cytoplasm and vice versa, essentially “integrating” the intracellular cytoskeleton with the ECM. These adhesion molecules activate signaling pathways which organize the cytoskeleton and increase cell proliferation. αvβ3 integrins can be associated with proliferating endothelial cells, and malignant cells, but are not found in mature blood vessels. αvβ3 integrin receptors contain a peptide binding pocket specific for the RGD (arg-gly-asp)peptide sequence. RGD peptide binding can initiate a multitude of signaling pathways including those controlling gene expression, tissue development, inflammation, angiogenesis, tumor cell growth and metastasis.
High αvβ3 expression has been demonstrated in melanomas, glioblastomas and certain sarcomas, with lower expression levels in breast cancers and renal cell carcinomas(RCC).(11)αvβ3 integrin levels have been correlated with disease progression in several malignancies including: melanoma, glioblastoma, ovarian cancer, and breast cancer.(12)(13)It has also been shown to mediate adhesive reactions of platelets and acts as a receptor for fibrinogen, Von Willebrand factor and fibronectin. (14)
Why image?
As the treatment of cancer moves towards the molecular control of cancer using targeted therapies, conventional anatomic imaging may prove insufficient. The current reliance on size criteria alone in determining whether a drug is effective can take many months. Moreover, determining activity within a tumor that is stable in size is impossible when using size criteria alone. Anti-angiogenic therapeutics targeting various steps in the angiogenesis pathway have entered the clinic(15)(i.e., bevacizumab, an antibody which neutralizes VEGF(16), sunitinib, which blocks VEGF receptors on vessels(17)and cilengitide, which blocks binding to integrins(18)). As the molecular changes occurring with anti-angiogenic treatment are not expected to result in rapid tumor volume loss, an imaging biomarker of therapeutic response could be of great value. Angiogenic inhibitors appear to have a bi-phasic (U-shaped) dose response curve—while their effect initially increases with dose, administration of higher doses actually results in a decreasing response.(19)Optimal dose and dosing schedules could be defined if one had an accurate marker for therapeutic response. Additionally, many angiogenic inhibitors appear to negatively regulate angiogenesis for a while before alternate molecular pathways develop to promote angiogenesis. (20)The point at which tumors begin to become resistant to angiogenic inhibition would be a useful marker for understanding the degree and duration of angiogenic suppression.
Angiogenesis is the key to a tumor’s independence. While it entails a complicated interaction of numerous effectors and pathways, control of this process may enable us to establish “permanent” tumor dormancy. A priori identification of the predominant signaling pathways could have prognostic value and may guide therapeutic selection. The ability to monitor the process in vivo can help direct such interventions.
How to image
There are several clinical imaging tools available, which can indirectly image angiogenesis by evaluating blood flow and perfusion. A growing number of imaging agents are being used to directly image angiogenesis by aiming at specific targets.
Indirect imaging of angiogenesis
There are several methods of indirectly monitoring angiogenesis using conventional imaging, notably, contrast enhanced ultrasound (US), computed tomography (CT)and Magnetic Resonance Imaging (MRI).
Routinely performed contrast “enhanced”(CE)MRI and CT allow for the subjective differentiation between areas that are “well perfused” and those with “low or no” perfusion. The contrast agents used in both modalities highlight arterial blood flow initially, rapidly followed by venous and blood pool, and extra-vascular diffusion. Since these agents are low in molecular weight, they readily leak from angiogenic vessels making it difficult to distinguish between intravascular containment and extra-vascular leakage. For typical clinical applications, “snap-shot” images from arterial and venous phases are sufficient for diagnostic purposes, however to attempt to quantify perfusion and vessel permeability, dynamic contrast enhanced (DCE) methods are used. DCE imaging collects sequential images over a period of time and can be used to monitor perfusion and permeability in select clinical trials.
DCE MR
With the evolution of faster MR imaging sequences, rapid sequential imaging following a controlled IV bolus injection of a low molecular weight gadolinium diethyltriamine pentaacetic acid (Gd-DTPA) based contrast agent is now feasible and widely available.(21)This dynamic imaging captures the entire time course of contrast enhancement in an area of interest. By drawing a focal region of interest (ROI) and applying it to each image in the time series, a time activity curve (TAC), from which parameters representing the kinetics of the blood flow and permeability, can be extracted. As Gd-DTPA based contrast agents do not enter the intracellular space to a significant extent, the resultant TAC can be fit to a two compartment kinetic model, representing transit to and from the vasculature and extravascular extracellular spaces. For DCE MR, the rate constant describing the transit of contrast agent from the blood into the extravascular extracellular space is often referred to as Ktrans and the rate constant describing the return of tracer (from the extracellular extravascular space) to vasculature is termed kep. Parametric maps can be created resulting in images where the image intensities can be colorized and made proportional to the magnitude of the rate constants, Ktrans or kep.(22)It can be seen from Figure 1, that high Ktrans (rapid influx into extravascular tumor space) and kep (the rate of tumor efflux) is associated with a tumor phenotype. While modeling can be performed assuming the contrast entrance into the blood is instantaneous, a more realistic model incorporates the rate at which blood initially enters the system, using the vascular input function (estimated from an ROI within a homogenous portion of a vessel in the field of view). In theory, the use of an arterial input function (AIF), results in more accurate parameter estimates;(23)however inclusion of an AIF also risks the introduction of new errors from flow based artifacts in the targeted vessel. (24)Initial single center clinical trials using DCE MR are promising, with visible changes in parameters between baseline and early post therapy scans. (Figure 2)(25). The clinical relevance of these findings has yet to be validated particularly in light of a recent study showing higher morbidity in patients receiving anti-angiogenic therapy (compared with chemotherapy alone). (26–27)
FIGURE 1.
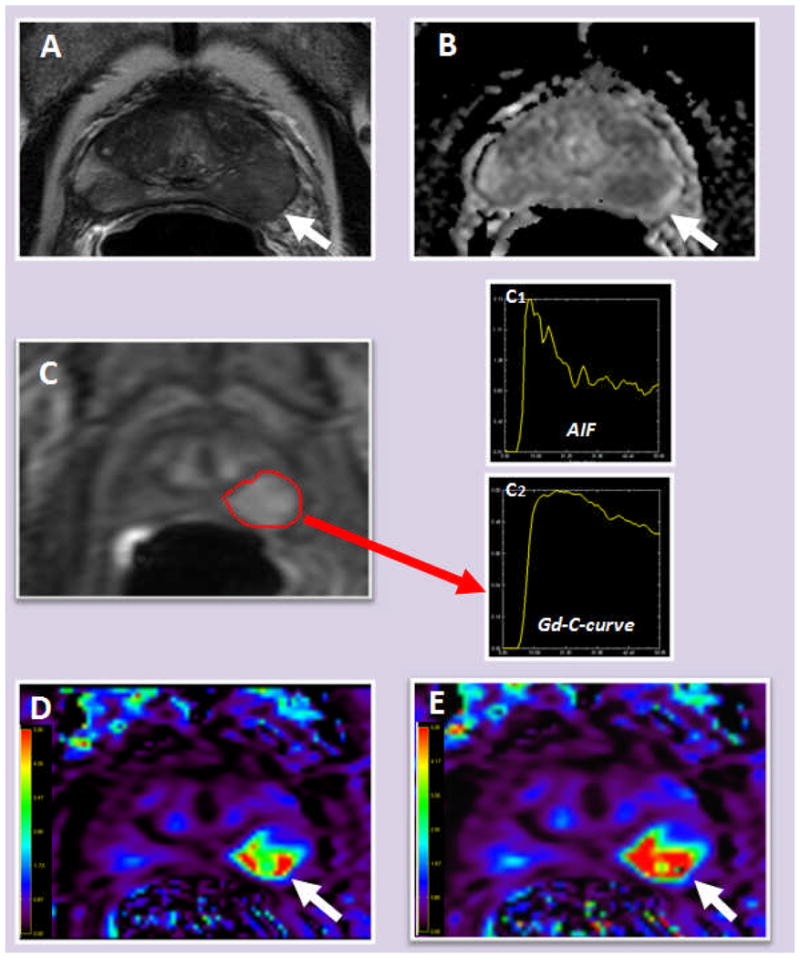
65-year-old man with serum prostate specific antigen (PSA) level of 9.2 ng/dl. Axial T2 weighted MRI shows a vague low signal intensity lesion in the left mid-base peripheral zone (arrow) (A); ADC maps derived from diffusion weighted MRI shows restricted diffusion within the left peripheral zone lesion (arrow) (B); raw DCE MR image demonstrates fast and early enhancement within the left peripheral zone lesion (marked in red) (C) (C1: arterial input function curve, C2: Gd concentration curve of the left peripheral zone lesion); Ktrans (S) and kep (E) maps derived from DCE MRI also localizes the left peripheral zone lesion (arrow).
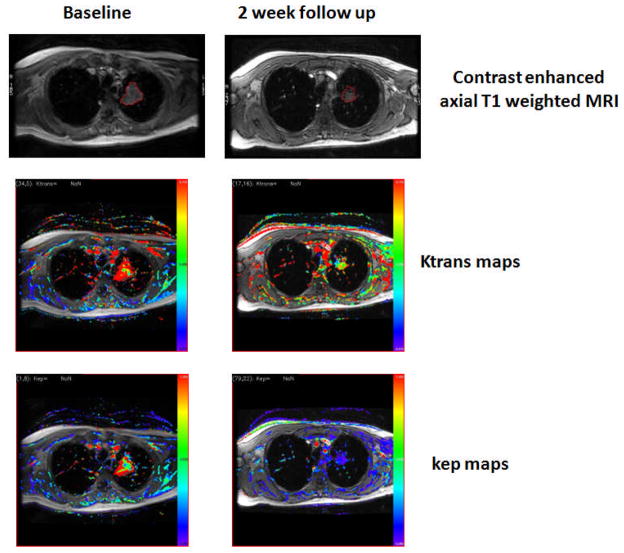
FIGURE 2.
57 year-old male with non-squamous cell lung cancer lesion in the upper lobe of the left lung (red region of interest (ROI). Initially high Ktrans and kep are seen in the baseline parametric maps, with the red coloring representing high flow (right column, second and third rows). Following Sorafenib treatment, the lesion size decreased and the Ktrans and kep values are reduced.
DCE MR provides the potential for semi-quantitative assessment; however the methodology first needs to be standardized if it is to be widely used and results are to be compared across centers. (28–29)Given the multiple vendors of MR imaging equipment, the vast range of available scanning sequences and coils and wide variability in compliance, standardization is not a simple process. One simplified method, that avoids the pitfalls of two compartment modeling, involves normalizing the MR signal intensity (SI) of the post contrast images to the baseline, thus establishing a relationship between SI and contrast agent concentration (i.e. each study serves as its own control); however the results are still semi-quantitative and the changes in signal intensity are not linear over the range of concentrations of gadolinium or background T1 values and therefore require further calibration.
There is significant ongoing effort to validate and standardize DCE MR. This work requires meticulous quality control and assurance, determination of parameter reproducibility, standardized imaging procedures and image analysis and, most importantly, correlation with an existing biomarker (i.e. proof that the process being measured actually represents the process of interest.) Such requirements have made accrual to trials with DCE-MRI difficult and cast doubt on the ability to actually recruit patients and conduct multi-institutional trials with rigid quality control, which hitherto has been lacking in radiology departments.
Routinely used low molecular weight Gd DTPA based imaging agents cannot be used to measure vascular volume since they easily leave the vasculature, diffusing into the extravascular spaces. Complexing Gd with albumin, dextran, liposomes, dendrimers etc, results in macromolecular contrast agents which remain confined to the vasculature at least for the period of the scanning, or enter the extravascular space only when the vessels are highly permeable; such agents may provide a method for measuring vascular volume in the future.
US
Ultrasound relies on acoustic reflections in soft tissue to construct an anatomic image. Contrast enhanced ultrasound is an appealing imaging modality for several reasons. US scanning equipment offers portability and low cost, data acquisition is rapid and in real time. Additionally, sound waves lack ionizing radiation which is advantageous for patient safety over repeated examinations. Doppler ultrasound can measure the velocity of blood, indicate flow direction and estimate blood flow.(30)Color Doppler can delineate tortuous vascular anatomy and malformations and help assess anti-angiogenic effects of therapy on tumors. Unfortunately, this technique is limited by variations in flow velocity from the cardiac cycle, and slow capillary flow, which is less than 1 mm/s, cannot be detected. Power Doppler is an improved feature that increases sensitivity at low flow rates and is not angle dependent. Blood volume flow can be calculated by this method, but there is no standardization.(31)Key features of Power Doppler include better edge definition and depiction of flow continuity.(32)The vascularity index (VI) is a quantitative parameter developed to assess in vivo tumor angiogenesis and is the ratio of the number of coloured pixels in the region of interest (ROI) divided by the total number of pixels in that ROI. Chen demonstrated that the VI was associated with tumor differentiation, lymph node metastasis and patient survival in colon cancer in one study and with lymph node metastasis, combined vascular endothelial growth factor (VEGF) and placenta growth factor (PIGF) expression status and patient survival in another study of gastric cancer.(33–34)Resistance to blood flow in the microcirculation can be determined with Doppler in tumors, but mixed high and low flow rates are often found secondary to characteristics of the tumor and compensatory response of surrounding tissue. Certain tumors, such as choriocarcinoma, demonstrate a consistent low resistance index which can be used to monitor effects of chemotherapy. (35)Power Doppler still has significant limitations. The resolution obtained with high frequencies restricts evaluation to only superficial tissue. Convoluted small vessel distribution is also difficult to distinguish. Vessels less than 100 um and blood flow rates less than 1 mm/sec (such as in the capillaries) are still challenging to evaluate and can be complicated by respiratory or cardiac motion artifact.(36) Combining contrast enhanced ultrasound and power Doppler methods have been applied to increase microvessel detection. In a preclinical mouse study with human breast cancer xenografts, contrast enhanced Doppler ultrasound correlated with angiogenic activity evaluated by immunohistochemistry in vessels measuring approximately 40 um in diameter. (37)(Magnon 2007) Advanced Doppler systems, including contrast-enhanced harmonic and pulse inversion imaging, may enhance small-vessel flow imaging.
Contrast agents refine these signals through backscatter or reflection of sound characterized by their chemical shape and size. Microscopic lipososomes, nanoparticle emulsions and microbubbles are examples of the contrast agents that have been used. (38)When gas containing microbubbles are injected, they are confined to the vascular space because of their size. The insonating pressure wave creates reverberations on the microbubble that are transmitted back to the receiver at harmonic frequencies that uniquely identify the microbubble as the source of the returning sound waves. This results in a very high target to background ratio. Microbubble sizes range from 1 to 4 μm (the largest imaging agent in use in humans) and the basic design is an inert gas-filled core, typically perflurocarbon, and an outer shell of albumin, lipid or biopolymers. With low ultrasound transmission frequencies, the nonlinear oscillation of microbubbles produces an acoustic signal that separates it from the background tissue. A high contrast-to-tissue background ratio results in highly sensitive detection (even one microbubble can be identified) and quantification of these signals is becoming possible. Microbubbles are administered intravenously and, once degraded, the encapsulated gas is exchanged through the lungs. They can be purposely destroyed by high-power ultrasound to facilitate repeated measurements in a single field of view. To improve their stability and residence times in circulation, polymers such as polyethylene glycol (PEG) can be attached to the microbubble surface. Microbubbles are similar in size to red blood cells and are confined intra-vascularly making them uniquely suited to assess blood flow and also target endothelial cells.
Published literature is scarce on indirect angiogenesis imaging in human studies assessing antiangiogenic therapy with ultrasound. Lassau et al showed that microbubble activity corresponds to response in metastatic renal cell carcinoma patients treated with an antiangiogenic medication. (39)Larger studies are necessary for further validation.
Microbubbles can also be labeled with molecular ligands such as antibodies or peptide binding ligands. Because the microbubble is already so large, the addition of antibodies or peptides to the surface of the microbubble does not change the pharmacokinetics, as it might with smaller carrier molecules. Molecular targeted microbubbles for angiogenesis have focused on targeting integrins and growth factor receptors with promising applications in detection and monitoring therapy response.
Nuclear Medicine/Positron Emission Tomography (PET)
The main advantage of radionuclide imaging is its potential for high specificity. Limitations of nuclear imaging include long acquisition times, increasing the potential for motion artifacts, and low spatial resolution. Future improvements in camera technology may decrease these limitations. The radiation doses are similar generally less than that of diagnostic CT.
Another imaging method that could be applied to angiogenesis is quantitative blood flow imaging using 15O water PET. (40)The major limitation of its use is the availability of the imaging agent (t1/2 = ~2min, requiring an on-site cyclotron) and subsequent complicated imaging procedure. Since 15O water is completely diffusible (i.e. freely transfers between the extra to intracellular spaces), the TACs derived from the dynamic images(analogous to DCE MR)can be fit to a 2-compartmental model. For brain imaging, the initial uptake of 15O water (k1, analogous to Ktrans in DCE MR) is used to measure flow, while for tumor and cardiac imaging, blood flow is modeled using the efflux (k2, analogous to kep in DCE MR) portion of the curve and parametric images of k1 and k2, can be made. Since the activity measured in tissues directly corresponds to the injected activity, quantitative blood flow measurements can be readily made. Like all PET imaging studies, the resolution of such studies is inferior to CT and MRI, and that, combined with its limited availability and complexity has led to limited usage.
Blood volume can be measured with 11C-carbon monoxide (CO) or C15O PET. CO binds tightly to red blood cells, which, in turn, are distributed uniformly throughout the vasculature. The volume fraction of blood in tissue can be determined by dividing the concentration within the ROI by the concentration in the blood. The measurement of CO uptake on the PET images, combined with the hematocrit ratio (estimated to be 0.85 by Grubb et al (41)permits quantitative calculation of the blood volume. Again, limited by the short half-life of the 11C positron emitter (11C~20min) these studies need to be performed near a cyclotron. An additional procedural hurdle is that the tracer is administered as a gas (CO), requiring special room ventilation due to the potential toxicities of carbon monoxide.
Myocardial perfusion imaging (MPI) has been extensively developed to study coronary artery disease in the heart. In theory, such methods can be applied to angiogenesis imaging. Routinely used cardiac perfusion agents include 201Tl chloride, 99mTc-tetrofosmin, sestamibi (Single Photon Emission Tomography (SPECT)) or 82Rb (less commonly 13N ammonia) PET/CT. Each of these have been used in tumor imaging with limited success due to their extraction from the blood and subsequent specific and non-specific cellular interactions resulting variations in background activity and distributions not distinctly representative of tumor perfusion. If an intravascular radio labeled imaging agent which does not significantly accumulate in the lungs or reticuloendothelial system where available, nuclear tumor perfusion/blood volume imaging may be more widely used.
Direct Imaging of Angiogenesis
As indirect measures of blood flow and permeability are not specific markers for angiogenesis, and may represent other processes (i.e. infection, inflammation, vascular dilatation), significant efforts are being put forth to create imaging agents which specifically image angiogenesis.
Targeted Radionuclide Imaging
As mentioned previously, the RGD binding pocket of integrins is important for downstream activation of angiogenesis. Angiogenic vessels are rich in integrins as a consequence can be targets for molecular imaging. Multiple imaging agents based on the RGD amino acid sequence motif have been successfully developed and tested in animal models of angiogenesis(42–45) and several RGD-binding PET agents have entered human clinical trials.
One such promising RGD-binding PET agent is the glycosylated cyclic pentapeptide 18F galactoRGD ([18F]galacto-RGD). [18F]galacto-RGD was developed by conjugating the RGD containing cyclic pentapeptide cyclo(–Arg–Gly–Asp–dPhe–Val–) with galactose-based sugar amino acids. PET imaging allows specific imaging of αvβ3 expression and the uptake of 18F-galacto-RGD correlates with αvβ3 expression in tumor xenografts as well as in patients. Successful human αvβ3 integrin imaging with 18F -galacto-RGD has been demonstrated in invasive ductal breast cancer and squamous cell head and neck cancer, sarcoma, melanoma, and glioblastoma. The resultant Standardized Uptake Value (SUV)and tumor to background ratios correlated with integrin immunohistochemistry (IHC)and αvβ3 expression and was shown to be high and variable in primary tumors as well as in metastases. (11, 44, 46–50) 18F - galacto-RGD has also been used to provide evidence of myocardial angiogenesis following a transmural infarction in humans.(51) While initial results are promising, its synthesis is long and complicated potentially slowing its clinical translation.
Also in clinical studies is 18F Fluciclatide ([18F]AH111585), a synthetic cyclic peptide containing the RGD tripeptide which preferentially binds with high affinity to αvβ3 integrins. Early studies have shown it to be safe and “imageable” in patients with breast cancer, with favorable dosimetry.(52)
An ongoing proof of concept study aimed at correlating the 18F Fluciclatide uptake with αvβ3 integrin levels in tumors is underway. Prelimianry data shows variable intratumoral distributions. FIGURE 3a shows a melanoma with diffuse uptake (SUVmax 6.4), while FIGURE 3b shows a metastatic melanoma focus in a different patient in which only the rim of the tumor shows uptake (SUVmax of 3.0).
FIGURE 3.
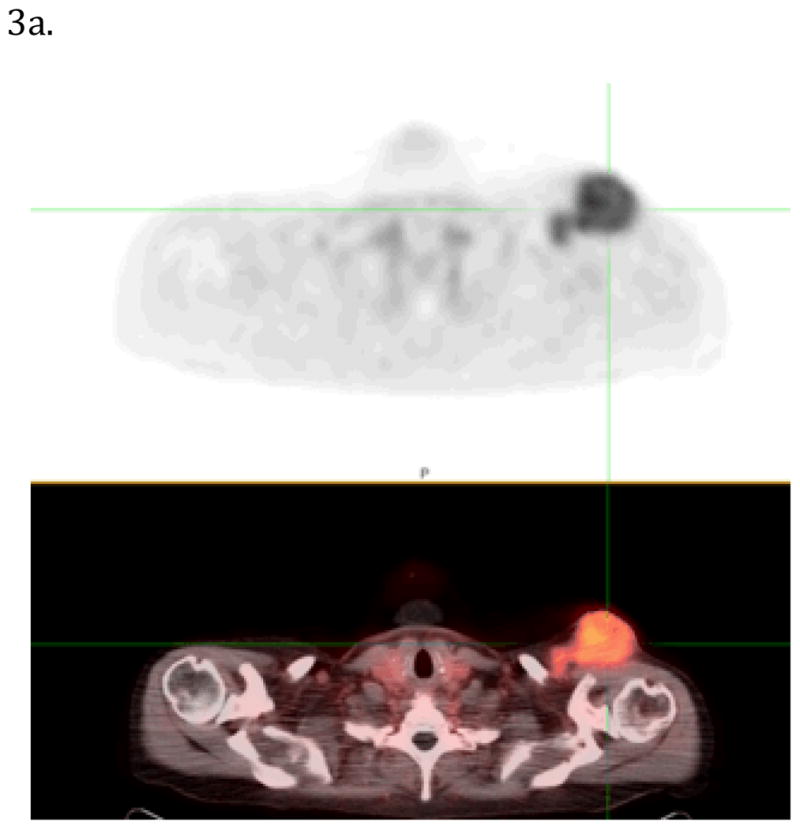
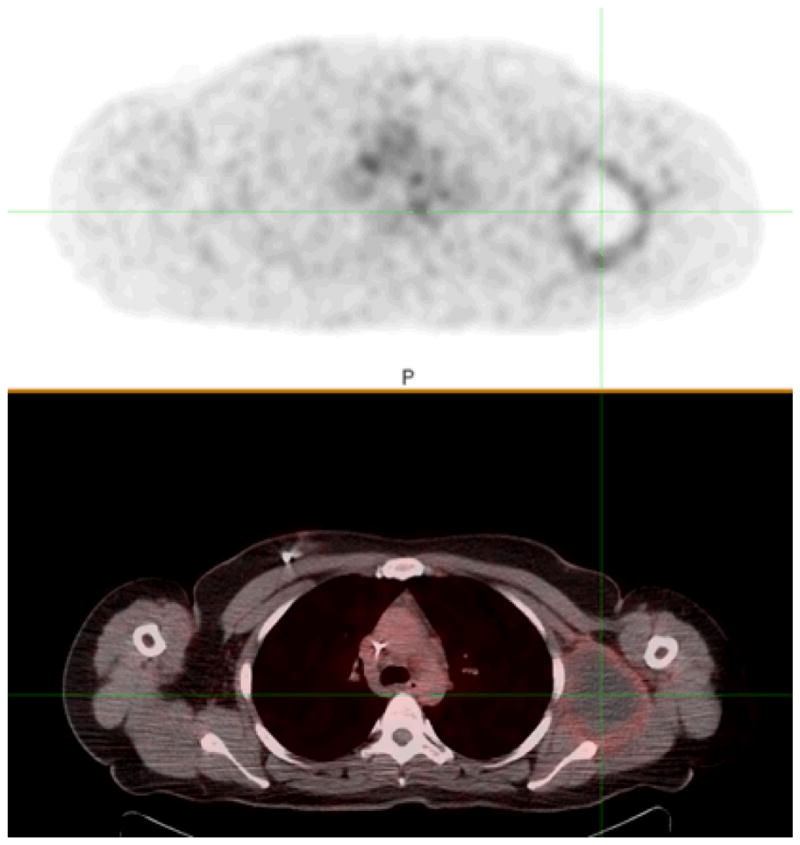
Figure 3a and 3b. Images of α4vβ3 integrin PET/CT imaging performed after the injection of 18F-Flucilatide in two patients with melanoma. In FIGURE 3a., diffuse high uptake (SUVmax 6.4) in the large soft tissue metastasis can be seen (cross hairs). The metastatic melanoma focus in Figure 3b. shows a central photon deficit and mild (SUVmax of 3.0) 18F-Flucilatide uptake around the periphery
Several other integrin targeted agents are under development with attempts to improve specificity and biodistribution to increase the tumor to background ratio. While still in the preclinical stages, 64Cu– 1,4,7,10-tetra-azacylododecane-N,N′,N″,N‴-tetraacetic acid (DOTA)–knottin (64Cu-DOTA-knottin 2.5F) is a peptide engineered for integrin binding. Binding the RGD receptor with high affinity (low nmol/L range), its low background activity may enable improved detection of lung tumors. Nielsen et. al. showed intense uptake in lung metastases in a transgenic mouse model, with tumor to background ratios ranging from 3.3 to 8.3 enabling the detection of metastastic lesions as small as 2.5 mm. (53)FIGURE 4
FIGURE 4.
A PET/CT volume rendering of a mouse thorax, imaged with 18FDG, imaging glucose metabolism (left) and 64Cu knottin 2.5F, imaging αvβ3 integrin expression(right). A lung nodule obscured by physiologic cardiac uptake on the 18FDG (right) imaged is clearly visualized in the 64Cu knottin 2.5F (left) image. Activity beneath the diaphragm represents physiology activity.
Reprinted (caption modified) from (39).
Nielsen CH, Kimura RH, Withofs N, et al. PET imaging of tumor neovascularization in a transgenic mouse model with a novel 64Cu-DOTA- knottin peptide. Cancer Res. Nov 15 2010;70(22):9022–9030.
Extensive work on the development of radiolabeled imaging agents targeting VEGF is also underway. Nuclear imaging using antibodies to VEGF has been successfully employed in preclinical models using both PET and SPECT radionuclides, including 99mTc, 111In, 89Zr, 64Cu and 86Y/90Y. Preclinical SPECT imaging with 111In VEGF121 and VEGF165 radiotracers was reported by Wagner et. el.(54) VEGF121 has also been labeled with 64Cu (t1/2 12.7 hours), a positron emitter yielding increased sensitivity and potentially quantitative monitoring of angiogenesis and VEGFR expression. MicroPET imaging with 64Cu DOTA- VEGF121 exhibited nanomolar receptor-binding affinity. In a small U87MG glioblastoma tumor with high VEGFR-2 expression, there was intense, rapid and specific uptake.(55)Willmann et. al. monitored the biological response to hindlimb ischemia with 64Cu DOTA VEGF121 in mice, and showed the angiogenic response to be greater in exercised than non-exercised mice (56)The kinetics of 64Cu-DOTA-VEGF121 uptake in a rat model of myocardial infarction was imaged by Rodriguezet al. (57)By radiolabeling the antiangiogenic drug bevacizumab with 89Zr and 111In, Nagengast et al imaged VEGF expression in mouse models(58). More recently the same group radiolabeled the anti-angiogenic drug ranibizimab, with a monoclonal antibody fragment derived from the same parent murine anti VEGF antibody and showed that sunitinib decreases89Zr-ranibizumab tumor uptake, most notably in the tumor center, with a marked rebound after discontinuation of the antiangiogenic therapeutic agent (59)
An exciting area of research involves the combination of an imaging agent with a therapeutic agent, creating a so-called “theranostic agent”. This would allow visualization of the target, quantification of the drug delivered to the target, and therapeutic monitoring all using just a single agent. The potential for a combined imaging and radiotherapy agent was reported by Nayak et al. (60)who developed the radioimmunoconjugate 86Y-CHX-A”-DTPA-bevacizumab which could serve as a surrogate imaging marker for therapeutic 90Y CHX-A”-DTPA-bevacizumab. Biodegradable integrin targeting dendritic PET nanoprobes have been developed for the noninvasive imaging of angiogenesis. Preliminary data showed them to have a 50 fold enhanced binding affinity when compared with monovalent RDG peptides. The biodegradable nature of these particles should reduce potential toxicities by promoting renal excretion, thereby reducing exposure time in the body. Its modular nature allows control of its blood circulation time and route of excretion (both highly dependent on molecule size) due to the ability to alter dendritic branching and poly ethylene glycol length, and to “switch out” the targeting moieties (i.e. target VEGF or other entity instead of integrins). It also permits attachment of a variety of radiohalogens (e.g. iodine, bromine, astatine etc.) used in both imaging and therapy. This nanoprobe could potentially have implications in both therapy and imaging. [FIGURE 5](61)
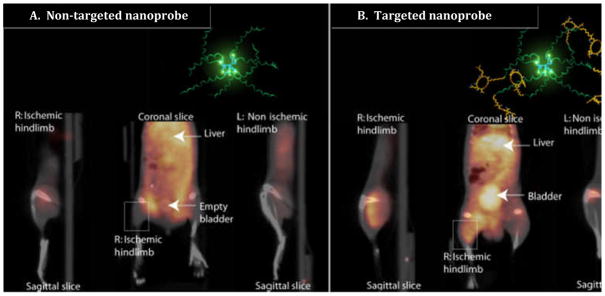
FIGURE 5.
Non-invasive PET/CT images of angiogenesis induced by hindlimb ischemia in a murine model. (A) Non-targeted dendritic nanoprobes. (B) Uptake of αvβ3 integrin targeted dendritic nanoprobes. Note accumulation of αvβ3 integrin targeted dendritic nanoprobes in the right ischemic hindlimb (box in B), when compared with the lack of uptake of the non-targeted agent (box in A). The structure and biodegradably nature of this nanoprobe may make it useful in developing a non-toxic, targeted combined therapy/imaging agent.
Reproduced with modifications, from Almutairi A, Rossin R, Shokeen M, et al. Biodegradable dendritic positron-emitting nanoprobes for the noninvasive imaging of angiogenesis. Proc Natl Acad Sci U S A. Jan 20 2009;106(3):685–690. with permission.
Targeted US
Targeted microbubbles for ultrasound, based on monoclonal antibodies and ligands such as the snake venom disintegrin, echistatin, which contains the RDG sequence, have also been used to detect integrins. Murine studies targeting tumor angiogenesis with these contrast agents have yielded strong ultrasound signals specific to new vascular growth. (62–63) Knottin is a peptide that binds to αvβ3 integrins and offers improved peptide and microbubble stability. Willmann et al demonstrated increased ultrasound signals in mouse models of human ovarian adenocarcinoma with knottin microbubbles which correlated strongly to tumor vasculature. (64)
Dual or multi-targeted microbubbles have two or more ligands specific for different angiogenic targets with the expectation that this will increase the probability for binding to new proliferative vessels. This was recently tested in human ovarian cancer xenografts in mice using microbubbles labeled with antibodies to VEGFR2 and integrin αvβ3. Increased tumor vessel attachment was noted in the dual-targeted microbubble compared to single-targeted microbubbles. (65)
VEGF specific targeting moieties can also be integrated into US contrast agents. Targeted ultrasound contrast agent scan be prepared by attaching a molecular complex to a microbubble through non-covalent bonds. These attachments can be on the polyethylene glycol (PEG)arm which can also serve as a molecular spacer. Ligand scan also be directly integrated into the microbubble shell. The biotin-streptavidin link (non-covalent) has been the most common route of attachment in animal studies, but its clinical usefulness is limited by its potential immunogenicity. Maleimide reactive groups can be added to the microbubble surface and conjugated to thiol ligands by thioether bonding, thus reducing the immunogenic response. Anderson et al linked scVEGF to microbubbles through thioether covalent bonds. Targeting the vascular endothelial growth factor receptor-2 (VEGFR-2), mouse models of colon adenocarcinoma demonstrated affinity for tumor vasculature on ultrasound.(66) Myrset et al also utilized the thiol-maleimide couplings to attach peptides to microbubbles targeting the angiogenic marker, VEGFR2 and the inflammatory marker, E-Selectin with successful results.(67)Exploring other chemical couplings of ligands such as amine (NH2)/amide attachments are additional options in developing targeted microbubbles that minimize the risk of immunogenicity. (68) Such efforts will facilitate translation into the clinical setting.
Microbubble studies examining response to anti-angiogenic therapy have shown significant changes that precede visible anatomic changes in the tumor. Kinase insert domain receptor (KDR) is a binding lipopeptide analogous to VEGFR-2 which can be directly inserted into the microbubble shell. Pysz et al. used murine models of human colon cancer treated with anti-VEGF therapy and found decreases in ultrasound signal when compared to baseline exams using KDR-targeted microbubbles. Findings were evident in mice treated with anti-angiogenic therapy as early as 24h after the start of treatment and decreased by approximately 46%.(65)There are no reports, at the time of this writing, of using molecular angiogenesis targeted imaging agents for ultrasound in patients.
Research has also focused on ultrasound contrast agents as vehicles for drug delivery. Drugs can be complexed to the lipid shell and selectively released when the contrast agent is destroyed by ultrasound signals at specific sites. Drug-loaded contrast agents have been developed for a variety of applications but the majority has focused on chemotherapeutic delivery for treatment of tumor angiogenesis. Several animal and in vitro studies have shown decreased systemic toxicity and increased potency at targeted locations. Specific to angiogenesis treatment, animal models have shown marked attenuation of tumor growth after delivery of chemotherapy by ultrasound contrast agents. (38)
Targeted MR
Attempts to measure angiogenesis directly with MR have met with limited success. Several imaging agents have been evaluated in pre-clinical models only. An approach using liposomes (diameter of 300–350 nm) containing Gd3+ and targeted using the αvβ3 specific antibody LM609 showed promise but has not been developed further.(43)
A major drawback to using MRI in this setting is its limited sensitivity (detected at millimolar levels) and it is technically challenging to label nanoparticles with large amounts of Gd. In the future, this limited sensitivity of MR might be overcome by signal amplification strategies that generate higher target to background contrast.(69) Hyperpolarized 13C MRI also holds promise for much greater sensitivity, although the hyperpolarization process is difficult to generate and suffers from a short (2–3 min)half life.)
Perspective
Angiogenesis is an integral component of tumor development and tissue remodeling. The ability to non-invasively detect and monitor this process has numerous potential clinical applications. A successful targeted imaging agent could potentially be used to identify patients who may benefit from anti- angiogenic therapies, to monitor anti-angiogenic therapy, to identify sites of high angiogenesis for focal therapies or to provide prognostic information. There are numerous clinical options for indirect measurement of angiogenesis, by measuring blood flow and perfusion as surrogates, but these parameters can be affected by processes other than angiogenesis, notably inflammation. For this reason, a more targeted approach is preferable.
As the process of angiogenesis involves a complicated dynamic interplay among numerous modulators, information about the system determined at a single time-point is not likely to be representative of the entire state of the angiogenic pathway. Targeted molecular imaging, using optical imaging agents in particular, has already shown itself to be a boon to the research efforts to better understand the process. Unfortunately, due to the significant light scattering, widespreadm clinical application is not practical. Attempts to develop similar targeted MR imaging agents have been made, with the hopes of maintaining directed specificity while improving the spatial resolution. There has been little success in the clinical translation of such imaging agents, likely attributable to the intrinsically low sensitivity of MR imaging (i.e. relatively large amounts of Gd are required to obtain an adequate signal, making the chemistry and safety of these agents challenging.)
The preclinical work using targeted ultrasound microbubbles is also promising. The ability to release a therapy payload “on demand” suggests the possibility of a combined imaging and therapeutic paradigm. Labeling microbubbles with specific targeted molecules may result in an imaging agent platform similar to that in nuclear medicine and PET; however compared to radionuclide imaging, US imaging requires a higher dose, and further safety testing will be necessary for regulatory approval.
Radionuclide imaging alone, is able to bridge the translational gap for targeted imaging, providing dynamic high sensitivity targeted information, albeit with low spatial resolution, in both the pre-clinical and clinical arenas. Several angiogenesis targeted PET imaging agents are already in clinical trials with promising results. While more safety and efficacy studies are needed, it is likely that an integrin targeted PET imaging agent will be translated to the clinic in the next decade.
While the clinical implication of modulating angiogenesis is currently uncertain, given the major role it plays in various disease states, the ability to monitor angiogenesis non-invasively over time will be a useful medical tool in the near future. Theranostic platforms currently in development offer the potential to select, properly dose and monitor patients with therapies directed at angiogenesis.
Executive Summary.
Background
As tumors increase in size, they begin to exceed the ~1 mm oxygen diffusion limit; to continue growing they must increase their blood supply
They accomplish this by increasing or developing new blood vessels: angiogenesis, a physiological process under tight control by numerous regulatory molecule and signally pathways
In the absence of angiogenesis, small tumors either become necrotic or become dormant (proliferation continues; however it is balanced by apoptosis, resulting in no net growth).
Under the appropriate conditions, an “angiogenic switch” may be thrown, resulting in increased pro-angiogenic factors and up regulation of angiogenesis. This appears to be the turning point in the tumor’s ability to be self sufficient and eventually to metastasize.
Non-invasive identification of which tumor foci have this capability could help direct therapy, provide prognostic information and provide a therapeutic opportunity. This can be done indirectly by measuring perfusion/blood flow or directly using targets imaging agents
The Players
Amongst the complicated interplay of angiogenic modulators, VEGF and integrins are the most studied as potential targeting platforms.
High αvβ3 integrin expression has been demonstrated in numerous cancer types and this expression has been correlated with disease progression in several malignancies.
Activation of the VEGF receptor results in initiation of several pro-angiogenic signaling pathways and its modulation has been shown to potentiate chemotherapy and radiotherapy effects.
Why image?
As the treatment of cancer moves towards the molecular control of cancer using targeted therapies, conventional anatomic imaging may prove insufficient.
Anti-angiogenic therapeutics targeting various steps in the angiogenesis pathway are entering the clinic with mixed response.
Angiogenic inhibitors appear to have a bi-phasic (U-shaped) dose response curve—while their effect initially increases with dose, administration of higher doses actually results in a decreasing response.(19)Optimal dose and dosing schedules could be defined if one had an accurate marker for therapeutic response.
How to Image
-
Indirect Imaging
Clinically available methods to image blood flow and perfusion using radiolabeled drugs, and contrast CT, MR and US (microbubbles).
-
Direct imaging
Targeted imaging agents (predominantly integrins and VEGF) are being developed for MR, US and Nuclear/PET imaging, most in preclinical phase.
Two promising radiotracers are in phase I/II studies in humans and at least one will likely translate to the clinic in the next decade.
The next Steps
Angiogenesis plays a key role in the establishment of life threatening tumors and non-invasive detection/monitoring of this process is essential.
Once accurate and specific targeting is established a combined therapy/diagnostic platform (Theranostic) currently in development offer the potential to select, properly dose and monitor patients with therapies directed at angiogenesis.
Contributor Information
Karen A. Kurdziel, Email: Karen.kurdziel@nih.gov.
Liza Lindenberg, Email: Liza.lindenberg@mail.nih.gov.
Peter L Choyke, Email: pchoyke@mail.nih.gov.
References
- 1.Folkman J. Tumor angiogenesis: Therapeutic implications. NEJM. 1971 November 18;282(21):1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 2.Black WC, Welch HG. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med. 1993 Apr 29;328(17):1237–1243. doi: 10.1056/NEJM199304293281706. [DOI] [PubMed] [Google Scholar]
- 3.Naumov GN, Akslen LA, Folkman J. Role of angiogenesis in human tumor dormancy: animal models of the angiogenic switch. Cell Cycle. 2006 Aug;5(16):1779–1787. doi: 10.4161/cc.5.16.3018. [DOI] [PubMed] [Google Scholar]
- 4.Folkman J. Angiogenesis. Annu Rev Med. 2006;57:1–18. doi: 10.1146/annurev.med.57.121304.131306. [DOI] [PubMed] [Google Scholar]
- 5.Udagawa T, Fernandez A, Achilles EG, Folkman J, D’Amato RJ. Persistence of microscopic human cancers in mice: alterations in the angiogenic balance accompanies loss of tumor dormancy. FASEB J. 2002 Sep;16(11):1361–1370. doi: 10.1096/fj.01-0813com. [DOI] [PubMed] [Google Scholar]
- 6.Sinusas AJ. Molecular imaging in nuclear cardiology: translating research concepts into clinical applications. Q J Nucl Med Mol Imaging. 2010 Apr;54(2):230–240. [PubMed] [Google Scholar]
- 7.Tumor angiogenesis: Basic mechanisms and cancer therapy. Berlin: Springer-Verlag Berlin; 2008. [Google Scholar]
- 8.Venkataraman G, Raman R, Sasisekharan V, Sasisekharan R. Molecular characteristics of fibroblast growth factor-fibroblast growth factor receptor-heparin-like glycosaminoglycan complex. Proc Natl Acad Sci U S A. 1999 Mar 30;96(7):3658–3663. doi: 10.1073/pnas.96.7.3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White CW, Sondheimer HM, Crouch EC, Wilson H, Fan LL. Treatment of pulmonary hemangiomatosis with recombinant interferon alfa-2a. N EnglJ Med. 1989 May 4;320(18):1197–1200. doi: 10.1056/NEJM198905043201807. [DOI] [PubMed] [Google Scholar]
- 10.Singh RK, Gutman M, Bucana CD, Sanchez R, Llansa N, Fidler IJ. Interferons alpha and beta down-regulate the expression of basic fibroblast growth factor in human carcinomas. Proc Natl Acad Sci U S A. 1995 May 9;92(10):4562–4566. doi: 10.1073/pnas.92.10.4562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beer AJ, Haubner R, Wolf I, et al. PET-based human dosimetry of 18F-galacto-RGD, a new radiotracer for imaging alpha v beta3 expression. J Nucl Med. 2006 May;47(5):763–769. [PubMed] [Google Scholar]
- 12.Smith-Jones PM, Solit D, Afroze F, Rosen N, Larson SM. Early tumor response to Hsp90 therapy using HER2 PET: comparison with 18F-FDG PET. J Nucl Med. 2006 May;47(5):793–796. [PMC free article] [PubMed] [Google Scholar]
- 13.Schwarz F, Sculean A, Romanos G, et al. Influence of different treatment approaches on the removal of early plaque biofilms and the viability of SAOS2 osteoblasts grown on titanium implants. Clin Oral Investig. 2005 Jun;9(2):111–117. doi: 10.1007/s00784-005-0305-8. [DOI] [PubMed] [Google Scholar]
- 14.Prandini MH, Denarier E, Frachet P, Uzan G, Marguerie G. Isolation of the human platelet glycoprotein IIb gene and characterization of the 5′ flanking region. Biochem Biophys Res Commun. 1988 Oct 14;156(1):595–601. doi: 10.1016/s0006-291x(88)80884-2. [DOI] [PubMed] [Google Scholar]
- 15.Cai J, Han S, Qing R, Liao D, Law B, Boulton ME. In pursuit of new anti-angiogenic therapies for cancer treatment. Front Biosci. 2011;16:803–814. doi: 10.2741/3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ignoffo RJ. Overview of bevacizumab: a new cancer therapeutic strategy targeting vascular endothelial growth factor. Am J Health Syst Pharm. 2004 Nov 1;61(21 Suppl 5):S21–26. doi: 10.1093/ajhp/61.suppl_5.S21. [DOI] [PubMed] [Google Scholar]
- 17.Batchelor TT, Sorensen AG, di Tomaso E, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007 Jan;11(1):83–95. doi: 10.1016/j.ccr.2006.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mas-Moruno C, Rechenmacher F, Kessler H. Cilengitide: the first anti-angiogenic small molecule drug candidate design, synthesis and clinical evaluation. Anticancer Agents Med Chem. 2010 Dec 1;10(10):753–768. doi: 10.2174/187152010794728639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Celik I, Surucu O, Dietz C, et al. Therapeutic efficacy of endostatin exhibits a biphasic dose-response curve. Cancer Res. 2005 Dec 1;65(23):11044–11050. doi: 10.1158/0008-5472.CAN-05-2617. [DOI] [PubMed] [Google Scholar]
- 20.Kerbel RS, Yu J, Tran J, et al. Possible mechanisms of acquired resistance to anti-angiogenic drugs: implications for the use of combination therapy approaches. Cancer Metastasis Rev. 2001;20(1–2):79–86. doi: 10.1023/a:1013172910858. [DOI] [PubMed] [Google Scholar]
- 21.Sourbron S. Technical aspects of MR perfusion. Eur J Radiol. 2010 Dec;76(3):304–313. doi: 10.1016/j.ejrad.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 22.Turkbey B, Shah VP, Pang Y, et al. Is Apparent Diffusion Coefficient Associated with Clinical Risk Scores for Prostate Cancers that Are Visible on 3-T MR Images? Radiology. 2011 Feb;258(2):488–495. doi: 10.1148/radiol.10100667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendichovszky IA, Cutajar M, Gordon I. Reproducibility of the aortic input function (AIF) derived from dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) of the kidneys in a volunteer study. Eur J Radiol. 2009 Sep;71(3):576–581. doi: 10.1016/j.ejrad.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 24.Cutajar M, Mendichovszky IA, Tofts PS, Gordon I. The importance of AIF ROI selection in DCE-MRI renography: reproducibility and variability of renal perfusion and filtration. Eur J Radiol. 2010 Jun;74(3):e154–160. doi: 10.1016/j.ejrad.2009.05.041. [DOI] [PubMed] [Google Scholar]
- 25.Kummar S, Gutierrez ME, Chen A, et al. Phase I trial of vandetanib and bevacizumab evaluating the VEGF and EGF signal transduction pathways in adults with solid tumours and lymphomas. Eur J Cancer. 2011 Jan 17; doi: 10.1016/j.ejca.2010.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hayes DF. Bevacizumab treatment for solid tumors: boon or bust? JAMA. 2011 Feb 2;305(5):506–508. doi: 10.1001/jama.2011.57. [DOI] [PubMed] [Google Scholar]
- 27.Ranpura V, Hapani S, Wu S. Treatment-related mortality with bevacizumab in cancer patients: a meta-analysis. JAMA. 2011 Feb 2;305(5):487–494. doi: 10.1001/jama.2011.51. [DOI] [PubMed] [Google Scholar]
- 28.Padhani AR, Leach MO. Antivascular cancer treatments: functional assessments by dynamic contrast-enhanced magnetic resonance imaging. Abdom Imaging. 2005 May-Jun;30(3):324–341. doi: 10.1007/s00261-004-0265-5. [DOI] [PubMed] [Google Scholar]
- 29.Zweifel M, Padhani AR. Perfusion MRI in the early clinical development of antivascular drugs: decorations or decision making tools? Eur J Nucl Med Mol Imaging. 2010 Aug;37( Suppl 1):S164–182. doi: 10.1007/s00259-010-1451-z. [DOI] [PubMed] [Google Scholar]
- 30.Ferrara N. VEGF: an update on biological and therapeutic aspects. Curr Opin Biotechnol. 2000 Dec;11(6):617–624. doi: 10.1016/s0958-1669(00)00153-1. [DOI] [PubMed] [Google Scholar]
- 31.Pinter SZ, Lacefield JC. Detectability of small blood vessels with high-frequency power Doppler and selection of wall filter cut-off velocity for microvascular imaging. Ultrasound Med Biol. 2009 Jul;35(7):1217–1228. doi: 10.1016/j.ultrasmedbio.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 32.Martinoli C, Pretolesi F, Crespi G, et al. Power Doppler sonography: clinical applications. Eur J Radiol. 1998 May;27( Suppl 2):S133–140. doi: 10.1016/s0720-048x(98)00054-0. [DOI] [PubMed] [Google Scholar]
- 33.Chen CN, Cheng YM, Liang JT, et al. Color Doppler vascularity index can predict distant metastasis and survival in colon cancer patients. Cancer Res. 2000 Jun 1;60(11):2892–2897. [PubMed] [Google Scholar]
- 34.Chen CN, Lin JJ, Lee H, et al. Association between color doppler vascularity index, angiogenesis-related molecules, and clinical outcomes in gastric cancer. J Surg Oncol. 2009 Jun 1;99(7):402–408. doi: 10.1002/jso.21193. [DOI] [PubMed] [Google Scholar]
- 35.Zhou Q, Lei XY, Xie Q, Cardoza JD. Sonographic and Doppler imaging in the diagnosis and treatment of gestational trophoblastic disease: a 12-year experience. J Ultrasound Med. 2005 Jan;24(1):15–24. doi: 10.7863/jum.2005.24.1.15. [DOI] [PubMed] [Google Scholar]
- 36.Cosgrove D, Lassau N. Imaging of perfusion using ultrasound. Eur J Nucl Med Mol Imaging. 2010 Aug;37( Suppl 1):S65–85. doi: 10.1007/s00259-010-1537-7. [DOI] [PubMed] [Google Scholar]
- 37.Magnon C, Galaup A, Rouffiac V, et al. Dynamic assessment of antiangiogenic therapy by monitoring both tumoral vascularization and tissue degeneration. Gene Ther. 2007 Jan;14(2):108–117. doi: 10.1038/sj.gt.3302849. [DOI] [PubMed] [Google Scholar]
- 38.Eisenbrey JR, Forsberg F. Contrast-enhanced ultrasound for molecular imaging of angiogenesis. Eur J Nucl Med Mol Imaging. 2010 Aug;37( Suppl 1):S138–146. doi: 10.1007/s00259-010-1449-6. [DOI] [PubMed] [Google Scholar]
- 39.Lassau N, Koscielny S, Albiges L, et al. Metastatic renal cell carcinoma treated with sunitinib: early evaluation of treatment response using dynamic contrast-enhanced ultrasonography. Clin Cancer Res. 2010 Feb 15;16(4):1216–1225. doi: 10.1158/1078-0432.CCR-09-2175. [DOI] [PubMed] [Google Scholar]
- 40.Kety SS. Observations on the validity of a two compartmental model of the cerebral circulation. Acta Neurol Scand Suppl. 1965;14:85–87. doi: 10.1111/j.1600-0404.1965.tb01961.x. [DOI] [PubMed] [Google Scholar]
- 41.Grubb RL, Jr, Phelps ME, Ter-Pogossian MM. Regional cerebral blood volume in humans. X-ray fluorescence studies. Arch Neurol. 1973 Jan;28(1):38–44. doi: 10.1001/archneur.1973.00490190056006. [DOI] [PubMed] [Google Scholar]
- 42.Line BR, Mitra A, Nan A, Ghandehari H. Targeting tumor angiogenesis: comparison of peptide and polymer-peptide conjugates. J Nucl Med. 2005 Sep;46(9):1552–1560. [PubMed] [Google Scholar]
- 43.Sipkins DA, Cheresh DA, Kazemi MR, Nevin LM, Bednarski MD, Li KC. Detection of tumor angiogenesis in vivo by alphaVbeta3-targeted magnetic resonance imaging. Nat Med. 1998 May;4(5):623–626. doi: 10.1038/nm0598-623. [DOI] [PubMed] [Google Scholar]
- 44.Haubner R, Wester HJ, Burkhart F, et al. Glycosylated RGD-containing peptides: tracer for tumor targeting and angiogenesis imaging with improved biokinetics. J Nucl Med. 2001 Feb;42(2):326–336. [PubMed] [Google Scholar]
- 45.Haubner R, Wester HJ, Weber WA, et al. Noninvasive imaging of alpha(v)beta3 integrin expression using 18F-labeled RGD-containing glycopeptide and positron emission tomography. Cancer Res. 2001 Mar 1;61(5):1781–1785. [PubMed] [Google Scholar]
- 46.Beer AJ, Niemeyer M, Carlsen J, et al. Patterns of alphavbeta3 expression in primary and metastatic human breast cancer as shown by 18F-Galacto-RGD PET. J Nucl Med. 2008 Feb;49(2):255–259. doi: 10.2967/jnumed.107.045526. [DOI] [PubMed] [Google Scholar]
- 47.Beer AJ, Haubner R, Goebel M, et al. Biodistribution and pharmacokinetics of the alphavbeta3-selective tracer 18F-galacto-RGD in cancer patients. J Nucl Med. 2005 Aug;46(8):1333–1341. [PubMed] [Google Scholar]
- 48.Beer AJ, Haubner R, Sarbia M, et al. Positron emission tomography using [18F]Galacto-RGD identifies the level of integrin alpha(v)beta3 expression in man. Clin Cancer Res. 2006 Jul 1;12(13):3942–3949. doi: 10.1158/1078-0432.CCR-06-0266. [DOI] [PubMed] [Google Scholar]
- 49.Haubner R, Kuhnast B, Mang C, et al. [18F]Galacto-RGD: synthesis, radiolabeling, metabolic stability, and radiation dose estimates. Bioconjug Chem. 2004 Jan-Feb;15(1):61–69. doi: 10.1021/bc034170n. [DOI] [PubMed] [Google Scholar]
- 50.Haubner R. Alphavbeta3-integrin imaging: a new approach to characterise angiogenesis? Eur J Nucl Med Mol Imaging. 2006 Jul;33( Suppl 1):54–63. doi: 10.1007/s00259-006-0136-0. [DOI] [PubMed] [Google Scholar]
- 51.Makowski MR, Ebersberger U, Nekolla S, Schwaiger M. In vivo molecular imaging of angiogenesis, targeting alphavbeta3 integrin expression, in a patient after acute myocardial infarction. Eur Heart J. 2008 Sep;29(18):2201. doi: 10.1093/eurheartj/ehn129. [DOI] [PubMed] [Google Scholar]
- 52.Kenny LM, Coombes RC, Oulie I, et al. Phase I trial of the positron-emitting Arg-Gly-Asp (RGD) peptide radiolig and 18F-AH111585 in breast cancer patients. J Nucl Med. 2008 Jun;49(6):879–886. doi: 10.2967/jnumed.107.049452. [DOI] [PubMed] [Google Scholar]
- 53.Nielsen CH, Kimura RH, Withofs N, et al. PET imaging of tumor neovascularization in a transgenic mouse model with a novel 64Cu-DOTA-knottin peptide. Cancer Res. 2010 Nov 15;70(22):9022–9030. doi: 10.1158/0008-5472.CAN-10-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wagner S, Fueller T, Hummel V, Rieckmann P, Tonn JC. Influence of VEGF-R2 inhibition on MMP secretion and motility of microvascular human cerebral endothelial cells (HCEC) J Neurooncol. 2003 May;62(3):221–231. doi: 10.1023/a:1023335732264. [DOI] [PubMed] [Google Scholar]
- 55.Cai W, Chen K, Mohamedali KA, et al. PET of vascular endothelial growth factor receptor expression. J Nucl Med. 2006 Dec;47(12):2048–2056. [PubMed] [Google Scholar]
- 56.Willmann JK, Chen K, Wang H, et al. Monitoring of the biological response to murine hindlimb ischemia with 64Cu-labeled vascular endothelial growth factor-121 positron emission tomography. Circulation. 2008 Feb 19;117(7):915–922. doi: 10.1161/CIRCULATIONAHA.107.733220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodriguez-Porcel M, Cai W, Gheysens O, et al. Imaging of VEGF receptor in a rat myocardial infarction model using PET. J Nucl Med. 2008 Apr;49(4):667–673. doi: 10.2967/jnumed.107.040576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nagengast WB, de Korte MA, Oude Munnink TH, et al. 89Zr-bevacizumab PET of early antiangiogenic tumor response to treatment with HSP90 inhibitor NVP-AUY922. J Nucl Med. 2010 May;51(5):761–767. doi: 10.2967/jnumed.109.071043. [DOI] [PubMed] [Google Scholar]
- 59.Nagengast WB, Lub-de Hooge MN, Oosting SF, et al. VEGF-PET imaging is a noninvasive biomarker showing differential changes in the tumor during sunitinib treatment. Cancer Res. 2011 Jan 1;71(1):143–153. doi: 10.1158/0008-5472.CAN-10-1088. [DOI] [PubMed] [Google Scholar]
- 60.Nayak TK, Garmestani K, Baidoo KE, Milenic DE, Brechbiel MW. PET imaging of tumor angiogenesis in mice with VEGF-A-targeted (86)Y-CHX-A″-DTPA-bevacizumab. Int J Cancer. 2011 Feb 15;128(4):920–926. doi: 10.1002/ijc.25409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Almutairi A, Rossin R, Shokeen M, et al. Biodegradable dendritic positron-emitting nanoprobes for the noninvasive imaging of angiogenesis. Proc Natl Acad Sci U S A. 2009 Jan 20;106(3):685–690. doi: 10.1073/pnas.0811757106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ellegala DB, Poi HL, Carpenter JE, et al. Imaging tumor angiogenesis with contrast ultrasound and microbubbles targeted to alpha(v)beta(3) Circulation. 2003 Jul 22;108(3):336–341. doi: 10.1161/01.CIR.0000080326.15367.0C. [DOI] [PubMed] [Google Scholar]
- 63.Xie F, Lof J, Matsunaga T, Zutshi R, Porter TR. Diagnostic ultrasound combined with glycoprotein IIb/IIIa-targeted microbubbles improves microvascular recovery after acute coronary thrombotic occlusions. Circulation. 2009 Mar 17;119(10):1378–1385. doi: 10.1161/CIRCULATIONAHA.108.825067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Willmann JK, Kimura RH, Deshpande N, Lutz AM, Cochran JR, Gambhir SS. Targeted contrast-enhanced ultrasound imaging of tumor angiogenesis with contrast microbubbles conjugated to integrin-binding knottin peptides. J Nucl Med. 2010 Mar;51(3):433–440. doi: 10.2967/jnumed.109.068007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pysz MA, Foygel K, Rosenberg J, Gambhir SS, Schneider M, Willmann JK. Antiangiogenic cancer therapy: monitoring with molecular US and a clinically translatable contrast agent (BR55) Radiology. 2010 Aug;256(2):519–527. doi: 10.1148/radiol.10091858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Anderson CR, Rychak JJ, Backer M, Backer J, Ley K, Klibanov AL. scVEGF microbubble ultrasound contrast agents: a novel probe for ultrasound molecular imaging of tumor angiogenesis. Invest Radiol. 2010 Oct;45(10):579–585. doi: 10.1097/RLI.0b013e3181efd581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Myrset AH, Fjerdingstad HB, Bendiksen R, et al. Design and characterization of targeted ultrasound microbubbles for diagnostic use. Ultrasound Med Biol. 2011 Jan;37(1):136–150. doi: 10.1016/j.ultrasmedbio.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 68.Deshpande N, Pysz MA, Willmann JK. Molecular ultrasound assessment of tumor angiogenesis. Angiogenesis. 2010 Jun;13(2):175–188. doi: 10.1007/s10456-010-9175-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Spuentrup E, Botnar RM. Coronary magnetic resonance imaging: visualization of the vessel lumen and the vessel wall and molecular imaging of arteriothrombosis. Eur Radiol. 2006 Jan;16(1):1–14. doi: 10.1007/s00330-005-2886-7. [DOI] [PubMed] [Google Scholar]