Abstract
Autoimmune pancreatitis (AIP) is a rare form of pancreatitis characterized by prominent lymphocyte infiltration and pancreatic fibrosis resulting in organ dysfunction. The pathogenesis and pathology of AIP remain unknown. A 64-year-old Chinese man presented with symptoms and signs of bile duct obstruction diffuse enlargement of the head of pancreas, elevated IgG levels, and negative autoimmune antibody responses. A pylorus-preserving pancreatoduodenectomy was performed and a pancreatic tumor was suspected. However, periductal lymphoplasmacytic infiltration and fibrosis were found in the head of pancreas and nearby organs instead of tumor cells. Four months after surgery, the patient was readmitted because of reoccurrence of severe jaundice and sustained abdominal distension. Prednisone 30 mg/d was administered orally as an AIP was suspected. One and a half months later, the symptoms of the patient disappeared, and globulin, aminotransferase and bilirubin levels decreased significantly. Over a 9-mo follow-up period, the dose of prednisone was gradually decreased to 10 mg/d and the patient remained in good condition. We further demonstrated dominant CD3+/CD8+ populations, CD20+ cells and a few CD4+ cells in the pancreatic parenchyma, duodenum and gallbladder wall by immunohistochemical assay. This AIP case presented with significant CD8+ T lymphocyte infiltration in the pancreas and extra-pancreatic lesions, indicating that this cell population may be more important in mediating AIP pathogenesis than previously known and that AIP might be a poorly defined autoimmune disease with heterogeneous pathogenesis.
Keywords: Autoimmune pancreatitis, Pancreas, Prednisone, CD8+ T and CD4+ T lymphocytes, CD20, Inflammatory cell, Infiltration
INTRODUCTION
Autoimmune pancreatitis (AIP) is a rare form of pancreatitis characterized by prominent lymphocyte infiltration and pancreatic fibrosis resulting in organ dysfunction[1]. This disease has been mainly reported in Japan and Europe with an estimated incidence of 4%-6% among chronic pancreatitis patients[2,3]. In China, only a few AIP cases have been reported even though approximately 5% of chronic pancreatitis cases resulted from autoimmune-associated responses[4]. To date, the pathogenesis and pathology of AIP remain undefined. Previously, CD4+ T lymphocytes were thought to be critical (relative to CD8+ T lymphocytes) in mediating AIP pathogenesis[5-7]. However, the case of AIP described herein demonstrated a significant CD8+ infiltration and an absence of CD4+ T lymphocytes in the pancreas and surrounding organs, including the duodenum.
CASE REPORT
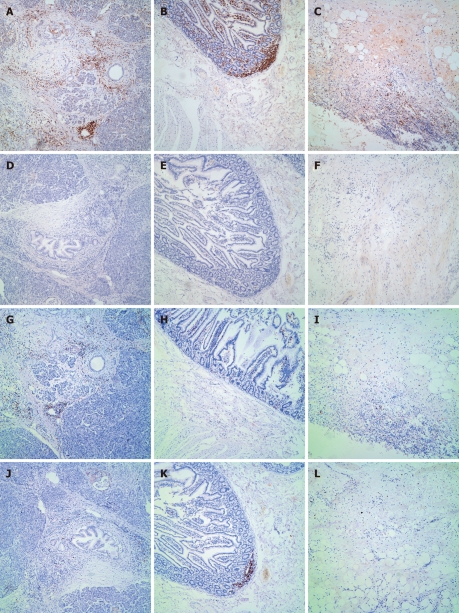
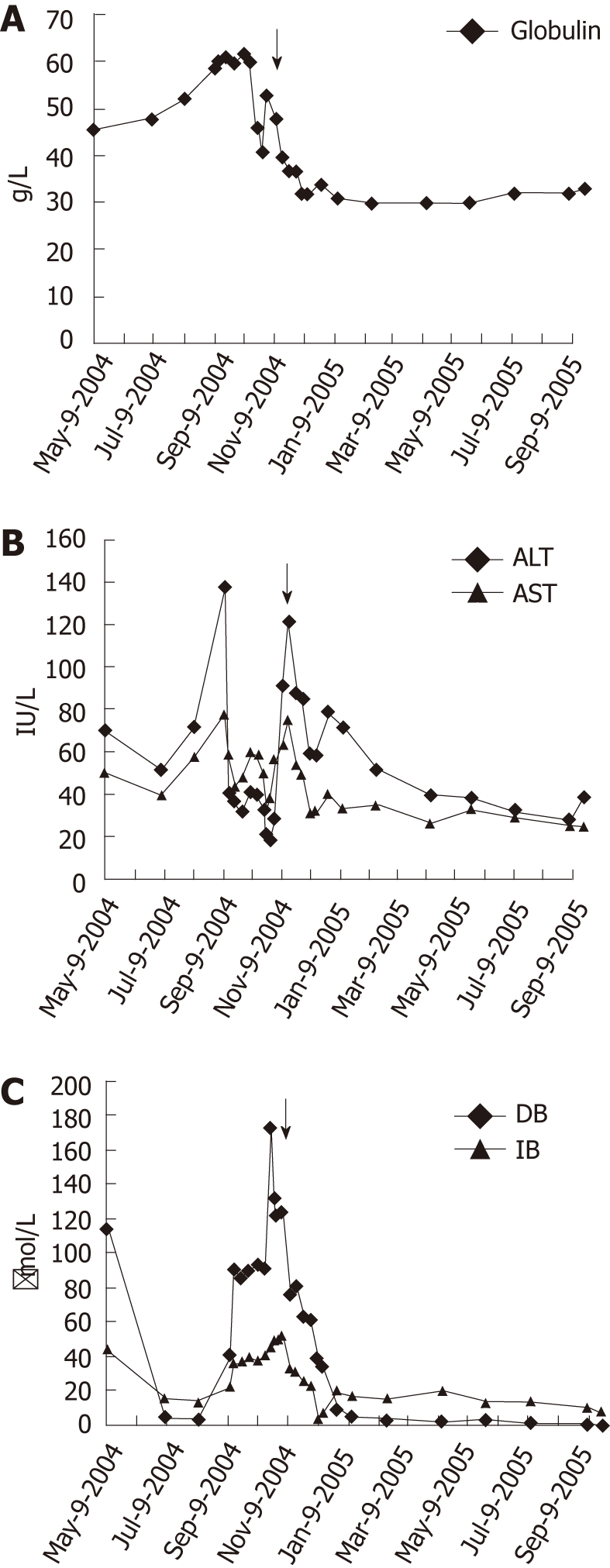
A 64-year-old Chinese man was admitted to the West China Hospital on May 8, 2004 with a history of 1-mo abdominal distension and 3-d jaundice. He was examined with blood biochemical tests, including direct bilirubin (DB, 114.71 μmol/L), indirect bilirubin (IB, 44.9 μmol/L), alanine amino transferase (ALT, 70 IU/L), aspartate amino transferase (AST, 51 IU/L), globulin (45.8 g/L) and fasting plasma glucose (FPG, 6.1 mmol/L) (Figure 1). Computed tomography (CT) showed a 3 cm × 3 cm mass at the head of the pancreas suspected to be a pancreatic tumor. Therefore, a pylorus-preserving pancreatoduodenectomy was performed on May 11 and a 3 cm × 3 cm mass was identified at the head of the sclerified pancreas, with cholestatic changes in the liver and gallbladder hydrop with dilation of the common bile duct (1.5-2 cm; the normal range is 0.3-0.8 cm). Pathological examination showed chronic inflammation with fibrosis in the pancreatic and common bile ducts as well as moderate to severe epithelial dysplasia (Figure 2). Adenoepithelial hyperplasia but not tumor cells were found in the pancreatic parenchyma. The patient was discharged 2 wk after surgery when jaundice symptoms abated.
Figure 1.
Blood biochemical analyses. Pre- and post-prednisone treatment levels of (A) immunoglobulin, (B) aminotransferase and (C) bilirubin. The black arrow indicates the start of prednisone treatment. ALT: Alanine amino transferase; AST: Aspartate amino transferase; DB: Direct bilirubin; IB: Indirect bilirubin.
Figure 2.
Characterization of pathological changes. The head of the pancreas was examined following Hematoxylin and eosin staining, demonstrating (A) pancreatic ductal atrophy and lymphocytic infiltration with fibrotic proliferation and (B) periductal infiltration of lymphocytes.
Four months later on September 13, 2004, the patient was readmitted to the West China Hospital due to a recurrence of severe jaundice and sustained abdominal distension. No obvious abnormal findings were identified following physical examination other than jaundice in the skin and sclera. Blood biochemical results (Figure 1) demonstrated the levels of DB at 91.5 μmol/L, IB at 37.7 μmol/L, ALT at 41 IU/L, AST at 59 IU/L, globulin at 60.4 g/L, FPG at 4.3 mmol/L, immunoglobulin gamma (IgG) at 47.2 g/L, IgA > 3000 mg/L and C-reactive protein at 14.3 mg/L. Detections of anti-nuclear antibodies, anti-double strand DNA antibodies (anti-ds-DNA), anti-Smith antibodies, anti-Sjogren syndrome A antibodies, anti-Sjogren syndrome B antibodies, anti-Jo-1 antibodies, anti-mitochondrial M2 antibodies, anti-liver-kidney microsome antibodies, anti-liver cytosol antibody type 1 and anti-soluble liver antigen antibodies were all negative. Magnetic resonance cholangiopancreatography showed a dilated intrahepatic biliary duct and a thickened and asperous wall of the common bile duct.
Based on the hypergammaglobulinemia and elevated IgG levels observed, this patient was suspected to have pancreatitis of autoimmune origin. Prednisone 30 mg/d was administered orally beginning on November 2, 2005. One and a half months later, the patient was discharged from the hospital after the jaundice and abdominal distension disappeared and the globulin (Figure 1A), aminotransferase (Figure 1B) and bilirubin (Figure 1C) levels decreased significantly. Over a 9-mo follow-up period, the dose of prednisone was gradually decreased to 10 mg/d and the patient remained in good condition without the presentation of either jaundice or abdominal distention and his globulin (Figure 1A), aminotransferase (Figure 1B) and bilirubin (Figure 1C) levels were within the normal range.
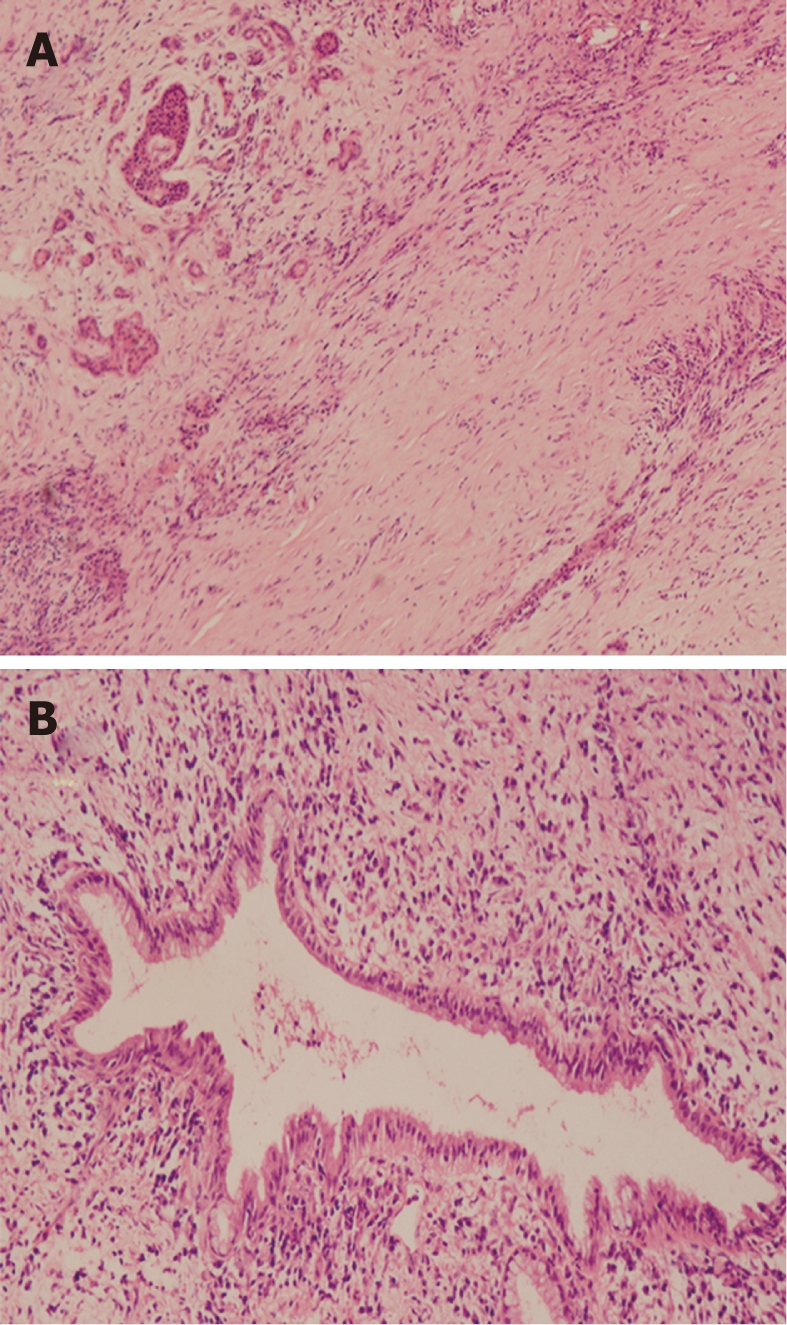
To further characterize the pathogenesis of AIP in this case, histopathologic and immunohistochemical analyses were carried out to determine the CD3, CD4, CD8 and CD20 positive profiles in paraffin sections taken from the head of the pancreas, duodenum and gallbladder. Hematoxylin and eosin staining of the head of pancreas showed ductal atrophy and periductal lymphocytic infiltration with fibrotic proliferation (Figure 2), and high levels of CD3+ cells were identified in the periductal region of the head of the pancreas (Figure 3A), duodenal villi (Figure 3B) and the gallbladder wall (Figure 3C). Interestingly, CD4+ cells were present at low levels in the specimens from the head of the pancreas (Figure 3D), duodenum (Figure 3E) and the gallbladder wall (Figure 3F). Parallel to the CD3 expression levels, CD8+ cells were detected at high levels in the periductal region of the head of the pancreas (Figure 3G), duodenal villi (Figure 3H) and the gallbladder wall (Figure 3I). The CD20 was expressed at low levels in the periductal region of the head of the pancreas (Figure 3J) and focally expressed in the duodenal villi (Figure 3K). No CD20 expression was detected in the gallbladder wall (Figure 3L).
Figure 3.
Immunohistochemical characterization. The head of the pancreas, duodenum and the wall of the gallbladder were examined for the presence of CD3+, CD4+, CD8+ and CD20+ cells; magnification × 100. A: CD3+ lymphocyte infiltration in the periductal region of the head of the pancreas; B: CD3+ lymphocyte infiltration and their focal concentration in duodenal villi; C: CD3+ lymphocyte infiltration in the wall of the gallbladder; D: CD4+ lymphocytes infiltration in the head of the pancreas; E: CD4+ lymphocyte infiltration in the duodenum; F: CD4+ lymphocyte infiltration in the gallbladder; G: CD8+ lymphocyte infiltration in the periductal region of the head of the pancreas; H: CD8+ lymphocyte infiltration in the duodenal villi; I: CD8+ lymphocyte infiltration in the wall of the gallbladder; J: CD20+ lymphocyte infiltration in the periductal region of the head of the pancreas; K: Focal CD20+ lymphocyte infiltration in duodenal villi; L: CD20+ lymphocyte infiltration in the wall of the gallbladder.
DISCUSSION
AIP, also described as chronic pancreatitis of autoimmune origin, is clinically similar in presentation to pancreatic carcinoma. AIP patients may undergo pancreatoduodenectomy as a consequence of treatment. It is reported that 2.5%-11% of the patients diagnosed with pancreatic malignancy actually had a benign pancreatic disorder confirmed by pathological examination after surgery[7] and 9.9% of the patients underwent pancreatoduodenectomy following a diagnosis of pancreatitis, 38% of them were reported to be caused by autoimmune responses[8,9].
AIP is characterized by an irregular narrowing of the main pancreatic duct, massive lymphoplasmacytic inflammation of the pancreatic parenchyma, hypergammaglobulinemia and a fair response to glucocorticoid treatment[10]. The case presented in this report was mainly characterized by symptoms and signs of bile duct obstruction, diffuse enlargement of the head of pancreas, elevated IgG levels, negative autoimmune antibody responses and periductal lymphoplasmacytic infiltration and fibrosis. After a strict treatment regimen of prednisone, the patient recovered quickly and his globulin, aminotransferase, and bilirubin levels returned to normal for more than half a year. In our case, AIP was diagnosed based on the criteria established by the Japan Pancreas Society [2,11].
AIP presentation has recently been divided into either subtype type 1 or 2[12-14]. In Asia, type 1 AIP presents at a higher frequency and is also referred to as lymphoplasmacytic sclerosing pancreatitis or AIP without granulocyte epithelial lesions (GELs). Type 2 AIP is referred to as idiopathic duct-centric pancreatitis or AIP with GELs. The case presented here with periductal lymphoplasmacytic infiltration (without granulocytes), fibrotic proliferation and pancreatic ductal atrophy is consistent with the histopathological features of type 1 AIP [13,15,16].
It was previously reported that infiltrating cells in AIP cases predominantly consisted of CD4+ T lymphocytes with few detectable CD8+ T lymphocytes and B lymphocytes[2,7]. T helper imbalance (Th1 vs Th2) is believed to be associated with the initiation of AIP[17] and elevated Th1 responses were reported in both pancreatic and extra-pancreatic lesions in AIP patients[18,19]. CD4+CD25+ regulatory T lymphocytes have also been demonstrated to contribute significantly to the pathology of AIP-associated lesions compared to lesions resulting from other pancreatic disorders[6,19]. In animal AIP disease models, administration of amylase-sensitized CD4+ T lymphocytes elicited autoimmune pancreatitis, suggesting that CD4+ T lymphocytes may be the most important components in mediating disease pathogenesis[20]. This observation is supported by the cases presenting with a reduced number of infiltrating CD4+ T lymphocytes in AIP lesions.
In contrast, our case presented with infiltrating CD8+ T (primarily cytotoxic T lymphocytes) instead of CD4+ T lymphocytes in both pancreatic and extra-pancreatic lesions. Since CD4+ T helper lymphocyte is believe to be indispensable in mediating various types of immune responses, we hypothesize that CD4+ T lymphocytes may have originally infiltrated these tissues and then recruited more CD8+ T lymphocytes functioning as effector cells of AIP pathogenesis. These data demonstrated that the presence of CD8+ T lymphocytes in AIP lesions may be more important than previously thought and that elicitation of AIP may have heterogeneous origins. A limitation in these observations is that they have only been reported in a single case, more investigations about the role of CD8+ T lymphocytes are required to further understand the pathogenesis of AIP.
In summary, we identified a significant number of CD8+ T lymphocytes infiltrating in both pancreatic and extra-pancreatic AIP lesions, instead of CD4+ T lymphocytes as commonly expected. It suggests that AIP might possess heterogeneous autoimmune origins.
ACKNOWLEDGMENTS
We want to thank the pathologists from the Department of Pathology, West China Hospital, Sichuan University, for their hard work in the immunohistochemistry. We also thank the physicians and surgeons from West China Hospital, Sichuan University for taking care of the patients and helping collect the data.
Footnotes
Supported by The National Basic Research Program of China No. 81072477 and No. 81072477; and Scientific and Technical Supporting Program of Sichuan Province, No. 2011SZ0124
Peer reviewers: Basil Ammori, MD, Department of Surgery, Salford Royal Hospital, Stott Lane, Salford, Greater Manchester, M6 8HD, United Kingdom; Dr. Thiruvengadam Muniraj, MBBS, MD, PhD, MRCP (UK), University of Pittsburgh Medical Center, 100 Chatham Park Drive, Apt 511, Pittsburgh, PA 15220, United States
S- Editor Tian L L- Editor Ma JY E- Editor Xiong L
References
- 1.Finkelberg DL, Sahani D, Deshpande V, Brugge WR. Autoimmune pancreatitis. N Engl J Med. 2006;355:2670–2676. doi: 10.1056/NEJMra061200. [DOI] [PubMed] [Google Scholar]
- 2.Kim KP, Kim MH, Song MH, Lee SS, Seo DW, Lee SK. Autoimmune chronic pancreatitis. Am J Gastroenterol. 2004;99:1605–1616. doi: 10.1111/j.1572-0241.2004.30336.x. [DOI] [PubMed] [Google Scholar]
- 3.Kamisawa T, Kim MH, Liao WC, Liu Q, Balakrishnan V, Okazaki K, Shimosegawa T, Chung JB, Lee KT, Wang HP, et al. Clinical characteristics of 327 Asian patients with autoimmune pancreatitis based on Asian diagnostic criteria. Pancreas. 2011;40:200–205. doi: 10.1097/mpa.0b013e3181fab696. [DOI] [PubMed] [Google Scholar]
- 4.Goliński P, Grabarkiewicz-Szczesna J, Chelkowski J, Hult K, Kostecki M. Possible sources of ochratoxin A in human blood in Poland. IARC Sci Publ. 1991;(115):153–158. [PubMed] [Google Scholar]
- 5.Zandieh I, Byrne MF. Autoimmune pancreatitis: a review. World J Gastroenterol. 2007;13:6327–6332. doi: 10.3748/wjg.v13.i47.6327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okazaki K, Uchida K, Miyoshi H, Ikeura T, Takaoka M, Nishio A. Recent concepts of autoimmune pancreatitis and IgG4-related disease. Clin Rev Allergy Immunol. 2011;41:126–138. doi: 10.1007/s12016-010-8214-2. [DOI] [PubMed] [Google Scholar]
- 7.Klöppel G, Lüttges J, Löhr M, Zamboni G, Longnecker D. Autoimmune pancreatitis: pathological, clinical, and immunological features. Pancreas. 2003;27:14–19. doi: 10.1097/00006676-200307000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Robison LS, Canon CL, Varadarajulu S, Eloubeidi MA, Vickers S, Mel Wilcox C. Autoimmune pancreatitis mimicking pancreatic cancer. J Hepatobiliary Pancreat Sci. 2011;18:162–169. doi: 10.1007/s00534-010-0321-1. [DOI] [PubMed] [Google Scholar]
- 9.de Castro SM, de Nes LC, Nio CY, Velseboer DC, ten Kate FJ, Busch OR, van Gulik TM, Gouma DJ. Incidence and characteristics of chronic and lymphoplasmacytic sclerosing pancreatitis in patients scheduled to undergo a pancreatoduodenectomy. HPB (Oxford) 2010;12:15–21. doi: 10.1111/j.1477-2574.2009.00112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanno A, Satoh K, Kimura K, Masamune A, Asakura T, Unno M, Matsuno S, Moriya T, Shimosegawa T. Autoimmune pancreatitis with hepatic inflammatory pseudotumor. Pancreas. 2005;31:420–423. doi: 10.1097/01.mpa.0000179732.46210.da. [DOI] [PubMed] [Google Scholar]
- 11.Kamisawa T, Okazaki K, Kawa S. Diagnostic criteria for autoimmune pancreatitis in Japan. World J Gastroenterol. 2008;14:4992–4994. doi: 10.3748/wjg.14.4992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chari ST, Kloeppel G, Zhang L, Notohara K, Lerch MM, Shimosegawa T. Histopathologic and clinical subtypes of autoimmune pancreatitis: the honolulu consensus document. Pancreatology. 2010;10:664–672. doi: 10.1159/000318809. [DOI] [PubMed] [Google Scholar]
- 13.Shimosegawa T, Chari ST, Frulloni L, Kamisawa T, Kawa S, Mino-Kenudson M, Kim MH, Klöppel G, Lerch MM, Löhr M, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40:352–358. doi: 10.1097/MPA.0b013e3182142fd2. [DOI] [PubMed] [Google Scholar]
- 14.Frulloni L, Amodio A, Katsotourchi AM, Vantini I. A practical approach to the diagnosis of autoimmune pancreatitis. World J Gastroenterol. 2011;17:2076–2079. doi: 10.3748/wjg.v17.i16.2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardacre JM, Iacobuzio-Donahue CA, Sohn TA, Abraham SC, Yeo CJ, Lillemoe KD, Choti MA, Campbell KA, Schulick RD, Hruban RH, et al. Results of pancreaticoduodenectomy for lymphoplasmacytic sclerosing pancreatitis. Ann Surg. 2003;237:853–858; discussion 853-859. doi: 10.1097/01.SLA.0000071516.54864.C1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deshpande V, Gupta R, Sainani N, Sahani DV, Virk R, Ferrone C, Khosroshahi A, Stone JH, Lauwers GY. Subclassification of autoimmune pancreatitis: a histologic classification with clinical significance. Am J Surg Pathol. 2011;35:26–35. doi: 10.1097/PAS.0b013e3182027717. [DOI] [PubMed] [Google Scholar]
- 17.Zen Y, Nakanuma Y. Pathogenesis of IgG4-related disease. Curr Opin Rheumatol. 2011;23:114–118. doi: 10.1097/BOR.0b013e3283412f4a. [DOI] [PubMed] [Google Scholar]
- 18.Okazaki K, Uchida K, Ohana M, Nakase H, Uose S, Inai M, Matsushima Y, Katamura K, Ohmori K, Chiba T. Autoimmune-related pancreatitis is associated with autoantibodies and a Th1/Th2-type cellular immune response. Gastroenterology. 2000;118:573–581. doi: 10.1016/s0016-5085(00)70264-2. [DOI] [PubMed] [Google Scholar]
- 19.Zen Y, Fujii T, Harada K, Kawano M, Yamada K, Takahira M, Nakanuma Y. Th2 and regulatory immune reactions are increased in immunoglobin G4-related sclerosing pancreatitis and cholangitis. Hepatology. 2007;45:1538–1546. doi: 10.1002/hep.21697. [DOI] [PubMed] [Google Scholar]
- 20.Kurzen CR, Beaver KW, McCluskey JA, Wecht DL. Criteria and guidelines for the evaluation of practical nursing programs. July 1991. NLN Publ. 1992;(38-2445):iii–v, 1-57. [PubMed] [Google Scholar]