Abstract
Paederus dermatitis is a peculiar, irritant contact dermatitis characterized by a sudden onset of erythematobullous lesions on exposed areas of the body. The disease is provoked by an insect belonging to the genus Paederus. This beetle does not bite or sting, but accidental brushing against or crushing the beetle over the skin provokes the release of its coelomic fluid, which contains paederin, a potent vesicant agent. This article describes this dermatitis, which occurred in three healthcare personnel aboard a medical mission boat on the Amazon River. The epidemiology and pathogenesis of paederus dermatitis is reviewed as well its treatment and prevention.
Paederus dermatitis is a peculiar, irritant contact dermatitis caused by a beetle belonging to the genus Paederus. This insect does not bite or sting, but releases a fluid containing paederin, a potent vesicant agent. If not immediately washed off, the chemical leads to a linear dermatitis composed of erythematobullous lesions.
In August 2006, the author joined 10 other medical personal on a medical mission trip to Brazil. They traveled for two weeks on a medical boat on the Amazon River, operated by the Central Brazil Mission, stopping at various villages along the river. One expects to encounter unusual tropical diseases when participating in a medical trip in an undeveloped region. However, it is unexpected to see these diseases on oneself. The following case reports describe paederus dermatitis occurring in three of the healthcare workers.
Case Reports
Case 1. A 49-year-old male dermatologist (and author of this article) first noticed an eruption on his left elbow on Day 3 of the trip. Aside from minor stinging, the area was fairly asymptomatic. Initially, the area appeared as a 6cm, linear, erythematous patch. He could not recall coming in contact with anything unusual that would cause this rash. However, he did sleep on the top deck of the boat, which was open to air. The following day, vesicles and a bulla appeared in the erythema, lasting for five days before starting to dry up and fade (Figure 1). Four months later, there still remained a linear macular area of hypopigmentation.
Figure 1.
Case 1. Linear erythematous patches with central blisters
Case 2. A 43-year-old female registered nurse started having an eruption on her left thigh on the sixth day of the trip. Her history and exam was similar as that described in Case 1; however, the erythema and blistering were more extensive and were in a stellate configuration, measuring 10cm in the longest dimension (Figure 2). After four months, there was still significant hyperpigmentation in the area.
Figure 2.
Case 2. Stellate patch of erythema with central blisters
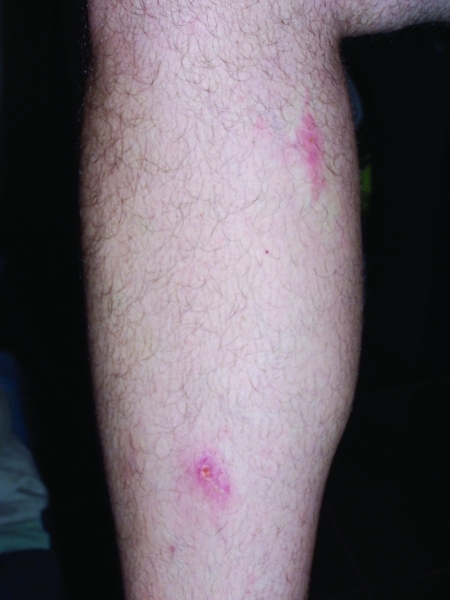
Case 3. A 37-year-old male physician assistant noticed lesions on his right lower leg eight days into the trip. His history was also similar to that described in Cases 1 and 2. However, he had two lesions, both of which were on his right lower leg, measuring 2 to 3cm. These were erythematous, linear patches with central vesicles (Figure 3). At four months, there remained some hyperpigmentation at the sites. His lesions, as well as those described in the other two cases, were shown to the crew who agreed they were caused by an insect, which is known locally as the “potó” bug.
Figure 3.
Case 3. Two small patches of erythema with erosions
Discussion
Paederus insects belong to the insect order Coleoptera (beetles) and the family Staphylinidae (rove beetles). The genus, Paederus, is quite large, with more than 600 species and a distribution in all continents except Antarctica.1 Species in South American countries are know by various names, such as bicho de fuego, pito, potó, and podó.2 Various outbreaks of dermatitis attributed to the Paederus beetle have been reported in southern Turkey,3 central Africa,4 Okinawa,5 and India.6
Adult Paederus beetles are usually 7 to 10mm long and 0.5 to 1mm wide. They have a black head, lower abdomen, and elytra (structure covering the wings) and a red thorax and upper abdomen (Figure 4). The beetles live in moist habitats and are often beneficial to agriculture because they will eat crop pests. Adults are attracted to incandescent and fluorescent lights, and as a result, inadvertently come into contact with humans. They can be especially troublesome if windows or doors are left open. This beetle does not bite or sting, but accidental brushing against it or crushing it over the skin provokes the release of its coelomic fluid, which contains paederin, a strong blistering chemical.
Figure 4.
Paederus beetle (photo courtesy of www.entomart.be)
It is important to note that Paederus beetles are not “blister beetles,” which are of the family Meloidae. Blister beetles, which also are widely distributed, release a defensive compound when threatened. The chemical released, cantharidin, a bicyclic terpenoid, is quite different from paederin, an amide.1
The manufacture of paederin is largely confined to the female insect. Recently, it has been demonstrated that the production of paederin relies on the activities of an endosymbiont (Pseudomonas species) within the beetle.7 Paederin is a potent vesicant, causing a reaction on the skin about 24 hours after contact. Different responses are seen in the skin depending upon its concentration, duration of exposure, and individual characteristics. In mild cases, there is a slight erythema lasting for a couple days. With moderate cases, the erythema evolves into vesicles and bullae over a few days, followed by a squamous stage when the blisters dry out over a week, and then a stage when they desquamate, leaving hyper- or hypopigmented patches. Scarring usually does not occur. The lesions are characteristically linear due to smearing the crushed insect across the skin. Severe cases, in addition to showing more extensive blistering, may demonstrate additional symptoms, such as fever, neuralgia, arthralgia, and vomiting.8,9
Usually, there is little discomfort from this dermatitis in mild-to-moderate exposure, unless the area becomes secondarily infected. Affected individuals may inadvertently transfer paederin to other areas of the body, such as the genitals or the face. If the periorbital area is affected, conjunctivitis may develop (referred to “Nairobi eye” in eastern Africa).9
A principle differential diagnosis to consider is phytophotodermatitis. There are many similarities to Paederus dermatitis including linear asymmetric areas of erythema, possible blister formation, and dyspigmentation. With phytophotodermatitis, however, there is a history of exposure to a light-sensitizing botanical substance, such as lime, celery, parsley, and fig. None of the three patients in this review had any exposures to these sensitizers.
Treatment initially involves removing the irritant by washing the area with soap and water. The blistered site should be treated with cool wet soaks, followed by a strong topical steroid. An interesting study was preformed in Sierra Leone with 36 patients. Half of the patients were given oral ciprofloxacin in addition to a topical steroid. Healing time was statistically faster in these patients, which suggests a concurrent bacterial infection was present, most likely from the Pseudomonas the Paederus beetle harbors.9
Preventing human/beetle contact is the primary method of avoiding Paederus dermatitis. Learning to recognize Paederus beetles and avoiding handling or crushing these insects will help decrease these eruptions. If a beetle lands on the skin, it should be blown off or encouraged to walk onto a piece of paper and then removed. The area in contact should be immediately washed with soap and water, and any clothes in contact with the beetle should be washed as well. Doors should be kept closed and window screening should be kept in good repair to help reduce entry of these insects into buildings. Since beetles are attracted to light, these should be switched off near areas where people sleep.10
Conclusion
Participating in an overseas medical mission trip has numerous benefits to both the people treated and to the healthcare providers. Although healthcare personnel are often focused on the diseases of their patients, they need to be aware of their surrounding environment, which can impact their own wellbeing. Paederus beetles are a common insect in undeveloped areas. Being aware of this beetle and the signs and treatment of its dermatitis can greatly aid a healthcare professional.
Footnotes
DISCLOSURE:The author reports no relevant conflicts of interest.
REFERENCES
- 1.Frank JH, Kanamitsu K. Paederus, Sensu Lato (Coleoptera: Staphylinidae): natural history and medical importance. J Med Entomol. 1987;24:155–191. doi: 10.1093/jmedent/24.2.155. [DOI] [PubMed] [Google Scholar]
- 2.Mullen G, Durden L. Medical and Veterinary Entomology. 2nd ed. London, UK: Academic Press; 2009. Beetles (Cloeoptera) p. 102. [Google Scholar]
- 3.Uslular C, Kavukcu H. An epidemicity of Paederus species in the Cukurova region. Cutis. 2002;69:277–279. [PubMed] [Google Scholar]
- 4.Penchenier L, Mouchet J, Cros B, et al. Invasions de Paederus sabaeus (Coleoptera : Staphylinidae) en Afrique Centrale. I. Aspects entomologiques et épidémiologiques. Bull Soc Path Ex. 1994;87:45–48. [PubMed] [Google Scholar]
- 5.Armstrong RK, Winfield JL. Paederus fuscipes dermatitis: an epidemic on Okinawa. The American Journal of Tropical Medicine and Hygiene. 1969;18:147–150. [PubMed] [Google Scholar]
- 6.Srichandan M. Skinpossible photo blog. 2011. www.flickr.com/ photos/skinpossible
- 7.Piel J. A polyketide synthase-peptide synthetase gene cluster from an uncultured bacterial symbiont of Paederus beetles. PNAS. 2002;99:14002–14007. doi: 10.1073/pnas.222481399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borroni G, Brazzelli V, Rosso R.M. Pavan. Paederus fuscipes dermatitis: a histopathological study. The American Journal of Dermatopathology. 1991;13:467–474. doi: 10.1097/00000372-199110000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Rahman S. Paederus dermatitis In Sierra Leone. Dermatol Online J. 2006;12:9. [PubMed] [Google Scholar]
- 10.Schofield S. Bugs don't have to bite to do damage: the tale of the Paederus beetle. 2004. www.forces.gc.ca Canadian National Defense website.