Abstract
A total of 382 stool samples were examined during a survey of intestinal parasites in members of the Tapirapé ethnic group, who live in the Brazilian Amazon region of Mato Grosso. Fecal DNAs from Blastocystis-positive samples were extracted, polymerase chain reaction amplified using Blastocystis-specific primers targeting the small subunit rRNA gene, and sequenced. Three subtypes (STs) were identified: ST1 (41%), ST2 (32%), and ST3 (17%). Seven mixed infections were found (11%). The subtype distribution was markedly different from that reported in Europe in that ST4 was not detected and ST3 was not the most common subtype. This study is the first to include molecular characterization of Blastocystis in Brazil and in indigenous communities from Latin America.
Blastocystis is a very common parasitic protist found in humans and a large variety of other animals.1–3 Numerous epidemiological surveys carried out in different countries report Blastocystis as the most common eukaryotic organism in human fecal samples,4 but the prevalence of Blastocystis infection in humans is still unknown in many parts of the world. The role of Blastocystis as a cause of diarrhea or other symptoms is controversial because it can be found in both symptomatic and asymptomatic individuals.2
Morphological identification of Blastocystis is challenging5 and traditional diagnostic methods differ significantly in their diagnostic sensitivity.6 Polymerase chain reaction (PCR) amplification of Blastocystis DNA from cultures or feces is probably the most sensitive detection method and also enables molecular characterization.7–10
Blastocystis exhibits extensive genetic diversity and comprises at least 13 subtypes (STs), nine of which have been found in humans.9,11–13 On a global scale, ST3 appears to be the most common subtype found in humans, followed in prevalence by ST1, ST2, and ST4.2 ST5–ST9 have a more sporadic occurrence and may be of zoonotic origin12,14; human infection with ST6 and ST7 appears to be more common in certain countries, such as Japan.15,16
The background prevalence of Blastocystis in Brazilian indigenous populations has been determined by direct examination of fecal samples on only two previous occasions,17,18 and nothing is known about the subtype distribution of Blastocystis in these cohorts. The only published study on Blastocystis subtypes in Latin America, a region inhabited by > 500 million people, was performed on only 12 isolates from Colombia.19 The aim of this study was to genetically characterize Blastocystis from inhabitants of six indigenous Indian communities in the Brazilian Amazonia, and to compare the subtypes present with those found in other countries.
The study was carried out in the Tapirapé community, situated 30 km from the Confresa municipality, state of Mato Grosso, Brazil (Figure 1). The indigenous reserve is located in Legal Amazonia and inhabited by 542 members of the Tapirapé ethnic group. The members of this tribe have many free roaming animals including dogs, cats, chickens, and pigs. The principal source of protein for this population is derived from fishing and hunting animals such as the paca, agouti, anteater, tortoise, capuchin monkey, deer, armadillo, tapir, mallard, and curassow. Piped water is drawn from nearby rivers and is delivered to every household, but it is neither filtered nor chlorinated. There is a general lack of adequate sanitation; only one public latrine is available for the entire village; however, this latrine is not used by all the villagers.
Figure 1.
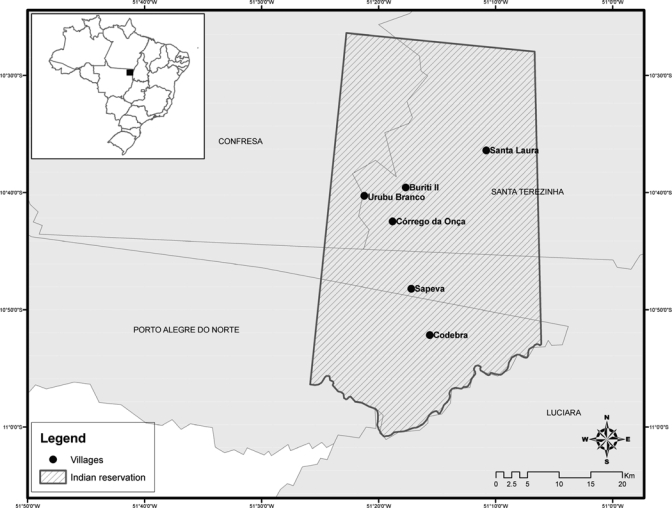
Localization of the six indigenous villages, Confresa Mato Grosso, Brazilian Amazon, Brazil.
A total of 382 fecal specimens (210 from females and 172 from males) were collected during January and February 2010 and examined by light microscopy (×400) of concentrates obtained by the techniques of Hoffmann and Ritchie.20–23 The consistency (formed, soft, loose, and watery) of all fecal samples was noted on collection. Demographic data and clinical information were recorded for all members of the tribe. The research was approved by the Ethics Committee of the Institute of Biomedical Sciences of the University of São Paulo, and consent was obtained from all human adult participants and from parents or legal guardians of minors according to National Committee for Ethics in Research (CONEP-120/2008).
Part of each microscopy-positive stool samples was preserved in 70% ethanol for subsequent DNA extraction and molecular analysis. Samples were washed three times in phosphate-buffered saline before extraction using the QIAamp DNA Stool Mini Kit (Qiagen, Hilden, Germany) according to the recommendations of the manufacturer, except that DNAs were eluted in 100 μL AE buffer.
The PCR and sequencing were performed as previously described,7 and sequences edited with Chromas version 2.33 (Technelysium Pty. Ltd., Queensland, Australia) were individually compared with Blastocystis SSU-rRNA gene sequences available in GenBank using the basic local alignment search tool (BLAST) algorithm. Subtypes were identified by determining a match or closest similarity to all known Blastocystis subtypes.9 Mixed subtype infections were identified by the presence of double peaks in semi-conserved gene areas.6
Demographic, such as age and gender, clinical, such as stool consistency and abdominal pain, and parasitological data were analyzed statistically using the Pearson χ2 test, in the cases with an expected count of < 20, and Fisher Exact test, when the expected count was > 20 (two-sided). We considered P values lower than 0.05 to be statistically significant.
Overall, 382 individuals from six indigenous villages were enrolled of whom 80 (21%) were positive for Blastocystis based on microscopy of fecal concentrates, 66 of which were confirmed by PCR. Blastocystis was more common in males than females (P < 0.05), and being < 15 years of age was associated with positivity for Blastocystis (P < 0.03).
Of 66 Blastocystis infections confirmed by PCR, sequences revealed single subtype infections in 59 cases and mixed subtype infections in seven cases (Table 1). ST1 was the predominant subtype, colonizing 27 individuals (41%), followed by ST2 in 21 individuals (32%), and ST3 in 11 (17%). Mixed infections consisting of ST1 and ST2 were seen in five individuals, ST1 and ST3 in one individual, and ST2 and ST3 in another individual.
Table 1.
Number of infections with Blastocystis confirmed by polymerase chain reaction (PCR) and Blastocystis subtype distribution among 382 indigenous people living in Tapirapé villages, Brazilian Amazon, Brazil
| Gender and age group | Microscopy-positive | Microscopy-negative | Total | Blastocystis sp. subtype | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PCR-positive | PCR-negative | ST1 | ST2 | ST3 | ST1/ST2 | ST1/ST3 | ST2/ST3 | ||||
| Females (< 15 y old) | 24 | 3 | 99 | 126 | 12 | 8 | 1 | 2 | 0 | 1 | 24 |
| Males (< 15 y old) | 22 | 7 | 73 | 102 | 7 | 8 | 6 | 1 | 0 | 0 | 22 |
| Females (> 15 y old) | 7 | 2 | 74 | 83 | 3 | 1 | 3 | 0 | 0 | 0 | 7 |
| Males (> 15 y old) | 13 | 2 | 56 | 71 | 5 | 4 | 1 | 2 | 1 | 0 | 13 |
| Total | 66 | 14 | 302 | 382 | 27 | 21 | 11 | 5 | 1 | 1 | 66 |
Among the 66 cases, 28 individuals had abdominal pain. Eleven of the latter had ST1, 10 had ST2, five had ST3, and two had a mixture of ST1 and ST2; there was no statistically significant association between Blastocystis STs and abdominal pain (P > 0.05). Likewise, no significant associations were found between infection with any of the observed Blastocystis subtypes and stool consistency, between gender and subtypes, or between age and subtypes (all P > 0.05).
An important step in understanding the geographical distribution of genetically distinct variants of Blastocystis was the adoption in 2007 of a standard nomenclature.9 Since then the most common subtype has proven to be ST3, followed by ST1, ST2, and ST4.4,12 Unlike almost all previously reported studies, the dominant subtype in this study was ST1 (41%), followed by ST2 (32%) and ST3 (17%). However, ST4, which has been recorded in studies from Europe and North America and some regions of Asia, was not detected in the Tapirapé Indian samples or, incidentally, in the small study of Colombian samples.19 Assuming the subtype distribution identified in this study and the Colombian samples19 is representative for Latin American Blastocystis, why is ST4 relatively prevalent throughout Europe and North America but absent in this and most other parts of the world? Further studies are needed to answer this and other questions involving the epidemiology of Blastocystis in Latin America, but the distribution of subtypes could be linked to the ethnic origin of the infected population, because there is little contact between indigenous groups and people in other communities.
Our subtyping results corroborate other studies in tropical developing countries. In Thai school children, 77.9% were infected with ST1 and 22.1% with ST2.24 ST1 was found in the school's water supply. In water treatment plants in the Philippines Blastocystis was found in 23% of the influent water and 7% of the effluent water, showing that treatment was not eliminating Blastocystis.25 Typing revealed ST1 and ST2 in both influent and effluent waters. As in these regions, one of the most likely sources of infection in our Brazilian study area is the water, because there is no water treatment in the Tapirapé community, and it raises the question as to whether certain subtypes are more resistant to water. More data from other ethnic groups in Brazil living in different biomes are needed to investigate whether the dominance of ST1 is a regional phenomenon or is linked to populations with a particular ethnic/ecological background.
In our study, 11% of the infections were subtype mixtures, which suggests either multiple sources of infection or one source containing multiple subtypes. This prevalence is similar to studies in China,26 Turkey,27,28 France,4 Denmark,2 and Egypt,29 and mixed infections were also seen in the Colombian samples.19 The true prevalence of mixed infections is difficult to ascertain as detection is likely to depend on the method used for subtyping.10
Understanding the prevalence and genetic structure of intestinal parasites, such as Blastocystis, in endemic areas may contribute to a better understanding of the risk factors for infection in different ecological situations. Because Blastocystis is apparently transmitted fecal-orally and is very common, this parasite appears to be an appropriate indicator for the overall level of intestinal parasitism in different populations. Therefore, data on Blastocystis could be helpful in elaborating and evaluating intervention methods to reduce the burden of intestinal parasites.
This study of Blastocystis subtypes is only the second in Latin America but represents the first in Brazil and the first involving an indigenous community of Latin America.
ACKNOWLEDGMENTS
We thank Mohammed Alfellani for his help in DNA extraction at the Department of Pathogen Molecular Biology, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London.
Footnotes
Financial support: This research was financially supported by the Brazilian Ministry of Health – FUNASA and the Brazilian Research Council - CNPq, FAPEMAT.
Authors' addresses: Antonio F. Malheiros, Department of Biology, Department of Nursing, Mato Grosso State University, Cáceres, Mato Grosso, Brazil; and Department of Parasitology, São Paulo University, São Paulo, Brazil, E-mails: malheiros@unemat.br and afmalheiros@usp.br. C. Rune Stensvold, Department of Microbiological Diagnostics, Statens Serum Institut, Copenhagen S, Denmark, E-mail: run@ssi.dk. C. Graham Clark, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, UK, E-mail: graham.clark@lshtm.ac.uk. Guilherme B. Braga, Department Medicine Veterinary Preventive and Animal Health, São Paulo University, São Paulo, Brazil, E-mail: guibraga@vps.fmvz.usp.br. Jeffrey J. Shaw, Department of Parasitology, São Paulo University, São Paulo, Brazil, E-mail: jayusp@hotmail.com.
References
- 1.Clark CG. Cryptic genetic variation in parasitic protozoa. J Med Microbiol. 2000;49:489–491. doi: 10.1099/0022-1317-49-6-489. [DOI] [PubMed] [Google Scholar]
- 2.Stensvold CR, Lewis HC, Hammerum AM, Porsbo LJ, Nielsen SS, Olsen KE, Arendrup MC, Nielsen HV, Mølbak K. Blastocystis: unraveling potential risk factors, and clinical significance of a common but neglected parasite. Epidemiol Infect. 2009;137:1655–1663. doi: 10.1017/S0950268809002672. [DOI] [PubMed] [Google Scholar]
- 3.Tan KS, Singh M, Yap EH. Current views on the clinical relevance of Blastocystis spp. Curr Infect Dis Rep. 2010;12:28–35. doi: 10.1007/s11908-009-0073-8. [DOI] [PubMed] [Google Scholar]
- 4.Souppart L, Sanciu G, Cian A, Wawrzyniak I, Delbac F, Capron M, Dei-Cas E, Boorom K, Delhaes L, Viscogliosi E. Molecular epidemiology of human Blastocystis isolates in France. Parasitol Res. 2009;105:413–421. doi: 10.1007/s00436-009-1398-9. [DOI] [PubMed] [Google Scholar]
- 5.Utzinger J, Botero-Kleiven S, Castelli F, Chiodini PL, Edwards H, Köhler N, Gulletta M, Lebbad M, Manser M, Matthys B, N'Goran EK, Tannich E, Vounatsou P, Marti H. Microscopic diagnosis of sodium acetate-acetic acid-formalin-fixed stool samples for helminths and intestinal protozoa: a comparison among European reference laboratories. Clin Microbiol Infect. 2010;16:267–273. doi: 10.1111/j.1469-0691.2009.02782.x. [DOI] [PubMed] [Google Scholar]
- 6.Stensvold CR, Arendrup MC, Jespersgaard C, Mølbak K, Nielsen HV. Detecting Blastocystis using parasitologic and DNA-based methods: a comparative study. Diagn Microbiol Infect Dis. 2007;59:303–307. doi: 10.1016/j.diagmicrobio.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Scicluna SM, Tawari B, Clark CG. DNA barcoding of Blastocystis. Protist. 2006;157:77–85. doi: 10.1016/j.protis.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Stensvold R, Brillowska-Dabrowska A, Nielsen HV, Arendrup MC. Detection of Blastocystis hominis in unpreserved stool specimens by using polymerase chain reaction. J Parasitol. 2006;92:1081–1087. doi: 10.1645/GE-840R.1. [DOI] [PubMed] [Google Scholar]
- 9.Stensvold CR, Suresh GK, Tan KS, Thompson RC, Traub RJ, Viscogliosi E, Yoshikawa H, Clark CG. Terminology for Blastocystis subtypes–a consensus. Trends Parasitol. 2007;23:93–96. doi: 10.1016/j.pt.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Meloni D, Sanciu G, Poirier P, El Alaoui H, Chabé M, Delhaes L, Dei-Cas E, Delbac F, Fiori PL, Cave DD, Viscogliosi E. Molecular subtyping of Blastocystis sp. isolates from symptomatic patients in Italy. Parasitol Res. 2011;109:613–619. doi: 10.1007/s00436-011-2294-7. [DOI] [PubMed] [Google Scholar]
- 11.Clark CG. Extensive genetic diversity in Blastocystis hominis. Mol Biochem Parasitol. 1997;87:79–83. doi: 10.1016/s0166-6851(97)00046-7. [DOI] [PubMed] [Google Scholar]
- 12.Stensvold CR, Alfellani MA, Nørskov-Lauritsen S, Prip K, Victory EL, Maddox C, Nielsen HV, Clark CG. Subtype distribution of Blastocystis isolates from synanthropic and zoo animals and identification of a new subtype. Int J Parasitol. 2009;39:473–479. doi: 10.1016/j.ijpara.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Parkar U, Traub RJ, Vitali S, Elliot A, Levecke B, Robertson I, Geurden T, Steele J, Drake B, Thompson RC. Molecular characterization of Blastocystis isolates from zoo animals and their animal-keepers. Vet Parasitol. 2010;169:8–17. doi: 10.1016/j.vetpar.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 14.Stensvold CR, Nielsen HV, Mølbak K, Smith HV. Pursuing the clinical significance of Blastocystis–diagnostic limitations. Trends Parasitol. 2008;25:23–29. doi: 10.1016/j.pt.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Kaneda Y, Horiki N, Cheng X, Fujita Y, Maruyama M, Tachibana H. Ribodemes of Blastocystis hominis isolated in Japan. Am J Trop Med Hyg. 2001;65:393–396. doi: 10.4269/ajtmh.2001.65.393. [DOI] [PubMed] [Google Scholar]
- 16.Yoshikawa H, Wu Z, Kimata I, Iseki M, Karim IKM, Hossain MB, Zaman V, Haque R, Takahashi Y. Polymerase chain reaction-based genotype classification among human Blastocystis hominis populations isolated from different countries. Parasitol Res. 2004;92:22–29. doi: 10.1007/s00436-003-0995-2. [DOI] [PubMed] [Google Scholar]
- 17.Aguiar JI, Gonçalves AQ, Sodré FC, Pereira SR, Bóia MN, Lemos ER, Daher RR. Intestinal protozoa and helminths among Terena Indians in the State of Mato Grosso do Sul: high prevalence of Blastocystis hominis. Rev Soc Bras Med Trop. 2007;40:631–634. doi: 10.1590/s0037-86822007000600006. [DOI] [PubMed] [Google Scholar]
- 18.Borges JD, Alarcón RS, Neto VA, Gakiya E. Intestinal parasitosis in Indians of the Mapuera community (Oriximiná, State of Pará, Brazil): high prevalence of Blastocystis hominis and finding of Cryptosporidium sp. and Cyclospora cayetanensis. Rev Soc Bras Med Trop. 2009;42:348–350. doi: 10.1590/s0037-86822009000300022. [DOI] [PubMed] [Google Scholar]
- 19.Santín M, Gómez-Muñoz MT, Solano-Aguilar G, Fayer R. Development of a new PCR protocol to detect and subtype Blastocystis spp. from humans and animals. Parasitol Res. 2010;109:205–212. doi: 10.1007/s00436-010-2244-9. [DOI] [PubMed] [Google Scholar]
- 20.Faust EC, Sawitz W, Tobie J, Odom V, Peres C, Lincicome DR. Comparative efficiency of various technics for the diagnosis of protozoa and helminths in feces. J Parasitol. 1939;25:241–262. [Google Scholar]
- 21.Allen AV, Ridley DS. Further observations on the formol-ether concentration technique for fecal parasites. J Clin Pathol. 1970;23:545–546. doi: 10.1136/jcp.23.6.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Truant AL, Elliott SH, Kelly MT, Smith JH. Comparison of formalin-ethyl ether sedimentation, formalin-ethyl acetate sedimentation and zinc sulfate flotation techniques for detection of intestinal parasites. J Clin Microbiol. 1981;13:882–884. doi: 10.1128/jcm.13.5.882-884.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zaman V, Khan KZ. A comparison of direct microscopy with culture for the diagnosis of Blastocystis hominis. Southeast Asian J Trop Med Public Health. 1994;25:792–793. [PubMed] [Google Scholar]
- 24.Leelayoova S, Siripattanapipong S, Thathaisong U, Naaglor T, Taamasri P, Piyaraj P, Mungthin M. Drinking water: a possible source of Blastocystis spp. subtype 1 infection in schoolchildren of a rural community in central Thailand. Am J Trop Med Hyg. 2008;79:401–406. [PubMed] [Google Scholar]
- 25.Banaticla JE, Rivera WL. Detection and subtype identification of Blastocystis isolates from wastewater samples in The Philippines. J Water Health. 2011;9:128–137. doi: 10.2166/wh.2010.127. [DOI] [PubMed] [Google Scholar]
- 26.Li LH, Zhou XN, Du XW, Wang XZ, Wang LB, Jiang JY, Yoshikawa H, Steinmann P, Utzinger J, Wu Z, Chen JX, Chen SH, Zhang L. Molecular epidemiology of human Blastocystis in a village in Yunnan province, China. Parasitol Int. 2007;56:281–286. doi: 10.1016/j.parint.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Dogruman-Al F, Dagci H, Yoshikawa H, Kurt Ö, Demirel M. A possible link between subtype 2 and asymptomatic infections of Blastocystis hominis. Parasitol Res. 2008;103:685–689. doi: 10.1007/s00436-008-1031-3. [DOI] [PubMed] [Google Scholar]
- 28.Dogruman-Al F, Kustimur S, Yoshikawa H, Tuncer C, Simsek Z, Tanyuksel M, Araz E, Boorom K. Blastocystis subtypes in irritable bowel syndrome and inflammatory bowel disease in Ankara, Turkey. Mem Inst Oswaldo Cruz. 2009;104:724–727. doi: 10.1590/s0074-02762009000500011. [DOI] [PubMed] [Google Scholar]
- 29.Souppart L, Moussa H, Cian A, Sanciu G, Poirier P, Alaoui HE, Delbac F, Boorom K, Delhaes L, Dei-Cas E, Viscogliosi E. Subtype analysis of Blastocystis isolates from symptomatic patients in Egypt. Parasitol Res. 2010;106:505–511. doi: 10.1007/s00436-009-1693-5. [DOI] [PubMed] [Google Scholar]


