Abstract
In developing countries, it is difficult to rally a radiologist to conduct field studies. Here, we report how a radiologist taught a clinician to carry out the ultrasound examination as defined by the World Health Organization (WHO) record sheet for Schistosoma haematobium related lesions. In a population infected with S. haematobium, the learner and teacher performed two ultrasound exams and the results were compared. One hundred thirty-two children were prospectively included, during 8 ultrasonography sessions split over 23 days. After 51 examinations the learner's sensitivity was above 90%. After the fifth session the specificity reached 100% (results remained stable until the end of the study period). This study shows that a clinician can quickly learn how to carry out a simple ultrasound examination to gather the items needed for the follow-up of S. haematobium related lesions, suggesting that clinicians could implement networks of ultrasound-based surveillance on the field.
Introduction
In African countries affected by schistosomiasis, there is a shortage of radiologists. These radiologists are often confined to public or private hospitals and are difficult to mobilize to participate in the screening or monitoring of patients infected with Schistosoma haematobium on the field. A radiologist is required to establish a diagnosis by means of an ultrasound machine. However, searching specific items to screen for particular pathologies or reporting on a local lesion are probably achievable by clinicians in the field. In this study, we investigated the ability of a clinician who is new to vesico-urinary ultrasonography to perform the clinical examination, and the number of examinations that he must complete to become efficient. If successful, this method would facilitate the delocalization of portable devices on the field to better monitor patients, the detection of severe forms of the disease, and the implementation of mass treatment.
The impoundment of the Diama dam in 1986 was the beginning of the epidemic/endemic schistosomiasis (urinary and digestive) in the Senegal valley. Numerous studies have shown a very high prevalence of patients with S. haematobium schistosomiasis1; the monitoring of such a population, particularly the assessment of the disease severity remains tricky. The difficulty lies not in the diagnosis of schistosomiasis, which is simple and based on the detection of the parasite in the urine, but in the morbidity appraisal, based on the vesico-urinary ultrasonography, hardly implemented in the field. Unlike schistosomiasis caused by Schistosoma mansoni, for the diagnosis of which ultrasound has a recognized place and has been used for many years in studies of morbidity (Symmer fibrosis), the use of ultrasound for S. haematobium morbidity assessment is rarer. Yet it should be more systematic because, as with the infections caused by S. mansoni, lesions observed by ultrasonography in the infection with S. haematobium are more common than the simple detection of the parasite in the urine and the incidence of microhematuria is greater than the findings of macrohematuria. Indeed, a study conducted in 10 villages in the Senegal River Valley showed that even if microhematuria was present in all the villages, whereas macrohematuria was reported in 7 villages.2 In addition, the finding of high infection rates a year after an adequate treatment3,4 suggests that the presence of eggs in urine or macroscopic hematuria are not sufficient to describe the severity of S. haematobium related lesions. Thus, we believe that use of ultrasound could be widely spread to study schistosomiasis, especially in a context of re-emergence of this infection in many African localities.
A record sheet was developed for the “universal” codification of this test,2 but the use of this sheet requires the expertise of a senior radiologist to carry out the examination.
The advantage of this classification is to assess the severity of lesions induced by S. haematobium. It tracks not only the early forms of the disease (isolated bladder lesions) but also looks for the impact on the upper urinary tract (dilatation of the urethras and renal lesions). The upper urinary tract lesions begin to show later than the bladder, but they also take longer to disappear after treatment. This ultrasound examination can thus produce an “index of severity” by adding the urinary bladder intermediate score and the upper urinary tract intermediate score. The first corresponds to the recognition of bladder lesions and is very supportive of S. haematobium related lesions when it is greater than three. The second is related to the severity of lesions of the upper urinary tract, and is of poor prognosis. In this sense, the finding of a dilated urethra has a score range of +3 to +4 (+6 to +8 when it is bilateral), and the presence of kidney damage is listed +6 to +8 (+12 to +16 when it is bilateral).
The objective of this study was to analyze how fast the items included in the “WHO S. haematobium ultrasound grid” was learned by a clinician, by comparing its results with those of a professional radiologist.
Patients and methods
Patients.
Patients included were children of a cohort followed up for S. haematobium infection in the Senegal River Valley. The inclusions were made prospectively during a visit planned as part of a routine follow-up, 4 months after the last treatment (a single administration of 40 mg/kg of praziquantel, p.o.). All the included children were from an area along the River Valley between the St.-Louis and Ross-Béthio region, where S. haematobium is hyperendemic.
Methods.
Two ultrasound examinations were performed for each child. The first one by the learning clinician (PB, later referred to as “learner”) and the second by the referent radiologist, usually in charge of monitoring children (ID, later referred to as “teacher”). The examinations were conducted by means of a General Electric Healthcare device, United Kingdom: LOGICe with a 4C-RS probe. Results were compiled using the WHO record sheet for S. haematobium-associated ultrasound findings published in 1996.5 Anomalies observed on ultrasound images elicit the establishment of a score ranging from 0 to 34 (Figure 1). A normal ultrasound image has a score of zero. The result of the learner is considered acceptable if it is the same as the teachers. Two error types were possible: the learner spotting lesions not observed by the teacher, or the learner missing lesions recorded by the teacher. Informed consent was obtained from parents or legal guardians, and the Senegalese National Committee for Ethics and Scientific Research (CNERS) approved the project on November 23, 2010.
Figure 1.
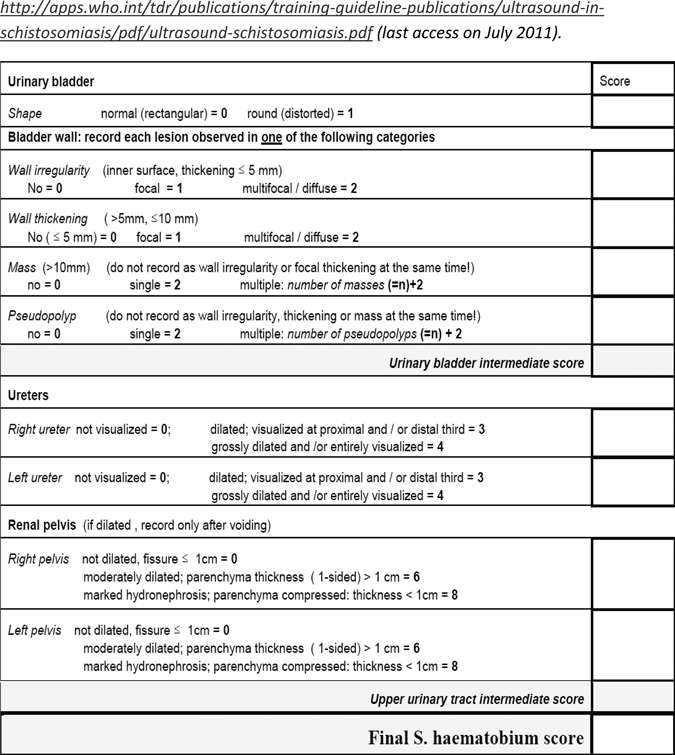
Record sheet for Schistosoma haematobium-associated ultrasound findings. Available at: http://apps.who.int/tdr/publications/training-guideline-publications/ultrasound-in-schistosomiasis/pdf/ultrasound-schistosomiasis.pdf (last accessed on July 2011).
For each day of the study, three variables were compared: the difference in scores between the two operators (teacher and learner), the sensitivity of the learner (% of odds that the learner finds an injury when the teacher sees one), and specificity of the learners (% of odds that the learner does not see any damage when the teacher does not find any).
Statistical analysis.
For quantitative variables the difference between both operators was calculated. For categorical variables the numbers and percentages were also calculated (similarity of ultrasound results between both operators, normal ultrasound per operator). To evaluate the learner's detection ability of Schistosoma lesions throughout the study period, calculations of sensitivity and specificity were performed for each study day. The χ2 test and Fisher's exact test were used for qualitative variables, whereas Wilcoxon and Student's t test were used for quantitative variables. Statistical analysis was performed using the STATA/IC 11.0 software (College Station, TX).
Results
One hundred thirty-two children (8.8 ± 0.8 years of age, gender ration M/F = 2) were included in the study, which lasted 8 days, spread over a 23-day period. During these 23 days, 8 ultrasound sessions were performed in 3 periods of 5, 2, and 1 days during which respectively 91, 26, and 15 examinations were performed. Concerning the intensity of infection, 35% of the children had S. haematobium eggs in urine, of whom 33% had a count > 50 eggs/10 mL.
The frequency of normal ultrasound images was 58% for the teacher and 59% for the learner. Mean score of teacher was 0.94 ± 2.01 [0–17], and mean score of learner was 1.11 ± 2.77 [0–19] without any statistical difference between them (P = 0.08). Of the 132 ultrasound examinations, only 12 discrepancies (9%) were found. Among these 12 discordant ultrasound images, 8 scores had 1 point difference (67%), 2 had 2 points difference, and 2 were found to have a discrepancy of more than 2 points (8 and 10 points). Moreover, in 9 of these discordant ultrasound images, it was the learner who had not seen the lesions seen by the teacher (underestimation) and in 3 cases it was the learner who reported injuries not found by the teacher (overestimation).
The learning curve and the evolution of sensitivity (Se) and specificity (Sp) of the learner in comparison to the teacher during the study period is shown in Figure 2, attesting the improving ability of the learner to reach teacher's results.
Figure 2.
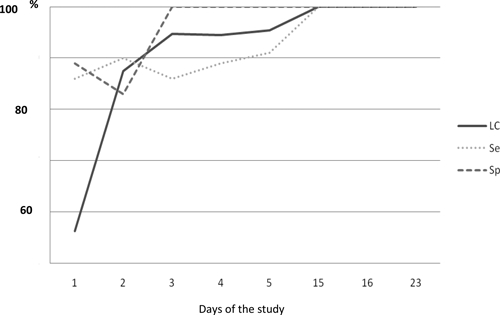
Learning curve (LC) of the learner (% concordance), sensibility (Se), and specificity (Sp) of the learner compared with the teacher.
Discussion
The possibility to train clinicians to perform ultrasound images for this purpose on the field is attractive for developing countries. The idea here is not to replace ultrasound imaging for a diagnostic purpose, which must remain under the responsibility of the radiologist, but to detect simple lesions known by the learner and to count them. The interest is of course to guide mass interventions and to follow-up in an easy way the regression of lesions or the identification of patients requiring special monitoring.
This study shows that within a few sessions (8 days divided into 3 periods of 23 days), a clinician could become independent in carrying out the examination and find the same results as the referent radiologist. The differences are mostly moderate (10 differences out of 12 are of 2 points or less), and the two most important differences are related to dilatation of the ureters missed by the learner at the beginning of the study period (D1 and D5).
By the third day of the study, after 50 examinations conducted by the learner and teacher (51 were conducted during the first 3 days), the learner finds the same result as the teacher in over 90% of the cases. Furthermore, the sensitivity/specificity analysis shows that after Day 3 the learner screens 100% of healthy subjects, and within two more days of learning, he manages to find all the lesions seen by the teacher without making any mistake.
Finally, this learning appears to persist over time because results were still satisfactory in the last days of the study, even though there was a period of 10 days without ultrasound between period 1 and period 2, and 7 days between period 2 and period 3. However, these results should be interpreted with caution because the proportion of normal ultrasound images (without injuries) was higher during the last days of the study, and it is probably easier for the learner to recognize a normal examination than to detect anomalies.
There is no literature available on the transfer of ultrasonographic skills between a radiologist and a clinician in developing countries. However, 50 tests to learn a simple ultrasound technique are consistent with the literature. For example, 65 examinations are sufficient for residents to learn how to find an abnormality in a fetal cardiac evaluation,6 40 are necessary to detect a complication of pregnancy during the first trimester,7 and only 30 are needed to learn how to detect an obstructive uropathy.8
This study suggests that the information contained in the evaluation record sheet established by the WHO is readily transferrable to a clinician. Although a regular control of the learner by the teacher should be implemented, these results indicate that diagnosis and basic surveillance of S. haematobium related lesions are feasible by clinicians on the field after a short training.
ACKNOWLEDGMENTS
We thank Lobna Gaayeb and Hakam Gharbi for their participation in the translation process.
Disclaimer: None of the authors of this study has a conflict of interest to declare in the scope of this article.
Footnotes
Authors' addresses: Philippe Bonnard, ONG Espoir Pour La Santé (EPLS), Saint Louis, Sénégal; Unité INSERM U1019, CIIC, Lille, France; Maladies Infectieuses et Tropicales, Hôpital Tenon (AP-HP), UPMC, Paris, France, E-mail: philippe.bonnard@tnn.aphp.fr. Samy Boutouaba, Modou Seck, and Jean-Pierre Dompnier, ONG Espoir Pour La Santé (EPLS), Saint Louis, Sénégal, E-mails: samy.boutouaba@espoir-sante.org, modou.seck@espoir-sante.org, and jpdompnier@gmail.com. Ibrahima Diakhate, Radiologie, Centre Hospitalier Universitaire FANN, Fann, Senegal, E-mail: idiakt@yahoo.fr. Gilles Riveau, ONG Espoir Pour La Santé (EPLS), Saint Louis, Sénégal; Unité INSERM U1019, CIIC, Lille, France, E-mail: gilles.riveau@gmail.com.
References
- 1.Delegue P, Picquet M, Shaw DJ, Vercruysse J, Sambou B, Ly A. Morbidity induced by Schistosoma haematobium infections, as assessed by ultrasound before and after treatment with praziquantel, in a recently expanded focus (Senegal River basin) Ann Trop Med Parasitol. 1998;92:775–783. doi: 10.1080/00034989859014. [DOI] [PubMed] [Google Scholar]
- 2.De Clerck D, Vercruysse J, Sene M, Seck I, Sall CS, Ly A, Southgate VR. The effect of irrigated agriculture on the transmission of urinary schistosomiasis in the Middle and Upper Valleys of the Senegal River Basin. Ann Trop Med Parasitol. 2000;94:581–590. doi: 10.1080/00034983.2000.11813581. [DOI] [PubMed] [Google Scholar]
- 3.Shaw DJ, Vercruysse J, Piquet M, Sambou B, Ly A. The effect of different treatment regimens on the epidemiology of seasonally transmitted Schistosoma haematobium infections in four villages in the Senegal River Basin. Trans R Soc Trop Med Hyg. 1999;93:142–150. doi: 10.1016/s0035-9203(99)90288-2. [DOI] [PubMed] [Google Scholar]
- 4.De Clercq D, Vercruysse J, Picquet M, Shaw DJ, Diop M, Ly A, Gryssels B. The epidemiology of a recent focus of mixed Schistosoma haematobium and Schistosoma mansoni infections around the ‘Lac de Guiers’ in the Senegal River Basin, Senegal. Trop Med Int Health. 1999;4:544–550. doi: 10.1046/j.1365-3156.1999.00444.x. [DOI] [PubMed] [Google Scholar]
- 5.Richter J, Hatz C, Campagne G, Bergquist NR, Jenkins JM. Ultrasound in Schistosomiasis: A Practical Guide to the Standardized Use of Ultrasonography for the Assessment of Schistosomiasis-Related Morbidity. Geneva: WHO; 1996. [Google Scholar]
- 6.Cruz-Martinez R, Figueras F, Jaramillo JJ, Meler E, Méndez A, Hernandez-Andrade E, Gratacos E. Learning curve for Doppler measurement of fetal modified myocardial performance index. Ultrasound Obstet Gynecol. 2011;37:158–162. doi: 10.1002/uog.7765. [DOI] [PubMed] [Google Scholar]
- 7.Jang TB, Ruggeri W, Dyne P, Kaji AH. Learning curve of emergency physicians using emergency bedside sonography for symptomatic first-trimester pregnancy. J Ultrasound Med. 2010;29:1423–1428. doi: 10.7863/jum.2010.29.10.1423. [DOI] [PubMed] [Google Scholar]
- 8.Jang TB, Casey RJ, Dyne P, Kaji A. The learning curve of resident physicians using emergency ultrasonography for obstructive uropathy. Acad Emerg Med. 2010;17:1024–1027. doi: 10.1111/j.1553-2712.2010.00850.x. [DOI] [PubMed] [Google Scholar]


