Abstract
This study examined sociocultural features of help-seeking for Buruli ulcer–affected persons with pre-ulcers and ulcers in a disease-endemic area in Ghana. A sample of 181 respondents were purposively selected. Fisher's exact test was used to compare help-seeking variables for pre-ulcers and ulcers. Qualitative phenomenologic analysis of narratives clarified the meaning and content of selected quantitative help-seeking variables. For pre-ulcers, herbal dressings were used to expose necrotic tissues and subsequently applied as dressings for ulcers. Analgesics and left-over antibiotics were used to ease pain and reduce inflammation. Choices for outside-help were influenced by the perceived effectiveness of the treatment, the closeness of the provider to residences, and family and friends. Health education is required to emphasize the risk of self-medication with antibiotics and the importance of medical treatment for pre-ulcers, and to caution against the use of herbs to expose necrotic tissues, which could lead to co-infections.
Introduction
Buruli ulcer is a debilitating disease of the skin and occasionally the bones. It affects persons of all ages, although children less than 15 years-of-age are more vulnerable to infection.1–5 Because the mode of Buruli ulcer transmission is unknown,5 public health programs in affected countries encourage early medical treatment to alleviate suffering and avoid disabilities.1 Studies on help-seeking of affected persons are important because they highlight the influence of social, cultural, economic, and behavioral influences on help-seeking choices. These influences and help-seeking preferences also account for delays in seeking effective medical treatment of pre-ulcer conditions before progressing into painful ulcers. Sociocultural studies of help-seeking practices for Buruli ulcer feature strongly on the research agenda of the World Health Organization (WHO) and are necessary to guide public health strategies for treatment and control.1
Buruli ulcer usually starts as a painless nodule, swelling (edema) or plaque (firmness of the skin), which is commonly referred to as the pre-ulcer stage of infection. If treatment is not sought at this stage, the disease is likely to progress into painful ulcers.1,4,5 There have been reported cases of Buruli ulcer from at least 30 countries in tropical and sub-tropical regions of the world, especially in countries in western Africa such as Benin, Côte d'Ivoire, and Ghana, where most persons with cases reside.1 Ghana reports approximately 1,000 cases of Buruli ulcer a year,1 and has a national prevalence of 20.7 cases/100,000 population; Buruli ulcer prevalence is 87.7 cases/100,000 population in the Ga-West and Ga-South municipalities.6
Studies have shown that most persons with Buruli ulcer infection do not seek early treatment. Cultural beliefs, financial capacity, access to treatment facilities, prolonged hospitalization, and the fear of surgical outcomes are possible explanations.7–11 However, there is limited information to distinguish help-seeking for pre-ulcer and ulcer infections. Explaining the distinguishing features of sociocultural features of help-seeking for pre-ulcer and ulcer conditions is important. Explanation of these features will clarify the status of actual help-seeking practices at early and late stages of Buruli ulcer, the range of providers consulted, the influence of initial help-seeking on delay in reaching effective services, and reasons for choice of provider types. These factors affect management of Buruli ulcer and are useful to inform health service providers and managers and help to reduce the treatment gap for Buruli ulcer. This study examined sociocultural features of help-seeking for persons with Buruli ulcer with pre-ulcer and ulcer conditions in the Ga-West and Ga-South municipalities in Accra, Ghana.
Methods
Research setting.
The study was conducted in the Ga-West and Ga-South Municipalities of the Greater Accra region during November 2008–July 2009. The population of Ga-West Municipality for 2009 was 215,824 on the basis of projected population estimates from the national housing and population census. Ga-West Municipality is rural (Annual Report of the Municipal Health Management Team, Ga-West Municipality). The projected population of Ga-South Municipality for 2009 was 284,712. Approximately 76% of the municipality is predominantly urban and peri-urban; 24% is rural.12 Both municipalities have a similar population structure; 35% of the population were less than 15 years-of-age and 65% were ≥ 15 years of age. The major Buruli ulcer medical treatment centers are Amasaman Hospital and the Kojo Ashong Clinic in Ga-West Municipality and the Obom Health Center in Ga-South Municipality. The Amasaman Hospital is the main referral center for Buruli ulcer treatment.
Study sample.
A sample of 181 respondents was obtained from 3 Buruli ulcer treatment centers and 67 communities in both municipalities. With the exception of children less than five years-of-age whose parents acted as proxy respondents, older children were interviewed first, then caretakers who were invariably parents of children. Clinical records from Amasaman Hospital indicated that approximately 90 persons are treated medically for Buruli ulcer annually. Therefore, we interviewed all patients undergoing treatment at the Amasaman Hospital, the Kojo Ashong Clinic, and the Obom Health Center, and purposively selected all affected persons from 67 disease-endemic communities. The intention to interview respondents from health facilities and communities, therefore was not to compare help-seeking behaviors among these two groups but rather to obtain a fairly adequate sample to make inferences for help-seeking behaviors for pre-ulcers and ulcers.
A list of disease-endemic communities was obtained from the municipal health directorates of the Ga-West Municipality and Ga-South Municipality. These communities were visited and community participants were located with the assistance of community-based surveillance volunteers (CBSVs) who kept registers of all affected persons. Neighboring communities (which were not listed as being endemic) were entered, and affected persons were located and interviewed with the help of CBSVs. Schools in sampled communities were also visited, and with the permission of the head teacher and class teacher, a WHO Buruli ulcer picture guide13 was shown to the children. Children who admitted to having suspicious lesions were screened by health personnel from the Kojo Ashong Clinic for confirmation. In disease-endemic areas with a long history of Buruli ulcer infection, trained health workers are capable of identifying cases by using the WHO classification.13 A register of all respondents was compiled to avoid double interviews of outpatients resident in the communities who had already been interviewed at health facilities.
Explanatory model interview catalog.
An explanatory model interview was used based on the explanatory model interview catalog (EMIC) framework for cultural epidemiology.14 The core structure of the EMIC was developed to examine patterns of help-seeking for Buruli ulcer. The design of the semi-structured interview was informed by preliminary ethnographic field experience, focus group discussions, and earlier studies.9,15 Help-seeking practices were elicited by questions on self-help, home-based care, places visited for help, and providers approached for care outside the home. The first source of outside help, reasons for this choice, and the most helpful outside help were queried in the interview. To enable comparison, the same set of questions was asked for pre-ulcer and ulcer conditions. Narratives in response to open-ended questions elaborated and explained coded categories and their responses. The instruments were developed in English, but interviews were conducted in the local Ghanaian languages (Ga, Ewe, and Twi) spoken by respondents in the study areas.
Data analysis.
Categorical and numeric data from the EMIC interviews were double-entered using EPI Info version 3.4.1 (Centers for Disease Control and Prevention, Atlanta, GA) and later cleaned and analyzed by using STATA Statistics/Data analysis software (Stata Corporation, College Station, TX).We examined and compared frequencies of self-help, home-based care, and use and first use of provider types for respondents with pre-ulcers and ulcers. Individual categories of treatment and provider-type were grouped thematically for analysis and comparisons were based on overarching concepts (e.g., home-based remedies/self medication, traditional and faith healers, private doctors and facilities, and government health facilities for help-seeking). Total reported responses were tabulated by summing spontaneous and probed responses. Fisher's exact test was used to compare associations between categorical help-seeking variables for pre-ulcers and ulcers. A two-sample test for proportions was used to test associations between effectiveness of treatment from providers for ulcers. Proportions were computed by dividing the number of respondents who considered the treatment by the number of respondents who used the provider.
Narrative data were transcribed into English during the interview by the data collector, entered into Microsoft Office Word 2007 (Microsoft Corporation, Redmond, WA), and imported into MAXqda. MAXqda software 2010 (Verbi Software Consult Sozialforschung, GmbH, Marburg, Germany) for textual analysis was used for a phenomenologic analysis of help-seeking quantitative variables of interest for selected respondents' records on the basis of thematic coding. This approach enabled clarification of content and dynamic features of explanatory variables associated with help-seeking preferences.
Ethical considerations.
The study was approved by the ethical review committee of the Ministry of Health, Ghana, and the ethics commission of Basel (Ethikkommission Beider, Basel, Switzerland). Verbal consent was preferred to written consent because it did not pose any psychological threat and reassured all interviewees of anonymity. Both ethical review boards approved verbal consent as long as participation in the study was voluntary; participants had been informed of the study aims and had the opportunity to ask questions. Before the start of all interviews, interviewees were informed of study aims, type of questions to be asked, and intended use of findings to guide Buruli ulcer–related health programs and for publication in academic journals and reports. They were informed of their rights to decline participation.
Results
Sample characteristics.
A total of 181 respondents were interviewed (48.1% male and 51.9% female). The mean age was 22.5 years. Most respondents had been enrolled in school; 54.1% had at least completed primary school and 23.8% had no education. Approximately 26.0% of respondents were unskilled laborers, 7.7% were unemployed, and 55.3% were still in school (Table 1).
Table 1.
Demographic characteristics of respondents, Ghana*
| Characteristic | Value |
|---|---|
| Sex | |
| M | 87 (48.1) |
| F | 94 (51.9) |
| Age of respondents, years | |
| Minimum | 3 |
| Maximum | 87 |
| Mean ± SD | 22.5 ± 18.1 |
| Education | |
| None | 43 (23.8) |
| Primary | 98 (54.1) |
| Secondary/vocational | 40 (22.1) |
| Occupation | |
| Pupil/student | 100 (55.3) |
| Unskilled labor | 47 (26.0) |
| Skilled laborer/professional | 13 (7.2) |
| Unemployed | 14 (7.7) |
| Other (too young for school and employment) | 7 (3.8) |
| Income | |
| Regular and dependable | 34 (18.8) |
| Uncertain/cannot tell | 78 (43.1) |
| Irregular | 69 (38.1) |
| Marital status | |
| Never married | 125 (69.0) |
| Married | 42 (23.2) |
| Separated/divorced | 5 (2.8) |
| Widowed | 9 (5.0) |
Values are no. (%) unless otherwise indicated.
Home treatment.
Help-seeking refers to various home remedies used, self-help actions, and subsequently outside providers who were visited for treatment of Buruli ulcer. Generally, respondents mainly used herbal dressings, leftover drugs and pills; some did not seek help. Respondents were more likely to treat pre-ulcers (63%) than ulcers (51.9%) by placing herbal dressings on affected body parts, (P < 0.001). They also used pills, mainly analgesics for pain management, and leftover antibiotics and blood tonics for pre-ulcers (34.3%) and ulcers (49.7%; P < 0.001) (Table 2).
Table 2.
Self-help at home among respondents with pre-ulcers and ulcers, Ghana*
| Category of self-help | Pre-ulcers (n = 181) | Ulcers (n = 181) | P |
|---|---|---|---|
| Drank herbal concoctions at home | 23.8 | 29.8 | < 0.001 |
| Placed herbal dressing on pre-ulcer/ulcers | 63.0 | 51.9 | < 0.001 |
| Used pills and other drugs at home | 34.3 | 49.7 | < 0.001 |
| Offered prayers at home | 7.7 | 16.6 | < 0.001 |
| Nothing | 26.0 | 32.6 | 0.003 |
| Other home remedies (hot compress, massage, slitting nodules) | 5.0 | 4.4 | 0.341 |
Categories reported by less than 5% of respondents are not presented. Total reported values in percentages include combined spontaneous and probed responses. Fisher's exact test was used for pre-ulcer and ulcer comparisons.
Narratives suggested that herbs were often obtained from the backyard. Herbal dressings were placed on pre-ulcers so that the skin would open up and expose the odonti (local term for necrotic tissues, meaning cotton wool). Herbal dressings were then directly applied to the exposed wound to speed up healing. When nodules did not burst, herbalists slit them open. Leftover analgesics at home or purchased across the counter from local chemists were often taken to ease the pain, and ointments and balms were used to reduce swellings. Blood tonics were taken to strengthen the blood because respondents often mentioned that they looked pale, felt weak, or were anemic as a result of their illness. Some respondents attributed edemas to evil spells because of the swelling of affected body parts and applied ointments to reduce swelling. An adult explained:
“It started as a sharp burning sensation with pain, and the skin looked red. I believe that someone placed some juju (black magic) at my work place. I applied some ointments at home to the affected part to reduce swelling” (38-year-old male respondent).
Adult respondents with ulcers commonly explained the need for quick recovery to continue working and fulfill family support obligations, as reasons for using home-based remedies.
Approximately 26% of respondents with pre-ulcers and 32.6% with ulcers (P = 0.003) did nothing for their conditions at home, and reasons for this finding varied. Some said' they thought nodules were ordinary boils that would burst in time, and because nodules were painless, they thought they posed no immediate health concern. Respondents were cautious with interventions for edemas, which they called swellings, because of fear that the condition could be made worse. They expressed a need to confer with family members and friends about types of treatment to use. Some respondents also mentioned difficulty identifying edemas and plaques as pre-ulcer infections. They described the cause of their illness as small scratches, bruises, or swellings sustained through work-related activities or play; these lesions were initially dismissed as trivial. Respondents who said they did nothing for ulcer conditions either said they had not yet sought help because they wanted to confer with neighbors, relatives or friends on what to do, or they just did not know what to do.
Outside help-seeking.
Respondents sought outside help for pre-ulcers and ulcers from traditional and faith healers, private doctors and facilities, and government health facilities. Analgesics, antibiotics, balms, ointments, and blood tonics were also obtained from itinerant drug peddlers and chemist shops. Aside from the health worker (minimal training), and respondents who did not seek help, significant differences were observed for all other providers (Table 3). Generally, most respondents reported that they sought treatment from the herbalist first, both for pre-ulcers (42.5%) and ulcers (47.5%). Although herbalists were frequently consulted for pre-ulcers and ulcers, respondents were more inclined to seek medical help from government health facilities for ulcers (66.9%) than for pre-ulcers (17.1%; P = 0.003) (Table 3). Furthermore, respondents with ulcers considered medical treatment from government health facilities as the most helpful provider type (51.9%; P = 0.042) (Table 3). They were also more likely to use medical facilities first for ulcers (20%) than pre-ulcers (10.5%). Diagnostic difficulty and the fear of possible deformities prompted some respondents to seek medical care for pre-ulcers. Health facilities used most were the municipal health hospital and clinics, where WHO-recommended antibiotics and surgery are administered.
Table 3.
Outside help among respondents with pre-ulcers and ulcers, Ghana*
| Category of outside help-seeking | Total reported | Most helpful | ||||
|---|---|---|---|---|---|---|
| Pre-ulcers (n = 181) | Ulcers (n = 181) | P | Pre-ulcers (n = 181) | Ulcers (n = 181) | P | |
| Traditional and faith healers | 54.7 | 58.5 | < 0.001 | 46.4 | 24.9 | < 0.001 |
| Herbalist | 49.2 | 53.0 | < 0.001 | 32.6 | 18.2 | 0.004 |
| Fetish spiritualist | 13.3 | 16.0 | < 0.001 | 7.2 | 5.5 | < 0.001 |
| Prayer camp | 14.9 | 19.3 | < 0.001 | 6.6 | 1.1 | 0.004 |
| Private health practitioners | 12.2 | 26.5 | < 0.001 | 4.2 | 3.9 | 0.007 |
| Health worker (minimal training) | 9.9 | 17.7 | < 0.018 | 3.3 | 0.6 | 1 |
| Private practitioner (trained) | 5.5 | 16.6 | < 0.016 | 1.1 | 3.3 | 1 |
| Government health facilities | 17.1 | 66.9 | 0.003 | 12.2 | 51.9 | 0.042 |
| Health center (Obom/Amasaman) | 14.4 | 58.0 | 0.002 | 9.9 | 41.4 | 0.083 |
| Government hospital outside the district | 2.8 | 18.8 | 0.237 | 2.2 | 10.5 | 0.055 |
| None | 33.2 | 13.8 | 0.110 | 31.5 | 14.9 | 0.122 |
| Others (analgesics, antibiotics, and balms obtained from drug peddlers or chemist shops) | 8.3 | 8.3 | < 0.001 | 5.5 | 4.4 | < 0.001 |
Grouped categories in bold were computed from responses. Categories reported by less than 5% of respondents are not presented but are included in group totals. Total reported values in percentages include combined spontaneous and probed responses. Fisher's exact test was used for pre-ulcer and ulcer comparisons.
Private health practitioners were also consulted by 26.5% of respondents with ulcers and 12.2% of respondents with pre-ulcers (P < 0.001) (Table 3). Narratives suggest that respondents used the services of private health practitioners for pain relief and because they lived nearby. Private health practitioners treated most respondents in their homes and often administered injections to prevent tetanus infection or to halt the spread of infection to other parts of the affected limb. Two narratives of respondents with ulcers indicate the rationale, referring to desire for a more effective alternative, perceived need for a specific intervention or motivation to respond to functional disability:
“Herbal treatment was not helping so I had to seek help from the private clinic, but this hasn't worked either. It was very close to my house and people in the community were urging me to seek medical care” (61 year-old female respondent).
“When I could not move my leg, a private practitioner from Adeiso (a neighboring community) came to inject me until I could move my leg” (20 year-old male respondent).
A respondent with a pre-ulcer used a private health practitioner based on the perceived need to prevent tetanus infection:
“A private practitioner was injecting me at home. I needed to take some tetanus injections” (15 year-old female respondent).
Narratives revealed that adults who had previously been infected relied on their prior personal experience to make choices for outside help. However, some respondents had no prior knowledge of Buruli ulcer and realized the nature of their conditions after conferring with friends, neighbors, community-based surveillance volunteers, and sometimes municipal health staff during community health programs. Some respondents also mentioned that they were referred to the municipal health centers by health workers, CBSVs, family, and friends. They expressed their desire for medical treatment but mentioned the need to save money to pay for transportation and hospitalization. Adult respondents also worried about their absence from home and the need to find someone to take care of the family during their absence. Some respondents did not have to travel for herbal treatment. There were itinerant herbalists, and some herbalists were relatives who offered their assistance at no cost. Some of these herbalists were known to have treated Buruli ulcer–affected persons. In their accounts, respondents frequently mentioned that these herbalists assured them that they could treat the sickness, and they were displeased when respondents decided to abandon herbal treatment and seek medical treatment.
Children made use of self-help or outside help selected by their parents. Infected school children who did not want their education disrupted and parents who wanted to protect their livelihoods used a combination of various providers to lessen the pain and suffering to achieve recovery. Narratives suggested that some infected children living near health facilities where Buruli ulcer treatment was available received daily antibiotic treatment and had their wounds dressed before proceeding to school.
Generally, it was common practice for respondents to use a combination of self-help and outside help approaches to seek relief. A mother explained that her treatment approach had been influenced by insufficient money to take her child to the hospital, the need for a quick recovery to go back to school, and the absence of a caregiver to take care of the home or stay in hospital with a sick child:
“I ground some herbs and mixed it with palm kernel oil and applied it to my son's sore. I also used the bark of the orange tree mixed with palm kernel oil as a dressing. I bought some castor oil from the chemist shop and placed it on the sore, which has helped to remove the odonti. When I went to the drug store to buy the oil, the store keeper asked me what I was going to do with it. When I told him, he advised me to take my child to the hospital but I did not have money. I did not want my son's condition to get worse. That is why I went to the drug store to purchase castor oil. I also bought penicillin v powder and ampicillin, mixed them together and used it on the sore. There is no one else to take care of the other children at home, and I am pregnant now. I will be giving birth soon, that is why I did not go to the hospital” (mother of 10 year-old child).
Factors influencing choice of first outside help for pre-ulcers and ulcers are shown in Table 4. Choices of treatment of first outside help for pre-ulcers and ulcers were influenced by the perceived effectiveness of treatment, the closeness of the provider to the place of residence, and the influence of family and friends. Preferences differed significantly. There appeared to be little influence from professional health workers and CBSVs. Independent of the influence of family and friends, respondents also made decisions on their own about which provider to consult first for pre-ulcers (62.9%) and ulcers (62.3%; P < 0.001) (Table 4). Narratives suggested that most adult respondents used the services of herbalists first for outside help so they could stay close to the home to work and earn income.
Table 4.
Reasons for first-help seeking among respondents with pre-ulcers and ulcers, Ghana*
| Reason | Pre-ulcers (n = 124), % | Ulcers (n = 154), % | P |
|---|---|---|---|
| Treatment is very effective | 54.8 | 61.7 | 0.206 |
| Closeness to home | 54.0 | 42.9 | < 0.001 |
| Affordable | 23.4 | 20.8 | < 0.001 |
| Self-referral | 62.9 | 62.3 | < 0.001 |
| Referral by family/friends | 71.0 | 70.1 | < 0.001 |
| Referral by health worker (professional) | 8.0 | 13.0 | 0.002 |
| Referral by CBSV | 7.2 | 4.0 | 1 |
| Education through IEC activities | 10.5 | 9.7 | 0.031 |
| Medical treatment is effective | 21.0 | 21.4 | < 0.001 |
| Herbal treatment is not effective | 17.7 | 21.4 | 0.119 |
Shown are responses of persons who sought outside help; responses of those who did not seek outside help are not included. Categories reported by less than 5% of respondents are not presented. Total reported values in percentages include combined spontaneous and probed responses. Fisher's exact test was used for pre-ulcer and ulcer comparisons. CBSV = community-based surveillance volunteers; IEC = information, education, and communication.
Perceived effectiveness of treatment from providers.
Respondents ranked their perceptions of the effectiveness of treatment from providers on a three-point scale: effective, dissatisfied, and ineffective. Treatment was considered effective when it fulfilled respondents' expectations of slowing disease progression and recovery. Respondents were dissatisfied withtreatment when it was perceived as having some value, but was so too slow-acting and failed to meet expectations. Treatment regarded as ineffective did not have any impact on respondent's disease status. Respondents who consulted herbalists for ulcers expressed their misgivings on the effectiveness of herbal treatment; 12.5% said it was effective, 49.0% were dissatisfied, and 38.5% said it was ineffective. Medical treatment at the government hospitals and municipal health centers was valued more than herbal treatment; 41% of respondents considered medical treatment effective, 48.2% were dissatisfied, and 11.0% said it was ineffective (Figure 1). Treatment at health facilities was regarded as significantly more effective than treatment from all the other providers.
Figure 1.
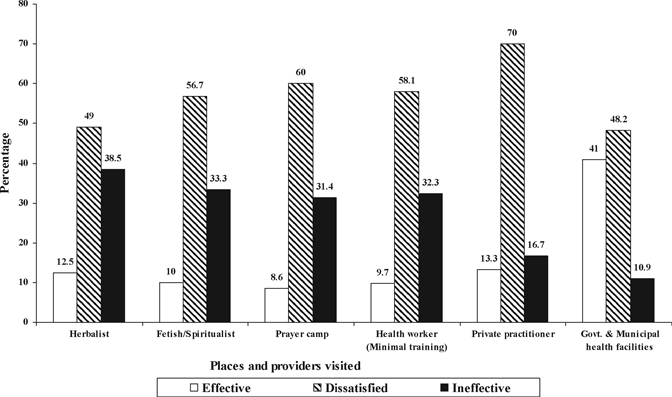
Respondents perceptions of the effectiveness of treatment of ulcers, Ghana.
Respondents' explanations of their dissatisfaction with herbal treatment reflected disappointment in the slow process of recovery, despite assurances from the herbalists of effective treatment and cure. Those persons who mentioned that herbal treatment was ineffective did not see any change in their disease status; some said their condition worsened. Narratives showed that medical care was valued because respondents said it cleans the sore, implying that it clears the odonti. Respondents who were dissatisfied with medical care appeared dissuaded by hospitalization and slow healing of ulcers, which disrupted their normal work routines and family life. Nevertheless, as ulcer conditions worsened and pain became unbearable, hospital care became the second option for outside help after traditional care. One adult explained how failure of home-based treatment to treat his condition and the desire to recover to continue with work, necessitated medical treatment:
“I was applying balms and ointments at home, but there was no improvement. I decided to come here (Amasaman hospital). I have been away from work for a long time because of this condition. I am the one who supports the family. I do not know what to do now” (35-year-old male respondent).
Discussion
Study findings highlight the preference for herbal treatment of pre-ulcers and ulcers, and indicate that respondents are more likely to seek medical care for ulcers than pre-ulcers. This finding reflects a need to respond to the higher level of distress for ulcers. Findings present a challenge for Buruli ulcer prevention and management because a considerable proportion of respondents did not seek help for pre-ulcers and ulcers in as much, which delayed medical treatment, and increased risk of serious ulcerative disease sequelae.
Our study complements findings of earlier sociocultural studies of Buruli ulcer3,9,16,17 and clarifies help-seeking for pre-ulcers and ulcers of persons affected by Buruli ulcer. This information is critical for health programming in the Ga-West and Ga-South municipalities, where sociocultural research has been lacking. The first sociocultural study of Buruli ulcer in the Ga-West municipality in 2005 explored community perceptions of Buruli ulcer, in which 71.8% of sampled heads of households indicated herbal treatment as the preferred treatment and stated that 7.7% of affected persons would go to the hospital if their illness got worse and 48.2% would use a local doctor or nurse. Additionally, 72% of respondents said there was no program in place to address Buruli ulcer.9 Since then, there has been a public health initiative to create awareness about Buruli ulcer and availability of medical care, improve case-management, and access to care. Our study not only supports previous findings of this study9 about herbal medicine as the first treatment choice, but shows evidence of increasing awareness and use of medical treatment, and clarifies current treatment needs and gaps for Buruli ulcer. The study also draws attention to some sociocultural features of help-seeking, especially difficulties in diagnosing pre-ulcers, reliance on help-seeking advice from a network of friends and family (which include herbalists), and the itinerant nature of herbal treatment.
Study findings suggest that respondents had a fair knowledge of local herbs that were easily obtained from the backyard and used as first aid. A significant proportion of respondents placed these herbal dressings on pre-ulcer lesions to open the skin. Nodules were also excised. Both practices heightened the transformation of pre-ulcers into ulcers. Although the health impact of these local practices has not been documented adequately, secondary infection could be a likely result. Another home remedy was indiscriminate use of analgesics and leftover antibiotics to reduce pain and inflammation. Use of self-medication for Buruli ulcer has been reported in a study in Benin.7 Indiscriminate use of antibiotics is a concern because of potentially undesirable health effects18 and implications for treatment, recovery, and pharmacodynamic interactions with WHO-recommended antibiotics (rifampin and streptomycin) when given later to respondents at health centers.
A considerable proportion of respondents did not seek treatment for their pre-ulcers and ulcers, and various reasons were given for this behavior. For pre-ulcers, these reasons included a genuine difficulty in diagnosing illness conditions, perceived imminence of disease progression and severity, and absence of pain and disability, which enabled them to carry on with normal routines of work and school. Respondents with pre-ulcers needed to confer with family or friends for advice on provider type, or simply did not know what to do. Findings, particularly narratives, indicate a genuine difficulty in diagnosing some pre-ulcer conditions, which is consistent with prior research findings.15 Perceptions of the imminent severity or progression of Buruli ulcer have been identified as a contributing factor for delay in seeking medical treatment.7,17 Buruli ulcer is known to affect poor, rural communities.9,11,19–22 Only 19% of our respondents received a regular income, 26.0% were unskilled workers, mainly subsistence farmers or petty traders, and most (55.3%) were in school.
Therefore, it is not unusual for study respondents to be concerned about securing their livelihoods and worry about disruption of education. These concerns have also been documented in other studies of Buruli ulcer.3,23 Furthermore, studies have linked delayed medical treatment for Buruli ulcer with other social issues of access and transportation costs.3,7,9,23 Therefore, some respondents used the services of nearby private health practitioners. Although it can be argued that private health practitioners provided medical treatment, the capacity of private practice to provide the recommended treatment for Buruli ulcer is doubtful and should be explored further.
Respondents with ulcers often sought advice for treatment options from family and friends, although a considerable proportion sought treatment on their own volition. Evidence from other studies on help-seeking for Buruli ulcer,7 malaria,24 and tuberculosis25 suggest that it is common for persons to rely on help-seeking advice from a network of friends and family. It is not clear from our study whether the advice from family and friends influenced the use of herbal treatment more than medical treatment. However, there is evidence from our study to suggest that some family and friends referred respondents to the appropriate health facilities for care. Considering the debilitating and distressing nature of Buruli ulcer, a network of family and friends is beneficial for emotional and social support. The influence of professional health staff and CBSVs on help-seeking for pre-ulcers and ulcers was minimal. Earlier research in our study municipalities showed the importance of community-based surveillance activities from CSBVs and health professionals to detect early cases, increase awareness of Buruli ulcer, and availability and effectiveness of WHO-recommended antibiotic treatment.15 Community-based surveillance has been used successfully for early case detection and in the management of Buruli ulcer in the study municipalities15 and for Guinea worm eradication programs.26
The presence of herbalists in the family (fathers, grandfathers, and uncles) and other itinerant herbalists made herbal treatment readily available and influenced respondent's choice of herbal treatment. The insistence of these herbalists to treat Buruli ulcer conditions resulted in delay of respondents starting medical treatment. Evidence from our study and other studies3,9,11 shows how prior use of herbalists delays medical care. Therefore, the role of herbalists as first outside help for most respondents who had pre-ulcers and ulcers provides a big challenge with respect to early medical care for Buruli ulcer public health programs.
Respondents had mixed feelings about the effectiveness of herbal treatment because of the prolonged period of treatment. There is evidence from our study that respondents who had benefited from medical care from government health facilities considered it a better option than herbal treatment, and treatment from other providers. This finding was due to the fact that they had clean wounds and experienced an improvement in their illness condition, particularly after antibiotic treatment with rifampin and streptomycin for eight weeks. Despite the benefits of medical care, herbal treatment was the first choice for most persons because it was easily accessible and provided the opportunity to continue with the normal routines of work and school. With increasing number of persons experiencing improvement in disease outcomes, affected persons might limit their dependence on herbal treatment.
Although there is paucity of research on the use of herbs for Buruli ulcer treatment and management, a study in Ghana has shown the effectiveness of herbal preparations, commonly used in treatment for Buruli ulcer, to inhibit Mycobacterium ulcerans activity in vitro.27 These herbs possess extended antimicrobial activity, which might simultaneously eliminate secondary infections associated with Buruli ulcer.27 The WHO encourages countries to integrate traditional medicine in the health system to improve access to health care for poor, rural populations.28 Ghana has a WHO collaborating research center for herbal medicine. There is also a national policy on traditional medicine and complementary and alternative medicine. Although the Ministry of Health in Ghana must ensure inclusion of herbal medicine and complementary and alternative medicine in the national health care system, it has failed to do this effectively.28 Nevertheless, to enhance research and practice of herbal medicine, the Kwame Nkrumah University of Science and Technology in Ghana introduced a program in 2001, the first in Africa,29 to train medical or science students in herbal medicine. Hopefully, with the increasing numbers of graduates from this program, known as medical herbalists, the use of herbal medicine would be streamlined into the main health care system, making it accessible to poor rural communities for the treatment of neglected tropical diseases such as Buruli ulcer.
This study was undertaken to examine help-seeking for pre-ulcers and ulcers. There is the likelihood of recall bias because study data was mainly based on reported and not directly observed help-seeking behavior for affected persons with Buruli ulcer. Considering the ad hoc use of home-based remedies and self medication, under-reporting is possible for these help-seeking practices. Because respondents with ulcers had to provide information on prior help-seeking for pre-ulcers, we presume a greater recall bias with respect to help-seeking for pre-ulcers for respondents with ulcers than those with pre-ulcers. Probes were used to minimize recall bias and under-reporting. Nevertheless, study findings are clearly relevant for the study communities, might have a broader relevance for other Buruli ulcer–endemic communities in the country, and clarify the sociocultural dimensions of help-seeking.
Nevertheless, our study findings have implications for community awareness of Buruli ulcer, particularly the pre-ulcer stages of infection, early and appropriate medical care, and access to appropriate health care. Other issues are the limited role of herbalists in the health system, the involvement of the community as disseminators of appropriate health messages, and treated patients as advocates for appropriate help-seeking. The following recommendations, based on study findings, should be considered.
Health education is required first to emphasize the risk of self-medication particularly with antibiotics, and the imminent danger of co-infection by exposing the necrotic tissue through local incision and the application of herbs on pre-ulcers, which may prolong healing. Health education should also highlight the effectiveness of treatment with WHO-recommended antibiotics for eight weeks for early lesions.1,30,31 This treatment might minimize deformities, the need for surgery, and consequently prolonged hospitalization, thus reducing the social burden of suffering and disruption of livelihoods and education. Health education must point out that Buruli ulcer is an ordinary disease and can be medically treated. Reliance on family and friends provides a basis for establishing community-based health education initiatives.
Health education initiatives can be sustained and expanded by creating a network of educators to include everyone in the community: former patients, community representatives, school teachers, parents, and community members. Support groups could be formed with successfully treated former patients to promote awareness and advocate for early medical treatment by sharing stories about treatment and its impact on social life. To ensure the effectiveness of health education programs, encourage early medical treatment, and improve access to antibiotic treatment, more treatment centers must be provided. Private health practitioners are a useful resource to improve access to antibiotic treatment of pre-ulcers and consequently encourage early medical treatment. Their inclusion in the health system as service providers should be considered. To ensure effective management of Buruli ulcer, public health programs must increase awareness of all stages of Buruli ulcer for easy recognition; encourage medical treatment of all suspicious stings, bites, and lesions; and encourage affected persons to confer with CBSVs and health professionals when in doubt of Buruli ulcer. Furthermore, community-based surveillance activities and periodic community health screening programs are also critical to identify pre-ulcer cases and refer them for medical treatment.
The challenge facing Buruli ulcer public health programs in the Ga-West and Ga-South municipalities is to dissuade affected persons from seeking herbal treatment first, and to minimize the influence of herbalists on provider choice. A complementary strategy should consider the potential role of herbalists as advocates for early medical care. This approach has not been considered or researched adequately. However, on the basis of the finding that some herbalists are family members, opportunities may exist to train them as health educators and advocates for change. First, health workers would have to gain the confidence of herbalists by acknowledging their role as traditional health providers and consider them partners. Collaborating with herbalists would enable them to refer patients for timely treatment and make a major contribution to control of Buruli ulcer.
Further research on effectiveness of herbs in treatment for Buruli ulcer is necessary. This research will improve herbalists' knowledge of the curative abilities of the herbs they use and enhance the scientific uses and benefits. These findings are also beneficial to a wider community of pharmacists, medical personnel, scientists, researchers, and academicians. Herbal medicine features strongly in health care for most persons in Ghana, not only for Buruli ulcer,9,17 but for other illnesses, such as malaria.32 Therefore, consideration should be given to inclusion of herbal medicine in the health system.
Our study findings show how sociocultural factors, the social context of poverty, and the need to secure livelihoods and prevent the disruption of education influenced help-seeking behavior. They also show how appreciation of sociocultural features of help-seeking can guide public health programs. Sociocultural studies of help-seeking are important assessments of achievements, and performance of the health system in control of Buruli ulcer. However, help-seeking behaviors are influenced by the sociocultural context of affected persons, which could change with exposure to health information and improvement in socioeconomic status. This indicates the need for regular sociocultural studies to guide public health programs to address current treatment needs and gaps.
ACKNOWLEDGMENTS
We thank the Municipal Health Directorates of the Ga-West and Ga-South municipalities, the staff at the Buruli ulcer ward, Amasaman Hospital, and Florence Foli for assistance; Donald Okine for acting as a field driver; and the respondents for participating in the study.
Footnotes
Financial support: This study was supported by the World Health Organization Global Buruli Ulcer Initiative.
Authors' addresses: Mercy M. Ackumey, School of Public Health, College of Health Sciences, University of Ghana, Legon, Ghana, and Swiss Tropical and Public Health Institute, University of Basel, Socinstrasse 57, CH-4002, Basel, Switzerland, E-mail: Mercy.Ackumey@unibas.ch. Mitchell G. Weiss, Swiss Tropical and Public Health Institute, University of Basel, Socinstrasse 57, CH-4002, Basel, Switzerland, E-mail: Mitchell-G.Weiss@unibas.ch. Margaret Gyapong, Dodowa Health Research Centre, Ghana Health Service, Dodowa, Ghana, E-mail: margaret.gyapong@ghsmail.org. Matilda Pappoe, School of Public Health, College of Health Sciences, University of Ghana, Legon, Ghana, E-mail: matildapappoe@yahoo.co.uk.
References
- 1.World Health Organization Buruli ulcer: progress report, 2004–2008. Wkly Epidemiol Rec. 2008;83:145–154. [PubMed] [Google Scholar]
- 2.Amofah GK, Sagoe-Moses C, Adjei-Acquah C, Frimpong EH. Epidemiology of Buruli ulcer in Amansie West district, Ghana. Trans R Soc Trop Med Hyg. 1993;87:644–645. doi: 10.1016/0035-9203(93)90272-r. [DOI] [PubMed] [Google Scholar]
- 3.Asiedu K, Etuaful S. Socioeconomic implications of Buruli ulcer in Ghana: a three-year review. Am J Trop Med Hyg. 1998;59:1015–1022. doi: 10.4269/ajtmh.1998.59.1015. [DOI] [PubMed] [Google Scholar]
- 4.Marston BJ, Diallo MO, Horsburgh CR, Jr, Diomande I, Saki MZ, Kanga JM, Patrice G, Lipman HB, Ostroff SM, Good RC. Emergence of Buruli ulcer disease in the Daloa region of Côte d'Ivoire. Am J Trop Med Hyg. 1995;52:219–224. doi: 10.4269/ajtmh.1995.52.219. [DOI] [PubMed] [Google Scholar]
- 5.Johnson PD, Stinear T, Small PL, Pluschke G, Merritt RW, Portaels F, Huygen K, Hayman JA, Asiedu K. Buruli ulcer (M. ulcerans infection): new insights, new hope for disease control. PLoS Med. 2005;2:e108. doi: 10.1371/journal.pmed.0020108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amofah G, Bonsu F, Tetteh C, Okrah J, Asamoa K, Asiedu K, Addy J. Buruli ulcer in Ghana: results of a national case search. Emerg Infect Dis. 2002;8:167–170. doi: 10.3201/eid0802.010119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mulder AA, Boerma RP, Barogui Y, Zinsou C, Johnson RC, Gbovi J, van der Werf TS, Stienstra Y. Healthcare seeking behaviour for Buruli ulcer in Benin: a model to capture therapy choice of patients and healthy community members. Trans R Soc Trop Med Hyg. 2008;102:912–920. doi: 10.1016/j.trstmh.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 8.Phanzu DM, Bafende EA, Dunda BK, Imposo DB, Kibadi AK, Nsiangana SZ, Singa JN, Meyers WM, Suykerbuyk P, Portaels F. Mycobacterium ulcerans disease (Buruli ulcer) in a rural hospital in Bas-Congo, Democratic Republic of Congo, 2002–2004. Am J Trop Med Hyg. 2006;75:311–314. [PubMed] [Google Scholar]
- 9.Renzaho AM, Woods PV, Ackumey MM, Harvey SK, Kotin J. Community-based study on knowledge, attitude and practice on the mode of transmission, prevention and treatment of the Buruli ulcer in Ga West District, Ghana. Trop Med Int Health. 2007;12:445–458. doi: 10.1111/j.1365-3156.2006.01795.x. [DOI] [PubMed] [Google Scholar]
- 10.Sizaire V, Nackers F, Comte E, Portaels F. Mycobacterium ulcerans infection: control, diagnosis, and treatment. Lancet Infect Dis. 2006;6:288–296. doi: 10.1016/S1473-3099(06)70464-9. [DOI] [PubMed] [Google Scholar]
- 11.Webb BJ, Hauck FR, Houp E, Portaels F. Buruli ulcer in West Africa: strategies for early detection and treatment in the antibiotic era. East Afr J Public Health. 2009;6:144–147. doi: 10.4314/eajph.v6i2.51744. [DOI] [PubMed] [Google Scholar]
- 12.Ga-South Municipal Directorate Greater Accra—Weija Municipal Demographic Characteristics. 2011. http://www.ghanadistricts.com/districts/?r=1&_=169&sa=6052 Available at. Accessed May 25, 2011.
- 13.World Health Organization, Global Buruli Ulcer Initiative . Recognizing Buruli Ulcer in Your Community. Geneva: World Health Organization; 1998. [Google Scholar]
- 14.Weiss MG. Explanatory model interview catalogue (EMIC): framework for comparative study of illness. Transcult Psychiatry. 1997;34:235–263. [Google Scholar]
- 15.Ackumey MM, Kwakye-Maclean C, Ampadu EO, de Savigny D, Weiss MG. Health services for Buruli ulcer control: lessons from a field study in Ghana. PLoS Negl Trop Dis. 2011;5:e1187. doi: 10.1371/journal.pntd.0001187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aujoulat I, Johnson C, Zinsou C, Guedenon A, Portaels F. Psychosocial aspects of health seeking behaviours of patients with Buruli ulcer in southern Benin. Trop Med Int Health. 2003;8:750–759. doi: 10.1046/j.1365-3156.2003.01089.x. [DOI] [PubMed] [Google Scholar]
- 17.Stienstra Y, van der Graaf WT, Asamoa K, van der Werf TS. Beliefs and attitudes toward Buruli ulcer in Ghana. Am J Trop Med Hyg. 2002;67:207–213. doi: 10.4269/ajtmh.2002.67.207. [DOI] [PubMed] [Google Scholar]
- 18.Reeves DS, Finch RG, Bax RP, Davey PG, Po AL, Lingam G, Mann SG, Pringle MA. Self-medication of antibacterials without prescription (also called ‘over-the-counter' use). A report of a Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother. 1999;44:163–177. doi: 10.1093/jac/44.2.163. [DOI] [PubMed] [Google Scholar]
- 19.Huygen K, Adjei O, Affolabi D, Bretzel G, Demangel C, Fleischer B, Johnson RC, Pedrosa J, Phanzu DM, Phillips RO, Pluschke G, Siegmund V, Singh M, van der Werf TS, Wansbrough-Jones M, Portaels F. Buruli ulcer disease: prospects for a vaccine. Med Microbiol Immunol (Berl) 2009;198:69–77. doi: 10.1007/s00430-009-0109-6. [DOI] [PubMed] [Google Scholar]
- 20.Kibadi K. Streptomycin injections for the treatment of Mycobacterium ulcerans (Buruli ulcer) in a rural health zone in the Democratic Republic of the Congo [in French] Sante. 2007;17:173–176. doi: 10.1684/san.2007.0083. [DOI] [PubMed] [Google Scholar]
- 21.Portaels F, Silva MT, Meyers WM. Buruli ulcer. Clin Dermatol. 2009;27:291–305. doi: 10.1016/j.clindermatol.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 22.Yemoa A, Gbenou J, Affolabi D, Moudachirou M, Bigot A, Anagonou S, Portaels F, Quetin-Leclercq J, Martin A. Buruli ulcer: a review of in vitro tests to screen natural products for activity against Mycobacterium ulcerans. Planta Med. 2011;77:641–646. doi: 10.1055/s-0030-1250642. [DOI] [PubMed] [Google Scholar]
- 23.Grietens KP, Boock AU, Peeters H, Hausmann-Muela S, Toomer E, Ribera JM. “It is me who endures but my family that suffers”: social isolation as a consequence of the household cost burden of Buruli ulcer free of charge hospital treatment. PLoS Negl Trop Dis. 2008;2:e321. doi: 10.1371/journal.pntd.0000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samuelsen H. Illness transmission and proximity: local theories of causation among the Bissa in Burkina Faso. Med Anthropol. 2004;23:89–112. doi: 10.1080/01459740490448885. [DOI] [PubMed] [Google Scholar]
- 25.Nyika A. The ethics of improving African traditional medical practice: scientific or African traditional research methods? Acta Trop. 2009;112((Suppl 1):):S32–S36. doi: 10.1016/j.actatropica.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cairncross S, Braide EI, Bugri SZ. Community participation in the eradication of guinea worm disease. Acta Trop. 1996;61:121–136. doi: 10.1016/0001-706x(95)00106-o. [DOI] [PubMed] [Google Scholar]
- 27.Addo P, Quartey M, Abass KM, Adu-Addai B, Owusu E, Okang I, Dodoo A, De Souza D, Ankrah N, Ofori-Adjei D. (In vitro susceptibility of Mycobacterium ulcerans to herbal preparations).Internet J Trop Med. 2008;4 http://www.ispub.com/journal/the_internet_journal_of_tropical_medicine/archive/volume_4_number_2_47.html Available at. Accessed September 15, 2011. [Google Scholar]
- 28.World Health Organization . WHO Traditional Medicine Strategy 2002–2005. Geneva: World Health Organization; 2002. [Google Scholar]
- 29.Adusi-Poku Y, Okine LK, Hlortsi-Akakpo FK, Fleischer TC, Mensah ML, Arhin P, Agyemfra G, Dabra T, Mensah EN. Assessing herbal medical practitioners in professional qualifying examination in Ghana, a model. Afr J Tradit Complement Altern Medicines. 2010;7:85–87. [PMC free article] [PubMed] [Google Scholar]
- 30.Nienhuis WA, Stienstra Y, Thompson WA, Awuah PC, Abass KM, Tuah W, Awua-Boateng NY, Ampadu EO, Siegmund V, Schouten JP, Adjei O, Bretzel G, van der Werf TS. Antimicrobial treatment for early, limited Mycobacterium ulcerans infection: a randomised controlled trial. Lancet. 2010;375:664–672. doi: 10.1016/S0140-6736(09)61962-0. [DOI] [PubMed] [Google Scholar]
- 31.Chauty A, Ardant MF, Adeye A, Euverte H, Guedenon A, Johnson C, Aubry J, Nuermberger E, Grosset J. Promising clinical efficacy of streptomycin-rifampin combination for treatment of Buruli ulcer (Mycobacterium ulcerans disease) Antimicrob Agents Chemother. 2007;51:4029–4035. doi: 10.1128/AAC.00175-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Asase A, Oppong-Mensah G. Traditional antimalarial phytotherapy remedies in herbal markets in southern Ghana. J Ethnopharmacol. 2009;126:492–499. doi: 10.1016/j.jep.2009.09.008. [DOI] [PubMed] [Google Scholar]


