Abstract
We need more clinical trials in the world's poorest regions to evaluate new drugs and vaccines, and also to find better ways to manage health issues. Clinical trials are expensive, time consuming, and cumbersome. However, in wealthier regions these limiting factors are being addressed to make trials less administrative and improve the designs. A good example is adaptive trial design. This innovation is becoming accepted by the regulators and has been taken up by the pharmaceutical industry to reduce product development times and costs. If this approach makes trials easier and less expensive surely we should be implementing this approach in the field of tropical medicine and international health? As yet this has rarely been proposed and there are few examples. There is a need for raising the awareness of these design approaches because they could be used to make dramatic improvements to clinical research in developing countries.
Introduction
Clinical trials stand to bring the most benefit to regions of the world most affected by disease, however these communities are underrepresented in trials and these regions have limited capacities for research. In Europe and the United States the pharmaceutical industry's drug and vaccine development programs have benefited greatly from using adaptive design in clinical trials as fewer patients are needed and development times can be drastically lowered. As yet these methods are sparsely in academic studies and rarely, if at all, in the field of Global Health. Some of the highest causes of death in the world's poorest regions could be improved by making changes in the way the disease is managed or simply by changing the way existing treatments are used, but these changes require evidence gathered through clinical research. These disease management studies could be particularly well suited to adaptive design because one of the main features is that this approach moves away from the standard phase I, II, and III model of separate protocols to a single study that adapts flexibly in real time as knowledge is gained. Disease management trials could logically and safely progress from the learning phase to confirmatory within a single protocol. This would save time and money and bring about evidence for improvement compared with conventional methods that are now being used through traditional clinical trial design approaches (Figure 1).
Figure 1.
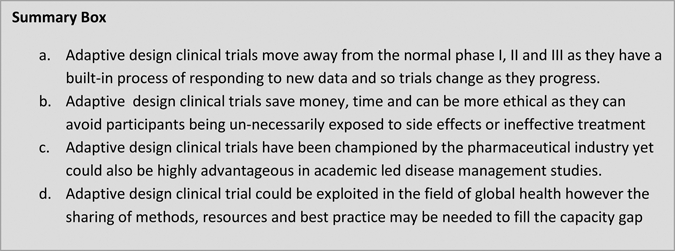
Summary box.
What is adaptive trial design?
Adaptive design is a relatively new approach to clinical studies that is being increasingly used within the pharmaceutical industry.1 It is recognized that conventional randomization can be ethically infeasible as it gathers information and ignores current knowledge.2 This design approach has an in-built capacity to change the study; in fact, the very point is to change the study while it is in process without compromising the integrity of the trial. Adaptive design moves away from the traditional phase I–III categories and allows within a single protocol the ability to move between what would be the normal divides between the phases in clinical trials. In drug and vaccine development the use of adaptive design shortens product development time and therefore is very cost-effective for industry.3–5 However, adaptive design is still not mainstream, which many find surprising.2
Adaptive clinical trial design is defined as a design that allows modifications to the trial and/or statistical procedures of the trial after its initiation without undermining its validity and integrity. The role of adaptive design is to make clinical trials more flexible, efficient, and fast. Because of the level of flexibility involved, these trial designs are also termed as flexible designs. In essence a clinical trial that uses adaptive design allows, and indeed plans for, substantial change as the trial progresses without the need for a separate new study or a protocol amendment.
In the setting of clinical trials in Global Health adaptive design could be very exciting, not only for product development time but for disease management trials where the approach could be used effectively. In disease management trials the typical phase I, II, and III approaches are applied but this is cumbersome and often illogical as these phases were developed to facilitate new drug and vaccine registration trials. In disease management trials a more pragmatic and rationale approach is needed and adaptive design could work well. Although the use of adaptive design is being widely championed, the opportunities that this approach could bring to research in developing countries has not been considered.6
For example, let us use the theoretical example of giving an intramuscular antibiotic preventative treatment before delivery to assess whether the incidence of maternal and neonatal sepsis can be reduced. This is a possible disease management question that a developing country research group might wish to explore. If the normal clinical development trial approach is used then there would be at least two trials, a phase II and then a phase III. The phase II trial would look closely at a small group of mothers in a tightly controlled setting, such as a maternity ward in a research facility, to establish safety and dose and get an indication of efficacy in the small numbers used. Once this study was completed, reported, and published the phase III trial could then be planned and further funding obtained. The phase III trial would then be the real test of efficacy, confirmation of safety, and give a better idea of effectiveness as a larger and more “real-life” situation would be used; therefore, in this case it could be community health centers rather than a hospital.
If an adaptive design approach had been used then all this could have been achieved within a single protocol. There is the obvious advantage of time and costs in only taking one protocol through the review and approval process and all the setup activities. This would be highly advantageous in the field of Global Health as these potentially life-saving new disease management approaches could be tested so much faster without the delay of waiting for each phase to be approved and receive funding. However, there is much more to adaptive design than just reducing the regulatory and approval steps. Adaptive design involves ongoing and detailed review of the data. This is fundamental to the approach and is the aspect that allows treatment arms to be added or dropped, new patient groups to be included and/or the dosage changed. This can also make trials more ethical as fewer patients are needed and the design should be such that it limits the exposure of participants to less effective treatment arms and to unexpected side effects.
There are some useful definitions and guidelines on adaptive design, which although written for drug and vaccine registration trials (as this is largely where the approach has been used), the concepts are helpful and adaptable to other trial settings. For example, the Food and Drug Administration (FDA) recently produced some guidelines for industry7 that include an explanation of how adaptive designs must be prospective: “The term prospective here means that the adaptation was planned (and details specified) before data were examined in an unblinded manner by any personnel involved in planning the revision.” The Drug Information Journal8 published an early work on this when the concept was just become recognized. The definition given here of “a clinical study design that uses accumulating data to decide on how to modify aspects of the study as it continues, without undermining the validity and integrity of the trial,” is often quoted as definitive.
When could it be useful?
Table 1 describes three possible adaptive trial designs. These examples are not finite, any number of approaches could be used in adaptive design because the aim is to be flexible and adapt the design as the data is gathered and knowledge is gained.
Table 1.
Types of adaptive trials
| Types of adaptive design | Description | Objective of design |
|---|---|---|
| Dose finding | Data is reported and extracted in interim reports in as short a time as possible, if technology allows this can be done in close to real time. The data is reviewed as it accumulates and then decisions can be taken and implemented on lowering or raising doses as determined in protocol. It is adaptive as there will not have been a set point where the dose is changed; the design is purposefully flexible and adaptive. | To avoid giving therapeutic doses, or to overdose. |
| Response adapting | Safety and efficacy data are captured as near to live as possible and further participants are randomized according to outcome of earlier participants. Some have called this a “play-the-winner” approach as subsequent participants are assigned to the treatment arm that has the best efficacy or fewer side effects. | To reduce exposure to an ineffective arm or to side effects. |
| Amending sample size | Sample sizes are based on assumptions and often there is too little information available that allow for accurate assumptions to be made.7 Therefore, many protocols set a sample size that may be too high or too small. The former results in a trial that exposes participants needless once the question has been answered and the latter results in the trial being unable to answer the question. In an adaptive design the limitation on the power calculations are acknowledged and as the trial begins to inform that assumption so the power calculation can be amended. | Allow the trial to run until the question has been answered and to avoid exposing participants to an experimental therapy unnecessarily. |
How do I conduct a trial using adaptive design?
To bring adaptive design to clinical trials in the field of Global Health there are two considerations that are likely to be the most pertinent. First the use of technology and second having strong statistical support as both of these are often lacking in resource-limited settings because of finances and capacity. However, neither should deter researchers and solutions can be sought that are pragmatic and appropriate. Here then we consider the processes in operating adaptive designs and the statistical input that is needed to design and implement the trial.
Time is important in the operation of an adaptive design trial. The ability to collect the data, enter it into whatever software is being used, extract this information, have it reviewed, and then implement the recommendation in close to real time is the key to success. In pharmaceutical trials there is increasing use of high technology to maximize efficiency and limit the time taken for this process.
In resource-limited settings, where trials addressing key questions in global health are mostly conducted, the use of new and expensive technology is limited. In industry, new technology has allowed this approach to become popular and enables real-time analysis of the data. However, systems can be designed that are not prohibitively expensive and the sharing of resources and methods between research groups could facilitate more groups using these methods.
The two most common technologies used are interactive voice response and electronic data capture. Let us first consider electronic data capture. This is becoming increasingly common in developing countries and many more groups are using open source products such as OpenClinica for their data management and these systems facilitate electronic data capture.9 Other groups are increasingly using the rapidly advancing use of handheld internet devices to capture clinical trial data in developing countries.10–12 This encouraging use of new technology by researchers makes the ability of using real-time data entry and extraction a realistic option for many developing country-based researchers.
Interactive voice recognition is a newer technology and more expensive. This is used by clinical trial groups in activities such as centralized randomization or dynamic treatment allocations through the use of a central data base. This is still relatively new and it does have its limitations13; in developing countries where computer and telephone access cannot always be relied upon, this may not always be feasible and the setup and operational costs could be limited. It should be considered, however, as it might be possible to devise a local scheme that offers the same feature and advantages. One possible solution would be to have an independent group responsible for allocation tasks that would operate a practical system within tight measures put in place to protect the blinding and general integrity of the trial.
A key operational step in the running of an adaptive trial will be establishing and managing the data monitoring committee and the surrounding steps and processes in reviewing the interim data sets, passing a decision, and implementing the recommendation. In developing countries, capacity for data monitoring committees is still largely limited14 and where there is experience it is unlikely to extend to the concepts and practices involved in adaptive trial designs. Therefore, the first groups running these trials will need to lead the way for others and establish systems and tools appropriate for this setting. It would be broadly beneficial if any such resources or guidance documents could then be shared with other groups.
Planning for an interim analysis is important,15 within this should be consideration of the key variables that should be cleaned before the dataset is released to a data monitoring committee.16 Although time is important, the validity and integrity of the trial must be a more important priority. Therefore, a balance should be struck to ensure the reliability of the endpoints being assessed in all interim reviews and the need for rapid data transfer. In practice, this is likely to require an intelligent monitoring approach where only the key variables are checked before the data is extracted. Later, and as an ongoing process of the trial, more extensive quality management can be applied and the data fully cleaned before the final data base is closed.
A more significant challenge for researchers wanting to conduct an adaptive trial design might be with the actual design rather than the implementation. Adaptive trial design is likely to need quite complex statistical considerations17 and for many clinical trial sites in resource-limited settings statistical support is a limitation.18,19 Here, a collaborative solution could be found if research sites that do have good statistical support offered support and advice to others through an open collaboration. This could be facilitated through the Global Health Clinical Trials Program.18
What do the regulations say about adaptive design and what will my institutional review board and ethics committee think of this approach?
Adaptive design is a common practice now in the United States and Europe and both regulatory authorities have a position and plenty of experience on this approach in trial methods20,21; where countries and institutions have not had the experience of this approach, difficulties may arise. In this situation a degree of prior education and sensitization of the committee might be advised. There are plenty of references and resources to draw upon, many of which have been cited here. Again, sharing experiences and strategies between research groups would be beneficial to the wider global health research community.
Conclusion
Clinical trials are needed to bring about improvements in public health as they test new drugs and vaccines and evaluate better ways to manage illnesses. Because developing countries have the largest burden of disease, they could benefit the most from clinical trials, but populations in these regions are underrepresented in trials compared with populations in wealthier regions. This is because there are too few trials and there are not enough people with the right skills to run trials.22–25 Adaptive trial design could make trials more cost-effective and minimize patient exposure to research interventions. All the advantages that adaptive design has brought to pharmaceutical trial stand to be at least as beneficial in resource-limited settings and therefore the approach is recommended to researchers in these settings. Disease management studies could be particularly well suited to adaptive design as they could logically and safely progress from the learning phase to confirmatory within a single protocol. In no sense should adaptive design be seen as a shortcut or less rigorous approach, rather as an optimal strategy that allows for a balance between learning about an unknown effect to benefit future patients and the ethical obligation to provide the best treatment of the patient on the trial. Indeed, it is unlikely that industry would have succeeded in widespread use of a design approach that risked suggestion of seeking shortcuts and weaker trial data.
Adaptive design clinical trials by definition allow for change during the trial without loss of validity. Although this stands to bring many advantages to enhancing research in resource-limited setting, there are limitations and potential pitfalls. Less familiar design methods incorporating these methodological features might be off-putting for sponsors, investigators, and reviewers. However, experience is growing and more reports using these methods are becoming available. The FDA guidance document provides detailed notes on how risks to study validity and interpretation can be avoided7 and these could reassure and help guide investigators and statisticians.
However, designing and operating adaptive clinical trials requires expert support, tools, resources, and training. Sharing of experience and best practice could facilitate more researchers using this approach and the Global Health Clinical Trials Program could provide the platform for this (www.globalhealthtrials.org).
Disclaimer: The author has no conflicts of interest to report.
Footnotes
Financial support: No specific funding has been received for this article. The author is funded and employed by the Centre for Tropical Medicine, University of Oxford, which receives core funding from the Wellcome Trust.
Author's address: Trudie Lang, Global Health Clinical Trials Programme, Centre for Tropical Medicine, University of Oxford, Oxford, UK, E-mail: Trudie.lang@ndm.ox.ac.uk.
References
- 1.Nelson NJ. Adaptive clinical trial design: has its time come? J Natl Cancer Inst. 2010;102:1217–1218. doi: 10.1093/jnci/djq319. [DOI] [PubMed] [Google Scholar]
- 2.Pullman DW, Wang X. Adaptive design, informed consent and the ethics of research. Control Clin Trials. 2001;22:203–210. doi: 10.1016/s0197-2456(01)00122-2. [DOI] [PubMed] [Google Scholar]
- 3.Mehta C, Gao P, Bhatt DL, Harrington RA, Skerjanec S, Ware JH. Optimizing trial design: sequential, adaptive, and enrichment strategies. Circulation. 2009;119:597–605. doi: 10.1161/CIRCULATIONAHA.108.809707. [DOI] [PubMed] [Google Scholar]
- 4.Jahn-Eimermacher A, Ingel K. Adaptive trial design: a general methodology for censored time to event data. Contemp Clin Trials. 2009;30:171–177. doi: 10.1016/j.cct.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Berry DA. Adaptive trial design. Clin Adv Hematol Oncol. 2007;5:522–524. [PubMed] [Google Scholar]
- 6.Brown CH, Ten Have TR, Jo B, Dagne G, Wyman PA, Muthén B, Gibbons RD. Adaptive designs for randomized trials in public health. Annu Rev Public Health. 2009;30:1–25. doi: 10.1146/annurev.publhealth.031308.100223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.FDA . Guidance for Industry: Adaptive Design for Drugs and Biologicals. 2010. [Google Scholar]
- 8.Dragalin V. Adaptive designs: terminology and classification. Drug Information Journal. 2006;40:425–435. [Google Scholar]
- 9.Fegan GW, Lang TA. Could an open-source clinical trial data-management system be what we have all been looking for? PLoS Med. 2008;5:e6. doi: 10.1371/journal.pmed.0050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nadol P, Stinson KW, Coggin W, Naicker M, Wells CD, Miller B, Nelson LJ. Electronic tuberculosis surveillance systems: a tool for managing today's TB programs. Int J Tuberc Lung Dis. 2008;12:8–16. [PubMed] [Google Scholar]
- 11.Abayomi A, Goodridge W, Asika O. Wireless networks for surveillance, data capture and data management in the human immunodeficiency virus epidemic care and treatment programs. Afr J Med Med Sci. 2006;35((Suppl)):149–152. [PubMed] [Google Scholar]
- 12.Gonzalez Moran F, Munoz Criado I, Vanaclocha H. Real time information. A necessary tool in epidemiological surveillance. Gac Sanit. 2008;22:162–167. doi: 10.1157/13119327. [DOI] [PubMed] [Google Scholar]
- 13.Abu-Hasaballah K, James A, Aseltine RH., Jr Lessons and pitfalls of interactive voice response in medical research. Contemp Clin Trials. 2007;28:593–602. doi: 10.1016/j.cct.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Lang T, Chilengi R, Noor RA, Ogutu B, Todd JE, Kilama WA, Targett GK. Data safety and monitoring boards for African clinical trials. Trans R Soc Trop Med Hyg. 2008;102:1189–1194. doi: 10.1016/j.trstmh.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 15.Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, Elbourne DR, McLeer SK, Parmar MKB, Pocock SJ, Spiegelhalter DJ, Sydes MR, Walker AE, Wallace SA. Issues in data monitoring and interim analysis of trials. Health Technol Assess. 2005;9:1–238. doi: 10.3310/hta9070. DAMOCLES Study Group. iii–iv. [DOI] [PubMed] [Google Scholar]
- 16.Gallo P, Chuang-Stein C, Dragalin V, Gaydos B, Krams M, Pinheiro J. Adaptive designs in clinical drug development—an Executive Summary of the PhRMA Working Group. J Biopharm Stat. 2006;16:275–283. doi: 10.1080/10543400600614742. [DOI] [PubMed] [Google Scholar]
- 17.Liu Q, Proschan MA, Pledger GW. A unified theory of two-stage adaptive designs. J Am Stat Assoc. 2002;97:1034–1041. [Google Scholar]
- 18.Lang TA, White NJ, Hien TT, Farrar JJ, Day NP, Angus BJ, Denis E, Merson L, Cheah PY, Kimutai R, Marsh K. Clinical research in resource-limited settings: enhancing research capacity and working together to make trials less complicated. PLoS Negl Trop Dis. 2010;4:e619. doi: 10.1371/journal.pntd.0000619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lang TA, Kokwaro GO. Malaria drug and vaccine trials in Africa: obstacles and opportunities. Trans R Soc Trop Med Hyg. 2008;102:7–10. doi: 10.1016/j.trstmh.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Wang M, Wu YC, Tsai GF. A regulatory view of adaptive trial design. J Formos Med Assoc. 2008;107:3–8. doi: 10.1016/s0929-6646(09)60002-4. [DOI] [PubMed] [Google Scholar]
- 21.Hung HM, O'Neill RT, Wang SJ, Lawrence J. A regulatory view on adaptive/flexible clinical trial design. Biom J. 2006;48:565–573. doi: 10.1002/bimj.200610229. [DOI] [PubMed] [Google Scholar]
- 22.Schluger N, Karunakara U, Lienhardt C, Nyirenda T, Chaisson R. Building clinical trials capacity for tuberculosis drugs in high-burden countries. PLoS Med. 2007;4:e302. doi: 10.1371/journal.pmed.0040302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Razzouk D, Sharan P, Gallo C, Gureje O, Lamberte EE, de Jesus Mari J, Mazzotti G, Patel V, Swartz L, Olifson S, Levav I, de Francisco A, Saxena S. Scarcity and inequity of mental health research resources in low-and-middle income countries: a global survey. Health Policy. 2010;94:211–220. doi: 10.1016/j.healthpol.2009.09.009. WHO-Global Forum for Health Research Mental Health Research Mapping Project Group. [DOI] [PubMed] [Google Scholar]
- 24.Mwaba P, Bates M, Green C, Kapata N, Zumla A. Research capacity strengthening in African countries. Lancet. 2010;375:1874. doi: 10.1016/S0140-6736(10)60874-4. [DOI] [PubMed] [Google Scholar]
- 25.Dolgin E. African networks launch to boost clinical trial capacity. Nat Med. 2010;16:8. doi: 10.1038/nm0110-8a. [DOI] [PubMed] [Google Scholar]


