Abstract
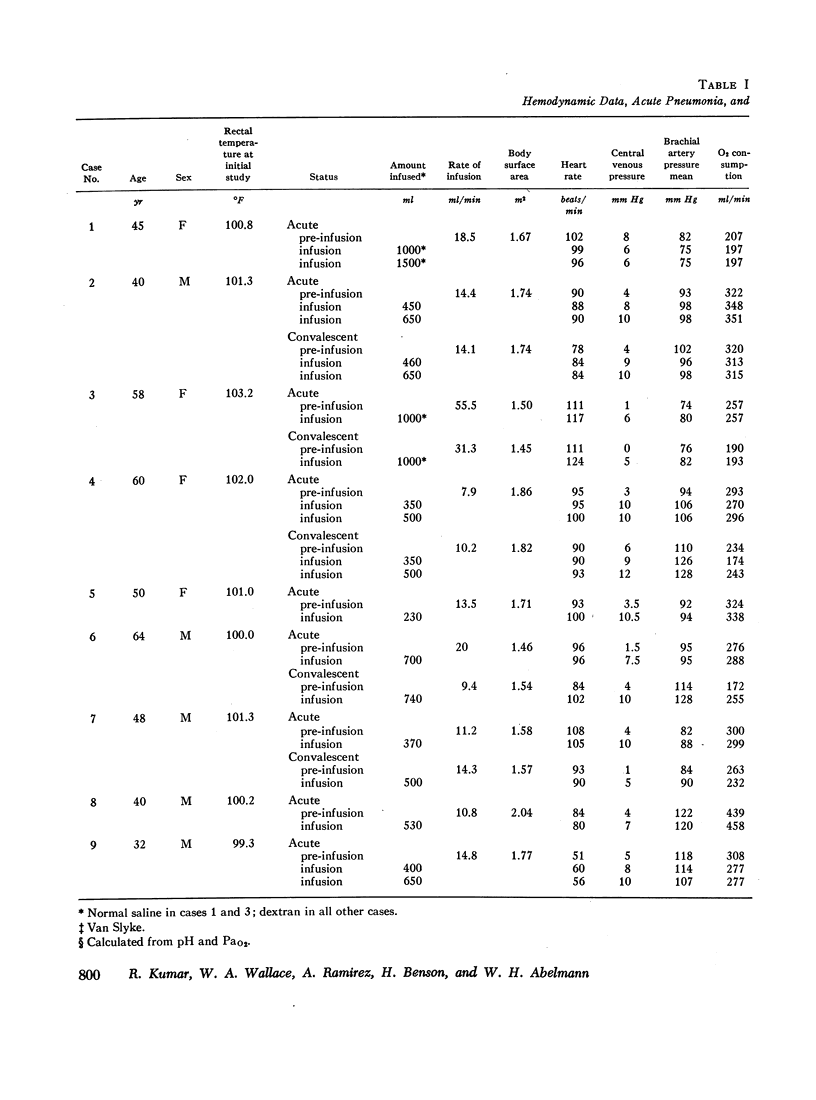
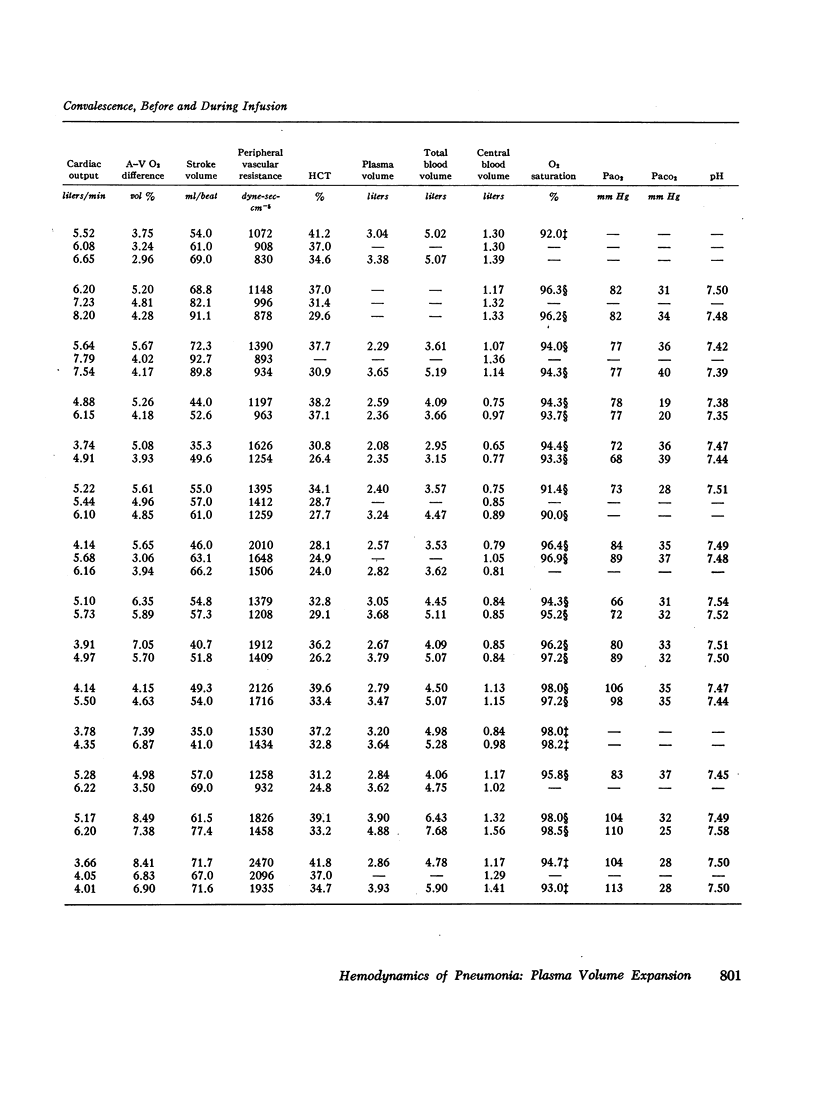
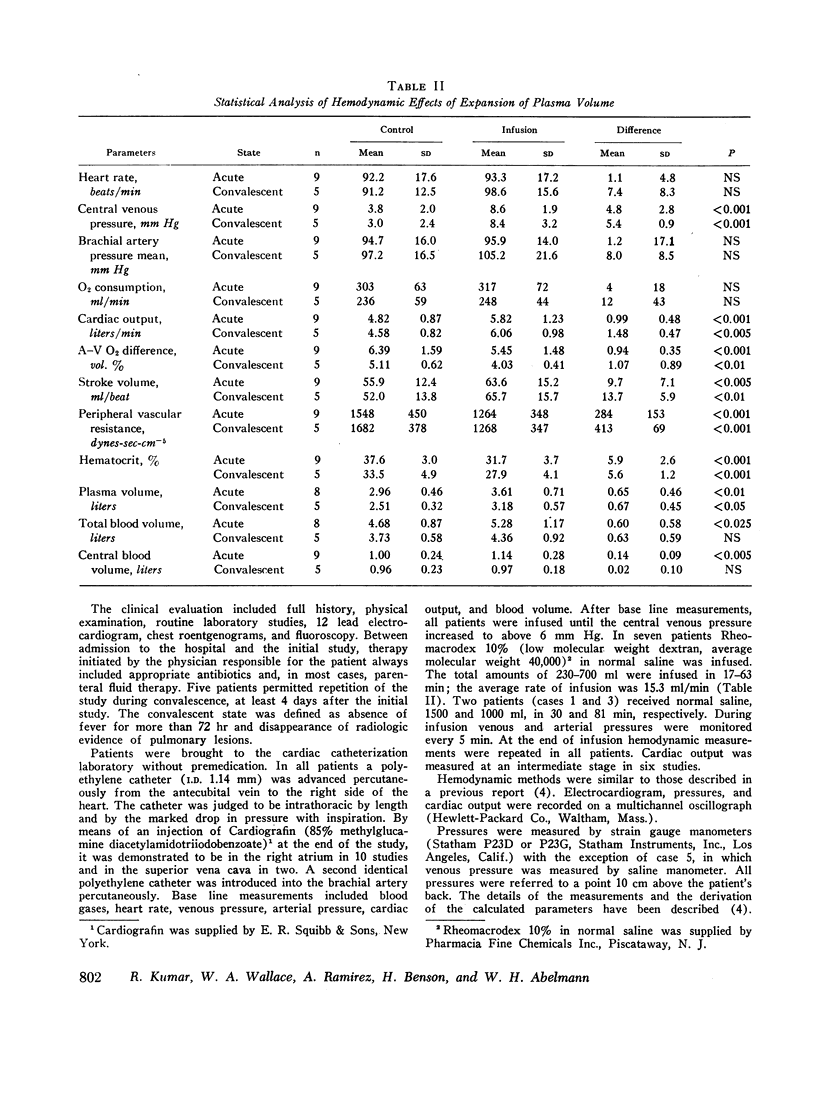
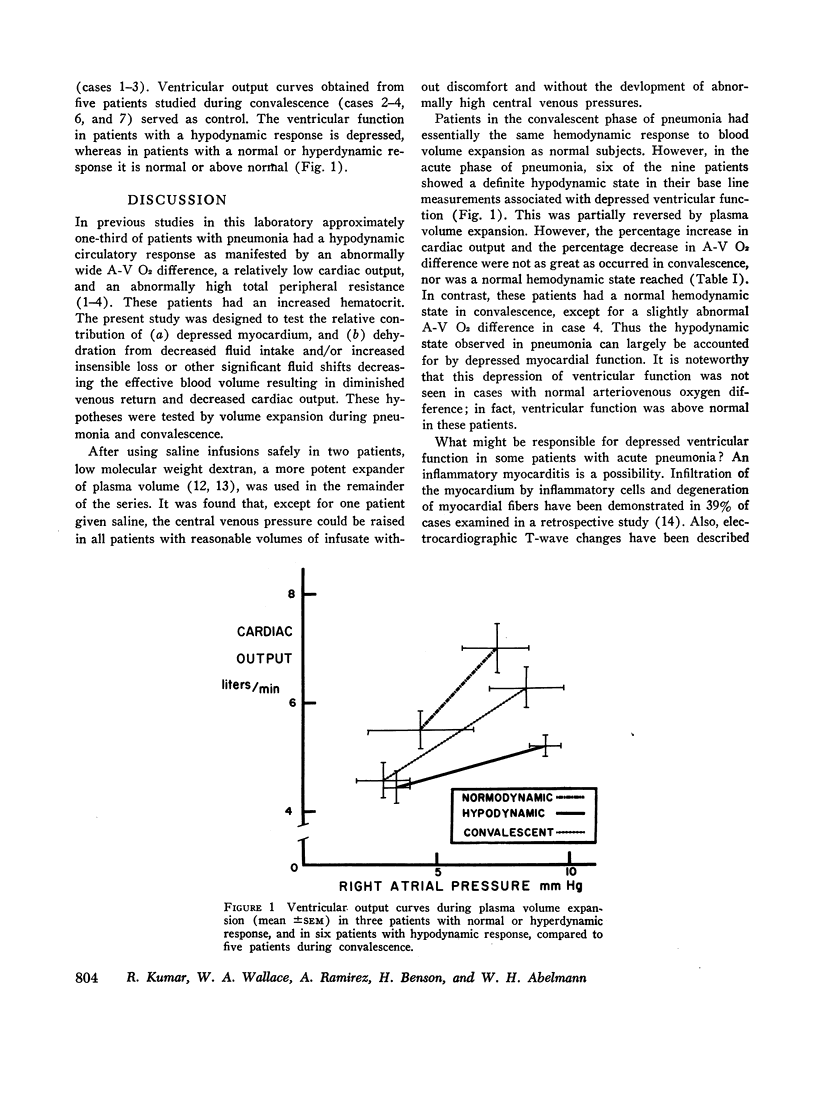
Previous work has demonstrated that approximately one-third of patients with pneumonia have a hypodynamic circulatory response. This response is characterized by an abnormally wide arteriovenous oxygen difference, a low cardiac output, increased peripheral resistance, and an increased hematocrit. This state was found to abate in convalescence. In an attempt to elucidate the pathogenesis of this hypodynamic state, nine additional patients were studied hemodynamically during the acute phase of pneumonia before and during acute expansion of blood volume by low molecular weight dextran (seven patients) or normal saline (two patients). Five patients were restudied before and during acute blood volume expansion in convalescence.
Three patients with pneumonia had a normal arteriovenous oxygen difference (< 5.5 vol%), and six patients were hypodynamic in that their arteriovenous oxygen differences were greater than 5.5 vol%. With expansion of blood volume in the acute phase of pneumonia, all patients showed an increase in cardiac output, a decrease in arteriovenous oxygen difference, and a decrease in peripheral vascular resistance; however, the percentage change in the hypodynamic patients was not as great as occurred in the patients with normal hemodynamics nor as great as occurred when restudied in convalescence. Likewise, all patients had a normal or near normal hemodynamic profile in convalescence. In addition, ventricular function in the acute phase of pneumonia was depressed. The findings suggest that the hypodynamic state associated with acute pneumonia is due to depressed myocardial contractility to which relative hypovolemia may contribute.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BISHOP V. S., STONE H. L., GUYTON A. C. CARDIAC FUNCTION CURVES IN CONSCIOUS DOGS. Am J Physiol. 1964 Sep;207:677–682. doi: 10.1152/ajplegacy.1964.207.3.677. [DOI] [PubMed] [Google Scholar]
- Benson H., Akbarian M., Adler L. N., Abelmann W. H. Hemodynamic effects of pneumonia. I. Normal and hypodynamic responses. J Clin Invest. 1970 Apr;49(4):791–798. doi: 10.1172/JCI106292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop V. S., Stone H. L. Quantitative description of ventricular output curves in conscious dogs. Circ Res. 1967 Jun;20(6):581–586. doi: 10.1161/01.res.20.6.581. [DOI] [PubMed] [Google Scholar]
- Carey J. S., Brown R. S., Mohr P. A., Monson D. O., Yao S. T., Shoemaker W. C. Cardiovascular function in shock. Responses to volume loading and isoproterenol infusion. Circulation. 1967 Feb;35(2):327–338. doi: 10.1161/01.cir.35.2.327. [DOI] [PubMed] [Google Scholar]
- Cohn J. N., Luria M. H., Daddario R. C., Tristani F. E. Studies in clinical shock and hypotension. V. Hemodynamic effects of dextran. Circulation. 1967 Feb;35(2):316–326. doi: 10.1161/01.cir.35.2.316. [DOI] [PubMed] [Google Scholar]
- GOODYER A. V., ECKHARDT W. F., OSTBERG R. H., GOODKIND M. J. Effects of metabolic acidosis and alkalosis on coronary blood flow and myocardial metabolism in the intact dog. Am J Physiol. 1961 Mar;200:628–632. doi: 10.1152/ajplegacy.1961.200.3.628. [DOI] [PubMed] [Google Scholar]
- Kettel L. J., Webster J. R., Moran F., Wagner S., Schultz I., Cugell D. W. Hemodynamic response to respiratory tract infections. Studies of total and peripheral blood flow. J Lab Clin Med. 1966 Jul;68(1):57–69. [PubMed] [Google Scholar]
- McNEELY W. F., GRAVALLESE M. A., Jr Measurement of cardiac output by dye dilution technique: use of an integrated sample collection in calibration of the photometric instrument. J Appl Physiol. 1954 Jul;7(1):55–58. doi: 10.1152/jappl.1954.7.1.55. [DOI] [PubMed] [Google Scholar]
- Regan T. J., Weisse A. B., Moschos C. B., Lesniak L. J., Nadimi M., Hellems H. K. The myocardial effects of acute and chronic usage of ethanol in man. Trans Assoc Am Physicians. 1965;78:282–291. [PubMed] [Google Scholar]
- SEVERINGHAUS J. W. Oxyhemoglobin dissociation curve correction for temperature and pH variation in human blood. J Appl Physiol. 1958 May;12(3):485–486. doi: 10.1152/jappl.1958.12.3.485. [DOI] [PubMed] [Google Scholar]


