Abstract
BACKGROUND:
Ventilator-induced lung injury is a recognized risk factor for bronchopulmonary dysplasia.
OBJECTIVE:
To determine whether primary continuous positive airway pressure (CPAP), defined as CPAP without previous endotracheal intubation for any indication, can reduce the need for intubation and mechanical ventilation in infants born at ≤32 weeks’ gestational age.
METHODS:
The literature was reviewed using the methodology for systematic reviews for the Consensus on Resuscitation Science adapted from the American Heart Association’s International Liaison Committee on Resuscitation.
RESULTS:
Fourteen studies were reviewed. Eleven studies provided varying degrees of supportive evidence (level of evidence 3 to 4) that the use of primary CPAP can reduce the need for intubation and mechanical ventilation.
CONCLUSION:
The use of CPAP as a primary intervention and mode of respiratory support is an option for infants ≤32 weeks’ gestation, but avoidance of intubation and mechanical ventilation is more likely in mature infants >27 weeks’ gestation.
Keywords: CPAP, Evidence review, Preterm infant
Abstract
HISTORIQUE :
Les lésions pulmonaires induites par les respirateurs constituent un facteur de risque connu de dysplasie bronchopulmonaire.
OBJECTIF :
Déterminer si la pression positive continue (PPC) primaire, définie comme une PPC sans intubation trachéale antérieure pour quelque indication que ce soit, peut réduire la nécessité d’intuber et d’administrer une ventilation mécanique aux nourrissons nés à 32 semaines d’âge gestationnel ou moins.
MÉTHODOLOGIE :
Les chercheurs ont analysé les publications au moyen de la méthodologie d’analyse systématique du Consensus on Resuscitation Science adapté de l’International Liaison Committee on Resuscitation de l’American Heart Association.
RÉSULTATS :
Les chercheurs ont analysé 14 études. Onze ont fourni des degrés divers de données probantes (qualité des preuves 3 à 4), appuyant le fait que le recours à la PPC primaire peut réduire la nécessité de procéder à une intubation et à la ventilation mécanique.
CONCLUSION :
Le recours à la PPC comme intervention primaire et mode de soutien respiratoire constitue une possibilité chez les nourrissons de 32 semaines d’âge gestationnel ou moins, mais il est davantage possible d’éviter l’intubation et la ventilation mécanique chez les nourrissons matures de plus de 27 semaines d’âge gestationnel.
Developed and established in Canadian neonatal intensive care units, EPIQ (Evidence-based Practice for Improving Quality) is a scientific method for continuous quality improvement that is evidence-based; targeted on key outcomes; collaborative, involving interprofessional teams of experts; and continuous, promoting a culture of change. Based on the International Liaison Committee on Resuscitation literature review template, the EPIQ review process addresses important clinical questions by summarizing relevant studies. They are intended as guides to best practices and do not represent unique or mandatory protocols. Full versions of these reviews are available at www.epiq.ca.
Khalid Aziz MD, Assistant Editor, Paediatrics & Child Health
BACKGROUND
Bronchopulmonary dysplasia (BPD) is a significant morbidity among surviving preterm infants (1). Rates of BPD vary widely across centres and range from 4.0% to 58.3% (2–4). The pathogenesis is multifactorial, with multiple risk factors such as early volutrauma, barotrauma and oxygen exposure superimposed on immature, developing lungs (1,5–7). Therefore, strategies to minimize these factors would be advantageous. One such strategy is the use of primary continuous positive airway pressure (pCPAP) after delivery to avoid ventilator-induced lung injury.
OBJECTIVE
We reviewed the literature to determine whether pCPAP, defined as CPAP without previous endotracheal intubation for any indication, as a mode of respiratory support after delivery reduces the need for intubation and mechanical ventilation in infants ≤32 weeks’ gestational age.
METHOD
Key words selected with synonyms were “continuous positive airway pressure” OR “CPAP” OR “nasal CPAP” OR “early CPAP”; “preterm” OR “premature infant” OR “neonate” OR “newborn”; “resuscitation” OR “delivery room”. These concepts were combined with the Boolean operator “AND”. Exclusion criteria were nonhuman subjects; non-English language; abstract only; review articles; CPAP as nonprimary intervention; children/adult subjects; late preterm or term infants; >32 weeks’ gestation; extubation to CPAP; and surfactant administration with CPAP.
Databases searched were Ovid Medline (1950 to 2009), Scopus (1997 to 2009), Web of Science (1997 to 2009), Embase (1987 to 2008), PubMed (1975 to 2009), CINAHL (1996 to 2008), Cochrane Central Register of Controlled Trials (first quarter of 2009) and Cochrane Database of Systematic Reviews (first quarter of 2009). The abstracts of all available reports and studies were reviewed including single-centre case series, observational studies with historical and other centre controls, and randomized controlled trials (RCTs). The bibliographies of all selected articles and several review articles were manually searched for additional studies.
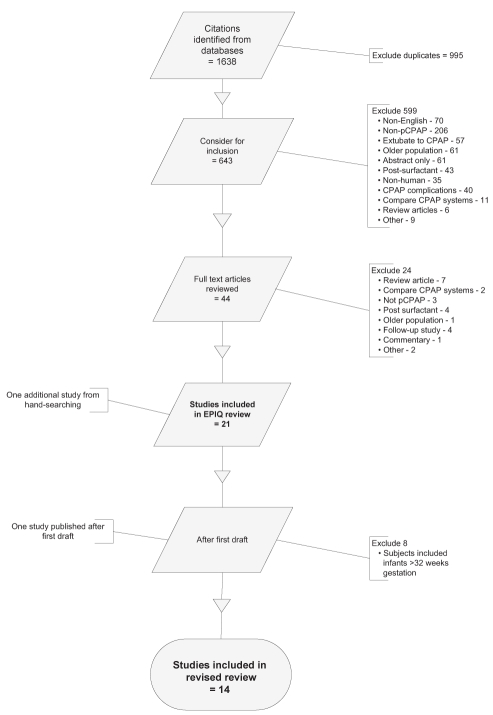
From an initial review of 1638 citations and 46 full-text articles (Figure 1), 14 studies were eligible for inclusion in the present review. They were scored using the Evidence Evaluation Worksheet adapted from the American Heart Association’s International Liaison Committee on Resuscitation (<www.amer-icanheart.org/presenter.jhtml?identifier=3052119>) (8). Four reviewers independently assigned level of evidence (LOE), direction of support and quality (<www.cebm.net/index.aspx?o=1157>) (9). Inconsistencies were resolved by consensus.
Figure 1).
Flow diagram for study selection. CPAP Continuous positive airway pressure; EPIQ Evidence-based Practice for Improving Quality; pCPAP Primary CPAP
RESULTS
The process for selection of the studies is outlined in Figure 1. With the exception of one, all studies included were published between 1999 and 2010. Included studies reported data that described the need for intubation and mechanical ventilation in infants ≤32 weeks’ gestation who were treated with pCPAP.
Characteristics of studies
In 1987, Han et al (10) reported an RCT with a population of infants (n=82) managed in the preantenatal corticosteroid and presurfactant era, using a nasopharyngeal continuous distending pressure device compared with headbox oxygen. They concluded that this mode of respiratory support was not beneficial and “may worsen the severity of RDS [respiratory distress syndrome]”. Only one other RCT addressed the question of our review. In 2004, Sandri et al (11) randomly assigned 230 infants, 28 to 31 weeks’ gestation, to early CPAP in the delivery room or delayed/rescue CPAP provided at 30 min of age. They concluded that the incidence of subsequent intubation in both groups was the same. Subramaniam et al (12) reviewed these two RCTs in a Cochrane systematic review and concluded that there was “insufficient information to evaluate the effectiveness of CPAP to reduce the need for IPPV [intermittent positive pressure ventilation]”. The remaining studies (n=2824 subjects) included six observational studies (13–18) in centres using historical controls ‘before-and-after’ implementing routine use of early CPAP (LOE 3), one study (19) reporting a national cohort’s experience with increasing use of CPAP over time and a parallel decrease in the use of intubation and mechanical ventilation (LOE 4), and one study (20) reporting a comparison between two centres with different resuscitation and ventilation practices (LOE 4). Additional observational data were identified from two RCTs (21,22). These studies were designed to address the primary outcome of death and/or BPD in patients treated with pCPAP compared with intubation and surfactant, rather than our primary question of pCPAP versus no prophylactic intervention. The group of infants (n=965) from the ‘CPAP arm’ of these studies (LOE 4) provided additional data regarding the effect of pCPAP. Another RCT (23) designed to address the feasibility of using a T-piece resuscitator in the delivery room before implementing CPAP as a mode of primary respiratory support also provided observational data (n=104) regarding the outcome of patients treated with pCPAP (LOE 4). These studies are presented in Table 1.
TABLE 1.
Studies of primary continuous positive airway pressure (pCPAP) in infants ≤32 weeks’ gestation
| Reference | Year | Study population | Study | Reported outcome | Comment | LOE* |
|---|---|---|---|---|---|---|
| Aly et al (13) | 2004 | Single centre n=101 infants <1000 g |
Observational study over three time periods from 1997–2002 (n=34, n=34, n=33) compared with a historical cohort of n=45 infants in baseline period 1995–1997 Unit adopted a policy for use of ENCPAP in the delivery room |
Increasing use of CPAP (17.6%, 61.8% and 66.7%) associated with progressive decrease in intubation and use of surfactant. Intubation increasingly avoided in first week (61.5%, 86.2% and 92.6%) over the three time periods Described trend to increase necrotizing enterocolitis, P=0.72 Decrease in BPD over the three time periods (definition of BPD not stated) |
Implemented policy for use of ENCPAP with education and training program. Assigned experienced nurses to provide care in first week with ‘minimal handling’ strategy. Small number of infants in each time period Criteria for CPAP failure not well defined |
3 (S) Q: fair |
| Finer et al (23) | 2004 | Five-centre RCT n=104 infants GA 23–28 weeks |
Study to address feasibility of randomization to use of the T-piece resuscitator (Neopuff†) in the delivery room to deliver CPAP/PEEP (n=55) during resuscitation compared with standard mask positive pressure ventilation without PEEP (n=49) | One-half of patients <28 weeks intubated in delivery room for resuscitation indication. Overall, 20% of infants <28 weeks avoided intubation within the first 7 days, regardless of mode of initial resuscitation. Infants >27 weeks were less likely to require intubation. All infants at 23 weeks were intubated in the delivery room | Criteria for CPAP failure, PCO2>55–60 mmHg, pH<7.25, apnea or FiO2>0.30 for surfactant administration Both groups treated with CPAP in NICU after initial resuscitation, if not intubated in delivery room |
4 (S) Q: good |
| Han et al (10) | 1987 | Single-centre RCT n=82 infants GA <32 weeks |
Nasopharyngeal CDP (n=43) use compared with headbox oxygen with possible ‘rescue’ CDP (n=39) | Unable to demonstrate advantage to early CDP in reducing RDS. Higher FiO2, lower a/A ratio in CDP early treated group, “worsen severity of RDS” | Predates current NICU care and use of antenatal corticosteroids | 1 (O) Q: good |
| Jegatheesan et al (14) | 2006 | Single centre n=171 infants ≤1000 g GA 23–32 weeks |
Observational study of two periods, before (2000–2004, n=96) and after (2002–2004, n=75) implementing a policy of early nCPAP in the delivery room with Infant Flow‡ nCPAP system | Using nCPAP in second period, 24% of infants were not intubated in delivery room and, overall, 12% were never intubated, proportions decrease to 15% and 3%, respectively for infants at GA <26 weeks No difference in CLD at 36 weeks |
Criteria for CPAP failure: PCO2>65 mmHg, pH<7.25, FiO2>0.60, apnea | 3 (S) Q: fair |
| Lindner et al (15) | 1999 | Single centre n=123 infants <1000 g GA ≥24 weeks |
Observational study of two periods before (1994, n=56) and after (1996, n=67) implementation of lung recruitment with positive pressure via NPT followed by NPT CPAP delivered by mechanical ventilator | Greater proportion of infants avoided intubation and mechanical ventilation in the second time period: 25% in second period and 7% in first period | Increase in dosage of antenatal betamethasone in second time period Criteria for CPAP failure not detailed |
3 (S) Q: fair |
| Morley et al (22); COIN trial | 2008 | Multicentre RCT n=610 infants GA 25–28 weeks (33% GA 25–26 weeks) CPAP group n=307 |
Randomized to use of CPAP versus endotracheal intubation in the delivery room at 5 min of age. Study conducted 1999–2006 | Overall, 54% of infants in the CPAP group avoided intubation and ventilation; 45% in 25 to 26-week infants and 60% in 27 to 28-week infants. Use of surfactant halved in the CPAP group. No difference in primary outcome of death or BPD at 36 weeks | Criteria for CPAP failure: PCO2>60 mmHg, pH<7.25, FiO2>0.60, apnea despite caffeine. Higher incidence of pneumothorax in the CPAP group, NNH 16. NNT 2.5 to avoid surfactant use. Observational data from one arm of RCT | 4 (S) Q: good |
| Narendran et al (16) | 2003 | Single centre n=171 infants <1000 g |
Comparing two periods before (1998–1999, n=929) and after (2000–2001, n=79) use of ENCPAP | Decreased intubation in the delivery room and reduced need for mechanical ventilation; mechanical ventilation avoided in 17.4% in the first period compared with 27.8% in the second period No difference in CLD at 36 weeks |
Criteria for CPAP failure: PCO2>65 mmHg, pH<7.15, FiO2>0.60 | 3 (S) Q: fair |
| Pelligra et al (17) | 2008 | Single centre n=1526 infants GA <32 weeks |
Observational study of two sequential time periods before (1996–2000, n=675) and after (2000–2004, n=851) the centre adopted practice of using nCPAP (underwater ‘bubble’ CPAP) as a delivery room intervention | Reduction in use of surfactant and need for mechanical ventilation in second period. In the second period, 19% of infants avoided intubation compared with 9% of infants in the first period No difference in BPD at 36 weeks |
Criteria for CPAP failure: PCO2>60 mmHg, pH<7.25, FiO2>0.50, apnea | 3 (S) Q: good |
| Sandri et al (11) | 2004 | Multicentre RCT n=230 infants GA 28–31 weeks |
Randomized infants to nCPAP within 30 min of age (n=115) or rescue nCPAP if FiO2>0.40 beyond 30 min of age (n=115), using the Infant Flow‡ Driver system. Study conducted 1999–2000 | No difference in the need for intubation or surfactant use in the two groups Practice of routine prophylactic surfactant in infants at GA <28 weeks |
Criteria for CPAP failure: PCO2>70 mmHg, pH<7.2, apnea or FiO2>0.80 in first 30 min | 1 (N) Q: good |
| Subramaniam et al (12) | 2005 | Meta-analysis 2 studies (n=312) GA <32 weeks |
Analysis of two RCTs conducted in 1987 and 1999, respectively | Concluded that there was “insufficient information to evaluate the effectiveness of CPAP to reduce need for IPPV” | Different population, time period and NICU practices in two studies | 2 (N) Q: fair |
| Finer et al (21) (SUPPORT Trial Group) | 2010 | Multicentre RCT n=1316 GA 24–28 weeks (43% GA 24–25 weeks) CPAP group: n=663 |
Randomized to CPAP or intubation in delivery room and surfactant treatment (within 1 h after birth). Also randomized to one of two target ranges of oxygen saturation. Study conducted 2005–2009 | Within the CPAP group, 65.6% avoided intubation in the delivery room, 32.9% avoided treatment with surfactant and intubation was avoided in 16.9% overall No difference in the primary outcome of death or BPD at 36 weeks |
Criteria for CPAP failure: PCO2>65 mmHg, FiO2>0.50, hemodynamic instability Observational data from one arm of RCT |
4 (S) Q: good |
| Swietlinski et al (19) | 2007 | National cohort 2003 to 2005 Subset of infants ≤30 weeks’ GA, n=236 |
Observational study after implementing use of the Infant Flow† Advance Driver CPAP within a national program across 57 secondary and tertiary care NICUs | In a subset of infants ≤30 weeks’ gestation, able to avoid intubation in 157 of 236 (66.5%) Incidence of nasal and facial complications noted to be higher in lower birth weight infants |
Multicentre, three modes of CPAP used: standard, bi-level and triggered bi-level. Criteria for CPAP failure: PCO2>65 mmHg, pH<7.25, FiO2>0.60, apnea | 4 (S) Q: poor |
| Vanpee et al (20) | 2007 | Two centres n=172 infants GA <28 weeks |
Comparison over two years at a European centre (n=102) and a United States centre (n=70) to evaluate differences in resuscitation and ventilation practices | nCPAP (Infant Flow‡ Driver system) was used initially in 56% of infants in the first centre; overall, 22% avoided intubation during the first week of life. Routine intubation and surfactant use in the second centre | Infants in first centre had higher SNAPPE-II scores, and antenatal steroids used less frequently in second centre | 4 (S) Q: poor |
| Zecca et al (18) | 2006 | Single centre n=324 infants GA 24–28 weeks |
Observational study of two periods before (1992–1997, n=161) and after (1998–2003, n=163) implementation of practice change from immediate intubation to use of nCPAP initiated in delivery room with T-piece resuscitator (NeoPuff†) | Overall, intubation avoided in 14% of infants in the second period compared with 3% in the first period. Infants 27–28 weeks’ GA, 21.3% avoided intubation in the second period compared with 2.8% in the first period. Infants 24–26 weeks’ GA, >95% intubated in both periods | Greater use of antenatal steroids in the second period Prophylactic ibuprofen used in the second period Criteria for CPAP failure: PCO2>60 mmHg, pH<7.25 |
3 (S) Q: fair |
Letters in parentheses under level of evidence (LOE): N Neutral to intervention; O Oppose intervention; S Support intervention;
Fisher & Paykel Healthcare Limited, Canada;
CareFusion, USA. BPD Bronchopulmonary dysplasia; CDP Continuous distending pressure; CLD Chronic lung disease; COIN Nasal CPAP or Intubation at Birth; CPAP continuous positive airway pressure; ENCPAP Early ‘bubble’ nasal CPAP; FiO2 Fraction of inspired O2; GA Gestational age; IPPV Intermittent positive pressure ventilation; nCPAP Nasal CPAP; NICU Neonatal intensive care unit; NNH Number needed to harm; NNT Number needed to treat; NPT Nasopharyngeal tube; PCO2 Partial pressure of CO2; PEEP Positive end expiratory pressure; Q Quality; RCT Randomized controlled trial; RDS Respiratory distress syndrome; SNAPPE Score for Neonatal Acute Physiology Perinatal Extension; SUPPORT Surfactant, Positive Pressure, and Oxygenation Randomized Trial
Quality of the studies
The majority of studies were observational, using historical controls or no controls in the context of observational data within a subset of subjects from an RCT designed to address a different primary outcome. The quality of the studies was generally good to fair, but was variable based on a clear definition of the comparison groups, outcomes measured objectively, known confounders identified and controlled for, and sufficient follow-up.
DISCUSSION
The overall observed rate of avoiding intubation and mechanical ventilation by using pCPAP in these studies ranged from 12% to 92.6%. This broad range reflects the heterogeneity of the observational studies along with the temporal changes in neonatal care that likely occurred over the reported time periods.
Some studies attempted to determine whether the use of pCPAP was associated with a decrease in the incidence of BPD. With the exception of the study by Aly et al (13), none of the studies identified a statistically significant decrease in the incidence of BPD, or differences in other neonatal morbidities including air leak and necrotizing enterocolitis. Aly et al reported avoiding intubation in 92.6% of patients and a decrease in BPD, but this was the result of a single centre’s experience at the end of four successive time periods, after implementing a policy for use of early nasal CPAP in extremely low birth weight infants, and incorporating an education and training program. They specifically assigned experienced nurses to provide care in the first week with a ‘minimal handling’ strategy. It is of note that the outcomes were actually worse in the first time period than at baseline, suggesting that there was a ‘learning curve’, with sequential improvement over the three time periods after the change in practice. Only the data from the ‘CPAP arm’ of one RCT (22) reported a higher incidence of air leak in the CPAP group compared with the group managed with intubation.
The set criteria for ‘CPAP failure’ resulting in intubation and mechanical ventilation were all very similar in the studies (Table 1), with the exception of the delivery room feasibility study of the T-piece resuscitator (23). Infants requiring a fraction of inspired O2 >0.30 could be intubated to receive surfactant, so in the present study, 80% of infants <28 weeks’ gestation placed on CPAP were subsequently intubated.
Despite its observational nature, data from the ‘CPAP arms’ of the large RCTs represent a large sample of similar, extremely premature infants exposed to pCPAP. The lower intubation rate in the Nasal CPAP or Intubation at Birth (COIN) trial (22), in contrast to the Surfactant, Positive Pressure, and Oxygenation Randomized Trial (SUPPORT) (21), likely reflects the lower gestational age of the patients in the SUPPORT trial. This is congruent with observations made in other studies (14,18,23). Collectively, the studies suggest that use of pCPAP is more likely to be successful in infants >27 weeks’ gestation.
The success of surfactant in treating respiratory distress in preterm infants led to the strategy of prophylactic surfactant (24). More recently, centres have adopted the practice of intubation for surfactant administration followed by extubation to early CPAP, in efforts to avoid the presumed deleterious effects of positive pressure ventilation (25). These practice strategies have made it difficult to conduct RCTs comparing pCPAP with a true noninterventional control group. With good prenatal care, including administration of antenatal corticosteroids, some extremely premature infants are observed to experience minimal clinical symptoms of respiratory distress, and the chest radiographs do not have the classical reticular granular pattern of RDS. It is in this group of infants that it may be possible to provide respiratory support with pCPAP, and avoid intubation and mechanical ventilation. The present review suggests that intubation may be avoided in some of these infants, but the success rate described is as low as 12% or as high as 92.6%. Most of the observational data report success rates ranging from 12% to 54%, with higher success rates identified in more mature infants >27 weeks’ gestation. The observational nature of these studies is confounded by biases that include, but are not limited to, the different types of CPAP systems used, different pressure used and other concurrent practices such as the changing use of antenatal corticosteroids because some of these ‘before-and-after’ studies spanned several years.
Successful use of pCPAP could circumvent the need for endotracheal intubation. The appeal of this strategy is that it could avoid the deleterious effects of mechanical ventilation and the occurrence of ventilator-induced lung injury.
CONSENSUS ON SCIENCE
There is good to fair-quality supportive evidence from 11 studies (LOE 3 to LOE 4) that the use of pCPAP can reduce the need for intubation and mechanical ventilation in infants ≤32 weeks’ gestation.
RECOMMENDATION
The use of CPAP as a primary intervention and mode of respiratory support is an option for infants ≤32 weeks’ gestation, but avoidance of intubation and mechanical ventilation is more likely in mature infants >27 weeks’ gestation.
Acknowledgments
The authors thank RS Sauve MD for his helpful advice and review of this manuscript.
Footnotes
EPIQ EVIDENCE REVIEW GROUP MEMBERS: Principal investigator: Dr Shoo K Lee, Mount Sinai Hospital, Toronto, Ontario. Chair: Dr Nalini Singhal, Foothills Medical Centre, Calgary, Alberta. Members: Dr Kim Dow, Kingston General Hospital, Kingston, Ontario; Dr Andrew James, The Hospital for Sick Children, Toronto, Ontario; Dr Ibrahim Mohamed, Hôpital Sainte-Justine, Montreal, Quebec; Dr Nicole Rouvinez-Bouali, Children’s Hospital of Eastern Ontario, Ottawa, Ontario; Dr Koravangattu Sankaran, Royal University Hospital, Saskatoon, Saskatchewan; Dr Vibhuti Shah, Mount Sinai Hospital, Toronto, Ontario. Principal author: Dr Wendy Yee, Foothills Medical Centre, Calgary, Alberta.
REFERENCES
- 1.Van Marter LJ. Epidemiology of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009;14:358–66. doi: 10.1016/j.siny.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Lee SK. Canadian Neonatal Network Annual Report. Toronto: Canadian Neonatal Network; 2007. [Google Scholar]
- 3.Payne NR, LaCorte M, Karna P, et al. Reduction of bronchopulmonary dysplasia after participation in the Breathsavers Group of the Vermont Oxford Network Neonatal Intensive Care Quality Improvement Collaborative. Pediatrics. 2006;118(Suppl 2):S73–7. doi: 10.1542/peds.2006-0913C. [DOI] [PubMed] [Google Scholar]
- 4.Zeitlin J, Draper ES, Kollee L, et al. Differences in rates and short-term outcome of live births before 32 weeks of gestation in Europe in 2003: Results from the MOSAIC cohort. Pediatrics. 2008;121:e936–44. doi: 10.1542/peds.2007-1620. [DOI] [PubMed] [Google Scholar]
- 5.Bancalari E, Claure N, Sosenko IR. Bronchopulmonary dysplasia: Changes in pathogenesis, epidemiology and definition. Semin Neonatol. 2003;8:63–71. doi: 10.1016/s1084-2756(02)00192-6. [DOI] [PubMed] [Google Scholar]
- 6.Coalson JJ. Pathology of new bronchopulmonary dysplasia. Semin Neonatol. 2003;8:73–81. doi: 10.1016/s1084-2756(02)00193-8. [DOI] [PubMed] [Google Scholar]
- 7.Merritt TA, Deming DD, Boynton BR. The ‘new’ bronchopulmonary dysplasia: Challenges and commentary. Semin Fetal Neonatal Med. 2009;14:345–57. doi: 10.1016/j.siny.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Morley PT. Evidence evaluation worksheets: The systematic reviews for the evidence evaluation process for the 2010 International Consensus on Resuscitation Science. Resuscitation. 2009;80:719–21. doi: 10.1016/j.resuscitation.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 10.Han VK, Beverley DW, Clarson C, et al. Randomized controlled trial of very early continuous distending pressure in the management of preterm infants. Early Hum Dev. 1987;15:21–32. doi: 10.1016/0378-3782(87)90097-1. [DOI] [PubMed] [Google Scholar]
- 11.Sandri F, Ancora G, Lanzoni A, et al. Prophylactic nasal continuous positive airways pressure in newborns of 28–31 weeks gestation: Multicentre randomised controlled clinical trial. Arch Dis Child Fetal Neonatal Ed. 2004;89:F394–8. doi: 10.1136/adc.2003.037010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subramaniam P, Henderson-Smart DJ, Davis PG. Prophylactic nasal continuous positive airways pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2005;(3):CD001243. doi: 10.1002/14651858.CD001243.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Aly H, Milner JD, Patel K, El-Mohandes AA. Does the experience with the use of nasal continuous positive airway pressure improve over time in extremely low birth weight infants? Pediatrics. 2004;114:697–702. doi: 10.1542/peds.2003-0572-L. [DOI] [PubMed] [Google Scholar]
- 14.Jegatheesan P, Keller RL, Hawgood S. Early variable-flow nasal continuous positive airway pressure in infants < or =1000 grams at birth. J Perinatol. 2006;26:189–96. doi: 10.1038/sj.jp.7211454. [DOI] [PubMed] [Google Scholar]
- 15.Lindner W, Vossbeck S, Hummler H, Pohlandt F. Delivery room management of extremely low birth weight infants: Spontaneous breathing or intubation? Pediatrics. 1999;103(5 Pt 1):961–7. doi: 10.1542/peds.103.5.961. [DOI] [PubMed] [Google Scholar]
- 16.Narendran V, Donovan EF, Hoath SB, Akinbi HT, Steichen JJ, Jobe AH. Early bubble CPAP and outcomes in ELBW preterm infants. J Perinatol. 2003;23:195–9. doi: 10.1038/sj.jp.7210904. [DOI] [PubMed] [Google Scholar]
- 17.Pelligra G, Abdellatif MA, Lee SK. Nasal continuous positive airway pressure and outcomes in preterm infants: A retrospective analysis. Paediatr Child Health. 2008;13:99–103. [PMC free article] [PubMed] [Google Scholar]
- 18.Zecca E, de LD, Costa S, Marras M, de TP, Romagnoli C. Delivery room strategies and outcomes in preterm infants with gestational age 24–28 weeks. J Matern Fetal Neonatal Med. 2006;19:569–74. doi: 10.1080/14767050600736739. [DOI] [PubMed] [Google Scholar]
- 19.Swietlinski J, Bober K, Gajewska E, et al. Introduction of Infant Flow nasal continuous airway pressure as the standard of practice in Poland: The initial 2-year experience. Pediatr Crit Care Med. 2007;8:109–14. doi: 10.1097/01.PCC.0000257096.57260.3F. [DOI] [PubMed] [Google Scholar]
- 20.Vanpée M, Walfridsson-Schultz U, Katz-Salamon M, Zupancic JA, Pursley D, Jonsson B. Resuscitation and ventilation strategies for extremely preterm infants: A comparison study between two neonatal centers in Boston and Stockholm. Acta Paediatr. 2007;96:10–6. doi: 10.1111/j.1651-2227.2007.00063.x. [DOI] [PubMed] [Google Scholar]
- 21.Finer NN, Carlo WA, Walsh MC, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;362:1970–9. doi: 10.1056/NEJMoa0911783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358:700–8. doi: 10.1056/NEJMoa072788. [DOI] [PubMed] [Google Scholar]
- 23.Finer NN, Carlo WA, Duara S, et al. Delivery room continuous positive airway pressure/positive end-expiratory pressure in extremely low birth weight infants: A feasibility trial. Pediatrics. 2004;114:651–7. doi: 10.1542/peds.2004-0394. [DOI] [PubMed] [Google Scholar]
- 24.Soll RF, Morley CJ. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2001;(2):CD000510. doi: 10.1002/14651858.CD000510. [DOI] [PubMed] [Google Scholar]
- 25.Stevens TP, Harrington EW, Blennow M, Soll RF. Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev. 2007;(4):CD003063. doi: 10.1002/14651858.CD003063.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]