Abstract
OBJECTIVE:
To identify early clinical factors that are correlated with death or severe disability in paediatric patients who have sustained an injury by hanging or strangulation.
METHODS:
A retrospective review of all patient records from January 1, 1997, to September 30, 2007, was conducted. Patient records were identified by International Classification of Diseases and Related Health Problems, Tenth Revision, Canada diagnostic codes for asphyxia, strangulation, hypoxic-ischemic encephalopathy, hanging, hypoxemia, hypoxia or anoxia.
RESULTS:
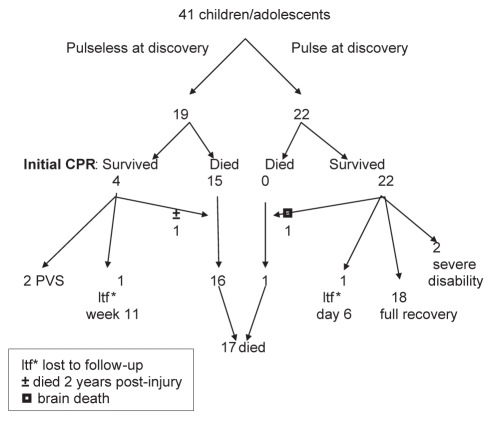
A total of 109 records were identified. Of these, 41 met the inclusion criteria for the study. Of 19 (46%) children who were pulse-less and received cardiopulmonary resuscitation, 16 died and the survivors were severely disabled. Of the 22 (54%) children who were found with a pulse, 18 made a full recovery.
CONCLUSIONS:
Children who are pulseless at discovery for hanging injuries are at high risk of death or severe disability. Early clinical and neurophysiological indicators should be applied systematically to best guide clinicians and parents in their decision making.
Keywords: Cardiac arrest, Hanging, Outcome
Abstract
OBJECTIF :
Déterminer les facteurs cliniques précoces corrélés avec un décès ou une grave incapacité chez des patients d’âge pédiatrique qui ont subi une lésion par pendaison ou strangulation.
MÉTHODOLOGIE :
Les chercheurs ont procédé à l’analyse rétrospective de tous les dossiers de patients entre le 1er janvier 1997 et le 30 septembre 2007. Ils ont repéré les dossiers par les codes diagnostiques de la Classification statistique internationale des maladies et des problèmes de santé connexes, 10e révision, Canada, relatifs à l’asphyxie, à la strangulation, à l’encéphalopathie hypoxique ischémique, à la pendaison, à l’hypoxémie, à l’hypoxie ou à l’anoxie.
RÉSULTATS :
Les chercheurs ont repéré un total de 109 dossiers. De ce nombre, 41 respectaient les critères d’inclusion de l’étude. Des 19 (46 %) enfants arrivés en réanimation cardiorespiratoire sans pouls, 16 sont décédés, et les survivants ont conservé de graves séquelles. Des 22 (54 %) enfants qui avaient encore un pouls lorsqu’ils ont été découverts, 18 se sont complètement rétablis.
CONCLUSIONS :
Les enfants qui n’ont pas de pouls lorsqu’ils sont découverts après une lésion par pendaison sont très vulnérables à un décès ou à une grave incapacité. Les indicateurs cliniques et neurophysiologiques précoces devraient s’appliquer systématiquement afin de mieux orienter les cliniciens et les parents dans leur prise de décision.
Factors related to poor prognosis for children and adolescents by hanging or strangulation are not well documented in the literature. More commonly reported are ‘near-hanging’ or ‘choking games’ in the teenage population (1,2). These situations are related to inducing altered mental status and pleasant sensations in the case of choking games, or as an autoerotic experience in which self-harm is not intended in the case of older males.
In the adult literature, hanging as a means of suicide is more widely reported. In adults, factors that portend a poor prognosis (death or severe neurological injury) include ‘vital signs absent’ requiring cardiopulmonary resuscitation (CPR) and a Glasgow coma score (GCS) of 3 at the time of discovery (3–5). For comatose survivors of an initial resuscitation for cardiac arrest from any cause, other poor prognostic factors include burst suppression on an electroencephalogram (EEG), bilateral absence of N20 latency on somatosensory evoked potentials (SSEPs) in conjunction with clinical features of myoclonic status epilepticus within the first 24 h, absent pupillary responses after 24 h, absent corneal reflexes after 48 h, and absent or extensor motor responses to pain after 72 h (6,7). Serum neuron-specific enolase has the potential to be a predictor of poor outcome in patients after cardiac arrest in both children and adults (8–10).
A substantial number of patients with hanging and strangulation injuries are referred to the Stollery Children’s Hospital (Edmonton, Alberta), with a high use of resources for severely impaired survivors. Parents and care providers are often in the position of having to make life and death decisions within the first week after such an injury. To avoid premature withdrawal of support in patients who have a possible chance at recovery, tests should have a near-zero rate of false positives for determining a poor prognosis (11). The goal of the present study was to describe predictors of death or functional disability in children and adolescents with a brain injury after hanging or strangling. Identifying such factors would help with decision making by parents and health care providers who are faced with this devastating event.
METHODS
Approval for the study was obtained through the Health Research Ethics Board for the University of Alberta Hospital and Stollery Children’s Hospital (Edmonton, Alberta). All patients presenting from January 1, 1997, to September 30, 2007, who were younger than 18 years of age were identified by admission and/or discharge diagnoses extracted from the Regional [Health Record] Meta Health Database (Meta Health Technology Inc, USA). This database houses patient administrative data for all emergency department visits, day surgery visits and inpatient separations. The database is populated by coders and coding charts within each health record department using the Regional Meta Health Abstracting System. Records were extracted based on emergency room visits having the International Classification of Diseases and Related Health Problems, Tenth Revision, Canada diagnosis code for the following conditions: asphyxia, strangulation, hypoxic-ischemic encephalopathy (HIE), hanging, hypoxemia, hypoxia or anoxia. Of these, 109 cases were identified, and all charts and microfiche records were obtained from health records at the Stollery Children’s Hospital and the University of Alberta Hospital in Edmonton (population 800,000, catchment area 1.5 million). Of these, 68 were excluded when it was established that the injury was not related to strangulation or hanging. These included cases that had been erroneously coded for threats of self-harm by hanging, but in which no actual harm or injury had occurred, or when another traumatic mechanism, such as a motor vehicle collision, resulted in the injury, rather than by hanging or strangulation. Also excluded were neonates who were diagnosed with HIE due to intrauterine or perinatal asphyxia. Forty-one patient records were, therefore, included in the detailed retrospective review.
A case report form was designed to record demographic information, events during the immediate resuscitation, and care beyond the first week where applicable. Outcomes were categorized as good, poor or death. Due to the retrospective nature of the study, the most frequently documented estimate of neurological status was used, which was the GCS (12,13). Good outcome was categorized as a return to a GCS of 15, and poor outcome as all those in which the GCS remained ≤14. Other scales, such as a clinical performance scale and the Glasgow outcome scale, were not chosen because the chart data did not reflect their use. Survivors documented to be in a ‘persistent vegetative state’ (PVS) are presumed to be in a state of persistent unawareness of self and environment, as originally described by Jennett and Plum (14).
For the purposes of the present study, CPR was not defined as assisted ventilation alone, but was resuscitation in which cardiac compressions with or without cardiotropic medications were used.
Data analysis
Chart reviews were performed independently by two separate reviewers (DD and ML). The data were entered onto paper data collection forms before being transcribed into separate data sets in an OpenClinica database. These electronic data were then validated according to a formal data validation plan, and any issues were referred to the original reviewer for resolution. Resultant data corrections were applied to the two data sets as appropriate. Once the two data sets were considered to be clean, they were extracted into SAS (SAS Institute Inc, USA) and compared using PROC COMPARE. This process highlighted differences in the reviewers’ interpretation of the charts, and the resultant mismatches were referred to the principal investigator for resolution. Corrections were applied to a single data set, which was designated as the primary data set; these data were re-extracted for analysis.
The data/statistical analysis method was primarily descriptive, using frequencies and proportions. Bivariable analyses (eg, cross-tabs and exact test) were used to test the relationship between a categorical variable, such as vital sign, and the main outcome. Kruskal-Wallis analysis tested the relationship between a continuous variable such as GCS value and the main outcome. All statistical analyses were performed using SAS/STAT version 9.2 (SAS Institute Inc, USA) for Windows (Microsoft, USA).
RESULTS
Of the 41 patient records that were included, 13 were female and 28 were male; more than two-thirds of patients were adolescents between 13 and 17 years of age (n=28 [68%]). Ten children were between six and 12 years of age, and the remaining three children were five years of age or younger. The mean age was 13.2 years (median 14.6 years). Nine (22%) children were Aboriginal in an area where Aboriginal children represent approximately 5% of the paediatric population. Additional details of patient characteristics are shown in Table 1. In younger children, some incidents were clearly accidental in nature (strangulation by cord, strap, high chair, etc). In the cases of a few school-age children, it was unclear whether the circumstance arose accidentally or intentionally.
TABLE 1.
Baseline characteristics of subjects
| Variable | n (%) |
|---|---|
| Subjects | 41 (100) |
| Sex | |
| Male | 28 (68) |
| Female | 13 (32) |
| Home location* | |
| Rural | 15 (37) |
| Urban | 22 (53) |
| Unknown | 4 (10) |
| Mental health diagnosis | 22 (53) |
| Medication for mood or behaviour problem | 12 (30) |
| Toxic screen | |
| Positive† | 4 (10) |
| Negative | 18 (44) |
| Not performed/not recorded | 19 (46) |
Determined by home postal code;
All were positive for ethanol
Of the 41 patients, 19 (46%) were found to be pulseless by the first emergency medical service assessment and received CPR (Figure 1). The remaining 22 had palpable pulses, although seven of these had ‘agonal’ respirations and were intubated for transport. Of the 19 who were pulseless and received CPR, 15 died during the initial resuscitation, while another was declared brain dead within the first week. Two patients survived in a PVS, while another survivor experienced significant neurological dysfunction with bilateral basal ganglia injury, was completely dependent for all care and died two years after her hanging injury, having never returned home from extended care or rehabilitation hospitals. These three patients all underwent tracheostomies, due to an inability to extubate after the first few weeks, and received prolonged mechanical ventilation. Eighteen patients who had a pulse at discovery were discharged with a full recovery, while four patients found with a pulse had a poor recovery (GCS <15) or died.
Figure 1).
Flow chart depicting outcome for 41 children/adolescents with hanging injuries. CPR Cardiopulmonary resuscitation; PVS Persistent vegetative state
In all cases, the length of time the patient had been hanging or asphyxiated was unknown because each incident was unwitnessed. Therefore, data could only be generated from the time the patient was found hanging, rather than from the event itself.
The ultimate outcome was highly predicted by whether the patient was found with a palpable pulse (Table 2). All complete recoveries were seen in patients who had a pulse at discovery, whereas 15 of the 16 children who died were pulseless at discovery and received CPR.
TABLE 2.
Variables at initial management
| Variable |
Clinical outcome, n (%) |
|||
|---|---|---|---|---|
| Good | Poor | Death | Total | |
| GCS at scene | ||||
| 11–15 | 3 (8) | 0 (0) | 0 (0) | 3 (8) |
| 4–10 | 8 (21) | 0 (0) | 0 (0) | 8 (21) |
| ≤3 | 2 (5) | 6 (15) | 16 (41) | 24 (62) |
| (4 undocumented) | ||||
| Pulse: Arrival of emergency medical service | ||||
| Yes | 17 (44) | 3 (8) | 2 (5) | 22 (56) |
| No | 0 (0) | 3* (8) | 14 (36) | 17 (44) |
| Intubated | ||||
| Yes | 11 (28) | 6* (16) | 16 (41) | 33 (84) |
| No | 6 (16) | 0 (0) | 0 (0) | 6 (16) |
| Initial blood gas† | ||||
| pH≤7.0 | 0 (0) | 0 (0) | 2 (5) | 2 (5) |
| pH 7.1–7.2 | 1 (3) | 1 (3) | 5 (13) | 7 (18) |
| pH 7.21–7.3 | 3 (8) | 1 (3) | 3 (8) | 7 (18) |
| pH 7.31–7.4 | 5 (13) | 3 (8) | 1 (3) | 9 (23) |
| pH≥7.4 | 1 (3) | 1 (3) | 0 (0) | 2 (0) |
| (14 undocumented) | ||||
| Ligature marks | ||||
| Yes | 16 (41) | 6 (16) | 13 (33) | 35 (90) |
| No | 2 (5) | 0 (0) | 0 (0) | 2 (5) |
| (2 undocumented) | ||||
| Suspension | ||||
| Full | 2 (5) | 3 (8) | 10 (26) | 15 (38) |
| Partial | 6 (15) | 1 (3) | 1 (3) | 8 (21) |
| None | 2 (5) | 0 (0) | 2‡ (5) | 4 (10) |
| (14 undocumented) | ||||
Two additional patients were found pulseless, but the outcome was unknown because they were lost to follow-up: one to a nursing home at week 11 postinjury and one to an adult intensive care unit 24 h postadmission. Therefore, both were excluded from the remainder of the table and n=39;
Most were arterial pH, and several were unclear as to venous or arterial specimen;
Strangulation without hanging. GCS Glasgow coma score
Of the patients who were classified as having a poor outcome (n=6), GCS reports ranged from 4 to 10. However, on chart review, most of these patients were only able to open their eyes spontaneously (not to voice or pain), resulting in erroneous scoring of full marks (ie, 4) for eye-opening on the GCS. All of these patients were noted to have an absence of purposeful movements. Two of these children were eventually transferred to a rehabilitation setting, but one died two years later of suspected aspiration leading to cardiac arrest and then to multisystem organ failure. The remaining patients were transferred to extended care centres or nursing homes.
Cervical spinal cord injuries or cervical vertebral fractures were not identified by C-spine x-rays and clinical examination in any of these 41 patients. Computed tomography of the C-spine was conducted in a minority of cases in which integrity of the C-spine was unclear.
SSEPs were recorded for seven patients who remained comatose; five showed bilateral absence of SSEPs including the N20 latency. Of these five patients, three died. The two remaining patients were eventually discharged with severe neurological injuries and were dependent for all aspects of their care. Of the two patients who did not have bilateral absence of SSEPs, one died months after the event but had remained completely dependent for all care until death, and the other was discharged in a PVS.
DISCUSSION
Paediatric patients in the present study either died or had severe neurological dysfunction (completely dependent for all care) when they had been injured by hanging or strangulation, and were found pulseless. The most common outcome for those who survived resuscitation was a PVS according to a description in the medical record.
The pathophysiology of brain ischemia in hanging injuries is controversial, but is theorized to be some combination of venous congestion, arterial occlusion or vagal collapse due to stimulation of carotid baroreceptors (15). However, the finding of a GCS of 3 at the time of discovery was less predictive of poor prognosis than cited in the adult literature. Two of the children who did not receive cardiac resuscitation and had a good outcome were found with an initial GCS of 3 as determined by ambulance attendants or paramedics, and also demonstrated ‘agonal’ breathing recorded at the time of discovery.
A recent review of the paediatric (non-neonatal) literature suggests that “when performed at least 24 hrs after the inciting event, abnormal exam signs (pupil reactivity and motor response), absent N20 waves bilaterally on SSEPs, electrocerebral silence or burst suppression patterns on EEG and abnormal MRI with diffusion restriction in the cortex and basal ganglia are each highly predictive of poor outcome. Combining these modalities improves the overall predictive value” (16). Authors of adult studies have come to similar conclusions, suggesting that SSEPs are powerful predictors of death or severe disability when N20 and other latencies are bilaterally absent even once in serial testing (17,18). While used in a limited capacity (seven of 41 patients) in our series, our SSEP results seem to support this predictive capability.
The role of head or total body cooling in the setting of absent vital signs due to hanging specifically is unclear. Induction of therapeutic hypothermia for 12 h to 24 h after cardiac arrest, based on adult data, is an International Liaison Committee on Resuscitation recommendation (19,20). Bilateral absence of the N20 latency is not noted to be affected by treatments for HIE including hypothermia (21). Some patients in this series did receive head cooling therapy. Although there was no variability in terms of which records were specifically evaluated, head cooling did not seem to affect clinical outcome.
The desire to save the life of a child is powerful. However, in the present study, the outcome for children found pulseless after a hanging/strangulation injury was overwhelmingly death, followed by survival in a PVS or with a severe dependent disability. Decisions by families to continue life-sustaining therapy in the face of negative predictors after CPR then led families to make even more difficult decisions such as forgoing hydration and nutrition in one case, or proceeding with tracheostomy and prolonged artificial ventilation in others.
The present study is limited because the data were collected retrospectively. However, the outcome of severe disability or death is unlikely to be lost even in this context, and was the main finding associated with cardiac resuscitation in our patient population. Another limitation was the coding for study inclusion. Suicide attempt was intentionally excluded due to the high number of records that would have been identified unrelated to hanging, and because the inclusion diagnoses were more specific to identify the condition under study. However, this approach did miss one patient known to one author (DD). This was an adolescent patient who was found pulseless and survived with severe neurological injury; this patient was transferred to a nursing home after many weeks in our acute care setting.
CONCLUSION
It is unlikely that first responders will ever simply not provide CPR when a child is found pulseless after a hanging injury, unless there are signs of prolonged death such as rigor mortis or dependent lividity. Given the dismal prognosis for children who survive their initial resuscitation, early predictors become crucially important in further guidance of the parents and health professionals in decision making.
Future studies that are prospective in nature, and that methodically evaluate EEG, SSEP, GCS and neuron-specific enolase, are most likely to predict poor outcome within three to six days of strangulation injury. Describing these important clinical and neurophysiological parameters to families at the time of injury, and reinforcing the importance of these findings as they evolve over those first few days will provide anticipatory guidance to families in their decisions about whether to proceed with further life-saving therapy.
Acknowledgments
The authors thank Dr R Rosychuk and Jing Wang for their assistance with statistical analysis.
Footnotes
FUNDING: Stollery Children’s Hospital Foundation.
REFERENCES
- 1.Teens flirt with death in choking game. The Edmonton Journal. 2008 May 2;:A19. [Google Scholar]
- 2.Egge MK, Berkowitz CD, Toms C, Sathyavagiswaran L. The choking game. Pediatr Emerg Care. 2010;26:206–8. doi: 10.1097/PEC.0b013e3181d1e3e3. [DOI] [PubMed] [Google Scholar]
- 3.Karanth S, Nayyar V. What influences outcome of patients with suicidal hanging. J Assoc Physicians India. 2005;53:853–6. [PubMed] [Google Scholar]
- 4.Matsuyama T, Okuchi K, Seki T, Murao Y. Prognostic factors in hanging injuries. Am J Emerg Med. 2004;22:207–10. doi: 10.1016/j.ajem.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Penney DJ, Stewart AH, Parr MJ. Prognostic outcome indicators following hanging injuries. Resuscitation. 2002;54:27–9. doi: 10.1016/s0300-9572(02)00050-3. [DOI] [PubMed] [Google Scholar]
- 6.Zandbergen EG. Postanoxic coma: How (long) should we treat? Eur J Anaesthesiol Suppl. 2008;42:39–42. doi: 10.1017/S0265021507003468. [DOI] [PubMed] [Google Scholar]
- 7.Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S, Quality Standards Subcommittee of the American Academy of Neurology Practice parameter: Prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67:203–10. doi: 10.1212/01.wnl.0000227183.21314.cd. [DOI] [PubMed] [Google Scholar]
- 8.Tasker RC. Validating serologic biomarkers of brain injury for cardiac arrest research. Pediatr Crit Care Med. 2009;10:529–30. doi: 10.1097/PCC.0b013e3181a0e102. [DOI] [PubMed] [Google Scholar]
- 9.Topjian AA, Lin R, Morris MC, et al. Neuron-specific enolase and S-100B are associated with neurologic outcome after pediatric cardiac arrest. Pediatr Crit Care Med. 2009;10:479–90. doi: 10.1097/PCC.0b013e318198bdb5. [DOI] [PubMed] [Google Scholar]
- 10.Schoerkhuber W, Kittler H, Sterz F, et al. Time course of serum neuron-specific enolase. A predictor of neurological outcome in patients resuscitated from cardiac arrest. Stroke. 1999;30:1598–603. doi: 10.1161/01.str.30.8.1598. [DOI] [PubMed] [Google Scholar]
- 11.Young GB. Clinical practice. Neurologic prognosis after cardiac arrest. N Engl J Med. 2009;361:605–11. doi: 10.1056/NEJMcp0903466. [DOI] [PubMed] [Google Scholar]
- 12.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 13.Schefold JC, Storm C, Kruger A, Ploner CJ, Hasper D. The Glasgow Coma Score is a predictor of good outcome in cardiac arrest patients treated with therapeutic hypothermia. Resuscitation. 2009;80:658–61. doi: 10.1016/j.resuscitation.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Jennett B, Plum F. Persistent vegetative state after brain damage: A syndrome in search of a name. Lancet. 1972;1:734–7. doi: 10.1016/s0140-6736(72)90242-5. [DOI] [PubMed] [Google Scholar]
- 15.Ernoehazy W. Hanging Injuries and Strangulation. Emedicine from WebMD. Jul 16, 2008. < http://emedicine.medscape.com/article/826704-overview> (Accessed on August 15, 2011).
- 16.Abend NS, Licht DJ. Predicting outcome in children with hypoxic ischemic encephalopathy. Pediatr Crit Care Med. 2008;9:32–9. doi: 10.1097/01.PCC.0000288714.61037.56. [DOI] [PubMed] [Google Scholar]
- 17.Carter BG, Butt W. Review of the use of somatosensory evoked potentials in the prediction of outcome after severe brain injury. Crit Care Med. 2001;29:178–86. doi: 10.1097/00003246-200101000-00036. [DOI] [PubMed] [Google Scholar]
- 18.Robinson LR, Micklesen PJ, Tirschwell DL, Lew HL. Predictive value of somatosensory evoked potentials for awakening from coma. Crit Care Med. 2003;31:960–7. doi: 10.1097/01.CCM.0000053643.21751.3B. (Comment in ACP J Club 2004;140:24; Crit Care Med 2003;31:994) [DOI] [PubMed] [Google Scholar]
- 19.International Liaison Committee on Resuscitation The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: Pediatric basic and advanced life support. Pediatrics. 2006;117:e955–77. doi: 10.1542/peds.2006-0206. [DOI] [PubMed] [Google Scholar]
- 20.Borgquist O, Friberg H. Therapeutic hypothermia for comatose survivors after near-hanging – a retrospective analysis. Resuscitation. 2009;80:210–2. doi: 10.1016/j.resuscitation.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 21.Tiainen M, Kovala TT, Takkunen OS, Roine RO. Somatosensory and brainstem auditory evoked potentials in cardiac arrest patients treated with hypothermia. Crit Care Med. 2005;33:1736–40. doi: 10.1097/01.ccm.0000171536.63641.d9. [DOI] [PubMed] [Google Scholar]