Abstract
Childhood cancer survivors are at increased risk for chronic health conditions that may be influenced by their cancer treatment and unhealthy lifestyle behaviors. Despite the possibility that interventions targeting the survivor-parent dyad may hold promise for this population, a clearer understanding of the role of family factors and the lifestyle behaviors of both survivors and parents is needed. A mailed cross-sectional survey was conducted in 2009 to assess weight status (body mass index), lifestyle behaviors (e.g., diet, physical activity), and the quality of the parent-child relationship among 170 childhood cancer survivors who were treated at M. D. Anderson Cancer Center and 114 of their parents (80% mothers). Survivors were more physically active and consumed more fruits and vegetables than their parents. However, fewer than half of survivors or parents met national guidelines for diet and physical activity, and their weight status and fat intakes were moderately correlated (r=.30–.57, p<.001). Multilevel models showed that, compared with survivors with better-than-average relationships, those with poorer-than-average relationships with their parents were significantly more likely to consume high-fat diets (p<.05). Survivors and their parents may thus benefit from interventions that address common lifestyle behaviors, as well as issues in the family environment that may contribute to an unhealthy lifestyle.
Keywords: childhood cancer, parent-child relationship, diet, physical activity
Introduction
Compared to the general U.S. population, survivors of childhood cancer are at increased risk for developing diabetes, cardiovascular disease, and second cancers later in adulthood given the long-term sequelae of their disease and its treatment (1). As demonstrated in individuals without cancer, engaging in physical activity (PA) and consuming a low-fat diet that is high in fruits and vegetables (F&V) and whole grains may prevent these conditions and improve overall health (2–3). In the few studies that have assessed the diet and exercise behaviors of cancer survivors, suboptimal dietary intakes and levels of PA were found. However, these studies focused on specific cancer subtypes (e.g., acute lymphoblastic leukemia) (4–5). Few trials have targeted the health behaviors of childhood cancer survivors and those that have, have achieved limited success (6–9). While conclusions are limited due to the diversity of approaches and behavioral targets of such interventions, one commonality is that they all have focused exclusively on the individual survivor. Considering the immediate family environment in which lifestyle change occurs may facilitate the design of more effective trials and lasting behavioral change.
For childhood cancer survivors, lifestyle change may best be addressed as a function of the family system. The emotional climate in the home can influence eating behaviors (10). Parents can also facilitate their children’s efforts to control or lose weight by providing reinforcement and modeling appropriate behaviors (11), but the extent and nature of parental involvement in diet and exercise interventions is open to debate (12–14).
Parental involvement in interventions can entail enlisting the parent as a supporter of the child’s behavior change or actively involving and treating the parent with the child (14–16). The latter approach is consistent with family systems (17) and interpersonal theories (18) and emphasizes the role of relationship factors such as closeness, communication, and the quality of the relationship in the behavior change process (18–19). It is also posits that change is more likely to occur when: 1) a communal focus is highlighted, and 2) parents and children are taught strategies to support each other’s behavior change efforts.
When designing diet and PA interventions for survivors and their parents, it is important to assess receptivity to joint interventions as well as behaviors within the dyad to determine whether a social support or communal focus is needed. Thus, the specific aims of this exploratory study were to 1) characterize the lifestyle behaviors (diet, PA, tobacco-use) and body mass index (BMI) of childhood cancer survivors and their parents and to examine the degree of similarity between them with regard to these factors; 2) determine whether survivors and parents are interested in participating in diet and exercise interventions; and 3) determine whether there is an association between lifestyle behaviors and the quality of the parent-child relationship. Given their shared family history, it was hypothesized that survivors and parents would have concordant lifestyle behaviors and that both survivors and parents who reported better relationship quality would ascribe to a healthier lifestyle (i.e., report a healthier weight status and dietary intakes, and more PA) than those who reported poorer relationship quality.
Methods
Procedure
This cross-sectional survey study was approved by the Institutional Review Board at the University of Texas M. D. Anderson Cancer Center (MDACC) and was conducted in 2009. Survivors of leukemia, lymphoma, sarcoma, and central nervous system (CNS) cancers were identified from the MDACC Children’s Cancer Hospital database. Survivors of these cancers were targeted because little is known about their behaviors post-treatment and because, compared to other cancer survivors, they are at greater risk for developing obesity (20–21). Additional eligibility criteria for survivors were: (1) diagnosed between 1992 and 2007; (2) ≤ 18 years old at diagnosis; (3) off treatment for ≥ six months; and (4) able to read English. Parents/guardians who could read English and who identified themselves as the survivor’s current “primary caregiver” (i.e., if the survivor was younger than 18 years old) or who were identified by an adult survivor (i.e., 18 years or older) as their “primary caregiver” also participated. Signed consent was obtained for parents and adult survivors; child assent was obtained for minor-aged survivors.
Five hundred-five survivors were identified through the hospital database, however, eight were deceased and addresses on record for 215 cases were no longer valid. Thus, separate parent-child packets containing a cover letter, survey, $5 gift card incentive, and postage-paid return envelope were mailed over a 12-month period to 282 survivors and their parents. Given the breadth of survivor ages and the detailed recall required by the survey measures, parents of young children (<12 years old) could provide assistance with survey completion and were instructed to indicate this on the survey.
Measures
Mailed surveys assessed weight status, lifestyle behaviors (e.g., diet, PA, tobacco-use), receptivity to intervention, and the quality of the parent-child relationship. Surveys were comprised largely of validated measures and were completed by survivors and parents unless otherwise specified.
Weight Status
Body Mass Index (BMI)
BMI was computed from self-reported height and weight (kg/m2). Adolescent and child survivors were categorized as underweight (<5th percentile), normal (≥5th to <85th percentile), and overweight or obese (≥85th percentile) based on guidelines established by the CDC (22). Adult survivors (≥21 years old) were categorized as underweight (BMI<18.5), normal (BMI 18.5–24.9), and overweight or obese (BMI>24.9) based on established clinical guidelines (23).
Lifestyle Behaviors
Dietary Intakes
The 17-item National Cancer Institute (NCI) Multifactor Screener was used to provide general estimates of F&V intake, percentage of calories from fat, and grams of fiber over a 12-month period using established algorithms (24). As this was a mailed survey, the use of dietary recalls or lengthy food frequency questionnaires was not possible. However, this screener has been shown to provide reasonable estimates for F&V, fat, and fiber intakes (24). Age- and gender-specific cutoffs were used to determine whether participants were meeting national guidelines (25–28).
Physical Activity (PA)
Minutes of moderate to vigorous PA over the past week were calculated using the Godin Leisure-Time Exercise Questionnaire (29–30). To determine whether respondents met national PA guidelines (31), an additional item was adapted from the Youth Risk Behavior Survey (YRBS; 32); (i.e., “During the past seven days, on how many days were you physically active for at least 30 [for adults]/60 [for children] minutes per day?”).
Tobacco-Use
Two items were adapted from the YRBS to assess current and former smoking and tobacco use (32). The first item was, “Are you a smoker?” Response options were one = “I have never smoked”; two = “I used to smoke but quit”; and three = “I currently smoke.” The second item (with similar response options) was, “Do you use other tobacco products now?”
Receptivity to Participating in Diet and PA Interventions
Using items developed specifically for this study, participants indicated interest (anchors: “extremely,” “very,” “somewhat,” “a little,” or “not at all”) in learning about weight control, eating to stay healthy, and getting in shape. Items were averaged to provide an index of general interest in participating in diet and PA programs. Survivors were also asked, “Would you want others to join in the intervention with you?” Options were, “No, I’d rather do it alone” or “Yes, I’d like to do it with others.” If they answered affirmatively, they were asked whether they would like to participate with their mother, father, sister, brother, a friend, and/or other cancer survivors.
Quality of the Parent-Child Relationship
Five items rated on a four-point Likert-type scale were adapted from Lawrence (33) and assessed general closeness, communication, similarity of views about life, degree of getting along, and similarity of views about diet and exercise. Items with higher scores indicated greater endorsement. Internal scale reliabilities (Cronbach’s alpha) were αsurvivors=.80 and αparents=.83.
Data Analysis Plan
Descriptive statistics were computed for survivors and parents for each of the major study variables, and the percentages of those meeting national guidelines for diet and PA were calculated. Within-dyad correlations (34) and paired t-tests were also conducted.
Multilevel Modeling
Even though the study aim was to examine the effects of each person’s reports of relationship quality on his/her own lifestyle behaviors, the data could not be analyzed separately because parent and survivor responses are not independent. A mixed-models approach can handle this non-independence while allowing flexibility to include data from all participants (regardless of whether both dyad members completed surveys) in the analyses (35). Thus, to evaluate the degree to which each of the lifestyle behaviors varied as a function of relationship quality, social role (i.e., survivor or parent), and the interaction between these variables, six models were tested using the Proc Mixed procedure in the Statistical Analysis Software (Version 9.2, 2010, SAS Institute Inc, Canary, NC). The simple slopes of the significant interactions were tested using procedures developed specifically for multilevel models (36).
Results
Sample Characteristics
Of the 282 survivor-parent dyads who received surveys, responses were received from one or both dyad members in 174 cases (overall response rate of 61%). Specifically, 106 surveys were returned by the survivor only, 50 by the parent only, and 64 by both survivor and parent (complete dyads), resulting in a final sample of 170 survivors and 114 parents. No significant differences were observed between respondents and non-respondents on the basis of race, diagnosis, age, or time since diagnosis. However, survivor respondents were more often female, younger, and closer to diagnosis (p-values < 0.05). Likewise, survivors from complete dyads were younger (M=15.17, SD=5.17) than those from incomplete dyads (M=22.16, SD=3.19; t(165)=−9.58, p=.0001).
Parents were mostly female (80%) and white (72%); 75% had at least some college education, and the average age was 42.6 years (SD=7.7). Differences between male and female parents on the major study variables were not significant. Approximately 32% of survivors had CNS tumors, 32% leukemia, 17% lymphoma, and 19% sarcoma. They were mostly white (69%), and relatively evenly divided by gender (52% male). The average age at diagnosis was 8.8 years (SD=10.2), and age at the time of the study was M=17.8 years, SD=8.3years; 32% of survivors were ≥ 21 years old. Approximately 81% of survivors over age 21 had completed at least some college, 65% were employed, and 42% still lived with their parents.
Thirty-nine survivors (23%) received assistance with survey completion. These survivors were significantly (p-values <.001) younger both at the time of the study (M=13.18 years, SD=2.82) and at diagnosis (M=5.30 years, SD=3.24) than survivors not receiving assistance (Mage at time of study=19.01 years, SD=5.56; Mage at diagnosis=10.16 years, SD=5.50).
Lifestyle Behaviors and Similarities between Survivors and Their Parents
Table 1 details descriptive statistics for survivors and parents for each of the major study variables.
Table 1.
Descriptive results for childhood cancer survivors and their parents
| Survivorsa (N=170)
|
Parents (N=114)
|
Paired t-testc | Partial correlation (r)d | |||||
|---|---|---|---|---|---|---|---|---|
| Mean±Standard deviation | Range | Percentage meeting guidelinesb | Mean±Standard deviation | Range | Percentage meeting guidelinesb | |||
| Body Mass Index (BMI) | 22.20 ± 5.24 | 13.48 – 50.60 | 55.6 | 27.40 ± 6.04 | 18.54 – 51.49 | 43.1 | −7.73** | .30** |
| Fruit and vegetable intake (servings/day) | 4.07 ± 1.69 | 1.10 – 9.23 | 24.0 | 3.71 ± 1.29 | 1.80 – 7.96 | 12.2 | 1.99* | .03 |
| Fiber intake (g/day) | 16.65 ± 5.94 | 7.51 – 34.54 | 4.3 | 15.11 ± 4.86 | 7.65 – 33.69 | 9.1 | 1.92 | .14 |
| Percent of energy from fat | 32.98 ± 6.17 | 15.43 – 59.96 | 63.9 | 33.07 ± 6.32 | 22.93 – 76.09 | 73.4 | .86 | .57** |
| Physical activity e | 164.44 ± 125.75 | 0 – 564.00 | 35.2 | 106.39 ± 372.23 | 0 – 392.00 | 30.0 | 4.08** | −.02 |
Note:
p<.05;
p<.001;
32% of survivors had CNS tumors, 32% leukemia, 17% lymphoma, and 19% sarcoma;
percentage meeting national guidelines are based on the following: for fruit and vegetable intake, percentages refer to those consuming 5 or more fruit and vegetable servings per day; percentages of those meeting guidelines for fiber intake are based on grams consumed as a function of assumed age-appropriate energy intakes and used cut points recommended by the Food and Nutrition Board of the Institute of Medicine; for dietary fat intake, those meeting national guidelines consumed 20–35% of their energy from fat; for physical activity, those meeting national guidelines are based on a single item from Youth Risk Behavior Survey (YRBS);
paired t-tests between survivor and parent means;
partial correlations between survivors and parents;
means and standard deviations are for Godin minutes of moderate and vigorous physical activity
Over one-half of parents and 45% of survivors were overweight or obese. Only one-third of survivors and parents met national guidelines for PA, and few met guidelines for F&V consumption. BMI and dietary fat intake of survivors and parents were significantly and moderately correlated, but levels of PA were not. Survivors also had significantly lower BMI than their parents, engaged in more PA, and consumed more servings of F&Vs. There was also a trend toward increased intake of fiber among survivors. Results for tobacco-use showed that only 7.4% (N=10) of survivors were current smokers and 5.2% (N=7) were recent quitters. Likewise, a small percentage of parents were either current smokers (6.3%, N=7) or recent quitters (20.5%, N=23), and few survivors (6.6%) and parents (9.9%) had ever used other tobacco products. Because so few participants were current smokers or had a prior tobacco history, it was excluded from subsequent analyses.
Are Survivors and Parents Interested in Participating in Diet and PA Programs?
Approximately 75% of survivors and 84.2% of parents indicated that they were either “very” or “extremely” interested in participating in weight control programs; 86.5% of survivors and 88.6% of parents were “very” or “extremely” interested in participating in PA programs. Programs focusing on eating better to stay healthy also were popular; 83.5% of survivors and 89.5% of parents indicated they would be very or extremely interested in participating in such programs. Most survivors (56%) favored partnered interventions. Survivors readily endorsed mothers (45.9%) and fathers (30.2%) as their preferred intervention partners. About 79% of the child/adolescent survivors and 85% of the adult survivors reported interest in participating with a parent, but this difference was not significant.
Is There an Association Between the Quality of the Parent-Child Relationship and Lifestyle Behaviors?
With regard to BMI, the interaction between relationship quality and social role was not significant; however, a significant main effect was found for social role, such that survivors had significantly lower BMI than their parents (Table 2). No significant main effects or interactions were found for F&V consumption, fiber, and PA (data not tabled).
Table 2.
Multilevel modeling results showing the effects of parent-child relationship quality on weight status and dietary fat intake among childhood cancer survivors (N=170) and their parents (N=114)
| Body Mass Index (BMI)
|
Percent energy from fat
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Raw Coefficient (B) | Standard Error | t-test | Effect size (r)c | Raw Coefficient (B) | Standard Error | t-test | Effect size (r)c | |
| Intercepta | 26.15 | .45 | -- | 33.03 | .50 | |||
| Social roleb | −1.96 | .36 | −5.50** | .45 | .02 | .37 | .05 | -- |
| Relationship quality | −.12 | .82 | −.15 | -- | −1.88 | .92 | −2.05* | .14 |
| Social role × Relationship quality | .55 | .73 | .76 | -- | −1.51 | .76 | −2.00* | .18 |
Note.
Predictor variables were grand-mean centered to more directly interpret the intercept.
Effect coding was used for the variable of social role (parent = −1, survivor = 1).
The effect size r associated with each t: ,
p<.05,
p<.01
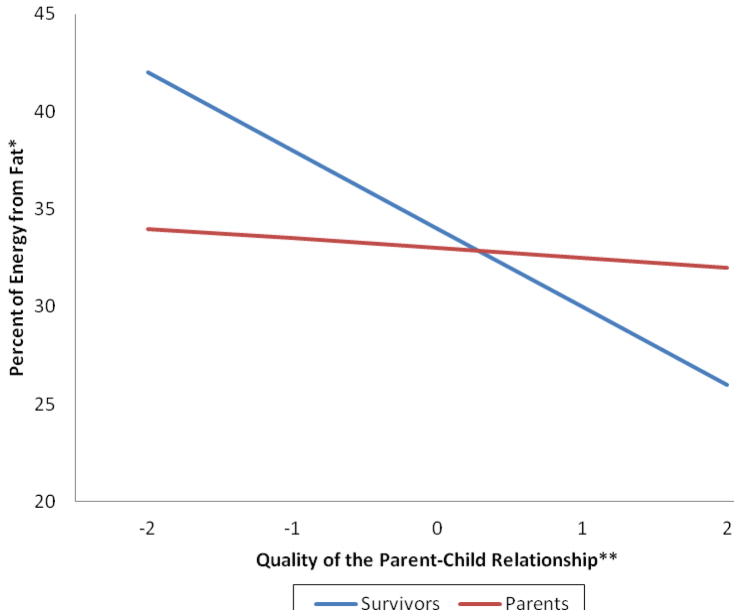
Regarding percentage of energy from fat, the relationship quality × social role interaction was significant (Table 2; Fig. 1). Simple slopes analysis showed that the slope for parents was not significant (b =−.36; p>.10) but that the slope for survivors was significant (b2=−3.4, SE=.15; t =−22.13, p=.001). Note that in Fig. 1, the “0” on the X-axis represents the mean for relationship quality because that variable was grand-mean centered. Thus, compared to survivors with better-than-average relationship quality, those with poorer-than-average relationship quality were significantly more likely to exceed national guidelines by obtaining more than 35% of their energy from fat.
Figure 1.
Graphical depiction of the different effects of parent-child relationship quality on dietary fat intake among childhood cancer survivors (N=170) and their parents (N=114)a
* To assess fat intake, the 17-item NCI multifactor screener was used.
** To assess the quality of the parent-child relationship, five items rated on a four-point Likert-type scale were adapted from Lawrence (33) that asked about general closeness, communication, similarity of views about life, degree of getting along, and similarity of views about diet and exercise.
a The figure shows that survivors reporting better than average parent-child relationship quality were significantly more likely to consume low-fat diets than those reporting poorer than average relationship quality. Parents who reported better than average relationship quality reported slightly lower levels of fat intake than those with poorer than average relationship quality, but the difference was not significant. Because relationship quality was grand-mean centered, −2 and 2 are the upper and lower possible values and 0 represents the mean.
Discussion
This is one of the first studies to document the diet and exercise behaviors of both childhood cancer survivors and their parents and to examine the degree of similarity between the two. Despite the fact that 64% of survivors and 73% of parents met guidelines for percent of energy obtained from fat, 45% of survivors and 57% of parents were overweight or obese and their weight status and fat intakes were significantly correlated. These rates are likely underestimated due to the use of self-report methods (37). They are also concerning because the rates of overweight/obesity reported by the childhood cancer survivors in the study (45%) far exceed rates reported for children and adolescents in the U.S. (17%) (38). The fact that 65–70% of the study sample was not meeting recommendations for moderate or vigorous intensity PA is a likely contributing factor. This rate of sedentary behavior is comparable to the rate for U. S. adults (70%) and slightly exceeds the rate for young adults aged 18–24 (57%) (39–40). Although survivors reported significantly more PA than parents, only one-third of parents and survivors met national exercise guidelines (41), and their reports of PA were not correlated, suggesting they may not exercise together. Percentages of survivors and parents who did not meet recommendations for F&V consumption (76–88%) also exceeded national averages (65–73%) (42). Thus, in some cases, the study sample had a more problematic risk profile than those of adults and children/adolescents nationally, and in other cases, their risk was comparable. This is similar to other published studies of health behaviors among childhood cancer survivors (43) and their guardians (5) and is troubling because of the increased vulnerability of childhood cancer survivors to weight-related illnesses like diabetes and cardiovascular disease (20–21).
Taken together, study findings underscore the need to address modifiable risk factors such as diet and PA in this population and that effort to reduce the prevalence of obesity in this population should focus on increasing energy expenditure as well as reducing energy intake. Indeed, most survivors (81%) and parents (86%) expressed interest in weight control and PA interventions, and both adult and child/adolescent survivors indicated a clear preference for participating in such interventions with a parent. Thus, childhood cancer survivors may desire and benefit from active parental involvement in diet and exercise programs. Given that a significant number of parents in the study sample were overweight and sedentary, parents of childhood cancer survivors may likewise benefit from active involvement in such programs.
Programs that include survivors and their parents may be enhanced by including a component that addresses the parent-child relationship. Survivors in this study who had poorer-than-average relationships were also significantly more likely to consume higher-fat diets than those with better-than-average relationships. Given the cross-sectional nature of the data and global nature of the relationship quality measure, interpretations of the data are limited. However, it is possible that in closer, more cohesive families, parents may closely regulate the amount of dietary fat their children consume (44). It is also possible that survivors may turn to comfort foods that are high in fat when the quality of their familial relationships is low (45). Finally, less cohesive families may be less likely to eat together and consume more fast food, which is often high in fat (46).
This study had limitations. The number of usable addresses from survivors’ medical records was initially overestimated. Despite this, 61% of those who were contactable returned surveys and this overall response rate is still within acceptable limits (47). The sample was relatively homogeneous with regard to race/ethnicity, and information about family structure was not collected. Although mothers are primary caregivers and more survivors nominated mothers as their preferred intervention partners, 80% of the parent participants were mothers, so findings may not generalize to all parent-child relationships. Additionally, developmental changes and changes in behaviors and relationship quality over time were not assessed, thus causality cannot be inferred. The study researchers did not collect any data on social desirability bias so it is impossible to know whether some individuals simply have more of a tendency to report more cohesive relationships or better adherence to guidelines than others. Finally, more precise measures of weight status and diet as well as a measure that taps more specific components of relationship quality (e.g., the amount of time parents and survivors spend together, communication about nutrition, and the number of times per week participants ate out or separately) may have yielded stronger results.
Conclusion
While the majority of childhood cancer survivors and their parents failed to meet national recommendations for dietary intake and PA and a sizeable proportion were overweight/obese, both reported strong interest in participating in diet and exercise interventions and pursuing such programs together. Results also suggested that the quality of the survivor-parent relationship was associated with some lifestyle behaviors. Thus, survivors and parents may benefit from joint interventions that address common lifestyle behaviors, as well as relationship factors that may contribute to an unhealthy lifestyle. More research is need to identify barriers to a healthy lifestyle in this population, whether joint interventions are more effective and result in lasting behavioral change compared to those that target the survivor alone, and whether interventions that simultaneously address multiple, interrelated behaviors (e.g., diet and PA) have a greater likelihood for reducing risk and improving quality of life compared to interventions that only address a single behavior (43).
Acknowledgments
This research was supported in part by a National Cancer Institute grant (R03CA136537) awarded to Dr. Badr and a generous donation from the Santa’s Elves Fund at MD Anderson Cancer Center awarded to Drs. Demark-Wahnefried and Ater.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hoda Badr, Department of Oncological Sciences, Mount Sinai School of Medicine, New York, NY
Raheem J. Paxton, Departments of Health Disparities Research and Epidemiology, The University of Texas MD Anderson Cancer Center, Houston, TX
Joann L. Ater, Division of Pediatrics, The Children’s Cancer Hospital at The University of Texas MD Anderson Cancer Center, Houston, TX
Diana Urbauer, Division of Quantitative Sciences, The University of Texas MD Anderson Cancer Center, Houston, TX
Wendy Demark-Wahnefried, Department of Nutrition Sciences, University of Alabama at Birmingham Comprehensive Cancer Center, Birmingham, AL
References
- 1.Mertens A, Cotter K, Foster B, Zebrack B, Hudson M, Eshelman D, Loftis L, Sozio M, Oeffinger K. Improving health care for adult survivors of childhood cancer: recommendations from a delphi panel of health policy experts. Health Policy. 2004;69(2):169–178. doi: 10.1016/j.healthpol.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Demark-Wahnefried W, Aziz NM, Rowland JH, Pinto BM. Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol. 2005;23(24):5814–5830. doi: 10.1200/JCO.2005.01.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown JK, Byers T, Doyle C, Coumeya KS, Demark-Wahnefried W, Kushi LH, McTieman A, Rock CL, Aziz N, Bloch AS, Eldridge B, Hamilton K, Katzin C, Koonce A, Main J, Mobley C, Morra ME, Pierce MS, Sawyer KA. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2003;53(5):268–291. doi: 10.3322/canjclin.53.5.268. [DOI] [PubMed] [Google Scholar]
- 4.Butterfield R, Park E, Puleo E, Mertens A, Gritz E, Li F, Emmons K. Multiple risk behaviors among smokers in the childhood cancer survivors study cohort. Psychooncology. 2004;13(9):619–629. doi: 10.1002/pon.764. [DOI] [PubMed] [Google Scholar]
- 5.Demark-Wahnefried W, Werner C, Clipp E, Guill A, Bonner M, Jones L, Rosoff P. Survivors of childhood cancer and their guardians. Cancer. 2005;103(10):2171–2180. doi: 10.1002/cncr.21009. [DOI] [PubMed] [Google Scholar]
- 6.Absolom K, Eiser C, Greco V, Davies H. Health promotion for survivors of childhood cancer: a minimal intervention. Patient Educ Couns. 2004;55(3):379–384. doi: 10.1016/j.pec.2003.04.007. [DOI] [PubMed] [Google Scholar]
- 7.Cox C, McLaughlin R, Rai S, Steen B, Hudson M. Adolescent survivors: A secondary analysis of a clinical trial targeting behavior change. Pediatr Blood Cancer. 2005;45(2):144–154. doi: 10.1002/pbc.20389. [DOI] [PubMed] [Google Scholar]
- 8.Hudson M, Tyc V, Srivastava D, Gattuso J, Quargnenti A, Crom D, Hinds P. Multi-component behavioral intervention to promote health protective behaviors in childhood cancer survivors: the protect study. Med Pediatr Oncol. 2002;39(1):2–11. doi: 10.1002/mpo.10071. [DOI] [PubMed] [Google Scholar]
- 9.Emmons K, Puleo E, Park E, Gritz E, Butterfield R, Weeks J, Mertens A, Li F. Peer-delivered smoking counseling for childhood cancer survivors increases rate of cessation: The partnership for health study. J Clin Oncol. 2005;23(27):6516–6523. doi: 10.1200/JCO.2005.07.048. [DOI] [PubMed] [Google Scholar]
- 10.Birch L, Fisher J. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(3):539–549. [PubMed] [Google Scholar]
- 11.Davison K, Birch L. Childhood overweight: a contextual model and recommendations for future research. Obes Rev. 2001;2(3):159–171. doi: 10.1046/j.1467-789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McLean N, Griffin S, Toney K, Hardeman W. Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. Int J Obes. 2003;27(9):987–1005. doi: 10.1038/sj.ijo.0802383. [DOI] [PubMed] [Google Scholar]
- 13.Golan M. Parents as agents of change in childhood obesity – from research to practice. Int J Pediatr Obes. 2006;1(2):66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- 14.Glenny A, O’meara S, Melville A, Sheldon T, Wilson C. The treatment and prevention of obesity: a systematic review of the literature. Int J Obes Relat Metab Disord. 1997;21(9):715–737. doi: 10.1038/sj.ijo.0800495. [DOI] [PubMed] [Google Scholar]
- 15.Epstein L, Myers M, Raynor H, Saelens B. Treatment of pediatric obesity. Pediatrics. 1998;101(3):554–570. [PubMed] [Google Scholar]
- 16.McLean N, Griffin S, Toney K, Hardeman W. Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. Int J Obes Relat Metab Disord. 2003;27(9):987–1005. doi: 10.1038/sj.ijo.0802383. [DOI] [PubMed] [Google Scholar]
- 17.Weihs KL, Fisher L, Baird M. Families, health, and behavior. Fam Syst Health. 1999;20:7–46. [Google Scholar]
- 18.Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. Understanding health behavior change among couples: An interdependence and communal coping approach. Soc Sci Med. 2006;62(6):1369–1380. doi: 10.1016/j.socscimed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychol Bull. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 20.Oeffinger K, Mertens A, Sklar C, Yasui Y, Fears T, Stovall M, Vik T, Inskip P, Robison L. Obesity in adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2003;21(7):1359–1365. doi: 10.1200/JCO.2003.06.131. [DOI] [PubMed] [Google Scholar]
- 21.Talvensaari K, Lanning M, Tapanainen P, Knip M. Long-term survivors of childhood cancer have an increased risk of manifesting the metabolic syndrome. J Clin Endocrinol Metab. 1996;81(8):3051–3055. doi: 10.1210/jcem.81.8.8768873. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(5):1314–1320. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- 23.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 24.Thompson FE, Midthune D, Subar AF, Kahle LL, Schatzkin A, Kipnis V. Performance of a short tool to assess dietary intakes of fruits and vegetables, percentage energy from fat and fibre. Public Health Nutr. 2004 Dec;7(8):1097–1105. doi: 10.1079/PHN2004642. [DOI] [PubMed] [Google Scholar]
- 25.Gidding SS, Dennison BA, Birch LL, Daniels SR, Gillman MW, Lichtenstein AH, Rattay KT, Steinberger J, Stettler N, Van Horn L. Dietary recommendations for children and adolescents: a guide for practitioners: consensus statement from the American Heart Association. Circulation. 2005 Sep 27;112(13):2061–2075. doi: 10.1161/CIRCULATIONAHA.105.169251. [DOI] [PubMed] [Google Scholar]
- 26.Kushi L, Byers T, Doyle C, Bandera E, McCullough M, Gansler T, Andrews K, Thun M. American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2006;56(5):254–281. doi: 10.3322/canjclin.56.5.254. [DOI] [PubMed] [Google Scholar]
- 27.Fogli-Cawley JJ, Dwyer JT, Saltzman E, McCullough ML, Troy LM, Meigs JB, Jacques PF. The 2005 Dietary Guidelines for Americans and risk of the metabolic syndrome. Am J Clin Nutr. 2007 Oct;86(4):1193–1201. doi: 10.1093/ajcn/86.4.1193. [DOI] [PubMed] [Google Scholar]
- 28.World Cancer Research Fund/American Institute for Cancer Research expert report: Food, Nutrition, Physical Activity, and the Prevention of cancer: a global perspective. 2007 http://www.dietandcancerreport.org/?p=er&JServSessionIdr010=xoaqdimtz2.app43a.
- 29.Godin G, Jobin J, Bouillon J. Assessment of leisure time exercise behavior by self-report: a concurrent validity study. Can J Public Health. 1986 Sep–Oct;77(5):359–362. [PubMed] [Google Scholar]
- 30.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985 Sep;10(3):141–146. [PubMed] [Google Scholar]
- 31.2008 Physical Activity Guidelines for Americans. 2008 www.health.gov/paguidelines.
- 32.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Brener ND, Wechsler H. Youth risk behavior surveillance--United States, 2007. MMWR Surveill Summ. 2008 Jun 6;57(4):1–131. [PubMed] [Google Scholar]
- 33.Lawrence R, Tennstedt S, Assmann S. Quality of the Caregiver-Care Recipient Relationship: Does It Offset Negative Consequences of Caregiving for Family Caregivers? Psychol Aging. 1998;13(1):150–158. doi: 10.1037//0882-7974.13.1.150. [DOI] [PubMed] [Google Scholar]
- 34.Gonzalez R, Griffin D. The correlational analysis of dyad-level data in the distinguishable case. Pers Relatsh. 1999;6(4):449–469. [Google Scholar]
- 35.Kenny D, Kashy DA, Cook D. Dyadic data analysis. New York: Guilford; 2006. [Google Scholar]
- 36.Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31(4):437–448. [Google Scholar]
- 37.Flood V, Webb K, Lazarus R, Pang G. Use of self report to monitor overweight and obesity in populations: some issues for consideration. Aust N Z J Public Health. 2000;24(1):96–99. doi: 10.1111/j.1467-842x.2000.tb00733.x. [DOI] [PubMed] [Google Scholar]
- 38.CDC. [Accessed August 13, 2010];Overweight Children Ages 6–17: Percentage has Increased from 6% in 1976 to 17% in 2006. http://www.cdc.gov/Features/dsOverweightChildren/
- 39.McCracken M, Jiles R, Blanck H. Health behaviors of the young adult US population: behavioral risk factor surveillance system, 2003. Prev Chronic Dis. 2007;4(2):A25. [PMC free article] [PubMed] [Google Scholar]
- 40.Schoenborn C, Adams P. Health behaviors of adults: United States, 2005–2007. Vital and health statistics. Series 10, Data from the National Health Survey. 2010;(245):1. [PubMed] [Google Scholar]
- 41.The Surgeon General’s call to action to prevent and decrease overweight and obesity. US Department of Health and Human Services, Public Health Service, Office of the Surgeon General; Rockville, MD: 2001. [PubMed] [Google Scholar]
- 42.Casagrande S, Wang Y, Anderson C, Gary T. Have Americans Increased Their Fruit and Vegetable Intake?:: The Trends Between 1988 and 2002. Am J Prev Med. 2007;32(4):257–263. doi: 10.1016/j.amepre.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 43.Rabin C, Politi M. Need for health behavior interventions for young adult cancer survivors. American Journal of Health Behavior. 2010;34(1):70–76. doi: 10.5993/ajhb.34.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kitzmann K, Dalton W, III, Buscemi J. Beyond Parenting Practices: Family Context and the Treatment of Pediatric Obesity*. Fam Relat. 2008;57(1):13–23. [Google Scholar]
- 45.Wyatt S, Winters K, Dubbert P. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. The American journal of the medical sciences. 2006;331(4):166. doi: 10.1097/00000441-200604000-00002. [DOI] [PubMed] [Google Scholar]
- 46.Patrick H, Nicklas T. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr. 2005;24(2):83. doi: 10.1080/07315724.2005.10719448. [DOI] [PubMed] [Google Scholar]
- 47.Dillman D. The design and administration of mail surveys. Annu Rev Sociol. 1991;17(1):225–249. [Google Scholar]