Abstract
Food insecurity, which affects >1 billion people worldwide, is inextricably linked to the HIV epidemic. We present a conceptual framework of the multiple pathways through which food insecurity and HIV/AIDS may be linked at the community, household, and individual levels. Whereas the mechanisms through which HIV/AIDS can cause food insecurity have been fairly well elucidated, the ways in which food insecurity can lead to HIV are less well understood. We argue that there are nutritional, mental health, and behavioral pathways through which food insecurity leads to HIV acquisition and disease progression. Specifically, food insecurity can lead to macronutrient and micronutrient deficiencies, which can affect both vertical and horizontal transmission of HIV, and can also contribute to immunologic decline and increased morbidity and mortality among those already infected. Food insecurity can have mental health consequences, such as depression and increased drug abuse, which, in turn, contribute to HIV transmission risk and incomplete HIV viral load suppression, increased probability of AIDS-defining illness, and AIDS-related mortality among HIV-infected individuals. As a result of the inability to procure food in socially or personally acceptable ways, food insecurity also contributes to risky sexual practices and enhanced HIV transmission, as well as to antiretroviral therapy nonadherence, treatment interruptions, and missed clinic visits, which are strong determinants of worse HIV health outcomes. More research on the relative importance of each of these pathways is warranted because effective interventions to reduce food insecurity and HIV depend on a rigorous understanding of these multifaceted relationships.
INTRODUCTION
Food insecurity, defined as having uncertain or limited availability of nutritionally adequate or safe food or the inability to acquire personally acceptable foods in socially acceptable ways (1), is a leading cause of morbidity and mortality worldwide and is inextricably linked to the HIV epidemic. More than 1 billion people worldwide are estimated to lack sufficient dietary energy availability (2), and the prevalence of food insecurity is particularly high among PLWHA5 in both resource-rich and resource-poor settings. For example, studies from Kenya and Uganda have shown that the vast majority of PLWHA are moderately or severely food insecure (3, 4). In San Francisco, Atlanta, and Vancouver, nearly one-half of HIV-infected patients on ART have been estimated to be food insecure (5–8). Women are the most affected by the parallel epidemics of HIV/AIDS and food insecurity, because of sex discrimination, poverty, and the absence of support as head of household (5, 9–13).
HIV/AIDS worsens family food insecurity because of the debilitation of the most productive household members, decreased individual and household economic capacity, and increased caregiver burden (14–17). Food insecurity, in turn, leads to both increased risk of HIV transmission and more rapid HIV disease progression across settings in both resource-rich and resource-poor countries. Specifically, food insecurity increases the likelihood of risky sexual practices, which exacerbates the horizontal spread of HIV/AIDS (13), and can also increase the likelihood of vertical transmission through risky infant-feeding practices (18) and malnutrition (19, 20). Among people already infected with HIV/AIDS, food insecurity has been associated with lower ART adherence (8, 21), declines in physical health status (7, 22), decreased viral suppression (8, 23), worse immunologic status (7, 24), increased incidence of serious illness (22), and increased mortality (6).
As a result of the bidirectional links between food insecurity and HIV/AIDS, numerous researchers, governments, and international organizations have proposed the integration of nutrition and HIV/AIDS programming activities (9, 25–28). A sound understanding of the complex linkages between food insecurity and HIV/AIDS is critical if we are to provide empiric evidence to guide the integration of food programs and HIV programs to decrease HIV acquisition, optimize treatment outcomes, and improve quality of life for PLWHA and their families. In this article, we propose a conceptual framework to explain the vicious cycle of food insecurity and HIV/AIDS, to inform research priorities and help in the development of effective interventions.
OVERVIEW OF CONCEPTUAL FRAMEWORK
Food insecurity and HIV/AIDS are intertwined in a vicious cycle through nutritional, mental health, and behavioral pathways. The complex relationships among these phenomena can best be portrayed with the use of a conceptual framework. Conceptual frameworks have been useful in the depiction and analysis of hypothesized causal associations in complicated health problems, especially those determined by social and biological factors such as malnutrition or infectious diseases in developing countries (29, 30).
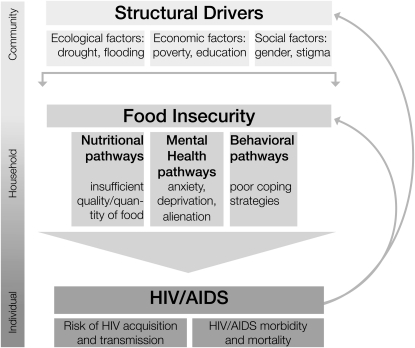
Our conceptual framework spans 3 levels of determinants (ie, community, household, and individual) and draws on several existing models that describe the linkages between HIV/AIDS, food security, and socioeconomic well-being (Figure 1) (31–34). Broader structural factors influence food insecurity, including ecologic features (eg, drought, flooding), socioeconomic factors (eg, poverty, access to education), and social factors (eg, sex inequality, HIV-related stigma). Food insecurity typically operates at the level of the household and is influenced by other household-level factors such as family structure and social support. Food insecurity, in turn, shapes individual actions and health outcomes through nutritional, mental health, and behavioral pathways. Within this framework, an outcome within one sphere precipitates changes in outcomes within another sphere. For example, when a household loses a family member to HIV-related illness or death, the household may have less income, become more food insecure, or need to sell household assets for additional income. With fewer assets, surviving household members may fall into behavioral patterns that increase the risk of HIV transmission to others, which reinitiates the cycle of food insecurity and HIV/AIDS.
FIGURE 1.
Conceptual framework for food insecurity and HIV/AIDS linkages.
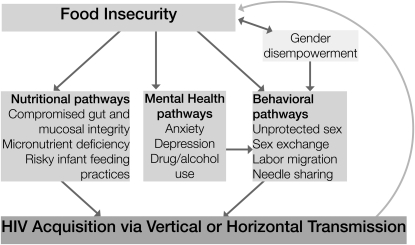
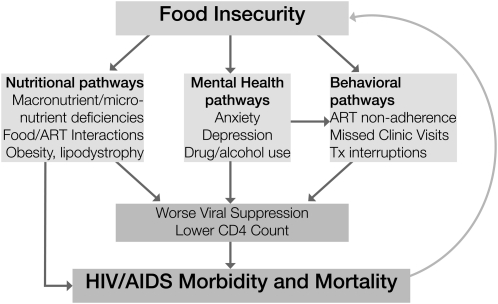
The nutritional, mental health, and behavioral pathways through which food insecurity negatively affects HIV acquisition and disease progression emerge directly from the USDA definition of food insecurity (35). Insufficient quality and quantity of food can lead to macronutrient and micronutrient deficiencies, which can affect both HIV acquisition and health outcomes among HIV-infected persons. Feelings of deprivation or anxiety about food supply can have mental health consequences, such as depression, that can contribute to HIV transmission risk as well as worse health outcomes among HIV-infected persons. The inability to procure food in socially or personally acceptable ways can, on one hand, lead to risky sex and enhanced HIV transmission, and, on the other hand, lead to ART nonadherence, treatment interruptions, and missed clinic visits, which can affect HIV health outcomes. Finally, HIV/AIDS and associated stigma can lead to decreased social support and greater food insecurity, which perpetuate the cycle between food insecurity and HIV/AIDS. In the sections that follow, we describe current research on the numerous links between food insecurity and HIV/AIDS, with an emphasis on the nutritional, mental health, and behavioral pathways through which food insecurity can lead to HIV acquisition and disease progression (Figures 2 and 3).
FIGURE 2.
Food insecurity and HIV acquisition.
FIGURE 3.
Food insecurity and HIV/AIDS morbidity and mortality. ART, antiretroviral therapy; Tx, treatment.
HIV/AIDS CONTRIBUTES TO FOOD INSECURITY
HIV/AIDS–related morbidity and mortality is well established as a cause of adverse social and economic consequences for households, including increased food insecurity (Figure 1) (16, 36). When working-age adults fall ill, households lose income, assets, labor, and skills; the subsequent treatment and funeral costs can be catastrophic (37–46). For example, national survey data from Kenya indicate that the net value of household crop production declined by 68% after the death of a male head of household, and that affected households adopted short-term survival strategies (such as the sale of productive assets and a shift from high-value to subsistence crops) that impaired financial viability in the long term (47). Even after people initiate ART, which can lead to rapid functional improvement (48), their livelihoods may have degraded to such a point that a return to previous levels of economic productivity is no longer possible (49). Furthermore, intergenerational transmission of poverty and food insecurity occurs when children are withdrawn from school to provide informal care, to compensate for lost adult labor, or because school fees become unaffordable (50, 51). Fewer assets (especially arable land), lower household earning potential, less education, and increased household expenses, in turn, worsen food insecurity.
Whereas households affected by HIV/AIDS are particularly susceptible to food insecurity, they are often least able to rely on social support for assistance. Borrowing and other transfers from kin and social networks typically serve as informal insurance against health and agricultural shocks (52–55). However, HIV, which is concentrated among the poor, continues to be heavily stigmatized in much of sub-Saharan Africa; this stigma can prevent HIV-affected households from drawing on informal support (56). For example, in a longitudinal study among HIV-infected ART-treated individuals in rural Uganda, both internalized HIV stigma (internalized negative views about HIV/AIDS by PLWHA) and enacted HIV stigma (experiences of discrimination related to HIV status) were strongly associated with food insecurity, which suggests that HIV stigma may contribute to the negative effects of HIV/AIDS on food security (57).
PATHWAYS THAT LINK FOOD INSECURITY AND HIV ACQUISITION
Data from a number of sources have suggested that food insecurity can increase susceptibility to HIV in resource-rich and resource-poor settings alike (13, 16, 58). Despite the observed association between food insecurity and HIV acquisition, the precise mechanisms that underlie potential causation are poorly understood. Our conceptual framework, which incorporates nutritional, mental health, and behavioral pathways, may provide a useful tool for the exploration of causal linkages between food insecurity and HIV acquisition (Figure 2).
Nutritional pathways
Food insecurity leads to general undernutrition (protein and energy deficiencies) as well as micronutrient deficiencies (59–64). Micronutrient deficiencies in uninfected, HIV-exposed individuals can impair the integrity of the gut and genital epithelial lining and the differentiation of target cells, and can cripple other host defense mechanisms, which can, in turn, increase susceptibility to infection in both adults and infants (65). In HIV-infected individuals oxidative stress caused by micronutrient deficiencies may cause HIV viral loads to increase (66), and thereby increase an individual's infectiousness and likelihood of transmission of HIV to others (67). Among those who receive ART, food insecurity has also been associated with unsuppressed viral loads (8), which are known to heighten the risk of secondary HIV transmission via vertical and sexual routes and through the use of injection drugs. In terms of macronutrient deficiencies and infectivity, wasting and low weight gain during pregnancy were associated with increased mother-to-child transmission in a prospective study in Tanzania (19). Food insecurity can also increase vertical transmission of HIV/AIDS by increasing the prevalence of mixed formula and breastfeeding, a practice that has been shown to increase the risk of mother-to-child transmission 4-fold compared with exclusive breastfeeding (68). In Malawi, for example, women who experienced food insecurity felt that their breast milk production was inadequate and were more likely to supplement with other non–breast milk sources of nutrition before their children were 6 mo of age (18).
Mental health pathways
Qualitative studies conducted in diverse cultural contexts among non-HIV-infected persons have identified feelings of helplessness, shame, and humiliation as central to the experience of food insecurity (69–72). Correspondingly, quantitative studies among HIV-uninfected persons have confirmed an association between food insecurity and depression (73–76). Among PLWHA, several studies have similarly reported that food insecurity is associated with depression (77, 78) and decreased overall mental health status (7). At least one study has shown that the effects of food insecurity on depression were most pronounced among women (79). Food insecurity has also been associated with drug and alcohol use and tobacco dependence in a number of studies (5, 7, 78). Worse mental health and drug abuse, in turn, are strongly associated with HIV transmission risk behaviors (80–83). However, there has been little study of the role of mental health in mediating HIV transmission risk among food-insecure individuals.
Behavioral pathways
Some people engage in high-risk sexual behaviors as a means of coping with food insecurity, which contributes to enhanced HIV transmission risk (84, 85). In a large population-based cross-sectional study in Botswana and Swaziland, food insufficiency (not enough food to eat, per self-report) was independently associated with inconsistent condom use with a nonprimary partner, sex exchange, intergenerational sexual relationships, and lack of control in sexual relationships among women (13). In a cross-sectional study among 320 sex workers in Lagos, Nigeria, 35% of respondents said that poverty and lack of other means to get food were responsible for their decision to join the sex trade industry (86). Qualitative studies conducted in Botswana, Swaziland, and Uganda showed that women's control over sexual decision making is severely constrained as a result of their dependence on men for food and other resources (87, 88). Women in these settings often feel that they have to engage in unsafe sex to negotiate their subsistence needs, and food insecurity can contribute to sex exchange in situations in which women feel they have no other options for feeding themselves and their children.
Food insecurity has also been shown to contribute to sexual victimization in sub-Saharan Africa. In Botswana, food insufficiency was associated with >2-times-higher odds of sexual violence among women (89). In qualitative studies from Uganda, Botswana, and Swaziland, women said that they were compelled to remain in abusive relationships as a result of food insecurity and poverty (87, 88). A recent longitudinal study from British Columbia found that severe food insecurity was strongly correlated with unprotected sex among HIV-infected injection drug users (90).
For men and women in resource-poor settings, another possible mechanism through which food insecurity may lead to increased sexual risk taking is that lack of food often leads to migration for work (91, 92). Migration, in turn, has been shown in multiple studies to be associated with increased sexual risk taking and HIV prevalence for both men and women (93–96). In addition to the above mechanisms, food insecurity may contribute to unsafe injection practices among HIV-infected injection drug users if food insecurity interferes with access to clean syringes, needle exchange programs, or health and social support services; more studies are needed to assess this possibility.
PATHWAYS THAT LINK FOOD INSECURITY AND HIV DISEASE PROGRESSION
Food insecurity is associated with a range of negative health outcomes among people infected with HIV/AIDS. Studies from San Francisco and Vancouver have shown strong associations between food insecurity and incomplete viral load suppression and lower CD4 counts (7, 8, 23). In rural Uganda, severe food insecurity has been associated with increased hospitalizations (97), higher odds of self-reported opportunistic infections, and lower physical health composite scores from the validated Medical Outcome Study–HIV Physical Health Summary (22). In a large survival analysis of data from British Columbia, after adherence, CD4 cell counts, and socioeconomic variables were controlled for, food insecurity was associated with an increased hazard of nonaccidental mortality over a median follow-up time of 8.2 y (6). We posit that there are a number of nutritional, mental health, and behavioral pathways through which food insecurity leads to increased HIV morbidity and mortality (Figure 3).
Nutritional pathways
Nationally representative studies of adults in the United States (59–62) and Canada (63) have linked food insecurity to inadequate dietary intakes and serum nutrient levels. Additionally, among PLWHA, cross-sectional studies have identified an association between food insecurity and HIV wasting (64). General undernutrition (protein and energy) and micronutrient deficiencies are both associated with a higher risk of disease progression and mortality in HIV-infected individuals (65, 98–100). Specifically, weight loss, low BMI (in kg/m2), low albumin, and micronutrient deficiencies have been shown to predict opportunistic infections, immunologic decline, and shorter survival time in both untreated and HAART-treated individuals (101–112). HIV increases metabolic requirements (107, 113) and is associated with diarrhea and malabsorption of fat and carbohydrates (113–116), which further compound the links between malnutrition and disease progression. Furthermore, PLWHA are at increased risk of malnutrition because of reduced energy intake from anorexia and early satiety; systemic effects from infections; impaired swallowing from oral and esophageal opportunistic infections; and progressive disability, which leads to unemployment and difficulties in the procurement of food (15, 113, 117). Finally, lack of food may impede optimal absorption of certain antiretroviral medications (118–120), which may, in turn, contribute to treatment failure. Several protease inhibitors, such as nelfinavir and ritonavir, require food for maximal absorption, and the absence of food may negatively affect the pharmacokinetics of these drugs (119, 121).
Among HAART-treated patients in Vancouver, we observed that whereas the effect of food insecurity on mortality was most pronounced among malnourished individuals (adjusted HR = 1.94; 95% CI: 1.10, 3.40), individuals who were malnourished but food secure were not more likely to die, and there was a trend toward increased mortality among individuals who were food insecure but had normal weights (adjusted HR = 1.40; 95% CI: 0.91, 2.05) (6). This suggests that undernutrition is not the only pathway through which food insecurity negatively affects health outcomes.
Food insecurity also exerts negative effects on health through its effects on obesity and poor diet quality (122). In cross-sectional studies of data from the US general population, food insecurity has been associated with hypertension (123), obesity (124), diabetes (122), and self-reported diagnosis of hyperlipidemia (123). Researchers have hypothesized that these associations are driven by substitutions of cheaper, energy-dense foods (125, 126), overconsumption during periods of food availability (127, 128); and compensatory changes in metabolism (129). HIV infection may be an adverse moderator of the relation between food insecurity and worsened metabolic outcomes, because HIV infection itself is known to be associated with a range of metabolic abnormalities, including endothelial dysfunction, atherogenic dyslipidemia, and abnormal glucose metabolism (130–132). Furthermore, treatment with certain antiretroviral medications has been linked to these same metabolic abnormalities (130–132). Thus, it is likely that the effect of food insecurity on metabolic outcomes may be even more pronounced among PLWHA. These abnormalities, together with the fact that the prevalence of obesity among PLWHA is increasing (133), underscores the need to study the relationships between food insecurity and metabolic outcomes so that preventive interventions can be implemented.
Mental health pathways
Food insecurity can also negatively affect health outcomes through mental health pathways, although longitudinal studies will be needed to confirm this. As described above, food insecurity has been strongly associated with depression and poor mental health status (5, 7, 77, 78, 134). Depression and anxiety disorders, in turn, have been shown to predict reduced uptake of, and nonadherence to, HAART (135–142), as well as higher viral loads and higher activated CD8+ cell counts (143). The effects of depression on HIV treatment outcomes are not fully explained via its effects on ART adherence. Even after adjustment for ART adherence, depression has been associated with worsened HIV treatment outcomes, including CD4+ T lymphocyte count decline (144, 145), increased probability of AIDS-defining illness (146), and AIDS-related mortality (145, 147). The role of depression in the acceleration of disease progression is strengthened by the fact that the treatment of depression has been observed to improve ART adherence (148, 149) and viral suppression (149). A number of studies (5, 7, 78) have shown that food insecurity, in addition to its links with depression and worse mental health status, has bidirectional associations with drug and alcohol use and tobacco dependence, which are known to contribute to decreased adherence and worse HIV/AIDS health outcomes (135, 150).
Behavioral pathways
Among low-income adults, food insecurity and other competing subsistence needs (eg, unstable housing) are associated with worsened access and adherence to care (151–154) because competing subsistence priorities such as obtaining food and shelter often interfere with adherence to regular medication use or attendance at outpatient appointments (15, 155–163). Research on adherence to other long-term medication regimens, such as tuberculosis, has also indicated the importance of food security to adherence and treatment outcomes (164, 165).
Both cross-sectional quantitative and qualitative studies have documented strong links between food insecurity and ART adherence among HIV-infected individuals. In cross-sectional studies among urban poor PLWHA in San Francisco, Vancouver, and Atlanta, food insecurity has been associated with ART nonadherence as measured by both unannounced pill counts and pharmacy refill (8, 23, 166, 167). In Atlanta, food insecurity was also associated with common barriers to adherence, such as lack of social support, drug use, and inability to afford medications (23). In a large nationally representative sample of ∼5000 HIV-infected individuals in France, food privation was associated with increased odds of self-reported ART nonadherence among heterosexual men, and a trend toward increased odds of nonadherence among heterosexual women (168). Whereas few quantitative studies to date have documented associations between food insecurity and nonadherence in resource-poor settings (169), qualitative studies in Kenya, Uganda, Botswana, and Swaziland have observed that food insecurity is one of the most commonly cited barriers to ART treatment adherence (15, 87, 160, 170). In addition to food insecurity, poverty and the attendant inability to afford user fees and transport fees are well known to adversely affect ART adherence in resource-limited settings (159, 169). HAART treatment interruptions (171–174) and average HAART adherence (175–177), in turn, are well-known determinants of HIV treatment outcomes.
Other studies have specifically looked at whether food supplementation affects ART adherence. One study in Zambia compared adherence among patients in 4 clinics that provided food supplementation with patients in 4 clinics that did not. They showed that 70% of patients in the food supplementation group achieved ≥95% adherence compared with only 48% in control groups (178). A qualitative study in Kenya also showed greater ART adherence among patients enrolled in a food support program compared with individuals not enrolled (25). Further rigorous studies are needed to explore the mechanisms by which such supplementation may improve adherence and HIV treatment outcomes.
In addition to ART nonadherence and treatment interruptions, as a result of competing demands between food and other resources, it has been shown that food-insecure individuals often miss scheduled clinic visits and may have decreased uptake of HAART (97, 160, 170, 179). In a national survey of low-income adults from the general United States population, food insecurity was associated with postponement of needed medications and care and with increased emergency department use and hospitalizations (151). Another study showed that competing subsistence needs were associated with worse access to health care among HIV-infected individuals (155). In rural Uganda, severe food insecurity was associated with decreased outpatient clinic visits, and many participants had forgone ART (15%), other medications (22%), outpatient care (28%), and inpatient care (28%) to secure food (97). An even greater proportion of study participants reported that they had prioritized medical care; participants had forgone food to obtain ART (83%), access outpatient care (76%), and access inpatient care (44%). This suggests that the relatively high levels of adherence reported among HAART-treated individuals in resource-poor settings (157, 180, 181) may not be sustainable in the long term unless food insecurity and poverty reduction become essential components of comprehensive HIV care programs. Longitudinal studies are needed to confirm the extent to which ART adherence, treatment interruptions, and missed clinic visits are on the causal pathway between food insecurity and worse HIV treatment outcomes in both resource-rich and resource-poor settings.
THE CYCLE OF FOOD INSECURITY AND HIV/AIDS: IMPLICATIONS FOR FUTURE RESEARCH
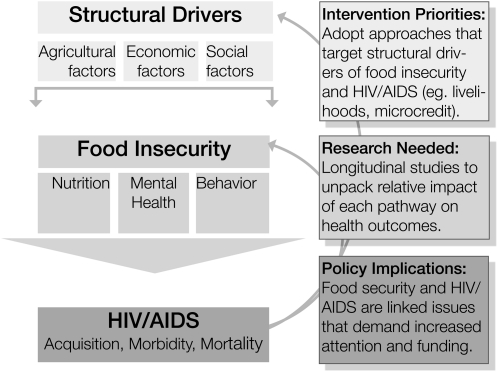
We have suggested that nutritional, mental health, and behavioral pathways explain how food insecurity affects HIV acquisition and HIV/AIDS treatment outcomes. The next step is to understand how these pathways operate across the spectrum of socioeconomic settings and the relative importance of each pathway. Here we identify specific priorities for future research and suggest lessons for both practitioners and policy makers who work in related fields (Figure 4).
FIGURE 4.
Implications for research, policy, and practice.
Whereas there is a rich body of literature in support of the various associations in the conceptual model, no longitudinal studies to date have confirmed these pathways. For example, studies have linked food insecurity to poor nutrition (under- and overnutrition), worse mental health, and nonadherence to treatment and care recommendations; yet no studies to date in either resource-rich or resource-poor settings have specifically assessed the extent to which each of these are on the causal pathway between food insecurity and poor health outcomes. Longitudinal studies based on larger, more representative samples are needed to further assess the relative importance of each mechanism that underlies the relationships between food insecurity and HIV acquisition and HIV health outcomes. We also need to understand whether the mechanisms by which food insecurity adversely affects HIV health outcomes and prevention differ between resource-rich and resource-poor settings. Further clarification of these mechanisms can have important policy and programmatic implications.
In terms of links between food insecurity and HIV acquisition, there are limited data on the effect of food security on sexual risk taking among PLWHA, which highlights an important gap in secondary HIV prevention. There is also a dearth of literature that examines these associations in resource-rich settings and among other populations such as men who have sex with men. We also need to understand more about the mechanisms by which malnutrition may enhance biological susceptibility to HIV among exposed individuals, particularly the role of micronutrient deficiencies. Likewise, research is needed to examine the relation between food insecurity and unsafe injection practices among HIV-infected and uninfected individuals, and whether food insecurity contributes via risky sex and needle sharing to other sexually transmitted infections and hepatitis C. Finally, we need to better understand the mechanisms by which food insecurity may increase the risk of mother-to-child transmission before birth, during labor, and in the first years of life.
There are limited data on the magnitude and extent of the effect of food insecurity on HIV clinical outcomes in resource-poor settings. There are still few data on the role of food insecurity in comorbidities such as hypertension, diabetes, hypercholesterolemia, and cardiovascular complications of HIV in any setting. This research is particularly important in light of the increasing contribution of cardiovascular and metabolic complications of HIV to overall morbidity and mortality among HIV-infected individuals. Finally, food insecurity may also contribute to increased inflammation and T cell activation, mediated by increased gut bacterial translocation (30), but this has not yet been evaluated in studies.
NEED FOR INTERVENTION STUDIES
Policy makers have long acknowledged the potential for food security interventions to positively affect the HIV/AIDS epidemic. For example, according to a 2003 policy statement by the World Food Program, “achieving food security is an important way to decrease transmission of HIV and improve outcomes among those infected” (90). Furthermore, the World Food Program has been working with governments and nongovernmental organizations to ensure that food assistance is incorporated into HIV/AIDS programs where appropriate. The United Nations Standing Committee on Nutrition in 2001 committed to the integration of food security and nutrition considerations into HIV/AIDS programming, to implementation of nutrition care and counseling as part of the essential HIV/AIDS package, and to implementation of optimal approaches to food assistance, processing, and production activities as part of larger HIV/AIDS care programs (182).
Despite these recommendations, little research exists to document the efficacy, effectiveness, or cost effectiveness of food-security interventions on HIV clinical outcomes or HIV acquisition risk in either resource-rich or resource-poor settings. A recent Cochrane review identified no randomized controlled trials conducted in developing countries that examined the effects of either macronutrient supplementation or sustainable food production strategies on HIV morbidity and mortality (183). Such research is critical if we are to provide empiric evidence to guide policies to integrate structural interventions into the expansion of HIV care, treatment, and prevention programs.
Existing intervention approaches to improve HIV treatment outcomes via food security are limited in their scalability and sustainability (184). A few small nonrandomized studies have shown the potential for macronutrient supplementation to affect health outcomes among PLWHA (25, 28, 178, 185–187). Yet macronutrient supplementation, although it provides critical nutritional support, does not address all of the downstream health consequences of food insecurity, and also causes dependency on health programs for receipt of food aid (25). Moreover, reliance on health programs for food may be socially unacceptable or may contribute to ongoing anxiety and uncertainty about food supply and feelings of deprivation and alienation. Finally, the provision of clinic-based food supplementation is costly, and may be difficult to scale up in a variety of settings (188).
Livelihood interventions, which address upstream causes of food insecurity, may have a better chance of improving health outcomes and decreasing HIV transmission by addressing the numerous pathways (nutritional, mental health, and behavioral) through which food insecurity negatively affects health. As an example of this approach, a small study in rural Kenya showed that an intervention that used a microirrigation water pump combined with a microfinance loan led to increases in crop yields, household income, BMI, and CD4 counts (189). More research is needed on structural interventions to address the root causes of poverty and food insecurity, to improve HIV health outcomes, and decrease HIV transmission risk (26, 49, 90, 182).
The development of comprehensive food security interventions that are well integrated with HIV programs will require multidisciplinary partnerships among health, agricultural, and economic experts. For example, because studies have shown that microcredit programs can improve health and prevent disease acquisition by helping address poverty and sex inequality (190–192), experts have recommended an integration of microfinance and other livelihood approaches to maximize health and to reduce HIV transmission and poverty (193, 194). Creative solutions will be required to best meet the food needs of impoverished populations in different parts of the world to prevent HIV transmission and to improve the health and well-being of those who live with HIV/AIDS.
Acknowledgments
We thank Jennifer Mattson for her invaluable contributions to this work.
The authors’ responsibilities were as follows: SDW, SLY, CRC, MBK, ACT, PCT, AMH, EAF, and DRB: conceptualization of the theoretic framework presented in this article; SDW: writing of the first draft of the manuscript and taking the lead on all subsequent drafts of the manuscript. SLY: literature review; SLY: drafting of the manuscript; SLY, CRC, MBK, ACT, PCT, AMH, EAF, and DRB: critical review and editing of all manuscript drafts. AMH: design of the graphics for the theoretic framework. EAF and DRB: advice on all aspects of the prior work contributing to this article. No conflicts of interest were reported.
Footnotes
Abbreviations used: ART, antiretroviral therapy; HAART, highly active antiretroviral therapy; PLWHA, people living with HIV or AIDS.
REFERENCES
- 1.Radimer KL, Olson CM, Greene JC, Campbell CC, Habicht JP. Understanding hunger and developing indicators to assess it in women and children. J Nutr Educ 1992;24(suppl 1):36S–45S [Google Scholar]
- 2.Barrett CB. Measuring food insecurity. Science 2010;327:825–8 [DOI] [PubMed] [Google Scholar]
- 3.Mbugua S, Andersen N, Tuitoek P, Yeudall F, Sellen D, Karanja N, Cole D, Njenga M, Prain G. Assessment of food security and nutrition status among households affected by HIV/AIDS in Nakuru Municipality, Kenya. XVII International AIDS Conference; Mexico City, Mexico, 2008 [Google Scholar]
- 4.Weiser SD, Tsai AC, Senkungu J, Emenyonu N, Kawuma A, Hunt P, Geng E, Martin J, Bangsberg DR. Food insecurity and morbidity among HIV-Infected persons accessing antiretroviral therapy (ART) in rural Uganda. XVIII International AIDS Conference; Vienna, Austria, 2010 [Google Scholar]
- 5.Normén L, Chan K, Braitstein P, Anema A, Bondy G, Montaner JS, Hogg RS. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J Nutr 2005;135:820–5 [DOI] [PubMed] [Google Scholar]
- 6.Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, Montaner JS, Hogg RS. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr 2009;52:342–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiser SD, Bangsberg DR, Kegeles S, Ragland K, Kushel MB, Frongillo EA. Food insecurity among homeless and marginally housed individuals living with HIV/AIDS in San Francisco. AIDS Behav 2009;13:841–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med 2009;24:14–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UNAIDS Report on the global AIDS epidemic. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS, 2008 [Google Scholar]
- 10.Farmer P, Lindenbaum S, Good M. Women, poverty and AIDS: an introduction. Cult Med Psychiatry 1993;17:387–97 [DOI] [PubMed] [Google Scholar]
- 11.Fuwa N. The poverty and heterogeneity among female-headed households revisited: the case of Panama. World Development 2000;28:1515–42 [Google Scholar]
- 12.Anema A, Vogenthaler N, Frongillo EA, Kadiyala S, Weiser SD. Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Curr HIV/AIDS Rep 2009;6:224–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiser SD, Leiter K, Bangsberg DR, Butler LM, Percy-de Korte F, Hlanze Z, Phaladze N, Iacopino V, Heisler M. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med 2007;4:1589–97, discussion 1598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gillespie S, Kadiyala S. HIV/AIDS and food and nutrition security: from evidence to action. Washington, DC: International Food Policy Reseach Institute, 2005 [Google Scholar]
- 15.Marston B, De Cock KM. Multivitamins, nutrition, and antiretroviral therapy for HIV disease in Africa. N Engl J Med 2004;351:78–80 [DOI] [PubMed] [Google Scholar]
- 16.de Waal A, Whiteside A. New variant famine: AIDS and food crisis in southern Africa. Lancet 2003;362:1234–7 [DOI] [PubMed] [Google Scholar]
- 17.The National Agricultural Advisory Services The impact of HIV/AIDS on the agricultural sector and rural livelihoods in Uganda. Rome, Italy: Integrated Support to Sustainable Development and Food Security Program, FAO, 2003 [Google Scholar]
- 18.Kerr RB, Berti PR, Chirwa M. Breastfeeding and mixed feeding practices in Malawi: timing, reasons, decision makers, and child health consequences. Food Nutr Bull 2007;28:90–9 [DOI] [PubMed] [Google Scholar]
- 19.Mehta S, Manji KP, Young AM, Brown ER, Chasela C, Taha TE, Read JS, Goldenberg RL, Fawzi WW. Nutritional indicators of adverse pregnancy outcomes and mother-to-child transmission of HIV among HIV-infected women. Am J Clin Nutr 2008;87:1639–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gillespie S, Kadiyala S. 2005. September, 23 HIV/AIDS and food and nutrition security: from evidence to action. International Food Policy Research Institute; Available from: http://www.ifpri.org/pubs/fpreview/pv07/pv07.pdf (cited 23 September 2008) [Google Scholar]
- 21.Weiser SD, Fernandes K, Anema A, Brandson E, Lima VD, Montaner J, Hogg RS. Food insecurity as a barrier to antiretroviral therapy (ART) adherence among HIV-infected individuals. 5th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention; Cape Town, South Africa, 2009 [Google Scholar]
- 22.Weiser S, Tsai A, Senkungu J, Emenyonu N, Kawuma A, Hunt P, Geng E, Hunt P, Martin J, Bangsberg D. Food insecurity and morbidity among HIV-infected persons accessing antiretroviral therapy (ART) in rural Uganda. XVIII International AIDS Conference; Vienna, Austria, 2010 [Google Scholar]
- 23.Kalichman SC, Cherry C, Amaral C, White D, Kalichman MO, Pope H, Swetsze C, Jones M, Macy R. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health 2010;87:631–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalichman SC, Cherry C, Amaral CM, Swetzes C, Eaton L, Macy R, Grebler T, Kalichman MO. Adherence to antiretroviral therapy and HIV transmission risks: implications for test-and-treat approaches to HIV prevention. AIDS Patient Care STDS 2010;24:271–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Byron E, Gillespie S, Nangami M. Integrating nutrition security with treatment of people living with HIV: lessons from Kenya. Food Nutr Bull 2008;29:87–97 [DOI] [PubMed] [Google Scholar]
- 26.The World Bank Washington, DC: The World Bank, 2007 [Google Scholar]
- 27.United Nations World Food Programme HIV, food security, and nutrition. Policy Brief; 2008. Available from: http://one.wfp.org/food_aid/doc/JC1515-Policy_Brief_Expanded.pdf (cited 13 October 2011) [Google Scholar]
- 28.Mamlin J, Kimaiyo S, Lewis S, Tadayo H, Jerop FK, Gichunge C, Petersen T, Yih Y, Braitstein P, Einterz R. Integrating nutrition support for food-insecure patients and their dependents into an HIV care and treatment program in Western Kenya. Am J Public Health 2009;99:215–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.UNICEF The state of the world's children 2009: maternal and newborn health. New York, NY: United Nations Children's Fund, 2008 [Google Scholar]
- 30.Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol 1997;26:224–7 [DOI] [PubMed] [Google Scholar]
- 31.Barnett T, Whiteside A. AIDS in the twenty-first century: disease and globalization. New York, NY: Palgrave Macmillan, 2006 [Google Scholar]
- 32.Hawkes C, Ruel M. The links between agriculture and health: an intersectoral opportunity to improve the health and livelihoods of the poor. Bull World Health Organ 2006;84:984–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lemke S. Nutrition security, livelihoods and HIV/AIDS: implications for research among farm worker households in South Africa. Public Health Nutr 2005;8:844–52 [DOI] [PubMed] [Google Scholar]
- 34.Seager J, Ganyaza-Twalo T, Tamasane T. Development of a conceptual framework to help understand the interactions between poverty and HIV/AIDS at the household level. Cape Town, South Africa: Human Sciences Research Council, 2007 [Google Scholar]
- 35.USDA Economic Research Service Food security in the United States: measuring household food security. Available from: http://www.ers.usda.gov/Briefing/FoodSecurity/measurement.htm (cited 6 October 2010)
- 36.Negin J. Assessing the impact of HIV/AIDS on economic growth and rural agriculture in Africa. J Int Aff 2005;58:267–81 [Google Scholar]
- 37.Parker DC, Jacobsen KH, Komwa MK. A qualitative study of the impact of HIV/AIDS on agricultural households in southeastern Uganda. Int J Environ Res Public Health 2009;6:2113–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baylies C. The impact of AIDS on rural households in Africa: a shock like any other? Dev Change 2002;33:611–32 [Google Scholar]
- 39.Rugalema G. Coping or struggling? A journey into the impact of HIV/AIDS in southern Africa. Rev Afr Polit Econ 2000;27:537–45 [Google Scholar]
- 40.Nabyonga-Orem J, Bazeyo W, Okema A, Karamagi H, Walker O. Effect of HIV/AIDS on household welfare in Uganda rural communities: a review. East Afr Med J 2008;85:187–96 [DOI] [PubMed] [Google Scholar]
- 41.Gregson S, Mushati P, Nyamukapa C. Adult mortality and erosion of household viability in AIDS-afflicted towns, estates, and villages in eastern Zimbabwe. J Acquir Immune Defic Syndr 2007;44:188–95 [DOI] [PubMed] [Google Scholar]
- 42.Brown LR, Webb P, Haddad L. The role of labour in household food security: implications of AIDS in Africa. Food Policy 1994;19:568–73 [Google Scholar]
- 43.Kaler A, Alibhai A, Kipp W, Rubaale T, Konde-Lule J. Living by the hoe in the age of treatment: perceptions of household well-being after antiretroviral treatment among family members of persons with AIDS. AIDS Care 2010;22(4):509–19 [DOI] [PubMed] [Google Scholar]
- 44.Chapoto A, Jayne TS. Impact of AIDS-related mortality on farm household welfare in Zambia. Econ Dev Cult Change 2008;56:327–74 [Google Scholar]
- 45.Beegle K, de Weerdt J, Dercon S. Adult mortality and consumption growth in the age of HIV/AIDS. Econ Dev Cult Change 2008;56:299–326 [Google Scholar]
- 46.Donovan C, Massingue J. Illness, death, and macronutrients: adequacy of rural Mozambican household production of macronutrients in the face of HIV/AIDS. Food Nutr Bull 2007;28(suppl):S331–8 [DOI] [PubMed] [Google Scholar]
- 47.Yamano T, Jayne TS. Measuring the impact of working-age adult mortality on small-scale farm households in Kenya. World Dev 2004;32:91–119 [Google Scholar]
- 48.Stangl AL, Wamai N, Mermin J, Awor AC, Bunnell RE. Trends and predictors of quality of life among HIV-infected adults taking highly active antiretroviral therapy in rural Uganda. AIDS Care 2007;19:626–36 [DOI] [PubMed] [Google Scholar]
- 49.Samuels FA, Rutenberg N. “Health regains but livelihoods lag”: findings from a study with people on ART in Zambia and Kenya. AIDS Care 2011;23:748–54 [DOI] [PubMed] [Google Scholar]
- 50.Yamano T, Jayne TS. Working-age adult mortality and primary school attendance in rural Kenya. Econ Dev Cult Change 2005;53:619–54 [Google Scholar]
- 51.Evans DK, Miguel E. Orphans and schooling in Africa: a longitudinal analysis. Demography 2007;44:35–57 [DOI] [PubMed] [Google Scholar]
- 52.Fafchamps M, Lund S. Risk-sharing networks in rural Philippines. J Dev Econ 2003;71:261–87 [Google Scholar]
- 53.de Weerdt J, Dercon S. Risk-sharing networks and insurance against illness. J Dev Econ 2006;81:337–56 [Google Scholar]
- 54.Fafchamps M. Solidarity networks in preindustrial societies: rational peasants with a moral economy. Econ Dev Cult Change 1992;41:147–74 [Google Scholar]
- 55.la Ferrara E. Kin groups and reciprocity: a model of credit transactions in Ghana. Am Econ Rev 2003;93:1730–51 [Google Scholar]
- 56.Danziger R. The social impact of HIV/AIDS in developing countries. Soc Sci Med 1994;39:905–17 [DOI] [PubMed] [Google Scholar]
- 57.Tsai AC, Bangsberg DR, Emenyonu N, Senkungu JK, Martin JN, Weiser SD. The social context of food insecurity among people living with HIV/AIDS in rural Uganda. Soc Sci Med (Epub ahead of print 10 October 2011). Available from: http://dx.doi.org/10.1016/j.socscimed.2011.09.026 [DOI] [PMC free article] [PubMed]
- 58.Oyefara JL. Poverty, food insecurity, and HIV/AIDS pandemic: evidence of relationship from reproductive behaviour of commercial sex workers in Lagos metropolis, Nigeria. International Conference on HIV/AIDS, Food and Nutrition Security; Durban, South Africa, 2005 [Google Scholar]
- 59.Rose D, Oliveira V. Nutrient intakes of individuals from food-insufficient households in the United States. Am J Public Health 1997;87:1956–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rose D. Economic determinants and dietary consequences of food insecurity in the United States. J Nutr 1999;129(2S suppl):S517–20 [DOI] [PubMed] [Google Scholar]
- 61.Lee JS, Frongillo EA., Jr Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. J Nutr 2001;131:1503–9 [DOI] [PubMed] [Google Scholar]
- 62.Dixon LB, Winkleby MA, Radimer KL. Dietary intakes and serum nutrients differ between adults from food-insufficient and food-sufficient families: Third National Health and Nutrition Examination Survey, 1988-1994. J Nutr 2001;131:1232–46 [DOI] [PubMed] [Google Scholar]
- 63.Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. J Nutr 2008;138:604–12 [DOI] [PubMed] [Google Scholar]
- 64.Campa A, Yang Z, Lai S, Xue L, Phillips JC, Sales S, Page JB, Baum MK. HIV-related wasting in HIV-infected drug users in the era of highly active antiretroviral therapy. Clin Infect Dis 2005;41:1179–85 [DOI] [PubMed] [Google Scholar]
- 65.Friis H. Micronutrients and HIV infection: a review of current evidence. Geneva, Switzerland: World Health Organization, 2005 [Google Scholar]
- 66.Schreck R, Rieber P, Baeuerle PA. Reactive oxygen intermediates as apparently widely used messengers in the activation of the NF-kappa B transcription factor and HIV-1. EMBO J 1991;10:2247–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Royce RA, Sena A, Cates W, Jr, Cohen MS. Sexual transmission of HIV. N Engl J Med 1997;336:1072–8 [DOI] [PubMed] [Google Scholar]
- 68.Iliff PJ, Piwoz EG, Tavengwa NV, Zunguza CD, Marinda ET, Nathoo KJ, Moulton LH, Ward BJ, Humphrey JH. Early exclusive breastfeeding reduces the risk of postnatal HIV-1 transmission and increases HIV-free survival. AIDS 2005;19:699–708 [DOI] [PubMed] [Google Scholar]
- 69.Coates J, Frongillo EA, Rogers BL, Webb P, Wilde PE, Houser R. Commonalities in the experience of household food insecurity across cultures: what are measures missing? J Nutr 2006;136:1438S–48S [DOI] [PubMed] [Google Scholar]
- 70.Hamelin AM, Beaudry M, Habicht JP. Characterization of household food insecurity in Quebec: food and feelings. Soc Sci Med 2002;54:119–32 [DOI] [PubMed] [Google Scholar]
- 71.Connell CL, Lofton KL, Yadrick K, Rehner TA. Children's experiences of food insecurity can assist in understanding its effect on their well-being. J Nutr 2005;135:1683–90 [DOI] [PubMed] [Google Scholar]
- 72.Piaseu N, Belza B, Shell-Duncan B. Less money less food: voices from women in urban poor families in Thailand. Health Care Women Int 2004;25:604–19 [DOI] [PubMed] [Google Scholar]
- 73.Weaver LJ, Hadley C. Moving beyond hunger and nutrition: a systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol Food Nutr 2009;48:263–84 [DOI] [PubMed] [Google Scholar]
- 74.Maes KC, Hadley C, Tesfaye F, Shifferaw S. Food insecurity and mental health: surprising trends among community health volunteers in Addis Ababa, Ethiopia during the 2008 food crisis. Soc Sci Med 2010;70:1450–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim K, Frongillo EA. Participation in food assistance programs modifies the relation of food insecurity with weight and depression in elders. J Nutr 2007;137:1005–10 [DOI] [PubMed] [Google Scholar]
- 76.Heflin CM, Siefert K, Williams DR. Food insufficiency and women's mental health: findings from a 3-year panel of welfare recipients. Soc Sci Med 2005;61:1971–82 [DOI] [PubMed] [Google Scholar]
- 77.Vogenthaler NS, Hadley C, Rodriguez AE, Valverde EE, Del Rio C, Metsch LR. Depressive symptoms and food insufficiency among HIV-infected crack users in Atlanta and Miami. AIDS Behav 2011;15:1520–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Anema A, Wood E, Weiser SD, Qi J, Montaner JS, Kerr T. Hunger and associated harms among injection drug users in an urban Canadian setting. Subst Abuse Treat Prev Policy 2010;5:20–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tsai A, Bangsberg D, Frongillo E, Senkungu J, Emenyonu N, Kawuma A, Hunt P, Martin W, Weiser S. Gendered effects of food insecurity on depression among HIV-infected persons accessing antiretroviral therapy (ART) in rural Uganda. 17th Conference on Retroviruses and Opportunistic Infections; San Francisco, CA, 2010 [Google Scholar]
- 80.Grassi L. Risk of HIV infection in psychiatrically ill patients. AIDS Care 1996;8:103–16 [DOI] [PubMed] [Google Scholar]
- 81.Carey MP, Carey KB, Kalichman SC. Risk for human immunodeficiency virus (HIV) infection among persons with severe mental illnesses. Clin Psychol Rev 1997;17:271–91 [DOI] [PubMed] [Google Scholar]
- 82.Sullivan G, Koegel P, Kanouse DE, Cournos F, McKinnon K, Young AS, Bean D. HIV and people with serious mental illness: the public sector's role in reducing HIV risk and improving care. Psychiatr Serv 1999;50:648–52 [DOI] [PubMed] [Google Scholar]
- 83.Weiser SD, Wolfe WR, Bangsberg DR. The HIV epidemic among individuals with mental illness in the United States. Curr HIV/AIDS Rep 2004;1:186–92 [DOI] [PubMed] [Google Scholar]
- 84.Dupas P, Robinson J. Coping with political instability: micro evidence from Kenya's 2007 election crisis. Am Econ Rev 2010;100(2):120–4 [Google Scholar]
- 85.Robinson J, Yeh E. Transactional sex as a response to risk in western Kenya. Am Econ Rev 2011;3(1):35–64 [Google Scholar]
- 86.Oyefara JL. Food insecurity, HIV/AIDS pandemic and sexual behaviour of female commercial sex workers in Lagos metropolis, Nigeria. SAHARA J 2007;4:626–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Physicians for Human Rights Epidemic of inequality: women's rights and HIV/AIDS in Botswana & Swaziland: an evidence-based report on the effects of gender inequity, stigma and discrimination. Cambridge, MA: Physicians for Human Rights, 2007 [Google Scholar]
- 88.Miller CL, Bangsberg DR, Tuller DM, Senkungu J, Kawuma A, Frongillo EA, Weiser SD. Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS Behav 2011;15:1512–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tsai AC, Leiter K, Wolfe WR, Heisler M, Shannon K, Phaladze NA, Hlanze Z, Iacopino V, Weiser SD. Prevalence and correlates of sexual violence perpetration and victimization among men and women in Botswana and Swaziland. Am J Public Health 2011;101:1068–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shannon K, Kerr T, Milloy MJ, Anema A, Zhang R, Montaner JS, Wood E. Severe food insecurity is associated with elevated unprotected sex among HIV-seropositive injection drug users independent of HAART use. AIDS 2011;25:2037–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Programming in the Era of AIDS WPF's Response to HIV/AIDS. Rome, Italy: World Food Programme, 2003. February 5-7. 1-23 p [Google Scholar]
- 92.Singh S. Food crisis and AIDS: the Indian perspective. Lancet 2003;362:1938–9 [DOI] [PubMed] [Google Scholar]
- 93.Boerma JT, Gregson S, Nyamukapa C, Urassa M. Understanding the uneven spread of HIV within Africa: comparative study of biologic, behavioral, and contextual factors in rural populations in Tanzania and Zimbabwe. Sex Transm Dis 2003;30:779–87 [DOI] [PubMed] [Google Scholar]
- 94.Lagarde E, Schim van der Loeff M, Enel C, Holmgren B, Dray-Spira R, Pison G, Piau JP, Delaunay V, M'Boup S, Ndoye I, et al. Mobility and the spread of human immunodeficiency virus into rural areas of West Africa. Int J Epidemiol 2003;32:744–52 [DOI] [PubMed] [Google Scholar]
- 95.Lurie MN, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett G, Sturm AW, Sweat MD, Gittelsohn J, Abdool Karim SS. The impact of migration on HIV-1 transmission in South Africa: a study of migrant and nonmigrant men and their partners. Sex Transm Dis 2003;30:149–56 [DOI] [PubMed] [Google Scholar]
- 96.Zuma K, Gouws E, Williams B, Lurie M. Risk factors for HIV infection among women in Carletonville, South Africa: migration, demography and sexually transmitted diseases. Int J STD AIDS 2003;14:814–7 [DOI] [PubMed] [Google Scholar]
- 97.Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkugu J, Hunt PW, Emenyonu NI, Mattson JE, Martin JN, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in rural Uganda. AIDS (Epub ahead of print 6 September 2011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Drain PK, Kupka R, Mugusi F, Fawzi WW. Micronutrients in HIV-positive persons receiving highly active antiretroviral therapy. Am J Clin Nutr 2007;85:333–45 [DOI] [PubMed] [Google Scholar]
- 99.Zachariah R, Fitzgerald M, Massaquoi M, Pasulani O, Arnould L, Makombe S, Harries AD. Risk factors for high early mortality in patients on antiretroviral treatment in a rural district of Malawi. AIDS 2006;20:2355–60 [DOI] [PubMed] [Google Scholar]
- 100.Johannessen A, Naman E, Ngowi BJ, Sandvik L, Matee MI, Aglen HE, Gundersen SG, Bruun JN. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect Dis 2008;8:52–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kotler DP, Tierney AR, Wang J, Pierson RN., Jr Magnitude of body-cell-mass depletion and the timing of death from wasting in AIDS. Am J Clin Nutr 1989;50:444–7 [DOI] [PubMed] [Google Scholar]
- 102.van der Sande MA, van der Loeff MF, Aveika AA, Sabally S, Togun T, Sarge-Njie R, Alabi AS, Jaye A, Corrah T, Whittle HC. Body mass index at time of HIV diagnosis: a strong and independent predictor of survival. J Acquir Immune Defic Syndr 2004;37:1288–94 [DOI] [PubMed] [Google Scholar]
- 103.Wheeler DA, Gibert CL, Launer CA, Muurahainen N, Elion RA, Abrams DI, Bartsch GE. Weight loss as a predictor of survival and disease progression in HIV infection. Terry Beirn Community Programs for Clinical Research on AIDS. J Acquir Immune Defic Syndr Hum Retrovirol 1998;18:80–5 [DOI] [PubMed] [Google Scholar]
- 104.Guenter P, Muurahainen N, Simons G, Kosok A, Cohan GR, Rudenstein R, Turner JL. Relationships among nutritional status, disease progression, and survival in HIV infection. J Acquir Immune Defic Syndr 1993;6:1130–8 [PubMed] [Google Scholar]
- 105.Chlebowski RT, Grosvenor MB, Bernhard NH, Morales LS, Bulcavage LM. Nutritional status, gastrointestinal dysfunction, and survival in patients with AIDS. Am J Gastroenterol 1989;84:1288–93 [PubMed] [Google Scholar]
- 106.Chlebowski RT, Grosvenor M, Lillington L, Sayre J, Beall G. Dietary intake and counseling, weight maintenance, and the course of HIV infection. J Am Diet Assoc 1995;95:428–32, quiz 433–5 [DOI] [PubMed] [Google Scholar]
- 107.Macallan DC, Noble C, Baldwin C, Jebb SA, Prentice AM, Coward WA, Sawyer MB, McManus TJ, Griffin GE. Energy expenditure and wasting in human immunodeficiency virus infection. N Engl J Med 1995;333:83–8 [DOI] [PubMed] [Google Scholar]
- 108.Jones CY, Hogan JW, Snyder B, Klein RS, Rompalo A, Schuman P, Carpenter CC. Overweight and human immunodeficiency virus (HIV) progression in women: associations HIV disease progression and changes in body mass index in women in the HIV epidemiology research study cohort. Clin Infect Dis 2003;37(suppl 2):S69–80 [DOI] [PubMed] [Google Scholar]
- 109.Tang AM, Forrester J, Spiegelman D, Knox TA, Tchetgen E, Gorbach SL. Weight loss and survival in HIV-positive patients in the era of highly active antiretroviral therapy. J Acquir Immune Defic Syndr 2002;31:230–6 [DOI] [PubMed] [Google Scholar]
- 110.Coutsoudis A, Bobat RA, Coovadia HM, Kuhn L, Tsai WY, Stein ZA. The effects of vitamin A supplementation on the morbidity of children born to HIV-infected women. Am J Public Health 1995;85:1076–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Baum MK, Shor-Posner G, Lu Y, Rosner B, Sauberlich HE, Fletcher MA, Szapocznik J, Eisdorfer C, Buring JE, Hennekens CH. Micronutrients and HIV-1 disease progression. AIDS 1995;9:1051–6 [DOI] [PubMed] [Google Scholar]
- 112.Allard JP, Aghdassi E, Chau J, Tam C, Kovacs CM, Salit IE, Walmsley SL. Effects of vitamin E and C supplementation on oxidative stress and viral load in HIV-infected subjects. AIDS 1998;12:1653–9 [DOI] [PubMed] [Google Scholar]
- 113.Babameto G, Kotler DP. Malnutrition in HIV infection. Gastroenterol Clin North Am 1997;26:393–415 [DOI] [PubMed] [Google Scholar]
- 114.Kotler DP, Tierney AR, Brenner SK, Couture S, Wang J, Pierson RN., Jr Preservation of short-term energy balance in clinically stable patients with AIDS. Am J Clin Nutr 1990;51:7–13 [DOI] [PubMed] [Google Scholar]
- 115.Stack JA, Bell SJ, Burke PA, Forse RA. High-energy, high-protein, oral, liquid, nutrition supplementation in patients with HIV infection: effect on weight status in relation to incidence of secondary infection. J Am Diet Assoc 1996;96:337–41 [DOI] [PubMed] [Google Scholar]
- 116.Fields-Gardner C, Fergusson P. Position of the American Dietetic Association and Dietitians of Canada: nutrition intervention in the care of persons with human immunodeficiency virus infection. J Am Diet Assoc 2004;104:1425–41 [DOI] [PubMed] [Google Scholar]
- 117.Macallan DC, Noble C, Baldwin C, Foskett M, McManus T, Griffin GE. Prospective analysis of patterns of weight change in stage IV human immunodeficiency virus infection. Am J Clin Nutr 1993;58:417–24 [DOI] [PubMed] [Google Scholar]
- 118.Gustavson L, Lam W, Bertz R, Hsu A, Rynkiewicz K, Ji Q, Ghosh S, Facey I, Bernstein B, Sun E. Assessment of the bioequivalence and food effects for liquid and soft gelatin capsule co-formulations of ABT-378/ritonavir (ABT-378/r) in healthy subjects. 2000; Toronto, Canada [Google Scholar]
- 119.Bardsley-Elliot A, Plosker GL. Nelfinavir: an update on its use in HIV infection. Drugs 2000;59:581–620 [DOI] [PubMed] [Google Scholar]
- 120.Colin A, Reggers J, Castronovo V, Ansseau M. [Lipids, depression and suicide.] Encephale 2003;29:49–58 (in French). [PubMed] [Google Scholar]
- 121.November 14. Abbot Laboratories Kaletra, US package insert. Available from: http://www.fda.gov/cder/foi/label/2005/021226s016lbl.pdf (cited 10 2007 November)
- 122.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med 2007;22:1018–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 2010;140:304–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc 2007;107:1952–61 [DOI] [PubMed] [Google Scholar]
- 125.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6–16 [DOI] [PubMed] [Google Scholar]
- 126.Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82(suppl):265S–73S [DOI] [PubMed] [Google Scholar]
- 127.Wilde PE, Ranney CK. The monthly food stamp cycle: shopping frequency and food intake decisions in an endogenous switching regression framework. Am J Agric Econ 2000;82:200–13 [Google Scholar]
- 128.Polivy J, Zeitlin SB, Herman CP, Beal AL. Food restriction and binge eating: a study of former prisoners of war. J Abnorm Psychol 1994;103:409–11 [DOI] [PubMed] [Google Scholar]
- 129.Weight cycling National Task Force on the Prevention and Treatment of Obesity. JAMA 1994;272:1196–202 [PubMed] [Google Scholar]
- 130.Grinspoon S, Carr A. Cardiovascular risk and body-fat abnormalities in HIV-infected adults. N Engl J Med 2005;352:48–62 [DOI] [PubMed] [Google Scholar]
- 131.Ho JE, Hsue PY. Cardiovascular manifestations of HIV infection. Heart 2009;95:1193–202 [DOI] [PubMed] [Google Scholar]
- 132.Fichtenbaum CJ. Does antiretroviral therapy increase or decrease the risk of cardiovascular disease? Curr HIV/AIDS Rep 2010;7:92–8 [DOI] [PubMed] [Google Scholar]
- 133.Crum-Cianflone N, Roediger MP, Eberly L, Headd M, Marconi V, Ganesan A, Weintrob A, Barthel RV, Fraser S, Agan BK. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PLoS ONE 2010;5:e10106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Vogenthaler NS, Hadley C, Lewis SJ, Rodriguez AE, Metsch LR, del Rio C. Food insufficiency among HIV-infected crack-cocaine users in Atlanta and Miami. Public Health Nutr 2010;13:1478–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tucker JS, Burnam MA, Sherbourne CD, Kung FY, Gifford AL. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. Am J Med 2003;114:573–80 [DOI] [PubMed] [Google Scholar]
- 136.Ammassari A, Antinori A, Aloisi MS, Trotta MP, Murri R, Bartoli L, Monforte AD, Wu AW, Starace F. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics 2004;45:394–402 [DOI] [PubMed] [Google Scholar]
- 137.Fairfield KM, Libman H, Davis RB, Eisenberg DM. Delays in protease inhibitor use in clinical practice. J Gen Intern Med 1999;14:395–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Tegger MK, Crane HM, Tapia KA, Uldall KK, Holte SE, Kitahata MM. The effect of mental illness, substance use, and treatment for depression on the initiation of highly active antiretroviral therapy among HIV-infected individuals. AIDS Patient Care STDS 2008;22:233–43 [DOI] [PubMed] [Google Scholar]
- 139.Chesney M. Adherence to HAART regimens. AIDS Patient Care STDS 2003;17:169–77 [DOI] [PubMed] [Google Scholar]
- 140.Horberg MA, Silverberg MJ, Hurley LB, Towner WJ, Klein DB, Bersoff-Matcha S, Weinberg WG, Antoniskis D, Mogyoros M, Dodge WT, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr 2008;47:384–90 [DOI] [PubMed] [Google Scholar]
- 141.Kacanek D, Jacobson DL, Spiegelman D, Wanke C, Isaac R, Wilson IB. Incident depression symptoms are associated with poorer HAART adherence: a longitudinal analysis from the Nutrition for Healthy Living Study. J Acquir Immune Defic Syndr 2010;53:266–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Singh N, Squier C, Sivek C, Wagener M, Nguyen MH, Yu VL. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: prospective assessment with implications for enhancing compliance. AIDS Care 1996;8:261–9 [DOI] [PubMed] [Google Scholar]
- 143.Evans DL, Ten Have TR, Douglas SD, Gettes DR, Morrison M, Chiappini MS, Brinker-Spence P, Job C, Mercer DE, Wang YL, et al. Association of depression with viral load, CD8 T lymphocytes, and natural killer cells in women with HIV infection. Am J Psychiatry 2002;159:1752–9 [DOI] [PubMed] [Google Scholar]
- 144.Ironson G, O'Cleirigh C, Fletcher MA, Laurenceau JP, Balbin E, Klimas N, Schneiderman N, Solomon G. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med 2005;67:1013–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, Moore J. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA 2001;285:1466–74 [DOI] [PubMed] [Google Scholar]
- 146.Anastos K, Schneider MF, Gange SJ, Minkoff H, Greenblatt RM, Feldman J, Levine A, Delapenha R, Cohen M. The association of race, sociodemographic, and behavioral characteristics with response to highly active antiretroviral therapy in women. J Acquir Immune Defic Syndr 2005;39:537–44 [PubMed] [Google Scholar]
- 147.Cook JA, Grey D, Burke J, Cohen MH, Gurtman AC, Richardson JL, Wilson TE, Young MA, Hessol NA. Depressive symptoms and AIDS-related mortality among a multisite cohort of HIV-positive women. Am J Public Health 2004;94:1133–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Safren SA, O'Cleirigh C, Tan JY, Raminani SR, Reilly LC, Otto MW, Mayer KH. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol 2009;28:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tsai AC, Weiser SD, Petersen ML, Ragland K, Kushel MB, Bangsberg DR. A marginal structural model to estimate the causal effect of antidepressant medication treatment on viral suppression among homeless and marginally housed persons living with HIV. Arch Gen Psychiatry 2010;67(12):1282–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Shuter J, Bernstein SL. Cigarette smoking is an independent predictor of nonadherence in HIV-infected individuals receiving highly active antiretroviral therapy. Nicotine Tob Res 2008;10:731–6 [DOI] [PubMed] [Google Scholar]
- 151.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med 2006;21:71–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health 1997;87:217–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Schlossstein E, St Clair P, Connell F. Referral keeping in homeless women. J Community Health 1991;16:279–85 [DOI] [PubMed] [Google Scholar]
- 154.Bengle R, Sinnett S, Johnson T, Johnson MA, Brown A, Lee JS. Food insecurity is associated with cost-related medication non-adherence in community-dwelling, low-income older adults in Georgia. J Nutr Elder 2010;29:170–91 [DOI] [PubMed] [Google Scholar]
- 155.Cunningham WE, Andersen RM, Katz MH, Stein MD, Turner BJ, Crystal S, Zierler S, Kuromiya K, Morton SC, St Clair P, et al. The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Med Care 1999;37:1270–81 [DOI] [PubMed] [Google Scholar]
- 156.Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health 2007;97:2238–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Weiser S, Wolfe W, Bangsberg D, Thior I, Gilbert P, Makhema J, Kebaabetswe P, Dickenson D, Mompati K, Essex M, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr 2003;34:281–8 [DOI] [PubMed] [Google Scholar]
- 158.Au JT, Kayitenkore K, Shutes E, Karita E, Peters PJ, Tichacek A, Allen SA. Access to adequate nutrition is a major potential obstacle to antiretroviral adherence among HIV-infected individuals in Rwanda. AIDS 2006;20:2116–8 [DOI] [PubMed] [Google Scholar]
- 159.Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, Kglatwane J, Kinsman J, Kwasa R, Maridadi J, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care 2007;19:658–65 [DOI] [PubMed] [Google Scholar]
- 160.Weiser SD, Tuller DM, Frongillo EA, Senkungu J, Mukiibi N, Bangsberg DR. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS ONE 2010;5:e10340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Olupot-Olupot P, Katawera A, Cooper C, Small W, Anema A, Mills E. Adherence to antiretroviral therapy among a conflict-affected population in Northeastern Uganda: a qualitative study. AIDS 2008;22:1882–4 [DOI] [PubMed] [Google Scholar]
- 162.Nachega JB, Knowlton AR, Deluca A, Schoeman JH, Watkinson L, Efron A, Chaisson RE, Maartens G. Treatment supporter to improve adherence to antiretroviral therapy in HIV-infected South African adults. A qualitative study. J Acquir Immune Defic Syndr 2006;43(suppl 1):S127–33 [DOI] [PubMed] [Google Scholar]
- 163.Kagee A, Remien RH, Berkman A, Hoffman S, Campos L, Swartz L. Structural barriers to ART adherence in Southern Africa: challenges and potential ways forward. Glob Public Health 2011;6:83–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Farmer P, Robin S, Ramilus SL, Kim JY. Tuberculosis, poverty, and “compliance”: lessons from rural Haiti. Semin Respir Infect 1991;6:254–60 [PubMed] [Google Scholar]
- 165.Baldwin MR, Yori PP, Ford C, Moore DA, Gilman RH, Vidal C, Ticona E, Evans CA. Tuberculosis and nutrition: disease perceptions and health seeking behavior of household contacts in the Peruvian Amazon. Int J Tuberc Lung Dis 2004;8:1484–91 [PMC free article] [PubMed] [Google Scholar]
- 166.Weiser S, Fernandes K, Anema A, Brandson E, Lima V, Montaner J, Hogg R. Food insecurity as a barrier to antiretroviral therapy (ART) adherence among HIV-infected individuals in British Columbia. 5th IAS Conference on HIV Pathogenesis, Treatment and Prevention; Cape Town, South Africa, 2009 [Google Scholar]
- 167.Kalichman SC, Pellowski J, Kalichman MO, Cherry C, Detorio M, Caliendo AM, Schinazi RF. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prev Sci 2011;12:324–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Peretti-Watel P, Spire B, Schiltz MA, Bouhnik AD, Heard I, Lert F, Obadia Y. Vulnerability, unsafe sex and non-adherence to HAART: evidence from a large sample of French HIV/AIDS outpatients. Soc Sci Med 2006;62:2420–33 [DOI] [PubMed] [Google Scholar]
- 169.Rachlis BS, Mills EJ, Cole DC. Livelihood security and adherence to antiretroviral therapy in low and middle income settings: a systematic review. PLoS ONE 2011;6:e18948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Tuller DM, Bangsberg DR, Senkungu J, Ware NC, Emenyonu N, Weiser SD. Transportation costs impede sustained adherence and access to HAART in a clinic population in southwestern Uganda: a qualitative study. AIDS Behav 2010;14:778-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ballif M, Ledergerber B, Battegay M, Cavassini M, Bernasconi E, Schmid P, Hirschel B, Furrer H, Rickenbach M, Opravil M, et al. Swiss HIV Cohort Study. Impact of previous virological treatment failures and adherence on the outcome of antiretroviral therapy in 2007. PLoS ONE 2009;4(12):e8275–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Parienti JJ, Massari V, Descamps D, Vabret A, Bouvet E, Larouze B, Verdon R. Predictors of virologic failure and resistance in HIV-infected patients treated with nevirapine- or efavirenz-based antiretroviral therapy. Clin Infect Dis 2004;38:1311–6 [DOI] [PubMed] [Google Scholar]
- 173.Parienti JJ, Das-Douglas M, Massari V, Guzman D, Deeks SG, Verdon R, Bangsberg DR. Not all missed doses are the same: sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherence levels. PLoS ONE 2008;3:e2783–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Oyugi JH, Byakika-Tusiime J, Ragland K, Laeyendecker O, Mugerwa R, Kityo C, Mugyenyi P, Quinn TC, Bangsberg DR. Treatment interruptions predict resistance in HIV-positive individuals purchasing fixed-dose combination antiretroviral therapy in Kampala, Uganda. AIDS 2007;21:965–71 [DOI] [PubMed] [Google Scholar]
- 175.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000;133:21–30 [DOI] [PubMed] [Google Scholar]
- 176.Liu H, Miller LG, Hays RD, Golin CE, Wu T, Wenger NS, Kaplan AH. Repeated measures longitudinal analyses of HIV virologic response as a function of percent adherence, dose timing, genotypic sensitivity, and other factors. J Acquir Immune Defic Syndr 2006;41:315–22 [DOI] [PubMed] [Google Scholar]
- 177.Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, Moss A. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS 2001;15:1181–3 [DOI] [PubMed] [Google Scholar]
- 178.Cantrell RA, Sinkala M, Megazinni K, Lawson-Marriott S, Washington S, Chi BH, Tambatamba-Chapula B, Levy J, Stringer EM, Mulenga L, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr 2008;49:190–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mshana GH, Wamoyi J, Busza J, Zaba B, Changalucha J, Kaluvya S, Urassa M. Barriers to accessing antiretroviral therapy in Kisesa, Tanzania: a qualitative study of early rural referrals to the national program. AIDS Patient Care STDS 2006;20:649–57 [DOI] [PubMed] [Google Scholar]
- 180.Laurent C, Ngom Gueye NF, Ndour CT, Gueye PM, Diouf M, Diakhate N, Toure Kane NC, Laniece I, Ndir A, Vergne L, et al. Long-term benefits of highly active antiretroviral therapy in Senegalese HIV-1-infected adults. J Acquir Immune Defic Syndr 2005;38:14–7 [DOI] [PubMed] [Google Scholar]
- 181.Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, Rachlis B, Wu P, Cooper C, Thabane L, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA 2006;296:679–90 [DOI] [PubMed] [Google Scholar]
- 182.Nutrition and HIV/AIDS Statement by the Administrative Committee on Coordination, Sub-Committee on Nutrition at its 28th Session. Nairobe, Kenya: United Nations Administrative Committee on Coordination, Sub-Committee on Nutrition, 2001 [Google Scholar]
- 183.Mahlungulu S, Grobler LA, Visser ME, Volmink J. Nutritional interventions for reducing morbidity and mortality in people with HIV. Cochrane Database Syst Rev 2007; (3):CD004536. [DOI] [PubMed] [Google Scholar]
- 184.Sztam KA, Fawzi WW, Duggan C. Macronutrient supplementation and food prices in HIV treatment. J Nutr 2010;140:213S–23S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Partners in Health 2009. January 13 Agricultural initiatives for health in Haiti, Rwanda, and Lesotho. Partners in Health. Available from: http://model.pih.org/food/agriculture (cited 13 January 2010)
- 186.Ochai R. HIV, livelihoods, nutrition and health research. Bamako, Mali: Global Ministerial Forum on Research for Health, 2008 [Google Scholar]
- 187.Njenga M, Karanja N, Gathuru K, Mbugua S, Fedha N, Ngoda B. The role of women-led micro-farming activities in combating HIV/AIDS in Nakuru, Kenya. : Hovorka A, de Zeeuw H, Njenga M, Women feeding cities: mainstreaming gender in urban agriculture and food security. Warwickshire, UK: Practical Action Publishing, 2009 [Google Scholar]
- 188.Ivers LC, Cullen KA, Freedberg KA, Block S, Coates J, Webb P. HIV/AIDS, undernutrition, and food insecurity. Clin Infect Dis 2009;49:1096–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Pandit JA, Sirotin N, Tittle R, Onjolo E, Bukusi EA, Cohen CR. Shamba Maisha: a pilot study assessing impacts of a micro-irrigation intervention on the health and economic wellbeing of HIV patients. BMC Public Health 2010;10:245–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ashburn K, Kerrigan D, Sweat M. Micro-credit, women's groups, control of own money: HIV-Related negotiation among partnered Dominican women. AIDS Behav 2008;12:396–403 [DOI] [PubMed] [Google Scholar]
- 191.Kim J, Pronyk P, Barnett T, Watts C. Exploring the role of economic empowerment in HIV prevention. AIDS 2008;22:S57–71 [DOI] [PubMed] [Google Scholar]
- 192.Schuler SR, Hashemi SM. Credit programs, womens empowerment, and contraceptive use in rural Bangladesh. Stud Fam Plann 1994;25:65–76 [PubMed] [Google Scholar]
- 193.Dworkin SL, Blankenship K. Microfinance and HIV/AIDS prevention: assessing its promise and limitations. AIDS Behav 2009;13:462–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Weinhardt LS, Galvao LW, Stevens PE, Masanjala WH, Bryant C, Ng'ombe T. Broadening research on microfinance and related strategies for HIV prevention: commentary on Dworkin and Blankenship (2009). AIDS Behav 2009;13:470–3 [DOI] [PubMed] [Google Scholar]