Abstract
Invasive and noninvasive monitoring facilitates clinical evaluation when resuscitating patients with complex haemodynamic disorders. If the macrocirculation is to be stable, then it must adapt to blood flow or blood flow must be optimized. The objective of flow monitoring is to assist with matching observed oxygen consumption (VO2) to pathophysiological needs. If an adequate balance cannot be maintained then dysoxia occurs. In this review we propose a simple schema for global reasoning; we discuss the limitations of VO2 and arterial oxygen delivery (DaO2) assessment; and we address concerns about increasing DaO2 to supranormal values or targeting pre-established levels of DaO2, cardiac output, or mixed venous oxygen saturation. All of these haemodynamic variables are interrelated and limited by physiological and/or pathological processes. A unique global challenge, and one that is of great prognostic interest, is to achieve rapid matching between observed and needed VO2 – no more and no less. However, measuring or calculating these two variables at the bedside remains difficult. In practice, we propose a distinction between three situations. Clinical and blood lactate clearance improvements can limit investigations in simple cases. Intermediate cases may be managed by continuous monitoring of VO2-related variables such as DaO2, cardiac output, or mixed venous oxygen saturation. In more complex cases, three methods can help to estimate the needed VO2 level: comparison with expected values from past physiological studies; analysis of the relationship between VO2 and oxygen delivery; and use of computer software to integrate the preceding two methods.
Introduction
Major advances have been made in monitoring the critically ill patient following the introduction in the 1970s of intravascular pressure and flow recording catheters [1]. Today, flow monitoring is one of the major reasons to admit patients into an intensive care unit (ICU), but which of the flow-based parameters are really interesting from a clinical perspective?
A reasonable assumption is that below a critical level the oxygen consumption (VO2) is inversely related to the risk for cell dysfunction and necrosis and to the severity of shock. Among the various haemodynamic variables that may be evaluated, a VO2 below the required level is most strongly related to death [2]. Once a substantial amount of cell necrosis has occurred, organ function recovery is not always possible, even when adequate VO2 is restored. Thus, it is intuitive that flow monitoring must be aimed at early adaptation of VO2 to metabolic needs [3,4]. Although this is universally accepted, its usefulness at the bedside has been challenged because of theoretical and practical limitations of VO2 assessment [5,6]. However, it has been shown that several of these limitations have been over-stated [4]. In addition, targeting a VO2 that is adequate to meet the patient's needs does not necessarily require continuous VO2 measurement. Monitoring VO2-related variables such as cardiac output (CO) and/or mixed venous oxygen saturation (SvO2) may represent an acceptable compromise, especially as these variables can be obtained less invasively.
This review proposes a simple and comprehensive schema for understanding and adapting flow monitoring in order to stabilize the macrocirculation.
Fundamental basis of the relationship between oxygen consumption and delivery
For each cell, life requires enough energy for metabolic activity. Energy depends on oxidative reactions that require nutrients and oxygen. For each cell most of the oxygen is used for oxidative mechanisms. Nonoxidative systems have lower affinity for oxygen than do cytochrome oxidase systems. Therefore, significant activity of the non-mitochondrial oxidase systems can only be present when there is no more dysoxia.
Hence, for each cell a match between VO2 and needed VO2 (nVO2) is necessary for life. This basic relationship between life and energy is also applicable to each organ and to the body as a whole. However, a whole body VO2 that equals body needs does not guarantee that circulation is adequate for each cell because distributive mismatch may lead to nonoxidative metabolism in some areas and dysoxia in others. However, it is a prerequisite that the macrocirculation must be stabilized before one may examine the microcirculation. Consequently, the first priority is to consider the balance between whole body VO2 and nVO2.
For all systems, VO2 is the difference between the input flow and the output flow. For the whole body circulation, the input flow is the arterial oxygen delivery (DaO2) and the output flow is the venous oxygen delivery. If one considers the oxygen extraction ratio (EO2) to be the ratio between VO2 and DaO2, then VO2 can be represented by the product DaO2 × EO2. The simple equation VO2 = DaO2 × EO2 is conventionally used to represent the macrocirculatory balance.
The VO2 observed (oVO2) by a clinician (either measured or calculated) is the product of an observed DO2 and an observed EO2, such that oVO2 = oDO2 × oEO2. Similarly, the specific patient's requirements (nVO2) may be formulated as the product of the needed DO2 and the needed EO2: nVO2 = nDO2 × nEO2. The ratio between these two equations represents the balance between what the doctor sees and what the patient needs: oVO2/nVO2 = oDO2/nDO2 × oEO2/nEO2. Any change in oDO2/nDO2 must be balanced by an inverse change in oEO2/nEO2 to maintain oVO2/nVO2 = 1 and vice versa. When oVO2/nVO2 = 1 cannot be maintained, dysoxia occurs. Consequently, three indices of performance may be described: oVO2/nVO2 is an index of global performance, with a value below 1 indicating shock; oDO2/nDO2 is an index of circulatory performance, with a value below 1 indicating circulatory failure; and oEO2/nEO2 is an index of tissue performance, with a value below 1 indicating tissue failure.
We do not propose that these indices be calculated for each and every patient, but they should perhaps be borne in mind to facilitate, at any time, empirical review of the patient's likely status and to determine the probable results of any therapeutic intervention.
Clinical means to deal with concepts
Evaluation of whether macrocirculatory adaptation is adequate requires one to answer several simple questions.
Is oxygen consumption equal to the patient's needs?
Otherwise stated, is the expression oVO2/nVO2 = 1 true? Three levels of complexity may be defined.
First, clinical improvement is a good indicator of adequate resuscitation [7]. In practice, the nVO2 is usually met by decreasing metabolic requirement, optimizing the haematocrit and arterial haemoglobin oxygen saturation, and increasing blood flow empirically until the clinical status improves. This situation does not require invasive haemodynamic investigation.
Second, a clear improvement in blood lactate clearance is also a good and minimally invasive indicator of adequate resuscitation [7]. The blood lactate concentration alone fails to discriminate between dysoxia and aerobiosis [8]. Although more reliable, the time course of lactate levels is not an ideal marker [2,7,9]. The limitations of lactate were recently reviewed [8]. Diabetes mellitus, liver dysfunction, tissue reperfusion, catecholamine infusion, cellular metabolic alterations and inhibition of pyruvate dehydrogenase can all result in a marked increase in blood lactate concentrations, despite improvement in tissue dysoxia.
Finally, in more complex situations in which clear clinical improvement and normalization in blood lactate are not observed, evaluation of oxygenation is required, followed by an evaluation of oVO2 and nVO2. The oVO2 can be measured at the bedside using expired gases [10] or it may be calculated from the product of CO and the arteriovenous difference in blood oxygen content. Demonstrating that oVO2/nVO2 = 1 requires one to evaluate nVO2 concomitantly. When oVO2 is evaluated alone, this provides no information of prognostic interest [2].
How may we estimate the needed oxygen consumption?
Needs can initially be estimated as the sum of VO2 at basal metabolism, as indicated by age-specific and sex-specific normative data, and the additional VO2 that results from other metabolic requirements. The latter can be approximated based on a number of factors, such as body temperature (nVO2 changes by ± 13% for each 1°C above or below 37°C). Pathologic situations such as respiratory failure and severe sepsis also increase metabolic needs. Based on metabolic conditions, nVO2 can vary from 0.7-fold to 3-fold the basal metabolism.
Needs can also be estimated by using the specific VO2/DO2 relationship (Figure 1). A biphasic relationship between oxygen use and resources has been established [6]. When DO2 is greater than a threshold value, VO2 remains stable (oxygen supply independency) because the EO2 changes proportionally. When DO2 falls below this threshold, a proportionate increase in EO2 cannot be maintained and the VO2 drops linearly to zero (oxygen supply dependency). There is consensus that the inflection point between the two slopes indicates the critical level of DO2 (Figure 1). Oxygen supply dependency is associated with increased blood lactate concentration, denoting possible activation of the anaerobic pathway.
Figure 1.
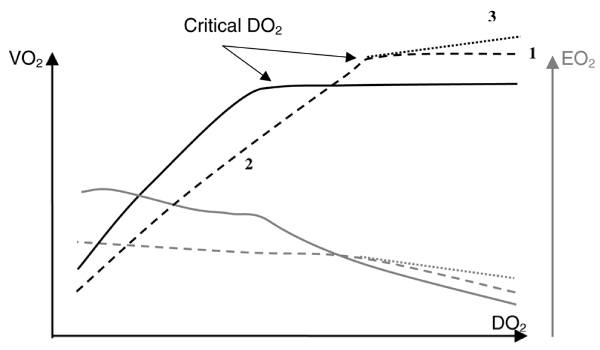
Pathophysiological changes in the VO2/DO2 relationship. Normal relationship is shown in a solid black line, and abnormal relationships in dotted lines. 1: Increased VO2 needs; 2: impaired EO2; 3: other mechanisms (see text). The grey curves are the corresponding EO2/DO2 relationships. DO2, oxygen delivery; EO2, oxygen extraction ratio; VO2, oxygen consumption. Reproduced with permission from Squara [4].
Assessment of the VO2/DO2 relationship is a theoretical means to evaluate the gap between actual VO2 and nVO2. When DO2 increases, an increase in VO2 suggests that oxygen supply is inadequate. In contrast, a stable VO2 value when DO2 increases suggests either that VO2 matches needs when it is associated with decreasing lactate levels [11,12] or that VO2 is limited by mechanisms other than oxygen supply when it is associated with increasing lactate levels [13,14].
In pathophysiology, two mechanisms delay achievement of the VO2 plateau and account for a rightward shift in the critical DO2 point (Figure 1). When VO2 needs are excessive (uncoupling and/or increased metabolic activity), the VO2 plateau is reached at a higher level of VO2 [15,16]. When oxygen tissue diffusion is impaired (impaired microcirculation and/or impaired oxygen mitochondrial use), the slope of the dependant part of the VO2/DO2 relationship is decreased [17,18].
Three other mechanisms result in an increase in VO2 as DO2 increases beyond the critical point, so that a slight upward slope – usually of less than 5% – replaces the expected VO2 plateau. Although more difficult, identification of the critical DO2 inflection point remains possible when these mechanisms are operative because the slope of the VO2/DO2 dependency segment ranges from 20% to 50% [19]. The first mechanism occurs during a DO2 challenge involving an increase in CO, because the VO2 needs of kidneys [20], stomach [21] and muscle [22] increase in direct proportion to flow. Furthermore, infusion of inotropic agents increases myocardial oxygen consumption [11,12,19]. Another mechanism is additional oxygen uptake due to non-mitochondrial oxidase systems when dysoxia has resolved [23]. The final mechanism, termed conformance, is a decrease in the metabolic needs of cells that occurs in response to a gradual decline in available oxygen. Although secondary to a chronic change, this phenomenon has been observed in acute situations [24]. Schumacker and coworkers [25] reported that a VO2 increase occurred in unshocked patients after aortic stenosis valvuloplasty.
A controversy arose during the late 1980s from several studies on acute respiratory distress syndrome and/or sepsis, in which the expected VO2 plateau was not observed in patients who were recovering from shock and had high DO2 values [26,27]. This was interpreted as evidence of 'pathologic oxygen supply dependency', possibly related to hidden oxygen deficit and contributing to multiorgan failure and death. However, increasing DO2 to supranormal values was beneficial in some studies [28,29] but not in others [30,31]. Furthermore, it has been suggested this so-called 'pathologic supply dependency' may result from spurious up-sloping of the VO2/DO2 relationship due to mathematical coupling of measurement errors when using a pulmonary artery catheter (PAC), because in some studies simultaneous independent VO2 assessment revealed a plateau [5,6,32]. In addition, VO2 and DO2 assessment are limited by theoretical and practical concerns [5,6]. However, these limitations were recently reviewed [4]. Use of the most recent generation of devices for continuous CO monitoring and blood gas analysis minimizes the variability in measurement. It has been proposed that the relevance of the VO2/DO2 relationship could be increased by combined analysis of the VO2/time relationship (Figure 2) [4]. Thus, although difficult, acceptable identification of the VO2 plateau, and of the nVO2, is possible when necessary.
Figure 2.
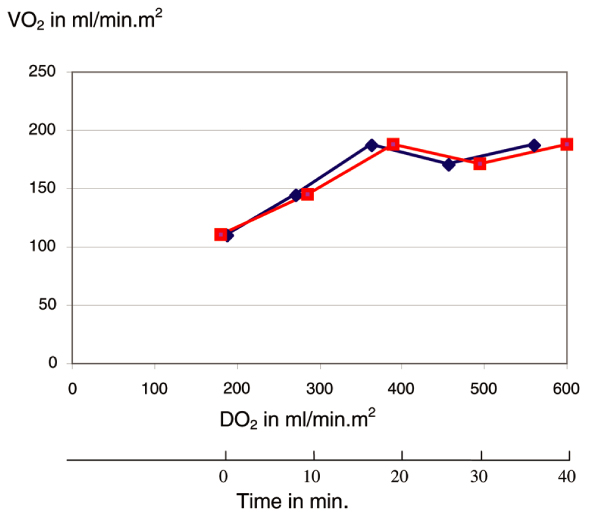
Comparison between the VO2/DO2 relationship and the VO2/time relationship in one hypothetical example. For this figure, DO2 increased linearly with time. This helps to identify the critical VO2 point and eliminates the possible effect of mathematical coupling of error. DO2, oxygen delivery; VO2, oxygen consumption. Reproduced with permission from Squara [4].
Finally, it may be concluded that oVO2 = nVO2 when one or several of the following factors is present: clinical improvement, decrease in blood lactate concentration, and oVO2 inside the expected range and/or inflexion point in the oVO2/DO2 curve. The two methods can be combined. When the oVO2 plateau is reached at a value close to the estimated needs, the patient's real needs are probably met. Handling the large amount of information required to assess oxygen needs can be difficult [33,34], and computer assistance may be helpful [2,35,36].
Are there other means to balance oxygen consumption and needs?
Supraphysiologic targets
Some investigators have recommended that DO2 be increased to supranormal values, greater than the usual critical level, without paying much attention to VO2. This simplification of the method based on the VO2/DO2 relationship was associated with favourable outcomes in homogeneous populations of patients undergoing high-risk surgery [37,38], with cardiogenic shock following myocardial infarction [39] and with acute respiratory failure [15,40]. However, those studies failed to demonstrate any beneficial effects after the onset of organ failure [38] or when different aetiologies of shock were pooled together [15,40].
Monitoring of cardiac output and mixed venous oxygen saturation
Other studies suggest that sequential DO2 and VO2 calculations can be advantageously replaced by continuous measurement of CO [41], SvO2 [42], or central venous oxygen saturation [43]. The use of these variables avoids compounding of measurement errors and allows for continuous comparison between measured values and targeted values.
However, targeting a pre-established value for DO2, CO, or SvO2 does not prove that these values meet the needs of an individual patient [16]. These pre-established targets are derived from normal findings or from survivors in selected populations of patients [44,45]. Determination of the needed value of one given variable must take into consideration the limitation in other variables that are specific to the patient, his past history, the actual pathologic event, the delay before onset of shock and often recent therapeutic interventions (Figure 3). Intuitive evaluation of the needed value of each variable in each specific case requires considerable expertise. Misinterpretation of information derived from PAC placement and heterogeneity in the medical decision process is frequent [30,31]. Even for experts, intuitive evaluation of needs may be subject to errors [16]. In some conditions, such as coronary disease, efforts to increase CO in order to 'normalize' the cardiac index to more than 2.5 l/min per m2 or the SvO2 value to more than 70% can be harmful (see examples given below). In addition, there is some evidence that an excessive oxygen supply may be deleterious, either via the useless metabolic cost of an excessive increase in DO2 or via activation of nonoxidative systems. Failure to consider these latter two mechanisms may also account for the poor results obtained in controlled studies targeting nonspecific 'supranormal' values of DO2 [30,31]. Thus, treatment efforts should be limited to what is necessary – no less and no more.
Figure 3.
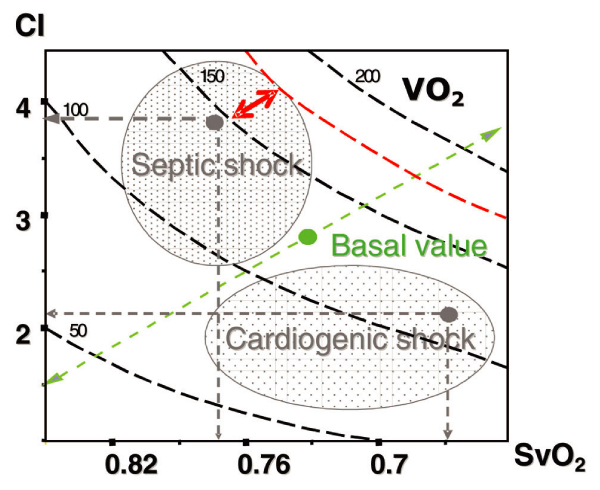
Nomogram showing CI, SvO2 and VO2 isopleths (dotted black lines). The green point shows the expected values for a 59-year-old woman at basal metabolism, and the green dotted arrow indicates the expected normal variations in case of hypo- or hypermetabolism. The real position of the patient in the nomogram can be continuously monitored. This is adequate for diagnostic purposes. The patient's position can move from the normal profile to a characterized area of septic or cardiogenic shock (grey dotted arrows and areas). However, for therapeutic objectives, this nomogram gives no idea of needs. If we made the hypothesis that the nVO2 (red isopleth) is higher than the oVO2, then the red double arrow indicates the difference between nVO2 and oVO2. Units for CI are l/min per m2 and for VO2 they are ml/min per m2. CI, cardiac index; (n/o)VO2, (needed/observed) oxygen consumption; SvO2, mixed venous oxygen saturation.
The relationship between cardiac output and mixed venous oxygen saturation
All haemodynamic variables are interrelated, and ensuring that VO2 meets needs is the best tool to ensure that global haemodynamic status is adequate. VO2, whether calculated by spirometry, indirect calorimetry, or using a PAC, is similar to the plateau of VO2 in the VO2/DO2 relationship. No other relationship between two variables allows a clear identification of a plateau or a clear inflection point between anaerobiosis and aerobiosis. The shape of the CO/SvO2 relationship or the CO/EO2 relationship is bi-curvilinear and similar to the DO2/EO2 relationship shown in Figure 1. A clear inflexion point between aerobiosis and anaerobiosis is much more difficult to identify than the VO2/DO2.
Clinical examples
Example 1
Patient 1, receiving sedative drugs and mechanical ventilation, was admitted to an ICU immediately after an aortic valve replacement. He was hypothermic, with marbled and cold extremities. Haemodynamic variables are listed in Table 1. In this patient, cold extremities may be due to hypothermia, and the supranormal serum lactate may result from postoperative washout. Therefore, clinical evaluation including lactate level is not relevant in evaluating macrocirculatory performance relative to metabolic needs. Other means to explore the balance between VO2 and needs are conflicting. The SvO2 (65%) was below the expected value and may be considered a marker of unacceptably low CO and oxygen flow [45,46]. In contrast the calculated oVO2 (88 ml/min per m2) is close to expected nVO2 (90 ml/min per m2) when assessed using the basal VO2 value for this 82-year-old man (119 ml/min per m2, as indicated by age-specific and sex-specific normative data), corrected according to the low body temperature. It would be difficult to exploit the VO2/DO2 relationship. No VO2 plateau is expected in the early postoperative period because of increasing metabolic needs.
Table 1.
Clinical parameters of two patients admitted to the ICU (sedative infusions and mechanical ventilation required)
| Patient 1 (male, 84 years) | Patient 2 (male, 24 years) | ||||
|---|---|---|---|---|---|
| Parameters | H0 | H2 | H0 | H5 | H6 |
| Temperature (°C) | 35.2 | 36.8 | 40.2 | 38.5 | 38.5 |
| MAP (mmHg) | 65 | 68 | 55 | 99 | 97 |
| Heart rate (beats/min) | 65 | 74 | 117 | 113 | 111 |
| SpO2 (%) | 100 | 100 | 97 | 96 | 97 |
| Haemoglobin (g/l) | 11.0 | 11.1 | 13.6 | 13.0 | 13.0 |
| Serum lactate (mEq/l) | 3 | 2 | 10.3 | 6.6 | 6.2 |
| Cardiac index (l/min per m2) | 2.1 | 2.3 | 4.1 | 6.5 | 6.4 |
| SvO2 (%) | 65 | 68 | 75 | 76 | 75 |
| oVO2 (mL/min per m2) | 88 | 119 | 178 | 240 | 237 |
H, delay in hours; ICU, intensive care unit; MAP, mean arterial pressure; SvO2, mixed venous oxygen saturation; oVO2, observed oxygen consumption.
The clinician on duty disregards the SvO2 threshold and concluded that the haemodynamic status was adequate to the patient's needs and no specific treatment was given. Two hours later (Table 1), a decrease in lactate serum value, normalization in SvO2 and a calculated oVO2 = basal VO2 demonstrate that metabolic needs were probably covered.
In this case, a rough interpretation of SvO2 below 70% as an indicator of insufficient CO as compared with needs would have led to an unjustified increase in CO. An SvO2 below 70% can be normal in elderly patients, especially if haemoglobin level is low, as is frequently observed postoperatively.
Example 2
Patient 2, requiring sedation and mechanical ventilation, was admitted to an ICU with a history of sudden shock and hyperkinetic state (Table 1). Was VO2 adequate to needs? There is agreement between the clinical signs of shock with elevated lactate level and a calculated oVO2 below the needed value (216 ml/min per m2) according to basal VO2 fora 24-year-old man (152 ml/min per m2) corrected for the high temperature. In contrast, the SvO2 value, higher than normal values, suggests that CO and oxygen flow are adequate.
Once again, the clinician on duty disregards the SvO2 threshold and concluded that the haemodynamic status was inadequate for the patient's needs. A resuscitation regimen combining cooling, fluid optimization, and dobutamine and noradrenaline (norepinephrine) was instituted in addition to antibiotics. CO increased, SvO2 remained stable (Table 1) and calculated oVO2 increased over its needed value, whereas lactate serum decreased, suggesting that metabolic needs were covered.
In this case, an interpretation of the SvO2 above 70% as an indicator that the hyperkinetic state was adequate to needs would have led to insufficient resuscitation. SvO2 can be above 70% in pathological states, for instance involving severe impairment in tissue oxygen diffusion.
Practical implications
The rationale for incorporating the VO2/DO2 relationship into clinical management strategies is supported by several studies in which most of the limiting factors listed above were avoided [13,14]. In contrast, the chances of survival are very small in patients whose DO2 and VO2 fail to increase with treatment, despite evidence of an oxygen deficit [13,14]. Thus, reaching the critical DO2 and ensuring that VO2 needs are met are crucial objectives, even though these two variables are calculated or intuitively estimated. To increase the likelihood of identifying clinical benefits related to bedside VO2 guided therapy, we suggest a number of practical guidelines. As stated above, computer assistance may be helpful in harmonizing the diagnostic reasoning processes of different clinicians for different patients [2,35].
Early detection of shock states
Shock responds better to haemodynamic resuscitation in the early stages [43]. Although the final objective is to provide sufficient oxygen to each cell, there is some evidence that rapidly achieving a sufficient total body VO2 is a prerequisite. Late-stage shock is a far more complex situation that involves not only the macrocirculation and microcirculation but also cell metabolism and the consequences of cell necrosis, which cannot be corrected by haemodynamic resuscitation alone.
Matching oxygen consumption to needs is the first objective
In most situations, targeting a clinical improvement, a decrease in lactate level, or a pre-established value for CO or SvO2, or both, is an acceptable and intuitive means of achieving adequate VO2. In complex situations, by plotting VO2/DO2 over time during a DO2 challenge, the critical DO2 value can be evaluated rapidly by identifying the inflection point on the curve, and resuscitation efforts can then be limited to what is necessary. Because the critical DO2 value can be determined visually with a 95% confidence interval of 20%, it is reasonable to limit DO2 to its observed critical value +20%. When lactate remains high despite evidence that a VO2 plateau has been reached, increasing DO2 further does not seem to add benefit [13,14]. Continuous efforts to decrease oxygen demand and to improve the microcirculation may be more appropriate [47]. Combined analysis of the VO2/DO2 and VO2/time relationships provides the most useful approach, because the effects of mathematical coupling of errors and the theoretical limitations resulting from DO2 variability in the regression line derivations are minimized. A mild up-sloping of the VO2 plateau (slope <10%) should not be confused with oxygen dependency. When necessary, the critical DO2 point can be determined more accurately using the method developed by John-Alder and coworkers [48].
To reach this objective, the best compromise must be identified, mostly based on metabolic cost
Hyperthermia, acute respiratory failure and/or pain all increase VO2 needs sharply. In contrast, cooling, sedation and mechanical ventilation often produce a 50% decrease in VO2 needs. The latter has exactly the same favourable effect as doubling the CO or doubling the EO2. Improving EO2 must be always considered, although this rarely produces a rapid increase in VO2. Treating infection, excessive sedation, or excessive water retention, for example, may increase EO2 [43]. When the only possibility is to increase DO2, clinicians must choose among various agents that presumably differ in their caloric effects. Arterial vasodilatation improves DO2 and decreases myocardial oxygen requirements. In contrast, inotropic agents and vasoconstrictors have major caloric effects. Whatever the method used, a metabolic price must be paid for improving VO2 and DO2 up to critical values. This metabolic price (a part of VO2 needs) must also be limited to what is strictly necessary.
Conclusion
Matching the VO2 and nVO2 is a crucial objective in critically ill patients, and must take into account the specific situation of the patient and its pathological limitations. Achieving this objective requires one to decrease oxygen needs first, to improve EO2 when possible and then to improve DO2. In most situations, targeting a clinical improvement, a decrease in lactate level, or a pre-established value for CO, SaO2, or SvO2 (or all of these) is an acceptable and intuitive means of achieving an adequate VO2. However, intuitive evaluation of the needed value for each variable in each specific case requires considerable expertise, considering all available variables, and may be subject to error.
In complex situations, by plotting VO2/DO2 over time during a DO2 challenge, the critical DO2 value can be rapidly identified as the inflection point on the curve, and resuscitation efforts can then be limited to what is necessary. Whatever the method used, a metabolic price must be paid for improving VO2 and DO2 to the critical values, and must be limited to what is strictly necessary. Thus, the more complex the critically ill presentation, the greater the number of global haemodynamic variables that are needed.
Flow monitoring is of major interest in terms of stabilizing the macrocirculation. A stabilized macrocirculation is a global pre-requisite, and must be achieved before one looks at the local microcirculation.
Although we do not have direct evidence of any clinical benefits from invasive hemodynamic monitoring, we believe that more intensive monitoring (invasive or non-invasive) is needed to ensure the safety of acutely ill patients, otherwise we would not have ICUs.
Bellomo and Uchino [49]
Abbreviations
CO = cardiac output; DaO2 = arterial oxygen delivery; DO2 = oxygen delivery; EO2 = oxygen extraction ratio; ICU = intensive care unit; PAC = pulmonary artery catheter; SvO2 = mixed venous oxygen saturation; VO2 = oxygen consumption.
Competing interests
PS is a consultant for Edwards Lifesciences. This manuscript was written from a slide presentation as part of a European PAC course promoted by Edwards Lifesciences.
Acknowledgements
The authors thank Professor Alexandre Mebazza for his critical review of the manuscript.
References
- Vincent JL, Thijs L, Cerny V. Critical care in Europe. Crit Care Clin. 1997;13:245–254. doi: 10.1016/S0749-0704(05)70307-9. [DOI] [PubMed] [Google Scholar]
- Squara P, Journois D, Formela F, Dhainaut J, Sollet JP, Bleichner G. Value of elementary, calculated and modeled hemodynamic variables. J Crit Care. 1994;9:223–235. doi: 10.1016/0883-9441(94)90002-7. [DOI] [PubMed] [Google Scholar]
- Russell JA, Phang PT. The oxygen delivery/consumption controversy. Approaches to management of the critically ill. Am J Respir Crit Care Med. 1994;149:533–537. doi: 10.1164/ajrccm.149.2.8306058. [DOI] [PubMed] [Google Scholar]
- Squara P. Matching total body oxygen consumption and delivery: a crucial objective? Intensive Care Med. 2004;30:2170–2179. doi: 10.1007/s00134-004-2449-4. [DOI] [PubMed] [Google Scholar]
- Granton JT, Walley KR, Phang PT, Russell JA, Lichtenstein S. Assessment of three methods to reduce the influence of mathematical coupling on oxygen consumption and delivery relationships. Chest. 1998;113:1347–1355. doi: 10.1378/chest.113.5.1347. [DOI] [PubMed] [Google Scholar]
- Hanique G, Dugernier T, Laterre PF, Dougnac A, Roeseler J, Reynaert MS. Significance of pathologic oxygen supply dependency in critically ill patients: comparison between measured and calculated methods. Intensive Care Med. 1994;20:12–18. doi: 10.1007/BF02425048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker J, Coffernils M, Leon M, Gris P, Vincent JL. Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest. 1991;99:956–962. doi: 10.1378/chest.99.4.956. [DOI] [PubMed] [Google Scholar]
- De Backer D. Lactic acidosis. Intensive Care Med. 2003;29:699–702. doi: 10.1007/s00134-003-1746-7. [DOI] [PubMed] [Google Scholar]
- Bakker J, Gris P, Coffernils M, Kahn RJ, Vincent JL. Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg. 1996;171:221–226. doi: 10.1016/S0002-9610(97)89552-9. [DOI] [PubMed] [Google Scholar]
- Smithies MN, Royston B, Makita K, Konieczko K, Nunn JF. Comparison of oxygen consumption measurements: indirect calorimetry versus the reversed Fick method. Crit Care Med. 1991;19:1401–1406. doi: 10.1097/00003246-199111000-00017. [DOI] [PubMed] [Google Scholar]
- Gilbert EM, Haupt MT, Mandanas RY, Huaringa AJ, Carlson RW. The effect of fluid loading, blood transfusion, and catecholamine infusion on oxygen delivery and consumption in patients with sepsis. Am Rev Respir Dis. 1986;134:873–878. doi: 10.1164/arrd.1986.134.5.873. [DOI] [PubMed] [Google Scholar]
- Vincent JL, Roman A, De Backer D, Kahn RJ. Oxygen uptake/supply dependency. Effects of short-term dobutamine infusion. Am Rev Respir Dis. 1990;142:2–7. doi: 10.1164/ajrccm/142.6_Pt_2.S2. [DOI] [PubMed] [Google Scholar]
- Rhodes A, Lamb FJ, Malagon I, Newman PJ, Grounds RM, Bennett ED. A prospective study of the use of a dobutamine stress test to identify outcome in patients with sepsis, severe sepsis, or septic shock. Crit Care Med. 1999;27:2361–2366. doi: 10.1097/00003246-199911000-00007. [DOI] [PubMed] [Google Scholar]
- Vallet B, Chopin C, Curtis SE, Dupuis BA, Fourrier F, Mehdaoui H, LeRoy B, Rime A, Santre C, Herbecq P. et al. Prognostic value of the dobutamine test in patients with sepsis syndrome and normal lactate values: a prospective, multicenter study. Crit Care Med. 1993;21:1868–1875. doi: 10.1097/00003246-199312000-00014. [DOI] [PubMed] [Google Scholar]
- Bihari D, Smithies M, Gimson A, Tinker J. The effects of vasodilation with prostacyclin on oxygen delivery and uptake in critically ill patients. N Engl J Med. 1987;317:397–403. doi: 10.1056/NEJM198708133170701. [DOI] [PubMed] [Google Scholar]
- Mohsenifar Z, Goldbach P, Tashkin DP, Campisi DJ. Relationship between O2 delivery and O2 consumption in the adult respiratory distress syndrome. Chest. 1983;84:267–271. doi: 10.1378/chest.84.3.267. [DOI] [PubMed] [Google Scholar]
- Gutierrez G, Marini C, Acero AL, Lund N. Skeletal muscle PO2 during hypoxemia and isovolemic anemia. J Appl Physiol. 1990;68:2047–2053. doi: 10.1152/jappl.1990.68.5.2047. [DOI] [PubMed] [Google Scholar]
- Nelson DP, Beyer C, Samsel RW, Wood LD, Schumacker PT. Pathological supply dependence of O2 uptake during bacteremia in dogs. J Appl Physiol. 1987;63:1487–1492. doi: 10.1152/jappl.1987.63.4.1487. [DOI] [PubMed] [Google Scholar]
- De Backer D, Moraine JJ, Berre J, Kahn RJ, Vincent JL. Effects of dobutamine on oxygen consumption in septic patients. Direct versus indirect determinations. Am J Respir Crit Care Med. 1994;150:95–100. doi: 10.1164/ajrccm.150.1.8025780. [DOI] [PubMed] [Google Scholar]
- Jeppsson A, Ekroth R, Friberg P, Kirno K, Milocco I, Nilsson F, Svensson S. Renal effects of amino acid infusion in cardiac surgery. J Cardiothorac Vasc Anesth. 2000;14:51–55. doi: 10.1016/S1053-0770(00)90056-9. [DOI] [PubMed] [Google Scholar]
- Jacobson E. Effects of histamine, acetylcholine, and norepinephrine on gastric vascular resistance. Am J Physiol. 1963;204:1013–1017. doi: 10.1152/ajplegacy.1963.204.6.1013. [DOI] [PubMed] [Google Scholar]
- Duran W, Renkin E. Oxygen consumption and blood flow in resting mamalians skeletal muscles. Am J Physiol. 1974;226:173–177. doi: 10.1152/ajplegacy.1974.226.1.173. [DOI] [PubMed] [Google Scholar]
- McCord J. Oxygen-derived free radicals in post ischemic tissue injury. N Engl J Med. 1985;312:159–161. doi: 10.1056/NEJM198501173120305. [DOI] [PubMed] [Google Scholar]
- Schumacker PT, Chandel N, Agusti AG. Oxygen conformance of cellular respiration in hepatocytes. Am J Physiol. 1993;265:L395–L402. doi: 10.1152/ajplung.1993.265.4.L395. [DOI] [PubMed] [Google Scholar]
- Schumacker PT, Soble JS, Feldman T. Oxygen delivery and uptake relationships in patients with aortic stenosis. Am J Respir Crit Care Med. 1994;149:1123–1131. doi: 10.1164/ajrccm.149.5.8173751. [DOI] [PubMed] [Google Scholar]
- Clarke C, Edwards JD, Nightingale P, Mortimer AJ, Morris J. Persistence of supply dependency of oxygen uptake at high levels of delivery in adult respiratory distress syndrome. Crit Care Med. 1991;19:497–502. doi: 10.1097/00003246-199104000-00007. [DOI] [PubMed] [Google Scholar]
- Gutierrez G, Pohil RJ. Oxygen consumption is linearly related to O2 supply in critically ill patients. J Crit Care. 1986;1:45–53. doi: 10.1016/S0883-9441(86)80116-2. [DOI] [Google Scholar]
- Edwards J, Brown G, Nightingale P, Slater RM, Faragher EB. Use of survivors' cardiorespiratory values as therapeutic goals in septic shock. Crit Care Med. 1989;17:1098–1103. doi: 10.1097/00003246-198911000-00002. [DOI] [PubMed] [Google Scholar]
- Shoemaker W, Appel P, Kram H, Waxman K, Lee T. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176–1186. doi: 10.1378/chest.94.6.1176. [DOI] [PubMed] [Google Scholar]
- Gattinoni L, Brazzi L, Pelosi P, Latini R, Tognoni G, Pesenti A, Fumagalli R. A trial of goal-oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995;333:1025–1032. doi: 10.1056/NEJM199510193331601. [DOI] [PubMed] [Google Scholar]
- Hayes MA, Timmings AC, Yau EH, Palazzo M, Hinds CJ, Watson D. Elevation of systemic oxygen delivery in the treatment of critically ill patients. N Engl J Med. 1994;330:1717–1722. doi: 10.1056/NEJM199406163302404. [DOI] [PubMed] [Google Scholar]
- Mira J, Fabre J, Baigorr IF, Coste J, Annat G, Artigas A, Nitenberg G, Dhainaut J. Lack of oxygen supply dependency in patients with severe sepsis. A study of oxygen delivery increased by military antishock trouser and dobutamine. Chest. 1994;106:1524–1531. doi: 10.1378/chest.106.5.1524. [DOI] [PubMed] [Google Scholar]
- Gnaegi A, Feihl F, Perret C. Intensive care physicians' insufficient knowledge of right heart catheterization at the bedside: time to act? Crit Care Med. 1997;25:213–220. doi: 10.1097/00003246-199702000-00003. [DOI] [PubMed] [Google Scholar]
- Squara P, Bennett D, Perret C. Pulmonary artery catheter: does the problem lie in the users? Chest. 2002;121:2009–2015. doi: 10.1378/chest.121.6.2009. [DOI] [PubMed] [Google Scholar]
- Squara P, Dhainaut J, Lamy M, Perret C, Larbuisson R, Poli S, Armaganidis A, de Gournay J, Bleichner G. Computer assistance for hemodynamic evaluation. J Crit Care. 1989;4:273–282. doi: 10.1016/0883-9441(89)90067-1. [DOI] [Google Scholar]
- Hemodyn homepage. http://www.hemodyn.com
- Boyd O, Grounds RM, Bennett ED. A randomized clinical trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk surgical patients. JAMA. 1993;270:2699–2707. doi: 10.1001/jama.270.22.2699. [DOI] [PubMed] [Google Scholar]
- Kern JW, Shoemaker WC. Meta-analysis of hemodynamic optimization in high-risk patients. Crit Care Med. 2002;30:1686–1692. doi: 10.1097/00003246-200208000-00002. [DOI] [PubMed] [Google Scholar]
- Creamer JE, Edwards JD, Nightingale P. Hemodynamic and oxygen transport variables in cardiogenic shock secondary to acute myocardial infarction, and response to treatment. Am J Cardiol. 1990;65:1297–1300. doi: 10.1016/0002-9149(90)91316-X. [DOI] [PubMed] [Google Scholar]
- Hankeln KB, Gronemeyer R, Held A, Bohmert F. Use of continuous noninvasive measurement of oxygen consumption in patients with adult respiratory distress syndrome following shock of various etiologies. Crit Care Med. 1991;19:642–649. doi: 10.1097/00003246-199105000-00010. [DOI] [PubMed] [Google Scholar]
- Mihm FG, Gettinger A, Hanson CW 3rd, Gilbert HC, Stover EP, Vender JS, Beerle B, Haddow G. A multicenter evaluation of a new continuous cardiac output pulmonary artery catheter system. Crit Care Med. 1998;26:1346–1350. doi: 10.1097/00003246-199808000-00018. [DOI] [PubMed] [Google Scholar]
- Armaganidis A, Dhainaut JF, Billard JL, Klouche K, Mira JP, Brunet F, Dinh-Xuan AT, Dall'Ava-Santucci J. Accuracy assessment for three fiberoptic pulmonary artery catheters for SvO2 monitoring. Intensive Care Med. 1994;20:484–488. doi: 10.1007/BF01711900. [DOI] [PubMed] [Google Scholar]
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- Madsen P, Iversen H, Secher NH. Central venous oxygen saturation during hypovolaemic shock in humans. Scand J Clin Lab Invest. 1993;53:67–72. doi: 10.1080/00365519309092533. [DOI] [PubMed] [Google Scholar]
- Jenstrup M, Ejlersen E, Mogensen T, Secher NH. A maximal central venous oxygen saturation (SvO2max) for the surgical patient. Acta Anaesthesiol Scand Suppl. 1995;107:29–32. doi: 10.1111/j.1399-6576.1995.tb04326.x. [DOI] [PubMed] [Google Scholar]
- Krafft P, Steltzer H, Hiesmayr M, Klimscha W, Hammerle AF. Mixed venous oxygen saturation in critically ill septic shock patients. The role of defined events. Chest. 1993;103:900–906. doi: 10.1378/chest.103.3.900. [DOI] [PubMed] [Google Scholar]
- Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van Straaten HM, Zandstra DF. Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet. 2002;360:1395–1396. doi: 10.1016/S0140-6736(02)11393-6. [DOI] [PubMed] [Google Scholar]
- John-Alder HB, Bennett AF. Thermal dependence of endurance and locomotory energetics in a lizard. Am J Physiol. 1981;241:R342–R349. doi: 10.1152/ajpregu.1981.241.5.R342. [DOI] [PubMed] [Google Scholar]
- Bellomo R, Uchino S. Cardiovascular monitoring tools: use and misuse. Curr Opin Crit Care. 2003;9:225–229. doi: 10.1097/00075198-200306000-00010. [DOI] [PubMed] [Google Scholar]


