Abstract
Purpose
To test the hypothesis that females with patellofemoral pain (PFP) have increased hip adduction, hip medial rotation, and knee valgus (medial collapse) during the stance phase of gait.
Methods
Twenty subjects with PFP and 20 pain-free subjects participated. Subjects underwent 3-dimensional motion analysis during free speed and fast speed walking. Hip frontal and transverse plane angles and knee frontal plane angles were calculated at 2 time points (peak knee extensor moment (PkMOM), and maximum knee extension/hyperextension angle (MxExt)) and averaged over 3 trials. Within each walking task, Student’s t-tests compared group differences in all variables. A post-hoc analysis was performed comparing a subgroup of 4 PFP subjects (those whose pain level was above 30/100) to pain-free subjects.
Results
Initially, there were no group differences during free speed walking. During fast speed walking, subjects with PFP had less hip adduction at PkMOM and greater hip adduction at MxExt. The subgroup of PFP subjects had greater hip adduction at PkMOM and greater knee valgus at MxExt during free speed walking and greater hip adduction and knee valgus at MxExt during fast speed walking.
Conclusions
During low-level tasks, frontal plane components of medial collapse were present at the hip and knee in a subgroup of PFP subjects with higher pain levels. Symptom behavior may be important in identifying individuals with medial collapse movement impairments.
Keywords: biomechanics, medial collapse, 3-d motion analysis, lower extremity overuse injuries
INTRODUCTION
Patellofemoral pain (PFP) is one of the most common musculoskeletal pain conditions (Grady et al., 1998; Sanchis-Alfonso, Rosello-Sastre, and Martinez-Sanjuan, 1999; Taunton et al., 2002), yet the mechanism of pain development is poorly understood. Prevailing theories propose that pain develops in response to elevated patellofemoral joint stress (force per unit area) (Goodfellow, Hungerford, and Woods, 1976; Grana and Kriegshauser, 1985; Seedhom, Takeda, Tsubuku, and Wright, 1979) due to abnormal patellar alignment (increased lateral displacement and tilt) (Hungerford and Lennox, 1983; Outerbridge and Dunlop, 1975). However, treatments aimed at restoring patellar alignment have been marginally successful, and numerous studies have reported no differences in patellar alignment when subjects with PFP were compared to a control group (Kannus, 1992; Laprade and Culham, 2003; Macintyre et al., 2006; Thomee, Renstrom, Karlsson, and Grimby, 1995). Collectively, these findings suggest that factors other than patellar malalignment may contribute to increased stress and ultimately pain development.
Investigators have begun to explore the contribution of hip and knee kinematics to PFP, with the rationale that, because the patella is mechanically linked to the femur and tibia, frontal and transverse plane motion of the hip and knee could affect patellofemoral joint contact patterns and stress (Fuchs, Schutte, and Witte, 1999; Huberti and Hayes, 1984; Lee et al., 1994; Powers et al., 2003; Ramappa et al., 2006; Salsich and Perman, 2007). Previous authors have described a link between the dynamic alignment of the lower limb and pain/pathology conditions (Earl and Vetter, 2007; Riegger-Krugh and Keysor, 1996; Sahrmann, 2002; Tiberio, 1987), and recently the term “medial collapse” has been used to describe a movement fault consisting of increased hip adduction, hip medial rotation and knee valgus during weightbearing (Powers, 2003). Components of medial collapse theoretically contribute to elevated joint stress and PFP because patellofemoral joint reaction forces are directed more laterally and patellofemoral contact area is reduced (Fuchs, Schutte, and Witte, 1999; Huberti and Hayes, 1984; Lee et al., 1994; Ramappa et al., 2006).
Several cadaver studies have supported the link between frontal and transverse plane movement of the femur and tibia and altered patellofemoral mechanics (Fuchs, Schutte, and Witte, 1999; Huberti and Hayes, 1984; Lee et al., 1994; Ramappa et al., 2006). Increased knee valgus has been linked to increased patellofemoral joint stress due to the resultant increase in quadriceps angle (Q-angle), which reflects the lateral component of the quadriceps muscle force. Huberti and Hays (Huberti and Hayes, 1984) reported that a 10° increase in Q-angle led to a 45% increase in patellofemoral contact stress when the knee was flexed to 20°, while Ramappa and colleagues (Ramappa et al., 2006) reported that increasing the Q-angle by 7.5° increased the mean patellofemoral contact stress by 15% and the stress borne by the lateral patellar facet by 41%. Lee and colleagues (Lee et al., 1994) and Fuchs, et al (Fuchs, Schutte, and Witte, 1999) reported that that medial rotation of the femur resulted in decreased patellofemoral joint contact area.
Two recent in vivo studies used MRI to investigate the relationship between transverse plane alignment of the lower extremity and patellofemoral mechanics (Powers et al., 2003; Salsich and Perman, 2007). Powers and colleagues (Powers et al., 2003) reported that during a single leg squat, abnormal patellofemoral alignment in subjects with patellar instability was due to medial rotation of the femur underneath the patella, and Salsich and Perman (Salsich and Perman, 2007) found that tibiofemoral rotation, defined as medial rotation of the femur relative to the tibia, was negatively correlated with patellofemoral joint contact area in individuals with PFP.
While the findings of the above-mentioned studies provide evidence of a relationship between the frontal and transverse plane alignment of the tibia and femur and patellofemoral joint contact area, the presence of medial collapse movement faults has not been established in individuals with PFP. Recent studies investigating components of medial collapse in individuals with PFP have produced conflicting results. Bolgla, et al (Bolgla, Malone, Umberger, and Uhl, 2008) reported no differences in average hip adduction, medial rotation or knee valgus angles during the stance phase of stair descent between groups of subjects with and without PFP. Conversely, Willson and Davis (Willson and Davis, 2008) reported increased hip adduction and decreased hip medial rotation during single leg squats, running and single leg jumps in subjects with PFP compared to controls. Based on these limited and controversial data, more investigation in this area is warranted.
The purpose of this study was to test the hypothesis that, compared to pain-free subjects, subjects with PFP would demonstrate increased hip adduction, hip medial rotation and knee valgus during the stance phase of free speed and fast speed walking. The identification of kinematic components of medial collapse in individuals with PFP could provide insight into the mechanism of pain development. Furthermore, knowledge of the specific kinematic faults could inform treatment strategies for this condition. For example, if increased hip adduction, hip medial rotation and knee valgus are identified in persons with PFP, treatments aimed at improving hip and femur control during weightbearing (e.g. hip muscle strengthening) might be warranted.
METHODS
Subjects
Male and female subjects between the ages of 18 and 40 were recruited as part of a larger study; however, for the purposes of the current study only female subjects were included based on reported differences in lower extremity kinematics between males and females (Chumanov, Wall-Scheffler, and Heiderscheit, 2008; Earl, Monteiro, and Snyder, 2007; Hewett et al., 2006) and reports of increased prevalence of PFP in females (DeHaven and Lintner, 1986; Taunton et al., 2002). Two groups of subjects participated. The PFP group consisted of 20 subjects (mean age: 25.6±6.8 yrs, height: 163.0±3.9 cm, body mass: 62.3±10.2 kg), and the pain-free group consisted of 20 subjects (mean age: 24.0±4.3 yrs, height: 165.7±6.7 cm, body mass: 66.1±13.2 kg). Groups were matched (mean values) on age, height, and body mass. Sample size was determined using pilot data generated from 4 subjects with PFP and 7 pain-free subjects. The original sample size was estimated for variables investigated in another study, however, a retrospective estimate was calculated from the same pilot data using the means and standard deviations for the hip and knee variables obtained in the current study. With a power = .80 and α = .05 (1-tailed) the number of subjects per group was estimated to be between 7 and 35.(Cohen, 1988) The higher subject number estimates correspond to the variables that had the most within-group variability (e.g. hip transverse plane angles).
Patellofemoral pain was defined as pain originating from the patellofemoral articulation that was readily reproducible with two of the following provocation tests: resisted quadriceps contraction, squatting, prolonged sitting, stair ascent or descent (McConnell, 1986). An additional inclusion criterion was a minimum pain duration of two months, to eliminate subjects who may have had pain develop from an isolated bout of intense activity. Patellar instability was not an exclusion criterion for the PFP group. Four subjects with PFP reported a history of patellar instability. The inclusion criterion for the pain-free group was current pain-free status of all lower extremity joints. Overall exclusion criteria for subjects in both groups were: a history (or current report) of knee ligament, tendon or cartilage injury, traumatic patellar dislocation, or prior knee surgery. Subjects were recruited from local universities, community centers, physicians’ offices, and word-of-mouth referrals. Approval for this study was granted from the Institutional Review Board at Saint Louis University. Written informed consent was obtained from all subjects and the rights of the subjects were protected.
Procedures
All procedures were carried out by the principal investigator (a physical therapist with 20 years of experience). Subjects with PFP underwent a clinical examination of the knee joint. Palpation was performed to rule out pain originating from associated structures (patellar tendon, quadriceps tendon, tibiofemoral joint and meniscii, synovial plicae). It is estimated that no more than 2 of the recruited subjects were excluded from the study based on this criterion. Subjects with PFP also completed a visual analog pain scale (VAS)(Carlsson, 1983) in response to the pain provocation tests to verify that the pain inclusion criterion (pain/no pain) was met. The VAS was a 100 mm horizontal line with left and right anchors representing “no pain” and “worst imaginable pain”, respectively. The VAS has been shown to be a valid measure for detecting clinical change in individuals with PFP (Chesworth, Culham, Tata, and Peat, 1989). Subjects marked the point on the line that corresponded to their pain level during the provocation tests. VAS scores were computed by measuring the length of the line from the left anchor to the subject’s mark in millimeters.
To obtain the hip and knee joint angles of interest, 3-dimensional motion analysis was performed using a 6-camera motion analysis system (Vicon, Los Angeles, CA). Kinematic data were sampled at 120 Hz. Foot contact and toe-off events were determined using a force platform (Kistler Instrument Corp, Amherst, NY) with a sampling rate of 1080 Hz. For each subject, anthropometric measurements were taken including height, body mass, bilateral knee width and ankle width (measured with calipers), and bilateral leg length (measured with a cloth tape measure). Reflective spherical markers (14mm) were taped to the skin of the lower extremities using a Helen Hayes marker set. The markers were placed bilaterally on the anterior superior iliac spines (ASIS), posterior superior iliac spines (PSIS), lateral thighs, lateral femoral epicondyles, lateral shanks, lateral malleoli, calcanei, and the dorsal surface of the 2nd metatarsals. The thigh and shank markers were mounted on 2-inch wands in order to assist with visualizing the frontal planes of the thigh and shank segments. All wand markers were secured with Coban® self-adherent elastic wrap (Sammons Preston, Bolingbrook, IL). Two additional spherical markers were taped to the medial femoral condyles for calibration of the standing trial only. Care was taken to align the femoral epicondylar markers to approximate the knee flexion/extension axis. The location of the epicondylar markers was visually confirmed by having the subject flex and extend the knee for several repetitions. Upon completion of the marker application a static standing trial was collected. Next, subjects performed two walking tasks, free speed walking (walking at a self-selected, usual walking pace) and fast speed walking (walking at a self-selected, fast walking pace). The order of the tasks was randomized and subjects were allowed several practice trials to adopt a consistent, comfortable walking pattern. Three trials of each task were recorded, after which subjects completed a VAS to indicate their pain level during each task.
Following data acquisition, gaps in marker trajectories were filled by fitting the data with a cubic spline. Next a quintic spline smoothing algorithm was applied, using a mean square error of 20. Three dimensional hip and knee joint angles were calculated using the Plug-in-Gait model (Vicon, Los Angeles, CA). To determine a time point of maximal patellofemoral joint loading, the internal knee extensor moment was calculated using inverse dynamics equations, also from the Plug-in-Gait model. The angle vs. time and moment vs. time curves were expressed as a percentage of the gait cycle. For each subject, variables used for analysis were obtained from each trial and averaged across the three trials. The selected variables were hip frontal and transverse plane angles and knee frontal plane angles at two discreet time points relevant to patellofemoral joint mechanics: peak knee extensor moment (PkMOM), and maximum knee extension/hyperextension angle (MxExt). The peak knee extensor moment (~12% of the gait cycle) corresponds to a point of increased patellofemoral joint reaction forces, and the maximum knee extension/hyperextension angle (~38% of the gait cycle) has relevance for abnormal patellar alignment, as the patella has minimal bony stability when the knee is fully extended. Maximum knee extension also has relevance for tibiofemoral rotation alignment, as the femur would likely be maximally medially rotated relative to the tibia due to the screw-home mechanism {Neumann, 2002 #270}. As such, kinematics at both time points could be altered in individuals with PFP.
Reliability of the gait variables was determined on a sample of 7 subjects who underwent testing on two occasions. Between-day intrarater reliability was calculated using the intraclass correlation coefficient (ICC(3,3)). ICC(3,3) values ranged from .74 to .98 for hip and knee frontal plane variables during free speed walking and from .74 to .97 during fast speed walking (Table 1). Reliability of hip transverse plane variables was poor for both walking conditions, as evidenced by low or negative ICCs (Table 1). Examination of the hip rotation data revealed a limited range of values, a small mean and a large standard deviation across subjects. The standard error of measurement (SEM) was calculated for all variables with non-negative ICCs (SEM = SD × √(1-ICC(3,3)), where SD is the pooled standard deviation of the measures across both days (Portney and Watkins, 2000)).
Table 1.
Reliability of Kinematic Variables
| Free Speed | Fast Speed | |||
|---|---|---|---|---|
| ICC*(3,3) | SEM§ (°) | ICC(3,3) | SEM (°) | |
| Hip Frontal Plane Angle at PkMOM | .80 | 0.8 | .81 | 1.1 |
| Hip Frontal Plane Angle at MxExt | .74 | 1.0 | .82 | 1.0 |
| Hip Transverse Plane Angle at PkMOM | .51 | 3.1 | .38 | 4.2 |
| Hip Transverse Plane Angle at MxExt | −.36 | NC | .24 | 3.5 |
| Knee Frontal Plane Angle at PkMOM | .90 | 1.0 | .74 | 1.2 |
| Knee Frontal Plane Angle at MxExt | .98 | 0.5 | .97 | 0.6 |
Intraclass Correlation Coefficient
Standard Error of the Measurement = SD * √(1-ICC(3,3)), where SD is the pooled standard deviation of measurements on day 1 and day 2
PkMOM = peak knee extensor moment
MxExt = peak knee extension/hyperextension angle
NC = Not calculated due to uninterpretable ICC
Walking speed was calculated automatically based on the stride characteristics obtained during the gait trials. Average walking speed was computed across the 3 trials for each walking condition.
Data Analysis
All statistical analyses were performed using SPSS software (version 13, SPSS, Inc., Chicago, IL). In the PFP group, descriptive statistics were computed for VAS scores during free speed and fast speed walking. Group differences were assessed using independent Student’s t-tests in order to accommodate directional hypothesis testing (Hays, 1994). For all variables, t-tests were computed separately for free speed and fast speed walking. T-tests were used instead of analysis of variance because the between-task comparison was not of interest and the ANOVA does not allow directional hypothesis testing (Hays, 1994). Significance levels were set at .05, 1-tailed for the direction hypothesized. If differences were observed opposite to the hypothesized direction the 2-tailed alpha level was used.
After examining the data, a subgroup of 4 PFP subjects were observed to have notably more pain during the walking tasks than the rest of the PFP group. As such, the analysis procedures were repeated comparing this subgroup of 4 PFP subjects to the pain-free group of 20 subjects.
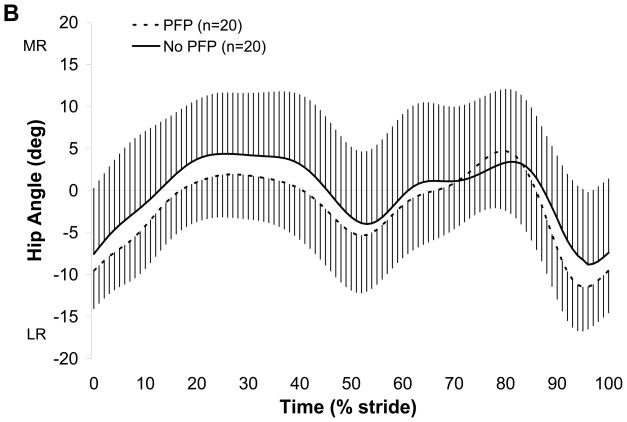
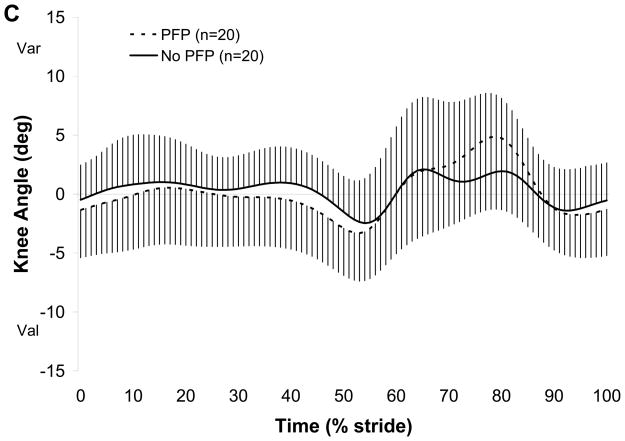
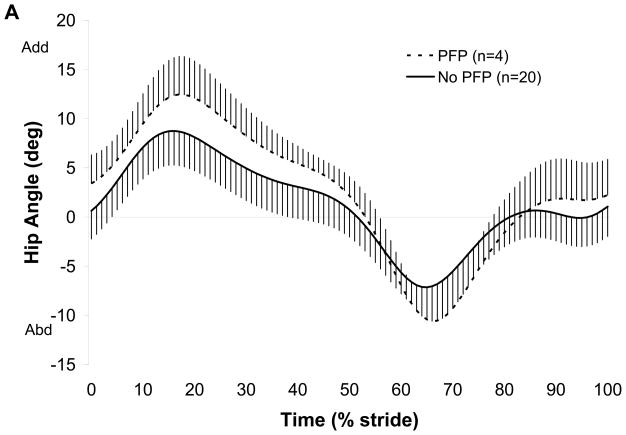
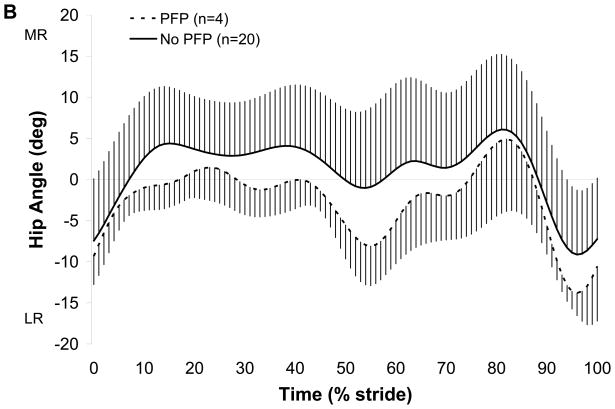
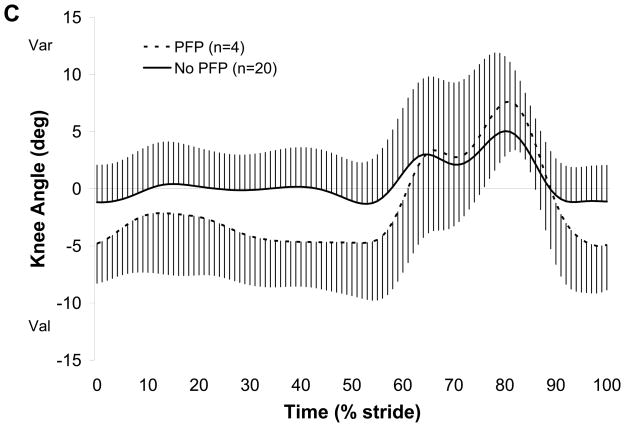
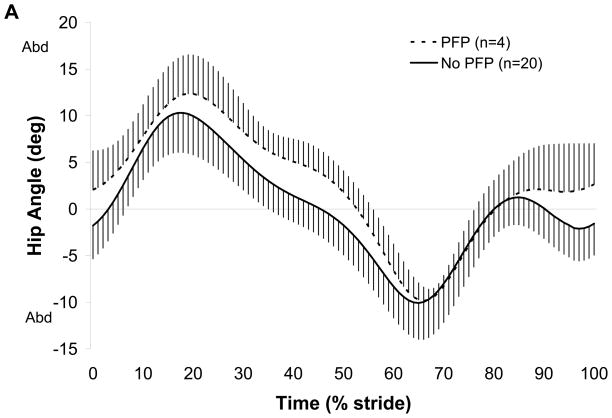
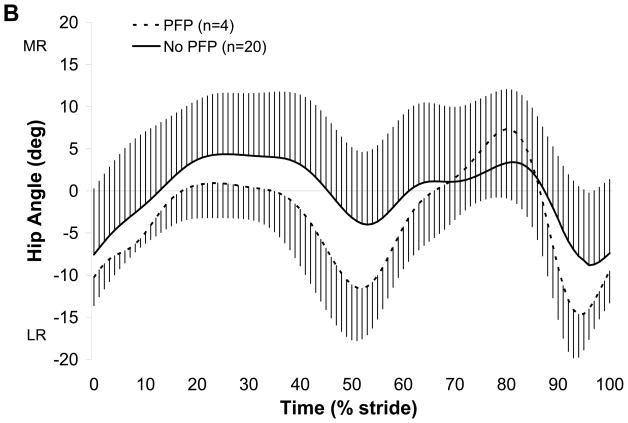
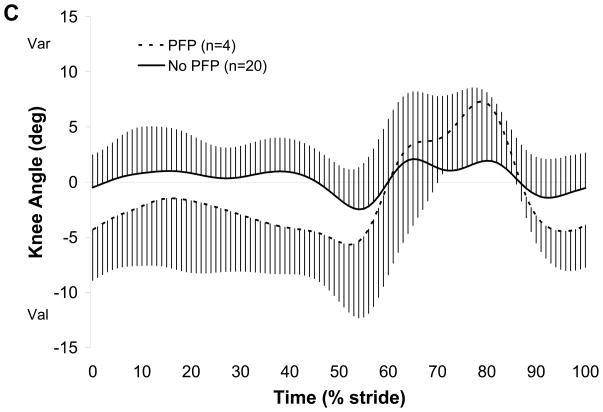
RESULTS
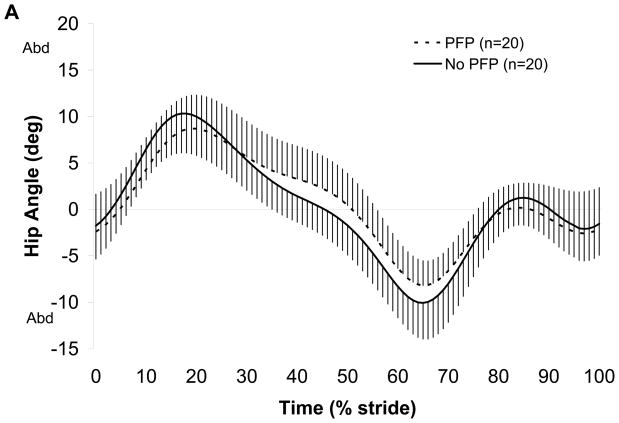
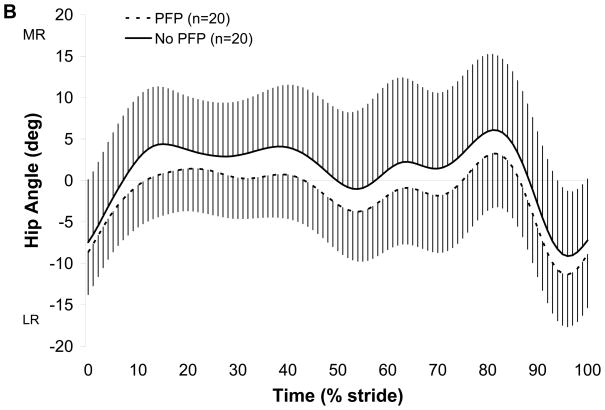
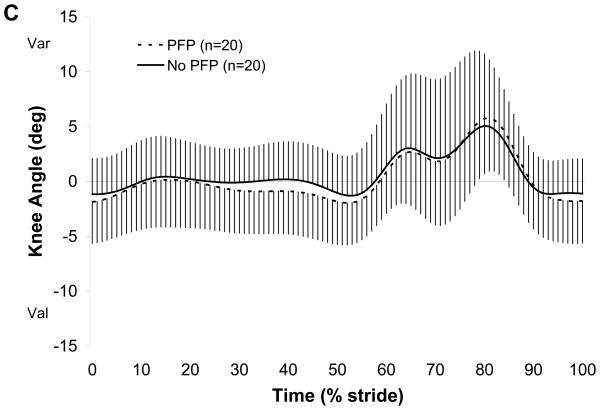
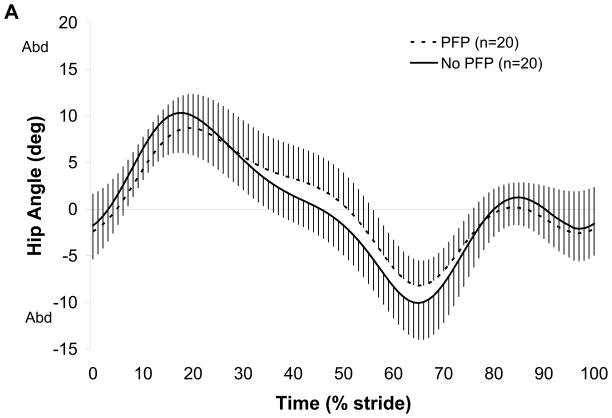
The average VAS score for the entire PFP group (n=20) was 9.0±16.6 during free speed walking and 14.2±18.0 during fast speed walking, however in the subgroup of 4 PFP subjects, the average VAS score was 40.8±7.5 during free walking and 44.5±5.3 during fast walking. The remaining 16 PFP subjects had an average VAS of 1.1±1.6 during free walking and 6.6±9.8 during fast walking. There were no group differences in any of the kinematic variables during free speed walking (Table 2, Fig. 1). During fast speed walking, subjects with PFP demonstrated less hip adduction at PkMOM and greater hip adduction at MxExt compared to control subjects (Table 3, Fig. 2). When the subgroup of 4 PFP subjects was compared to the pain-free group, the PFP subjects demonstrated greater hip adduction at PkMOM (p=.06) and greater knee valgus at MxExt during free speed walking (Table 4, Fig. 3). During fast speed walking, the subgroup of 4 PFP subjects had greater hip adduction at MxExt and greater knee valgus at MxExt (Table 5, Fig 4). Hip rotation at either time point was not different between groups during free or fast speed walking. Walking speed was not different between groups for either walking condition (Tables 2–5).
TABLE 2.
Group Comparisons - Free Speed Walk
| PFP Group (n=20) | Pain-free Group (n=20) | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p value | |
| Hip Frontal Plane Angle§ at PkMOM (°) | 6.3 (3.4) | 7.5 (4.0) | .32# |
| Hip Frontal Plane Angle at MxExt (°) | 4.0 (3.1) | 3.4 (3.4) | .29* |
| Hip Transverse Plane Angle‡ at PkMOM (°) | −0.6 (4.9) | 2.8 (6.6) | .08# |
| Hip Transverse Plane Angle at MxExt (°) | −0.7 (5.1) | 3.6 (6.7) | .14# |
| Knee Frontal Plane Angle§ at PkMOM (°) | −0.3 (4.1) | 0.1 (3.7) | .39* |
| Knee Frontal Plane Angle at MxExt (°) | −0.9 (3.9) | 0.3 (3.4) | .17* |
| Walking Speed (m/sec) | 1.3 (0.2) | 1.3 (0.1) | >.99# |
1 tailed
2 tailed
Positive values are adduction/varus, negative values are abduction/valgus
Positive values are medial rotation, negative values are lateral rotation
PkMOM = peak knee extensor moment
MxExt = peak knee extension/hyperextension angle
FIGURE 1.
Ensemble averaged kinematic curves for free speed walking. A: Hip frontal plane angle, B: Hip transverse plane angle, C: Knee frontal plane angle. Time axis is expressed as a percentage of one stride. Thick lines represent the mean of n subjects; vertical error bars represent one standard deviation. Abd=abduction, Add=adduction, MR=medial rotation, LR=lateral rotation, Var=varus, Val=valgus. No group differences were detected.
TABLE 3.
Group Comparisons - Fast Speed Walk
| PFP Group (n=20) | Pain-free Group (n=20) | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p value | |
| Hip Frontal Plane Angle§ at PkMOM (°) | 4.8 (3.5) | 7.1 (3.8) | .05# |
| Hip Frontal Plane Angle at MxExt (°) | 3.4 (3.6) | 1.6 (2.8) | .04* |
| Hip Transverse Plane Angle‡ at PkMOM (°) | −3.5 (5.0) | −0.9 (7.6) | .22# |
| Hip Transverse Plane Angle at MxExt (°) | 0.5 (5.8) | 2.9 (7.8) | .28# |
| Knee Frontal Plane Angle§ at PkMOM (°) | 0.2 (4.5) | 0.9 (4.1) | .30* |
| Knee Frontal Plane Angle at MxExt (°) | −0.2 (3.9) | 1.0 (3.0) | .13* |
| Walking Speed (m/sec) | 2.0 (0.3) | 2.0 (0.3) | .98# |
1 tailed
2 tailed
Positive values are adduction/varus, negative values are abduction/valgus
Positive values are medial rotation, negative values are lateral rotation
PkMOM = peak knee extensor moment
MxExt = peak knee extension/hyperextension angle
FIGURE 2.
Ensemble averaged kinematic curves for fast speed walking. A: Hip frontal plane angle, B: Hip transverse plane angle, C: Knee frontal plane angle. Time axis is expressed as a percentage of one stride. Thick lines represent the mean of n subjects; vertical error bars represent one standard deviation. Abd=abduction, Add=adduction, MR=medial rotation, LR=lateral rotation, Var=varus, Val=valgus. *indicates hip adduction at PkMOM was less in the PFP group (p=.05) and hip adduction at MxExt was greater in the PFP group (p = .04).
TABLE 4.
Subgroup Comparisons - Free Speed Walk
| PFP Group (n=4) | Pain-free Group (n=20) | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p value | |
| Hip Frontal Plane Angle§-PkMOM (°) | 10.8 (3.5) | 7.5 (4.0) | .06* |
| Hip Frontal Plane Angle-MxExt (°) | 5.6 (1.3) | 3.4 (3.4) | .11* |
| Hip Transverse Plane Angle‡-PkMOM (°) | −0.9 (3.1) | 2.8 (6.6) | .30# |
| Hip Transverse Plane Angle-MxExt (°) | −0.7 (3.6) | 3.6 (6.7) | .24# |
| Knee Frontal Plane Angle§-PkMOM (°) | −2.2 (5.2) | 0.1 (3.7) | .15* |
| Knee Frontal Plane Angle-MxExt (°) | −4.7 (4.0) | 0.3 (3.4) | .01* |
| Walking Speed (m/sec) | 1.4 (0.2) | 1.3 (0.1) | .40# |
1 tailed
2 tailed
Positive values are adduction/varus, negative values are abduction/valgus
Positive values are medial rotation, negative values are lateral rotation
PkMOM=time of peak knee extensor moment
MxExt=time of peak knee extension/hyperextension angle
FIGURE 3. Subgroup analysis.
Ensemble averaged kinematic curves for free speed walking. A: Hip frontal plane angle, B: Hip transverse plane angle, C: Knee frontal plane angle. Time axis is expressed as a percentage of one stride. Thick lines represent the mean of n subjects; vertical error bars represent one standard deviation. Abd=abduction, Add=adduction, MR=medial rotation, LR=lateral rotation, Var=varus, Val=valgus. *indicates hip adduction at PkMOM and knee valgus at MxExt were greater in the PFP group, p <.05.
TABLE 5.
Subgroup Comparisons - Fast Speed Walk
| PFP Group (n=4) | Pain-free Group (n=20) | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p value | |
| Hip Frontal Plane Angle§-PkMOM (°) | 8.5 (3.9) | 7.1 (3.8) | .25* |
| Hip Frontal Plane Angle-MxExt (°) | 5.3 (2.2) | 1.6 (2.8) | .01* |
| Hip Transverse Plane Angle‡-PkMOM (°) | −2.0 (3.3) | −0.9 (7.6) | .78# |
| Hip Transverse Plane Angle-MxExt (°) | −2.9(7.2) | 2.9 (7.8) | .18# |
| Knee Frontal Plane Angle§-PkMOM (°) | −1.0 (5.4) | 0.9 (4.1) | .22* |
| Knee Frontal Plane Angle-MxExt (°) | −3.3 (3.2) | 1.0 (3.0) | .008* |
| Walking Speed (m/sec) | 1.8 (0.3) | 2.0 (0.3) | .16 # |
1 tailed
2 tailed
Positive values are adduction/varus, negative values are abduction/valgus
Positive values are medial rotation, negative values are lateral rotation
PkMOM=time of peak knee extensor moment
MxExt=time of peak knee extension/hyperextension angle
FIGURE 4. Subgroup analysis.
Ensemble averaged kinematic curves for fast speed walking. A: Hip frontal plane angle, B: Hip transverse plane angle, C: Knee frontal plane angle. Time axis is expressed as a percentage of one stride. Thick lines represent the mean of n subjects; vertical error bars represent one standard deviation. Abd=abduction, Add=adduction, MR=medial rotation, LR=lateral rotation, Var=varus, Val=valgus. *indicates hip adduction and knee valgus at MxExt were greater in the PFP group, p <.05.
DISCUSSION
When the entire group of PFP subjects was compared to the pain-free group, there were no differences in hip or knee kinematics during free speed walking, indicating that individuals with PFP did not demonstrate medial collapse during weightbearing. While this finding was contrary to our hypothesis, it agrees with the findings of Bolgla and colleagues (Bolgla, Malone, Umberger, and Uhl, 2008) who reported no differences in average hip adduction, hip medial rotation or knee valgus angles during the stance phase of stair descent between groups of individuals with and without PFP. The authors attribute this finding to the low-level nature of the task, suggesting that a more demanding task might have resulted in group differences. Similarly, the task of free speed walking likely places relatively minimal demand on the lower extremity. The average pain level of the PFP group in the current study was less than 10 (out of 100) during free speed walking, and as such, subjects probably were able to maintain normal hip and knee kinematics during this low-level task.
The finding of less hip adduction at PkMOM during fast walking was surprising and contrary to our hypothesis, however one possible explanation was that subjects with PFP were attempting to minimize the demand on the patellofemoral joint at a point in the gait cycle where patellofemoral joint reaction forces are relatively high (PkMOM). Although in a different plane, such a compensatory pattern is consistent with the findings of Willson and Davis (Willson and Davis, 2008) who reported decreased hip medial rotation during single leg squats, running and single leg jumps in female subjects with PFP compared to controls. It is possible that as the demand of the task increased with fast walking, the subjects with PFP attempted to avoid medial collapse by minimizing hip adduction during early stance.
During fast speed walking, subjects with PFP had greater hip adduction motion at MxExt compared to pain-free subjects. This finding supports those of Willson and Davis (Willson and Davis, 2008) who examined hip and knee kinematics in individuals with PFP across a variety of tasks. The authors reported greater hip adduction angles at discreet time points during the stance phase of single limb squatting, running and jumping in subjects with PFP compared to pain-free subjects. Our finding of greater hip adduction at MxExt during fast speed walking, but not during free speed walking, suggests that as the demands of the task increased, subjects with PFP had a diminished ability to control the hip in the frontal plane during late stance. This finding is in contrast, however, to those of Bolgla and colleagues (Bolgla, Malone, Umberger, and Uhl, 2008). One reason for this discrepancy could be that the stair descent task used in the study by Bolga et al is less “demanding” than fast walking. While knee extensor moments during stair descent are reportedly greater than during walking (Luepongsak et al., 2002), and thus should place greater demands on the patellofemoral joint due to increased reaction forces, the speed of the activity may be another important factor influencing joint mechanics. As walking speed increases, muscle activation (amplitude) increases (Winter, 1983) in response to increased body segment accelerations. Perhaps the subjects with PFP were not able to respond to the greater segmental accelerations present during fast walking, resulting in a diminished ability to control the hip in the frontal plane during late stance.
When the subgroup of 4 PFP subjects was compared to the pain-free group, more components of medial collapse were observed, namely, greater hip adduction during early stance and greater knee valgus during late stance of free speed walking, and greater hip adduction and knee valgus during late stance of fast speed walking. These findings suggest that medial collapse movement faults may be more evident in people with greater symptom severity. All 4 subjects in the PFP subgroup had VAS levels greater than 30 during the low-level tasks of free and fast walking, which was in contrast to the remainder of the PFP subjects whose average pain levels were 1.1 and 6.6 during free and fast speed walking, respectively. The lack of difference in hip adduction at PkMOM during fast walking is contrary to the finding at this time point when the whole PFP group was analyzed (less hip adduction in the PFP group) suggesting that the subgroup of painful subjects might not have been able to compensate in the frontal plane by reducing hip adduction during early stance.
Although one cannot infer causation from the results of this study, as the design was cross-sectional in nature, the data support the proposed mechanism of medial collapse in the development of PFP, at least in the frontal plane. These results should be interpreted with caution, however, as the subgroup analysis was performed a posteriori and the sample size was notably small. Furthermore the mean differences in hip adduction and knee valgus variables, although statistically significant, were relatively small, raising the question of clinical significance. Examining the SEMs, however, revealed that all significant differences were greater than the SEMs for the respective variables. In fact, the mean differences noted in the subgroup analysis were more than 3 times greater than the SEMs. As such, the data suggest that future studies should investigate whether symptom behavior can assist in classifying individuals with PFP. Future studies also should address whether or not medial collapse movement faults, when identified, can be corrected and if correction of the faults results in decreased pain.
Poor frontal plane control of the hip could be due to impaired muscle performance of the hip abductors, as has been postulated (Powers, 2003), and several investigators have reported diminished strength of hip abductor muscles in individuals with PFP (Bolgla, Malone, Umberger, and Uhl, 2008; Ireland, Willson, Ballantyne, and Davis, 2003; Mascal, Landel, and Powers, 2003). Future studies should investigate the relationship between hip muscle performance and kinematics during gait. If such a relationship is identified, treatments aimed at improving hip muscle performance impairments might be warranted.
Contrary to the proposed hypothesis, there were no group differences in hip rotation at either time point for either task, a finding that remained even upon analysis of the subgroup. This corresponds to the findings of Bolgla et al (Bolgla, Malone, Umberger, and Uhl, 2008) who reported no differences in hip transverse plane kinematics during stair descent. One reason for the lack of difference in hip rotation may be that the amount of transverse plane hip motion present during gait is inherently small. Furthermore, for the hip rotation variables calculated, the ratio of the standard deviation to the mean for both groups during free and fast speed walking was very large (greater than 1) and the reliability coefficients were small or uninterpretable. With such a poor “signal to noise ratio,” detection of small differences in hip rotation motion would be unlikely, especially in a sample of this size. Interestingly, the data, although not significant, were in the direction of less medial rotation in the PFP group, which supports the findings of Willson and Davis (Willson and Davis, 2008) who suggested that subjects with PFP might have been compensating for pain (avoiding medial collapse) in the transverse plane.
While this study provides insight into factors contributing to PFP, there are several limitations to acknowledge. The first pertains to the cross-sectional nature of the study which limits causal inferences. It is possible that the kinematic faults observed in the subgroup of individuals with PFP were the result, not the cause, of the pain. Future studies should investigate prospectively whether directional relationships between kinematics and pain are present. The second limitation is related to the study sample. The PFP group had very few subjects with notable symptoms during the tasks, resulting in a subgroup analysis with a small sample size (n=4). As such, the results should be interpreted with caution as stated previously. Future studies should attempt to recruit larger samples of subjects across a spectrum of pain levels. The third limitation pertains to the motion analysis procedures. The lower extremity model involved the use of surface markers placed directly on the skin. Such models are subject to error from skin motion artifact (Benoit et al., 2006; Manal et al., 2000) which may have contributed to the variability in the hip transverse plane kinematics. Future studies should employ models that use marker sets comprised of rigid clusters to improve the accuracy of transverse plane kinematics.
CONCLUSION
Compared to pain-free subjects, subjects with PFP had less hip adduction during the early stance phase and greater hip adduction during the late stance phase of fast walking. A subgroup of 4 PFP subjects with greater symptom severity displayed additional characteristics of medial collapse, namely, greater hip adduction during early stance and greater knee valgus during late stance of free speed walking, and greater hip adduction and knee valgus during late stance of fast speed walking. Symptom behavior may play an important role in identifying frontal plane medial collapse movement faults in individuals with PFP.
Acknowledgments
This study was funded in part by the National Center for Medical Rehabilitation Research, National Institute of Child Health and Human Development, K01-HD043352.
The authors would like to thank the study participants who gave their time and effort in support of this research. We also acknowledge our source of funding for conduction and dissemination of this research (National Center for Medical Rehabilitation Research, National Institute of Child Health and Human Development, K01-HD043352).
Footnotes
Conflict of Interest
The authors have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript.
References
- Benoit DL, Ramsey DK, Lamontagne M, Xu L, Wretenberg P, Renstrom P. Effect of skin movement artifact on knee kinematics during gait and cutting motions measured in vivo. Gait & Posture. 2006;24:152–164. doi: 10.1016/j.gaitpost.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Bolgla LA, Malone TR, Umberger BR, Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. Journal of Orthopaedic & Sports Physical Therapy. 2008;38:12–18. doi: 10.2519/jospt.2008.2462. [DOI] [PubMed] [Google Scholar]
- Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- Chesworth BM, Culham EG, Tata GE, Peat M. Validation of outcome measures in patients with patellofemoral syndrome. Journal of Orthopaedic & Sports Physical Therapy. 1989;10:302–308. doi: 10.2519/jospt.1989.10.8.302. [DOI] [PubMed] [Google Scholar]
- Chumanov ES, Wall-Scheffler C, Heiderscheit BC. Gender differences in walking and running on level and inclined surfaces. Clinical Biomechanics. 2008;23:1260–1268. doi: 10.1016/j.clinbiomech.2008.07.011. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates, Inc; 1988. [Google Scholar]
- DeHaven KE, Lintner DM. Athletic injuries: Comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–224. doi: 10.1177/036354658601400307. [DOI] [PubMed] [Google Scholar]
- Earl JE, Monteiro SK, Snyder KR. Differences in lower extremity kinematics between a bilateral drop-vertical jump and a single-leg step-down. Journal of Orthopaedic & Sports Physical Therapy. 2007;37:245–252. doi: 10.2519/jospt.2007.2202. [DOI] [PubMed] [Google Scholar]
- Earl JE, Vetter CS. Patellofemoral pain. Physical Medicine and Rehabilitation Clinics of North America. 2007;18:439–458. doi: 10.1016/j.pmr.2007.05.004. [DOI] [PubMed] [Google Scholar]
- Fuchs S, Schutte G, Witte H. Effect of knee joint flexion and femur rotation on retropatellar contact of the human knee joint. Biomedizinische Technik. Biomedical Engineering. 1999;44:334–338. [PubMed] [Google Scholar]
- Goodfellow J, Hungerford DS, Woods C. Patello-femoral joint mechanics and pathology. 2. Chondromalacia patellae. Journal of Bone and Joint Surgery -- British Volume. 1976;58:291–299. doi: 10.1302/0301-620X.58B3.956244. [DOI] [PubMed] [Google Scholar]
- Grady EP, Carpenter MT, Koenig CD, Older SA, Battafarano DF. Rheumatic findings in gulf war veterans. Archives of Internal Medicine. 1998;158:367–371. doi: 10.1001/archinte.158.4.367. [DOI] [PubMed] [Google Scholar]
- Grana WA, Kriegshauser LA. Scientific basis of extensor mechanism disorders. Clinics in Sports Medicine. 1985;4:247–257. [PubMed] [Google Scholar]
- Hays WL. Statistics. 5. Fort Worth, TX: Harcourt Brace College Publishers; 1994. [Google Scholar]
- Hewett TE, Ford KR, Myer GD, Wanstrath K, Scheper M. Gender differences in hip adduction motion and torque during a single-leg agility maneuver. Journal of Orthopaedic Research. 2006;24:416–421. doi: 10.1002/jor.20056. [DOI] [PubMed] [Google Scholar]
- Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. Journal of Bone and Joint Surgery -- American Volume. 1984;66:715–724. [PubMed] [Google Scholar]
- Hungerford DS, Lennox DW. Rehabilitation of the knee in disorders of the patellofemoral joint: Relevant biomechanics. The Orthopaedic Clinics of North America. 1983;14:397–402. [PubMed] [Google Scholar]
- Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. Journal of Orthopaedic & Sports Physical Therapy. 2003;33:671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- Kannus PA. Long patellar tendon: Radiographic sign of patellofemoral pain syndrome--a prospective study. Radiology. 1992;185:859–863. doi: 10.1148/radiology.185.3.1438776. [DOI] [PubMed] [Google Scholar]
- Laprade J, Culham E. Radiographic measures in subjects who are asymptomatic and subjects with patellofemoral pain syndrome. Clinical Orthopaedics and Related Research. 2003:172–182. doi: 10.1097/01.blo.0000079269.91782.f5. [DOI] [PubMed] [Google Scholar]
- Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clinical Orthopaedics and Related Research. 1994:69–74. [PubMed] [Google Scholar]
- Luepongsak N, Amin S, Krebs DE, McGibbon CA, Felson D. The contribution of type of daily activity to loading across the hip and knee joints in the elderly. Osteoarthritis and Cartilage. 2002;10:353–359. doi: 10.1053/joca.2000.0511. [DOI] [PubMed] [Google Scholar]
- Macintyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. Journal of Bone and Joint Surgery -- American Volume. 2006;88:2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- Manal K, McClay I, Stanhope S, Richards J, Galinat B. Comparison of surface mounted markers and attachment methods in estimating tibial rotations during walking: An in vivo study. Gait Posture. 2000;11:38–45. doi: 10.1016/s0966-6362(99)00042-9. [DOI] [PubMed] [Google Scholar]
- Mascal CL, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. Journal of Orthopaedic & Sports Physical Therapy. 2003;33:647–660. doi: 10.2519/jospt.2003.33.11.647. [DOI] [PubMed] [Google Scholar]
- McConnell J. The management of chondromalacia patellae: A long term solution. Australian Journal of Physiotherapy. 1986;32:215–223. doi: 10.1016/S0004-9514(14)60654-1. [DOI] [PubMed] [Google Scholar]
- Outerbridge RE, Dunlop JA. The problem of chondromalacia patellae. Clinical Orthopaedics and Related Research. 1975:177–196. doi: 10.1097/00003086-197507000-00024. [DOI] [PubMed] [Google Scholar]
- Portney LG, Watkins MP. Foundations of clinical research -- applications to practice. 2. Upper Saddle River, NJ: Prentice-Hall, Inc; 2000. [Google Scholar]
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. Journal of Orthopaedic & Sports Physical Therapy. 2003;33:639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- Powers CM, Ward SR, Fredericson M, Guillet M, Shellock FG. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: A preliminary study. Journal of Orthopaedic & Sports Physical Therapy. 2003;33:677–685. doi: 10.2519/jospt.2003.33.11.677. [DOI] [PubMed] [Google Scholar]
- Ramappa AJ, Apreleva M, Harrold FR, Fitzgibbons PG, Wilson DR, Gill TJ. The effects of medialization and anteromedialization of the tibial tubercle on patellofemoral mechanics and kinematics. American Journal of Sports Medicine. 2006;34:749–756. doi: 10.1177/0363546505283460. [DOI] [PubMed] [Google Scholar]
- Riegger-Krugh C, Keysor JJ. Skeletal malalignments of the lower quarter: Correlated and compensatory motions and postures. Journal of Orthopaedic & Sports Physical Therapy. 1996;23:164–170. doi: 10.2519/jospt.1996.23.2.164. [DOI] [PubMed] [Google Scholar]
- Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. St. Louis, MO: Mosby, Inc; 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salsich GB, Perman WH. Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. Journal of Orthopaedic & Sports Physical Therapy. 2007;37:521–528. doi: 10.2519/jospt.2007.37.9.521. [DOI] [PubMed] [Google Scholar]
- Sanchis-Alfonso V, Rosello-Sastre E, Martinez-Sanjuan V. Pathogenesis of anterior knee pain syndrome and functional patellofemoral instability in the active young. The American Journal of Knee Surgery. 1999;12:29–40. [PubMed] [Google Scholar]
- Seedhom BB, Takeda T, Tsubuku M, Wright V. Mechanical factors and patellofemoral osteoarthrosis. Annals of Rheumatic Diseases. 1979;38:307–316. doi: 10.1136/ard.38.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. British Journal of Sports Medicine. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomee R, Renstrom P, Karlsson J, Grimby G. Patellofemoral pain syndrome in young women. I. A clinical analysis of alignment, pain parameters, common symptoms and functional activity level. Scandinavian Journal of Medicine & Science in Sports. 1995;5:237–244. [PubMed] [Google Scholar]
- Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. Journal of Orthopaedic & Sports Physical Therapy. 1987;9:160–165. doi: 10.2519/jospt.1987.9.4.160. [DOI] [PubMed] [Google Scholar]
- Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clinical Biomechanics. 2008;23:203–211. doi: 10.1016/j.clinbiomech.2007.08.025. [DOI] [PubMed] [Google Scholar]
- Winter DA. Biomechanical motor patterns in normal walking. Journal of Motor Behavior. 1983;15:302–330. doi: 10.1080/00222895.1983.10735302. [DOI] [PubMed] [Google Scholar]