Abstract
Health care–associated infections (HAIs) are common and costly patient safety problems that are largely preventable. As a result, numerous policy changes have recently taken place including mandatory reporting and lack of reimbursement for HAIs. A qualitative approach was used to obtain dense description and gain insights about the current practice of infection prevention in California. Twenty-three in-depth, semistructured interviews were conducted at six acute care hospitals. Content analysis revealed 4 major interconnected themes: (a) impacts of mandatory reporting; (b) impacts of technology on HAI surveillance; (c) infection preventionists’ role expansion; and (d) impacts of organizational climate. Personnel reported that interdisciplinary collaboration was a major facilitator for implementing effective infection prevention, and organizational climate promoting a shared accountability is urgently needed. Mandatory reporting requirements are having both intended and unintended consequences on HAI prevention. More research is needed to measure the long-term effects of these important changes in policy.
Keywords: health care quality, nursing/health care workforce issues, patient safety, state legislation
Health care–associated infections (HAIs) are common, costly patient safety problems. Each year, HAIs affect approximately 1.7 million patients, lead to 4.5 infections per 100 hospital admissions, and are associated with 99,000 deaths (Klevens et al., 2007). In 2007, the annual direct inpatient cost attributable to HAIs was estimated to range from US$28 billion to US$45 billion (Scott, 2009). Furthermore, HAIs are a largely preventable problem (Centers of Disease Control and Prevention, 2005; Pronovost et al., 2006). With the staggering attributable morbidity, mortality, and costs of this preventable problem, numerous initiatives and policy changes have recently taken place.
In 2005, as part of the Deficit Reduction Act (section 5001 (c)), the Secretary of Health and Human Services was required to identify high cost and high volume preventable conditions that result in higher Medicare hospital payments. As a result, beginning October 2008, Medicare no longer reimburses hospitals for treatment costs of certain preventable HAIs (Stone et al., 2010). In an effort to promote transparency and encourage hospitals to prioritize infection prevention, major policy changes have also occurred at the state level. As of June 1, 2009, 36 states reported to have some form of legislation or regulation regarding mandatory reporting (Stone et al., 2010). Many states now require hospitals to disclose their HAI rates to state health departments. Beginning January 2009, all general acute care hospitals in California were mandated to report select HAIs and process data related to HAI prevention to the State Department of Public Health, with further public reporting expected to follow in 2011 (California Department of Public Health, 2010).
An example of a private sector initiative is the California Healthcare-Associated Infection Prevention Initiative (CHAIPI) funded by the Blue Shield of California Foundation. In the fall of 2008, 49 California hospitals voluntarily participated in the CHAIPI quality-improvement collaborative. The collaborative was staffed by infection-prevention leaders from the Association for Professionals in Infection Control and Epidemiology, Inc. (APIC) and other nationally recognized organizations such as the Institute for Healthcare Improvement and the California Institute for Health Systems Performance. Webinars, face-to-face meetings, and sharing of best practices were conducted from the fall of 2008 and throughout 2009.
Limited research attention has focused on exploring the implications of these changes. As part of a larger evaluation of CHAIPI (Blue Shield of California Foundation, 2011), we visited participating hospitals and conducted qualitative in-depth interviews with various personnel. The purpose of qualitative research is to discover meaning and interpret experiences (Sandelowski, 2004). For this study, a qualitative approach was used to obtain dense description and gain insights about the experience of the current practice of infection prevention in California.
Method
In-depth, semistructured interviews were conducted at six general, acute care hospitals in California during the summer of 2009. A purposive sample of six hospitals was recruited to gain regional representation across the state. All hospitals participated in CHAIPI. In each hospital, a range of personnel that were involved in infection prevention and control were interviewed.
This qualitative study was informed by Donabedian's conceptual framework of health care quality. This theoretical framework defines three dimensions in quality care: structures, processes, and outcomes (Donabedian, 1992). Donabedian's framework is particularly applicable to understanding the influences in health care environments and how they impact care processes and outcomes. Thus, interview guides were framed around these three care dimensions. Specifically, participants were asked about the following areas related to infection prevention and control: (a) characteristics of the hospital (e.g., number of hospital beds) and the infection control department (e.g., staffing and organization of the department); (b) recent changes in processes as a result of the state mandatory reporting of HAIs and the ways in which policy changes occurred within their organizations; (c) utilization of the electronic surveillance systems (ESS) and its impact on the processes of care; and (d) what was working or not working in the prevention of HAIs. The interviews were audiotaped and typically lasted 1 hr. The study was approved by the Columbia University Medical Center's Institutional Review Board.
Data Analysis
The audiotaped interviews were transcribed verbatim. All personal identifiers were removed from the transcripts and each transcript was assigned a heading (role title) and number (hospital code). The transcripts were then entered into NVivo 8© (QSR International) software to facilitate the content analysis. An audit trail was also developed. Throughout the data analysis, the investigative team met biweekly with an expert qualitative researcher (VR) to discuss the ongoing coding and content analysis.
Two members of the research team (MU and LC) were the “coders” of the transcripts. To generate a comprehensive set of codes, prior to beginning the actual coding process, the coders worked independently reviewing the transcripts to establish a “general tone” and developed a set of topics of discourse present in the participants’ narrative accounts. Through joint discussion between themselves and the larger research team, these topics were merged and expanded on to develop an initial set of core and secondary codes. The core codes represented the larger context of the phenomena (i.e., mandatory reporting). The secondary codes served to further contextualize the phenomena and suggest underlying meaning (i.e., frustrations with mandates due to increased workload).
An iterative process of analysis then followed in which the coders reread and independently coded the same subset of four randomly selected interviews. There was general consensus in how both coders applied the initial coding scheme to these interviews, allowing the coders to code the additional transcripts separately. To maintain consistency throughout the coding process, 30% of the transcripts were double coded and isolated coding discrepancies were resolved at the coders’ weekly discussions. The interrater agreement was found to be excellent (exceeding 90%).
Results
Twenty-three in-depth interviews (22 one-on-one interviews and 1 interview with multiple personnel) were conducted with 25 hospital professionals. The interviewees included infection preventionists (IPs), infection control department directors (ICDs), hospital epidemiologists (HEs), hospital administrators (HAs), and ICU nurse managers (NMs). See Table 1 for breakdown of participants from each hospital.
Table 1.
Participation by Role Across Hospital Sites
| Participants (n = 25) | Hospital 1 | Hospital 2 | Hospital 3 | Hospital 4 | Hospital 5 | Hospital 6 | Total |
|---|---|---|---|---|---|---|---|
| Infection preventionist (IP) | 1 | 1 | 0 | 1 | 0 | 3 | 6 |
| Infection control director (ICD) | 1 | 0 | 1 | 0 | 1 | 1 | 4 |
| Hospital epidemiologist (HE) | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| ICU nurse manager (NM) | 1 | 1 | 1 | 1 | 1 | 2 | 7 |
| Hospital administrator (HA)a | 1 | 1 | 1 | 1 | 1 | 0 | 5 |
Note: ICU = intensive care unit.
Included chief nursing officers, director of quality and risk, and the like.
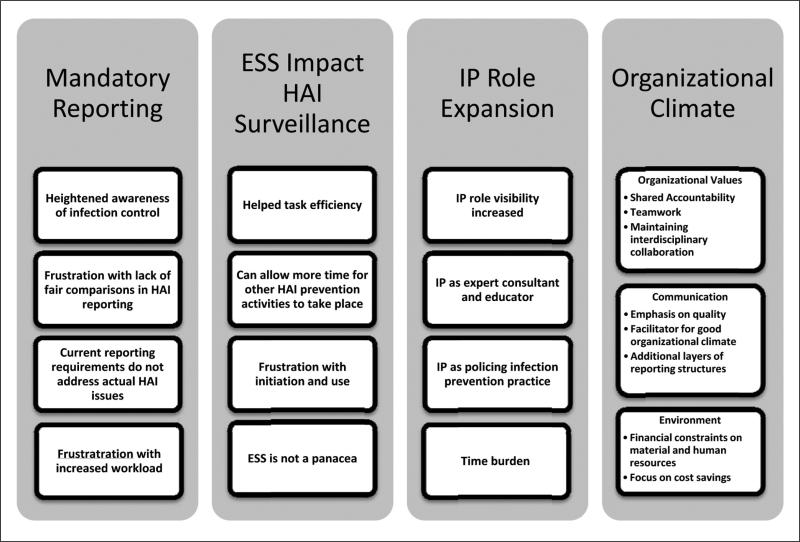
Analysis of the participants’ narrative accounts yielded 4 major themes related to the experience of infection control: (a) mandatory reporting/regulations, (b) impact of technology for HAI surveillance, (c) IP role expansion, and (d) organizational climate. Each of these themes has associated subthemes (Figure 1), which are described below with exemplar quotations provided.
Figure 1.
Emerging four major themes and subthemes from content analysis
Mandatory Reporting/Regulations
Not surprisingly, given the interview guide, the theme of mandatory reporting/regulations occurred in interviews from all settings. The related subthemes included positive and negative responses to the recent legislative changes. Among the beneficial consequences was an increased awareness in their organizations of infection control. As one ICU NM explained, mandatory regulations made a “small deal (into) a very big deal.” Many participants shared that the mandates helped facilitate obtaining resources for infection control: “Now that the mandate has come in, it actually has helped us to argue that that should go into the budget.”
However, strong opponents of mandatory regulations expressed a number of concerns including lack of comparability between hospitals and frustration. As one respondent stated,
Nationally, I'd like to see them (state and federal agencies) use the right metrics for the right definitions and really make comparisons meaningful. Even as . . . prescriptive (as) they try to be . . . interpretation at the local level can be widely divergent . . . it's fine for internal consistencies, but it's another thing if you want (statewide) report cards.
These accounts also reflected a level of frustration with current reporting requirements. For many, this frustration emanated from a belief that current reporting requirements do not address the actual HAI issues that are being encountered in their institution. As an IP shared,
So we're recording what the state wants us to record . . . we put policies and processes in place, but we're not seeing that (infection). . . . What we are seeing is that central line infections are much more prevalent and a problem for us . . . We want to be compliant, but it's not top of my infection priorities.
Infection control professionals also were experiencing frustration over the increased workload that these regulations imposed. As both a HE and a HA each explained,
I just want to take care of patients and now it's all different . . . I have to get it all documented . . . show documentation, show proof of compliance . . . it's a lot more work in proving you're doing the right thing.
Now there's layers and layers of regulatory reporting, documenting all the education and training. . . . (State) adds 15 levels of bureaucratic regulatory things that, guess what, costs money and takes people away from the real business of taking care of patients.
In relating the impact of mandatory regulations, some participants discussed the need to view both the benefits and detriments. The comments of one HA reflect such an attempt to present a balanced viewpoint: “A lot of regulations don't make sense, but overall I see it being a good thing . . . it's going to move us into a direction that we really want to move in.”
Impact of Technology for HAI Surveillance
The spread of health care information technology has made tremendous impacts on how HAIs are tracked and reported. The related subthemes that emerged include (a) efficiency, (b) increased time for other HAI prevention activities, (c) frustration with initiation and use, and (d) electronic surveil-lance system (ESS) is not a panacea. Although not all hospitals had ESS in place at the time their hospital personnel were interviewed, those who were using ESS reported that their daily surveillance tasks “just got a lot easier.” As one ICD related, “With the new ESS, we don't have to spend so much time on surveillance . . . It is easier to get the (surveil-lance) information . . .”
It was also noted that the reduction in time spent on surveillance should enable infection control specialists to allocate more time to important activities. The lack of time to provide staff education on relevant infection control issues was repeatedly reported in interviews and was a main concern of IPs. As one ICD shared, “I'd like to see us out more. Right now, we get tied an awful lot into data collection and going to meetings and not out to the bedside or the bedside nurses’ training.”
Although there was widespread acknowledgement of the benefits of ESS, it was also noted that initiating and maintaining ESS in hospitals can be a challenge. One IP shared that initiating ESS into the hospital system was a “very frustrating process. . . . It took us a really long time to get everyone on board that this was the system to go with . . . It took a while for the Chief Financial Officer to sign off.”
Similarly, many noted that the lack of a standardized ESS system across hospitals was a barrier to effective time usage. As a HA shared, “If we could get people on a standardized objective (ESS) system that was comparable, hospital to hospital, then you can spend your time out doing the . . . staff education, interpretation (of infections) for staff nurses, being the expert for them.”
It was also acknowledged that ESS was not a panacea and had limitations. As one ICU NM commented,
(Name of ESS software) is automated, so it only gets what is available electronically. . . . To overcome this problem . . . nurses can do observations. It's one thing to say everybody's washing their hands . . . but watching staff wash their hands . . . none of that's automated, so ESS is not going to get any of that.
Although many perceived ESS as a tool to decrease workload, some personnel expressed concern with how the data from ESS should be interpreted and implemented. One IP cautioned, “You can't just use that number (ESS gives). You have to go through and look at the cases and make sure that they are all meaningful . . . that it's truly an infection.”
IP Role Expansion
In general, participants perceived that among the changes that have occurred regarding infection control is an increase in IP responsibilities with the subthemes of (a) increased visibility, (b) IP as expert consultant and educator, (c) IPs as policing infection prevention practice, and (d) time burden. As one IP simply stated, “We are no longer just data gatherers.” A HA details the evolving focus and growth in responsibilities:
It used to be infection control, and now it's infection prevention. As I think back, the role was more in terms of putting out fires, making sure that we were doing the right thing when a patient came into the hospital, so we didn't spread communicable diseases . . . and now, it's more proactive. IPs being aware, partnering with the Health Department . . . preparing the hospital for some pandemic event . . . the knowledge of the IP and the reliance on that person's knowledge and skill, and partnering of skills with the medical staff . . . has just increased many, many times.
IPs expressed that a positive development is increased visibility and recognition of their role within their organization. One IP related how in a recent public health crisis situation involving infection control their organization relied on IPs to provide critical guidance:
When we had the pandemic flu, (the hospital board) called infection control and said, “Okay, we need you to lead us through what we're going to do, how we're going to approach this, what resources we need.” . . . So it was nice that they recognized and said: “We need you to lead” instead of just saying: “This is what we're going to do.”
Increasingly within their organization, IPs are being turned to as expert consultants for infection issues and have a more visible and respected role in the organization. As one HA noted,
(Name of ICD)'s role is very important. I look at (Name of ICD) now when she speaks to the medical staff, and they seek her out for advice because they really value her expertise. That's very different than the way it used to be. . . . Now physicians call (Name of ICD) and say: “What do we need, how should we handle this?”
An added benefit of this increased recognition and reliance on IPs by varied staff is that it enhances IPs’ ability to perform the role of educator. This unexpected consequence is reflected in the following comments made by one IP: “I got a lot more calls about just regular stuff that they just needed some better information about. And then we find out about some of the practices that are going on.”
IPs are also assigned a broad educational mandate as part of their responsibilities. One HA summed up this aspect of the roles concisely:
I think the infection control folks’ role is to educate us as an organization; us being medical staff, everybody. So I think they have a huge responsibility because they have a large audience, and make us aware of what is coming down the cue (new regulations), and how do we need to position ourselves to be ready for that.
Another responsibility involves participating in the formulation and implementation of policies and practices for HAI prevention. Many IPs serve on product review committees and negotiate resources necessary for HAI prevention. Indeed, as the following comment by an IP indicates, policing the implementation of recommendations is a critical element of infection prevention:
I'm on the product review committee and approve kits like stat locks in Foley trays. I went up (to the floors) one day and I still saw the garter belt Velcro strap . . . I find out that you really have to go back to make sure something gets to the end point; Once we have approved something, we need some process to make sure it got put in place.
Time burden was a negative consequence of recent expansions to the IP role. A number of IPs commented that as new infection control activities have been added to their role, they are hampered in following through on all of their earlier responsibilities. One IP eloquently shared how an overwhelming amount of responsibilities prevented her from addressing the local issues:
I used to be a lot more in the weeds . . . helping with exposures or helping with surveillance when they needed it. I don't really do any of that anymore. I am helping draft the pandemic plan and getting that through the organization and I am doing much broader things. I have always done things sort of there, but much more of the day-to-day, I really don't do anymore.
This difficult balancing act that IPs are now confronting is captured in another IP's comments:
Virtually everything in the hospital is in some shape or form related to infection prevention. So we a lot of times get asked to read a lot of things that may be, or not, we have to really pick and choose which things we do now.
Organizational Climate
Organizational Climate encompasses the larger infrastructure of the organizational support participants encountered related to infection control. Three subthemes emerged: (a) organizational values, (b) communication, and (c) environments.
Organizational values was the most frequently mentioned subtheme. In this subtheme, shared accountability, teamwork, and maintaining interdisciplinary collaboration were recurrently emphasized. The majority of respondents expressed the need to “engage everybody” in the infection-control process. One HA's comments illustrated this point, “Now it's really involving everybody . . . infection control isn't just one person's job but is everyone's.” This feeling of communal responsibility within the organization is conveyed simply in one ICU NM's words:
Infection control is only a part of the bigger picture. . . . It can't be isolated. It has to be in every single individual and if it's not, it's never going to work, no matter how many people you have.
Indeed, the importance of shared accountability was endorsed by personnel across all the different roles. Linked to shared accountability is a new emphasis on teamwork and pooling of resources. Many felt that such an approach has been a major facilitator for implementing effective infection prevention. One HA explained,
We work together as a team. I can remember years ago where you didn't have that. (In the past people would say) why should I pay for it? You should pay for it; it shouldn't come out of my budget. But now, it's for the good of the facility.
Maintaining interdisciplinary relationships emerged in the narrative accounts as a powerful link that bridged shared accountability and teamwork and shaped the organizational culture regarding infection control. An ICD explained this complex process,
I think it's a multi-factorial approach. . . . It has a lot to do with a good will approach, . . . enough people who were willing to make it happen, . . . having a team that can get buy-in from the multiple areas. . . . I think it's important, that even if you do an outstanding job to reach out to nursing. I think the buy-in to get the chief-of-surgery to let you (IPs) into their grand rounds . . . or sometimes having the physician contact actually helps (facilitate infection prevention).
Nonetheless, establishing and maintaining multidisciplinary buy-in on infection control can be challenging as one IP related: “There's so many priorities and to have people focus on what you think is a priority and then to be able to work together effectively is hard.”
Effective communication, the second subtheme, was closely related to the organizational values subtheme. Communication was frequently mentioned as a facilitator for enforcing infection-prevention efforts. Indeed, many personnel reported that infection control meetings increased the opportunity for interdisciplinary collaboration. Some also shared how such communication opportunities could be enhanced. As one HA noted, “Yes there is collaboration on the committee, but I would like to see even more discussion. . . . I would like to actually see them being more . . . about practices in the organization.”
A communication strategy was to emphasis quality. As another HA pointed out,
If I've got an (infection) issue around quality, I know that the board will 100% get behind doing the right thing as it relates to quality. They will help me figure out how to find the resources to make that happen.
Many infection-prevention personnel report using ESS to provide compelling data evidence when communicating about safety and allocation of resources. One ICD explained, “ESS has helped us bring information forward in a timely fashion . . . (reporting) how many infections were prevented in one month. Those costs and lengths of stay numbers really help when talking to administration.”
Effective communication skills were mentioned numerous times as a facilitator for supporting a good organizational climate. As one IP eloquently expressed,
It would be most helpful to strengthen our communication skills . . . we need to learn how to take our data and condense it so our staff understand what we're saying so that it will make an impact. I see in our profession that we have a lot of people who are very meticulous with detail and practice, but . . . we need to learn how to effectively communicate to change behavior and to help people understand. We also need to understand the sphere of practices, not just infection control . . . but at the same time it's very hard to get people to also see through our eyes sometimes. So if there would be one nut I would crack, it would be to help my team more effectively communicate what we're seeing to more effectively change our culture.
Despite the benefits of information sharing among the professions, a negative consequence has been the addition of layers in the reporting structures. As one IP stated,
Instead of working with (just) the Infection Control Committee, now we work with Infection Control Committee and each practice counsel, and each Performance Improvement Committee, and each unit-based blah, blah. So there are just a lot more hierarchy that we're working with. Now I feel like we work more with the middle management type of people (and not the frontline).
However, some IPs also expressed frustration at not being included at the discussion table. As one IP observed,
What I have found is that once discussions are made at the higher level, (the administrators) will come back and say: “Okay, there's discussion about wanting central line reduction to be the goal, what should that look like?”. . . And we'll basically help with the nuts and bolts. But we are not at the same level with the senior directors discussing what those goals are.
The final subtheme, organizational environment, not only encompassed the need for material resources but also included support for human resources. The recent economic crisis has affected IP department staffing. One IP acknowledged the ongoing challenge of practicing infection control in a financially constrained setting: “I have a very supportive boss, but with the economy, the CEO is saying we just can't hire everybody . . . it's an exciting field but we could do a good job if we had the right tools.”
Although no personnel reported 100% satisfaction with current environmental support, many recognized that these fiscal measures transcended their institutional setting. One HA shared, “You could always use more staff . . . I could keep three more busy with projects but that's not a real-world scenario.”
The majority of personnel recognized data collection as an area being “understaffed and undersupplied” and called for help in data analysis. As one ICD stated, “Having another person on my team that was just a data analyst . . . that could be helpful.”
As a result of the current budget issues present in the California hospital system, an increasing number of personnel reported being more conscious about cost issues related to infection control. Many personnel shared that they maintained a focus on cost savings when presenting information at board meetings and negotiating budgets for infection prevention. As one IP related,
The ability to know how to give a business case, is absolutely critical when you go up to the CMO or higher-level. . . . When it really comes down to buying software or that type of big-ticket stuff, then you have to be able to know how to stand up and give (your argument).
Indeed, a barrier to ESS implementation is the cost of the system. As one HA related,
It (ESS) is a chunk of change and it's a battle with administration. And it's an ongoing expense; it's not a one time. It's questioned every year and every year the price is up a bit. So we need to make the case that benefits far outweigh the costs.
Discussion
This is the first qualitative study to examine the impact of recent policy changes on hospital infection prevention. From the thick, rich data gathered in the interviews, we found that infection control and prevention in hospitals is changing as a result of recent legislative policies at the state and federal level as well as increased use of technology. Within the 4 major themes identified (mandatory reporting, ESS impact on HAI surveillance, IP role expansion, and organizational climate), respondents described both positive changes and frustrations.
Our findings suggest that prevention of infections needs an interdisciplinary team approach, highlight the need for common well-developed definitions for public reporting, and suggest that long-term research is needed to fully understand the impact of these important policy changes. Many participants expressed frustration over increased workload related to reporting regulations and ESS data entry. Unless clinicians clearly understand why they are following these mandated requirements, or any other infection prevention process, compliance is likely to be variable. Increasing interdisciplinary collaboration and education may facilitate information sharing and reduce barriers for promoting infection prevention.
Positively, in January of 2009, the Department of Health and Human Services released a plan to prevent HAIs: Action Plan to Prevent Healthcare-Associated Infections. The overall goal of the plan was to improve the coordination of existing interventions and resources at the federal level to maximize reducing HAIs (Department of Health and Human Services, 2009). Another federal initiative announced by Medicare after the interviews were conducted is that beginning with January 2011 all hospitals must join the National Healthcare Safety Network (NHSN) and report critical care–specific central line–associated bloodstream-infection rates with aims to enhance public reporting and ultimately inform value-based purchasing or be penalized on payment (Federal Register, 2010). Because the Centers for Disease Prevention and Control NHSN monitoring surveillance system uses well developed HAI definitions, it may encourage increased standardization in reporting requirements.
In another qualitative study examining the role of champions in infection prevention, researchers found that more than one champion was needed to lead HAI prevention improvements that required a behavioral change and interdisciplinary relationships (Damschroder et al., 2009). In addition, the authors of that study concluded that champions who worked under a poor organizational climate had a harder time implementing change. These findings were similar to what was found in the California hospitals. It is evident that effective infection prevention cannot happen alone, but a high level of organizational climate and interdisciplinary collaboration can give impetus to further improvements.
Limitations
A number of study limitations need to be acknowledged. Though efforts were made to purposefully enroll hospitals across the state of California, the study is limited to this state and therefore may not be nationally representative. However, Damschroder et al.'s qualitative study was conducted in six veteran and nonveteran hospitals across the nation, and there were some similar results suggesting these findings may resonate with employees of other hospitals. Nevertheless, our goal was to deeply understand infection and prevention in hospitals that chose to enroll in the CHAIPI learning collaborative and therefore caution is needed. All participants contacted agreed to be interviewed; however, not all clinicians/personnel (e.g., nurse's aides, staff nurses and housekeepers) who may also directly affect infection prevention were interviewed. Nonetheless, as the participants’ quotes illustrate, a range of both positive and negative impacts surrounding recent changes were revealed. This suggests that not all changes have been constructive and further opportunities exist for improvement.
Conclusion
This study contributes to the understanding of infection prevention and control in light of new legislative and technological changes and explores how these changes are affecting the everyday activities of many health care professionals. By examining the meanings of these perceptions—be it positive or negative—this study has affirmed the relevance of further exploring infection prevention structures and processes (what is currently working or not working).
It is clear that we need to bridge the gap between policy makers and clinical settings. As long as disconnect exist between policy makers and bedside clinicians, HAI prevention methods may be arbitrary; and as a result, prevention activities may be subpar. To overcome such challenges, most urgently, diverse groups of professionals must first come together within institutional settings and enhance interdisciplinary partnerships that foster a positive organizational climate.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was generously funded by the Blue Shield Foundation of California (Grant No. BSCAFND 2490932) and conducted in collaboration with APIC. Preliminary work was funded by the National Institute of Nursing Research (R01NR010107).
Biography
Mayuko Uchida, MSN, GNP-BC, is a PhD student at Columbia University School of Nursing and served as the principal coder for the qualitative data.
Patricia W. Stone, PhD, RN, FAAN, is a professor and the director of the Center for Health Policy at Columbia University School of Nursing. She was also the principal investigator of this study.
Laurie J. Conway, MS, RN, CIC, has worked as an infection preventionist and is a PhD student at Columbia University School of Nursing. She served as a coder for the qualitative data.
Monika Pogorzelska, PhD, MPH, is the project director of this study and a recent PhD graduate in epidemiology at Columbia University Mailman School of Public Health.
Elaine L. Larson, PhD, RN, FAAN, CIC, is professor of pharmacological and therapeutic research and associate dean of research at Columbia University School of Nursing. She is a certified infection control (CIC) preventionist and also a coinvestigator on this study.
Victoria H. Raveis, PhD, is a research professor and the director of the Psychosocial Research Unit on Health, Aging and the Community at New York University. She is an expert qualitative researcher.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Blue Shield of California Foundation The California Healthcare-Associated Infection Prevention Initiative (CHAIPI) 2011 Retrieved from http://www.blueshieldcafoundation.org/california-healthcare-associated-infection-prevention-initiative-chaipi.
- Centers of Disease Control and Prevention Reduction in central line—Associated bloodstream infections among patients in intensive care units—Pennsylvania, April 2001—March 2005. MMWR. 2005;54:1013–1016. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5440a2.htm. [PubMed]
- California Department of Public Health Healthcare Associated Infections Program. 2010 Retrieved from http://www.cdph.ca.gov/programs/hai/pages/default.aspx.
- Damschroder L, Banaszak-Holl J, Kowalski C, Forman S, Saint S, Krein L. The role of the “champion” in infection prevention: Results from a multisite qualitative study. Qual Saf Health Care. 2009;18:434–440. doi: 10.1136/qshc.2009.034199. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services HHS action Plan to Prevent Healthcare-Associated Infections: Information systems and technology. 2009 Retrieved from http://www.hhs.gov/ash/initiatives/hai/infosystech.html.
- Donabedian A. Quality assurance: Structure, process and outcome. Nursing Standard. 1992;7(11 Suppl. QA):4–5. [PubMed] [Google Scholar]
- Federal Register. U.S. Department of Health and Human Services; Washington, DC: 2010. Retrieved from http://edocket.access.gpo.gov/2010/pdf/2010-19092.pdf. [Google Scholar]
- Klevens RM, Edwards JR, Richards CL, Jr., Horan TC, Gaynes RP, Pollock DA, Cardo DM. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Reports. 2007;122(2):160–166. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Goeschel C. An intervention to decrease catheter-related bloodstream infections in the ICU. New England Journal of Medicine. 2006;355:2725–2732. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Using qualitative research. Qualitative Health Research. 2004;14:1366–1386. doi: 10.1177/1049732304269672. [DOI] [PubMed] [Google Scholar]
- Scott RD., II The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention (pp. 1-13): Division of Healthcare Quality Promotion National Center for Preparedness, Detection, and Control of Infectious Diseases, Coordinating Center for Infectious Diseases Centers for Disease Control and Prevention. 2009 Retrieved from http://www.cdc.gov/ncidod/dhqp/pdf/Scott_CostPaper.pdf.
- Stone PW, Glied SA, McNair PD, Matthes N, Cohen B, Landers TF, Larson EL. CMS changes in reimbursement for HAIs: Setting a research agenda. Medical Care. 2010;48:433–439. doi: 10.1097/MLR.0b013e3181d5fb3f. [DOI] [PMC free article] [PubMed] [Google Scholar]