Abstract
Objective
The purpose of this study was to test a cognitive behavioral treatment protocol for adolescents with a co-occurring alcohol or other drug use disorder (AOD) and suicidality in a randomized clinical trial.
Method
Forty adolescents (Mage = 15; 68% females, 89% Caucasian) and their families recruited from an inpatient psychiatric hospital were randomly assigned to an integrated outpatient cognitive behavioral intervention for co-occurring AOD and suicidality (I-CBT) or enhanced treatment-as-usual (E-TAU). Primary measures include the Schedule for Affective Disorders and Schizophrenia for School-Aged Children, Suicide Ideation Questionnaire, Columbia Impairment Scale, Timeline Followback, Rutgers Alcohol Problem Index, and the Rutgers Marijuana Problem Index. Assessments were completed at pre-treatment as well as 3, 6, 12, and 18 months post-enrollment.
Results
Using intent-to-treat analyses, I-CBT was associated with significantly fewer heavy drinking days and days of marijuana use relative to E-TAU, but not drinking days. Those randomized to I-CBT in comparison to E-TAU also reported significantly less global impairment as well as fewer suicide attempts, inpatient psychiatric hospitalizations, emergency department visits, and arrests. Adolescents across groups showed equivalent reductions in suicidal ideation.
Conclusions
I-CBT for adolescents with co-occurring AOD and suicidality is associated with significant improvement in both substance use and suicidal behavior, as well as markedly decreased use of additional health services including inpatient psychiatric hospitalizations and emergency department visits. Further testing of integrated protocols for adolescent AOD and suicidality with larger and more diverse samples is warranted.
Keywords: Adolescent suicide, alcohol abuse, substance abuse, cognitive-behavioral therapy
Alcohol and other drug use disorders (AOD) and suicidal behavior commonly co-occur among adolescent clinical populations. In a review of the adolescent suicide literature, rates of any AOD were found to range from 27% to 50% among adolescents who died by suicide and were associated with 6- to 8.5- fold increase in risk of suicide (Esposito-Smythers & Spirito, 2004). Rates of AOD among adolescents who attempted suicide ranged from 12% to 50% and an AOD was associated with a three- to four-fold increase in the likelihood of suicide attempts (Esposito-Smythers & Spirito, 2004). Prospective research also suggests that AOD increases risk for future suicidal behavior, particularly in the presence of other mental health problems (Goldston et al., 2009). Further, the relation between AOD and suicidality appears to strengthen as each problem increases in severity (Esposito-Smythers & Spirito, 2004; Goldston et al., 2009).
Though AOD and suicidal behavior co-occur at high rates and may be functionally interrelated (Goldston, 2004), the current standard of care is to treat these problems separately. When individuals with co-occurring suicidality and AOD are cross-referred to separate mental health and substance abuse systems, many fail to receive effective treatment. This failure stems, in part, from conceptual differences and lack of coordination between the mental health and substance abuse treatment systems, as well as a high degree of treatment burden for patients (Hawkins, 2009). Many substance abuse providers subscribe to a medical or disease model of addiction, whereas mental health providers often integrate biological and psychological perspectives in their conceptualization of substance related problems (Hawkins, 2009). Such differences can leave individuals with conflicting treatment messages which, in turn, can negatively affect treatment adherence. Further, substance abuse services may not be reimbursed by insurance companies that provide mental health coverage (Hawkins, 2009), and individuals may not be able to afford both services when reimbursement is unavailable.
Due to the problems associated with sequential or parallel care across separate mental health and substance abuse systems, many have argued for an integrated approach to care (Hawkins, 2009). Integrated treatments for individuals with co-occurring AOD and suicidality are potentially more cost effective and allow ongoing attention to both problems, use of a consistent therapeutic approach, and prioritization of treatment goals. This is particularly important to the degree that suicidal and substance abuse behaviors are interrelated and share commonalities in some of the precipitants, risk factors, and maintaining factors (Goldston, 2004).
Within the adult literature, only Linehan and colleagues have published treatment studies that target suicidality (experienced in the context of borderline personality disorder) and AODs. Linehan et al. (1999) compared Dialectical Behavior Therapy (DBT) to treatment-as-usual in a sample of 28 women with substance abuse. DBT in comparison to treatment as usual was associated with a greater proportion of total alcohol and drug abstinent days at 16-month follow-up, but there were no differences in frequency of self-harm (suicide attempts and/or non-suicidal self-injury). In a second study, Linehan et al. (2002) compared DBT to Comprehensive Validation Therapy plus a 12-step program (CVT + 12S) in a sample of 23 women with heroin dependence on opiate agonist therapy. CVT included the acceptance based strategies employed in DBT (e.g., warmth, empathy) and case management, but not CBT techniques. Only those in DBT maintained self-reported reductions in opiate use through the 16 month follow-up, though no differences were found in positive urinalyses across groups. The incidence of self-harm did not differ across groups. In a third study, Harned, Murray, Comtois, and Linehan (2008) conducted secondary analyses using data from a prior DBT study with 101 adults. DBT was associated with higher rates of full remission from AOD and more self-reported drug and alcohol abstinent days than non-behavioral therapy provided by community psychotherapy experts. DBT was also associated with fewer suicide attempts by the 24 month follow-up period.
Linehan and colleagues’ work suggests that interventions for adults with co-occurring suicidality and AOD are feasible and associated with symptomatic improvement. Similar interventions for adolescents are less well studied. We tested an integrated cognitive behavioral treatment protocol, with a motivational interview, for adolescents with co-occurring alcohol use disorders and suicidality in an open pilot trial with six adolescents and their families. Similar to DBT, this cognitive behavioral protocol was 12 months in duration (6 month active, 3 month continuation, and 3 month maintenance treatment phases). The protocol included individual therapy with a few family sessions delivered by one therapist. All participants reported decreases in alcohol use and suicidal ideation. Two participants re-attempted during the active protocol but improved over the rest of treatment (Esposito-Smythers, Spirito, Uth, & LaChance, 2006).
The present study builds upon our open pilot trial (Esposito-Smythers et al., 2006) to test the efficacy of an expanded version of this protocol in a Stage I clinical trial (Rounsaville, Carroll, & Onken, 2001). The focus of this Stage I research was to conduct pilot and feasibility testing of our intervention, with close attention to participant acceptance of the assessment and intervention (e.g., retention), recruitment procedures, feasibility of treatment delivery (e.g., therapist fidelity), and clinically significant participant improvement. Consistent with Stage I research, our focus was on internal validity and the demonstration of efficacy of our intervention under relatively tightly controlled conditions.
A randomized, controlled, repeated measures design was used to assess the efficacy of an integrated CBT protocol (I-CBT) for co-occurring AOD and suicidality in comparison to an enhanced treatment-as-usual (E-TAU). We hypothesized that I-CBT, in comparison to E-TAU, would lead to greater reductions in adolescent alcohol and marijuana use, alcohol and marijuana related problems, suicidal ideation, and general impairment. We also hypothesized that I-CBT would be associated with fewer suicide attempts and other adverse psychiatric outcomes relative to E-TAU. Further, due to the early developmental phase of this intervention, we also explored the effect of I-CBT relative to E-TAU on adolescent mental health symptoms and diagnoses.
Method
Participants
Participants included 40 adolescents (See Table 1) recruited from a psychiatric inpatient unit in the Northeast from November 2004 through February 2007. Participants were eligible for the study if they were: (a) 13–17 years of age, (b) made a suicide attempt within the prior 3 months or reported clinically significant suicidal ideation during the past month (score ≥ 41 on the Suicide Ideation Questionnaire; Reynolds, 1985), (c) had an alcohol or cannabis use disorder, and (d) lived in the home with a parent/guardian willing to participate. They were ineligible if they: 1) had an Verbal IQ estimate < 70 (as per Kaufman Brief Intelligence Test; Kaufman & Kaufman, 1990); 2) were actively psychotic; 3) were homicidal; 4) had bipolar disorder; and 5) were dependent on substances other than alcohol and marijuana.
Table 1.
Summary of Socio-Demographic, Clinical History, and Baseline Variables by Condition
| Variable | Full Sample | I-CBT (n = 19) | E-TAU (n = 17) |
|---|---|---|---|
| N (%)/M ± SD | N (%)/M ± SD | N (%)/M ± SD | |
| Gender (female) | 24 (66.7) | 13 (68.4) | 11 (64.7) |
| Age | 15.72 ± 1.19 | 15.79 ± 0.98 | 15.65±1.41 |
| Race (white) | 32 (88.9) | 17 (89.5) | 15 (88.2) |
| Ethnicity (hispanic) | 5 (13.9) | 3 (15.8) | 2 (11.8) |
| Parents married | 20 (55.6) | 10 (52.6) | 10 (58.8) |
| Income (in dollars) | 63.8K ± 36.6K | 63.3K ± 36.6K | 64.3K± 38.0K |
| Medication | 28 (77.8) | 13 (68.4) | 15 (88.2) |
| Full scale IQ score | 98.23 ±11.22 | 99.44 ± 11.28 | 96.94 ± 11.36 |
| Unipolar mood disorder | 34 (94.4) | 18 (94.7) | 16 (94.1) |
| Anxiety disorder | 20 (55.6) | 11 (57.9) | 9 (52.9) |
| Disruptive behavior disorder | 18 (50) | 8 (42.1) | 10 (58.8) |
| Alcohol use disorder* | 23 (63.9) | 10 (52.6) | 13 (76.5) |
| Cannabis use disorder | 30 (83.3) | 15 (78.9) | 15 (88.2) |
| Other substance abuse | 5 (13.9) | 2 (10.5) | 3 (17.6) |
| Non-suicidal self-injury | 26 (72.2) | 14 (73.7) | 12 (70.6) |
| Any suicide attempt | 27 (75) | 14 (73.7) | 13 (76.5) |
| Single attempt | 15 (55.6) | 8 (57.1) | 7 (53.8) |
| Multiple attempts | 12 (44.4) | 6 (42.9) | 6 (46.2) |
| SIQ | 71.56 ± 40.56 | 74.00 ± 44.74 | 68.82 ± 36.50 |
| CIS – Teen | 1.61 ± 0.61 | 1.59 ± 0.71 | 1.63 ± 0.50 |
| CIS – Parent* | 1.62 ± 0.81 | 1.84 ± 0.92 | 1.38 ± 0.63 |
| TLFB drinking days | 3.31 ± 4.78 | 4.32 ± 5.97 | 2.18 ± 2.70 |
| TLFB heavy drinking days | 2.28 ± 3.88 | 2.95 ± 4.86 | 1.53 ± 2.29 |
| TLFB marijuana use days | 10.08 ± 9.95 | 9.58 ± 9.73 | 10.65 ± 10.46 |
| RAPI | 13.22 ± 13.94 | 12.95 ± 14.71 | 13.53 ± 13.47 |
| RMPI | 16.22 ± 14.38 | 14.84 ± 13.81 | 17.76 ± 15.26 |
| RADS-2 | 60.86 ± 12.76 | 60.79 ±13.34 | 60.94 ± 12.49 |
| SCARED | 26.14 ± 15.72 | 27.21 ± 18.18 | 24.94 ± 12.87 |
| BASC-Depression | 67.44 ±16.85 | 71.21 ± 19.54 | 63.24± 12.48 |
| BASC-Anxiety | 58.00 ±11.96 | 57.11 ±10.74 | 59.00 ± 13.46 |
| BASC-Conduct Problems | 77.67±16.45 | 79.89 ±17.17 | 75.18 ± 15.76 |
Note. Of the 4 (11.1%) of participants who were non-White in the full sample, 1 was African American, 1 was biracial, 1 was Asian American, and 1 was Native American.
medium effect size (Cohen’s h & d). All other comparisons yielded ≤ small effect size. SIQ = Suicide ideation Questionnaire; CIS = Columbia Impairment Scale; TLFB = Timeline Followback 30 day recall; RAPI = Rutgers Alcohol Problem Inventory; RMPI = Rutgers Marijuana Problem Inventory; RADS- 2 = Reynolds Adolescent Depression Scale – 2; SCARED = Screen for Child Anxiety Related Emotional Disorders; BASC = Behavioral Assessment Scale for Children.
Procedures
Screening and Recruitment
All study procedures were approved by the participating hospital and university institutional review boards. A two tier screening and recruitment procedure was used. The inpatient charts of hospitalized adolescents were screened by a research assistant for initial study eligibility and permission to recruit potentially eligible families was obtained from the attending psychiatrist. The first author or study coordinator recruited families from the inpatient unit. Those families who provided parental consent and adolescent assent were enrolled in the study and asked to participate in a second screening to confirm study eligibility and obtain data for randomization. Those deemed eligible were scheduled for a baseline assessment and were randomized. All baseline assessments were conducted on the inpatient unit or within 10 days of discharge.
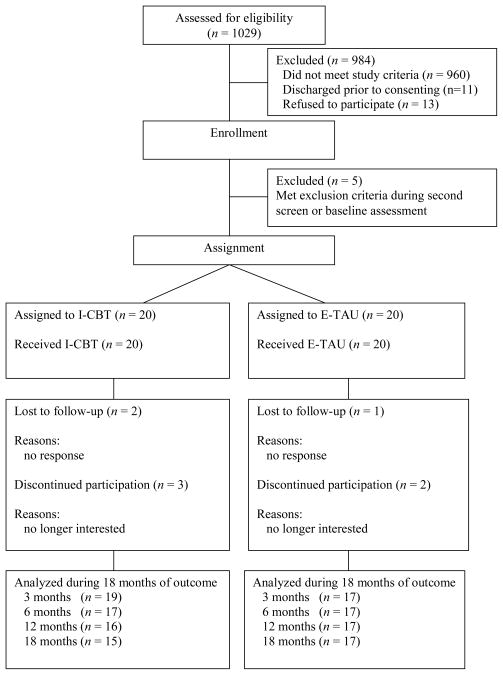
Figure 1 provides information about participant flow. A total of 1029 inpatient charts were screened for initial eligibility. Based on chart reviews and information obtained from the inpatient treatment team, 960 (93%) families were deemed ineligible. Of the 69 potentially eligible families, 58 (84%) were approached for recruitment. Eleven youth were not approached because they were discharged from the inpatient unit too quickly. Forty-five families provided consent (78%) to participate in the study and completed the second screen. The reasons for the 13 refusals included: family planned to move away, wanted a provider closer to home, and wanted to remain with current outpatient provider. Two youth were excluded based on the second screen (one reported heavy use of substances other than alcohol or marijuana, one denied any suicidal ideation or suicide attempt). Of the forty-three remaining families, three additional families were excluded after baseline assessment (one for bipolar disorder, two for active psychotic symptoms). This resulted in forty eligible confirmed families who were randomized into I-CBT (n = 20) or the E-TAU (n = 20) condition. All 40 randomized participants were considered for intent-to-treat analyses but four did not provide any follow-up data and could not be included, one in I-CBT and three in E-TAU. The follow-up assessment completion rates were as follows: 90% at 3 months, 85% at 6 months, 83% at 12 months, and 80% at 18 months.
Figure 1.
Participant flow through the study. I-CBT = integrated cognitive behavioral therapy; E-TAU = enhanced treatment as usual.
Randomization
Participants were randomized to I-CBT or E-TAU, by the first author or study coordinator, using a computerized urn randomization program (Stout, Wirtz, Carbonari, & Del Boca, 1994). Urn randomization was used to retain random allocation while balancing the treatment conditions on four a priori variables including gender, suicide attempt history, primary use of alcohol or marijuana, and presence of significant conduct problems.
Schedule of Assessments
The baseline assessment included a diagnostic interview administered by masters or doctoral level clinical trainees and self-report instruments administered by a bachelor level research assistant. The first author provided training in all assessments with the exception of the Timeline Followback (TFLB) which was covered in the context of a professional workshop. Research assistants who completed the follow-up assessments were not informed of treatment assignment, but they did learn of treatment assignment on occasion due primarily to spontaneous comments made by study participants. The date of enrollment served as the reference point for the follow-up assessments, with follow-up assessments administered at 3, 6, 12, and 18 months post-enrollment.
Study Conditions
Participants in both the I-CBT and E-TAU conditions were both offered two free services through the study. First, results of the comprehensive diagnostic evaluation conducted as part of the baseline assessment was provided directly to the treating therapist, with parental permission. Second, all participants were offered a free medication evaluation and medication management over the course of their study participation (18 months) by a board certified child psychiatrist employed by the study. The cost of medication was not covered. Due to the heterogeneity of the study population, it was not possible to control type of medication prescribed. However, having one prescribing psychiatrist for all study participants helped minimize heterogeneity of prescribing practices. All but two participants in E-TAU prescribed medication opted to have their medication managed by the study psychiatrist, who was not blind to treatment assignment.
I-CBT
The I-CBT protocol is grounded in social cognitive learning theory. From a social-cognitive learning theory perspective (Bandura, 1986), mental health problems may result in part from prior learning histories, especially the learning of social behaviors and core beliefs. Learning experiences are based on operant and classical conditioning processes, social reinforcement, and observation and modeling of others. To promote change in these areas, adolescents must re-learn adaptive ways of relating to self and others and develop self-efficacy in the use of their new skills (Bandura, 1986). This can be accomplished through the use of CBT which combines behavior change and cognitive information processing methods to facilitate skill acquisition. To effectively intervene with adolescents with co-occurring AODs and suicidality in particular, CBT must target the common maladaptive behaviors and beliefs that underlie problems in these areas, including cognitive distortions as well as poor coping, communication, and parenting skills. This entails work with the adolescent on individual skill development (e.g., cognitive restructuring, problem-solving, affect regulation, communication) as well as parents around appropriate modeling and parenting practices (e.g., affect management, monitoring, communication, contingency management, etc.). Improvement in adolescent and parent skill development, in turn, should lead to reductions in youth AOD and suicidality.
Consistent with social-cognitive learning theory, the I-CBT protocol integrated CBT techniques to remediate maladaptive cognitions and behaviors found to underlie both adolescent suicidality and AOD. The I-CBT manual was developed by modifying earlier versions of CBT protocols for adolescents who made a suicide attempt (Donaldson, Spirito, & Esposito-Smythers, 2005) and those with co-occurring suicidality and AODs (Esposito-Smythers et al., 2006). The I-CBT protocol was comparable in length to the Esposito-Smythers et al. (2006) protocol but included individual adolescent, family, and parent training sessions. An adolescent therapist and a family/parent training therapist were assigned to each case. In the acute (6 months) treatment phase, adolescents attended weekly sessions and parents weekly to bi-weekly sessions. In the continuation (3 months) treatment phase, adolescents attended bi-weekly sessions and parents biweekly to monthly sessions. In the maintenance treatment phase (3 months), adolescents attended monthly sessions and parents attended monthly sessions as needed.
The I-CBT protocol offered a menu of cognitive-behavioral individual adolescent (e.g., problem-solving, refusal skills), family (e.g., communication, behavioral contracting), and parent training (e.g., monitoring, emotion regulation) sessions. It also included one motivational interviewing session for adolescents to improve readiness for AOD treatment and one for parents to facilitate treatment engagement. Sessions could be repeated and practiced throughout the protocol. Outside of sessions, case management calls were made (e.g., school, social services) as needed. See Esposito-Smythers et al. (2011) for a list of sessions and a case study using I-CBT.
If an adolescent became actively suicidal during treatment, a psychiatric evaluation was scheduled at a local hospital. Re-hospitalization was recorded as an outside treatment contact and the adolescent continued in the study unless more intensive services (e.g., residential, in-home) was indicated by the inpatient treatment team who served as an independent evaluator.
Training and Fidelity
Twelve therapists delivered the I-CBT protocol, including three Ph.D. level licensed clinical psychologists, eight clinical psychology post-doctoral trainees, and one master’s level clinician. All therapists had prior training and experience using CBT. They were trained by the first-author through didactic instruction and role-plays. All therapists reviewed treatment sessions with the first author, developed outlines of sessions to facilitate material acquisition, and then role played each session. Sessions were role-played until the first author was confident in each therapists’ ability to deliver each session with fidelity.
All I-CBT sessions were audiotaped. Audiotapes for the first two cases seen by each therapist and a random selection of other audiotapes were reviewed for supervision and rated for fidelity by the first or second author and detailed feedback was provided in group supervision. These reviews included 20% of the initial skill building sessions completed by each therapist to ensure adequate skill implementation and a random sample of other treatment sessions to prevent therapist drift. Fidelity instruments used to rate audiotapes included the Cognitive Therapy Rating Scale (CTRS; Young & Beck, 1980) and Adherence Checklists (see measures below), which were piloted in the open pilot trial (Esposito-Smythers et al., 2006). Scores ≥ 44 on the CTRS and adherence to at least 80% of items on adherence checklists were deemed acceptable.
Weekly group supervision was provided by the first and second authors and was used to discuss skills employed in session, review photocopies of I-CBT worksheets completed with participants, and review ratings from audiotape reviews. Individual supervision was also provided when emergent situations arose. If therapist drift was evident through any method of supervision, obstacles to adherence were processed, solutions generated, and role-plays conducted to enhance training. If fidelity ratings did not meet study criterion on two consecutive audiotapes, supervision would have been increased but this did not occur.
E-TAU
The outpatient treatment schedule and therapeutic approach in the E-TAU condition was determined independently by community providers. As noted above, community treatment was enhanced with the provision of a diagnostic evaluation report that was shared with community providers, and medication management provided by the study psychiatrist. Further, families in E-TAU were provided with a study number that they could call to obtain information about resources available to adolescents and families in their community (e.g., mental health, substance abuse, school, family court, and vocational services). Emergent and non-emergent appointments with the study psychiatrist were also available and facilitated by study staff.
Measures
Cognitive Functioning
The Kaufman Brief Intelligence Test (K-BIT; Kaufman & Kaufman, 1990) was administered to obtain a Verbal IQ estimate.
Treatment Services
The Child and Adolescent Services Assessment (CASA; Burns et al., 1997) was used to obtain information about service use for mental health problems. Adequate reliability has been demonstrated for the CASA (Farmer et al., 1994). The Psychosocial Treatments Interview (PTI: Steketee et al., 1997) assesses participant perception of techniques used in psychotherapy. The PTI was adapted to assess for a greater number of CBT techniques. The revised PTI yielded strong reliability for cognitive and behavioral subscales in the present sample including general individual, alcohol/drug specific, and family subscales (α = .83–.95).
Psychiatric Diagnosis
Psychiatric diagnosis was assessed using the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version (K-SADS- PL; Kaufman et al., 1997). Masters and post-doctoral level interviewers were trained through didactics, ratings of interviews, supervisor observation of in-person interviews, and supervisor audiotape review of interviews. All cases were staffed during clinical consensus meetings that included clinical child psychologists and the interviewers. A best-estimate clinical consensus procedure was used to resolve discrepancies between adolescent and parent report which yields good to excellent reliability (Cantwell, Lewinsohn, Rohde, & Seeley, 1997).
Alcohol/Marijuana Consumption and Problems
Alcohol and marijuana use were assessed with the Timeline Followback (TLFB; Sobell & Sobell, 1995), a calendar-assisted daily drinking and drug use estimation method that has been used successfully in clinical trials with substance abusing youth (e.g., Waldron et al., 2001). A 30-day recall of alcohol (number of drinks) and marijuana (any use) use was collected. Urine toxicology screens were used to corroborate TLFB data. The Rutgers Alcohol Problem Index (RAPI; White & Labouvie, 1989) and the Rutgers Marijuana Problem Index (RMPI; Johnson & White, 1989), which have strong psychometric properties with adolescents (White & Labouvie, 1989; Simons et al., 1998), were used to assess alcohol and marijuana related problems, respectively, in the prior 3 months.
Suicide Attempts, Ideation, and Other Adverse Psychiatric/Legal Outcomes
The suicide items from the K-SADS-PL depression module (Kaufman et al., 1997) were administered to adolescents and their parents to assess for suicide attempts. This information was staffed during a clinical consensus meeting, as described above, and those acts performed with suicidal intent were coded as suicide attempts. Self-report of adolescent suicidal ideation over the prior month was assessed with the psychometrically sound Suicide Ideation Questionnaire-Senior Version (SIQ-Sn; Reynolds, 1985). Data on arrests and running away episodes was obtained with a case management form created for this study. Hospitalization, emergency room visits, and long-term residential placement data was obtained with the CASA (Burns et al., 1997) as described above.
General Impairment
The Columbia Impairment Scale (CIS; Bird et al., 1993) is a psychometrically sound self-report and parent-rated instrument that was used to assess for adolescent global impairment. Participants completed questions with reference to the last 12 months at baseline and three months at all follow-ups.
Mental Health Symptoms
Self-report of depressive symptoms were assessed with the Reynolds Adolescent Depression Scale-2 (RADS-2; Reynolds, 2002), which has excellent psychometric properties in normative and clinical adolescent samples (Reynolds, 2002). The Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et. al., 1999) is a well validated self-report measure that was used to assess adolescent symptoms of anxiety. The well validated Behavioral Assessment Scale for Children (BASC; Reynolds, & Kamphaus, 1992) was used to assess parent perceptions of adolescent symptoms over the past 6 months. T-scores from the depression, anxiety, and conduct problems subscales were used in study analyses.
Therapist Fidelity
The Cognitive Therapy Rating Scale (CTRS; Young & Beck, 1980) was used to measure therapist competence in the delivery of the I-CBT protocol. The CTRS has strong psychometric properties (Vallis et al., 1986). Scores ≥ 44 on the CTRS are considered acceptable. Approximately 92% of rated sessions met this criterion (M = 51, SD = 4.95, range = 35–66). I-CBT adherence checklists were created by the first author. A checklist was created for each module and included components common (e.g., assessed for suicidality) and unique (e.g., identified suicide triggers) to each session. Number of items on checklists ranged from 10 to 17 across sessions. Adherence to 80% of items in a session was deemed acceptable. Approximately 85% of rated sessions met this criterion (M = 93%, SD = 17.68, range = 50%–100%).
Data Analysis Plan
Main Outcome Analyses
To test the study hypotheses, we ran models to examine whether I-CBT compared to E-TAU would result in superior AOD outcomes (less days of alcohol use, heavy alcohol use, marijuana use, and alcohol and marijuana problems) and lower suicidal ideation and general impairment, at 3, 6, 12, and 18 months post-enrollment. Nine separate analyses were conducted using generalized estimating equations (GEE; Liang & Zeger, 1986) using PROC GENMOD in SAS (SAS Institute, 1997). GEE provides an extension of regression analyses to repeated or correlated data, allows inclusion of participants with some missing data, and is flexible in its ability to handle a range of distributions.
GEE analyses covaried the baseline value of the respective dependent variable and included a linear effect of time. Treatment condition was coded using an orthogonal contrast (−.5 for E-TAU vs. .5 for I-CBT), and time was centered so that we could evaluate the main effect of treatment and the time X treatment interaction in one simultaneous model; the time X treatment interaction indicates whether treatment effects became more or less pronounced over time. Use variables followed a count distribution with overdispersion due to positive skewness. We therefore used a negative binomial distribution and the logit link function for analyzing these outcomes. The exponent of the model coefficient reflects the ratio of the number of events expected to occur in one condition relative to the number of events expected to occur in the other condition. The continuous measures of problems (RAPI and RMPI) were square-root transformed to correct positive skewness, standardized, and analyzed using a normal distribution function; the model coefficients for these GEE model represent the differences in standard deviation units associated with the predictor. GEE analyses predicting abstinence from both alcohol and marijuana using a binomial distribution and logit link function were also conducted. Analyses of general impairment (parent and child versions of the CIS) and suicidal ideation (SIQ) at each follow-up were also conducted using GEE and mirrored those for alcohol and marijuana problems. Only the SIQ needed to be square-root transformed due to positive skewness; all variables were standardized to ease interpretation of effect sizes. The number of treatment sessions attended was not significantly associated with any dependent variable in these analyses. Therefore, it was not included as a covariate in the analyses presented herein.
Seven analyses were conducted to examine the rates of suicide attempts and other major adverse psychiatric outcomes. These events were so rare that they were aggregated across the 18 months of follow-up and compared by treatment condition using contingency tables.
Exploratory Study Analyses
Five exploratory analyses were conducted to examine the effect of I-CBT relative to E-TAU on adolescent self-report (RADS, SCARED) and parent report (three scores on the BASC) of mental health symptoms at each follow-up using GEE analyses that mirrored those for alcohol and marijuana problems. Further, six chi-square analyses were run to examine differences in rates of diagnoses at pre-treatment and 18 month follow-up across treatment condition. Finally, multiple exploratory t-tests and chi-square analyses were conducted to examine factors that may help explain study findings, including the number of sessions attended, use of CBT techniques, and prescribed medications, across treatment conditions.
Results
Study Sample
Participants included 24 female (66.7%) and 12 male (33.3%) adolescents, with a mean age of 15.7 years (SD = 1.19, Range = 13–17) at pre-treatment. The sample was primarily White (88.9%) and of non-Hispanic ethnicity (86.1%). More than half of the study participants had married parents (55.6%). The yearly household income was variable, with 28.1% of households at less than $30,000/year, 25% at $30,000 to $60,000/year, 18.8% at $60,000 to $90,000/year, and 28.1% at greater than $100,000/year. Approximately 64% of the sample met criteria for an alcohol use disorder and 83.3% a cannabis use disorder. Further, 25% of the sample reported suicidal ideation only and 75% reported a suicide attempt. Among those who attempted suicide, method of prior attempt(s) included overdose (59.3%), cutting (40.7%), hanging (14.8%), drowning (7.4%), suffocation (7.4%), and car accident (3.7%). Adolescents received an average of three years of mental health treatment provided by an average of two prior therapists before study entry. Demographic, clinical history, and baseline pre-treatment characteristic variables across treatment conditions are presented in Table 1. All comparisons were non-significant.
Amount of Treatment and Overlap of CBT Techniques Received Across Conditions
In the I-CBT protocol, participants who completed at least an acute dose of outpatient treatment, equivalent to 24 sessions for adolescents and 12 sessions for parents, were defined as treatment completers. Based on these criteria, approximately 74% of adolescents, 90% of parents, or 74% of families (M = 34.3 sessions, Range = 11–48) randomized to I-CBT were treatment completers. For comparison purposes, using these same criteria, approximately 44% of adolescents, 25% of parents, or 19% of families (M = 19.9 sessions, Range = 0–41), randomized to the E-TAU condition would be considered treatment completers.
Number of outpatient treatment sessions attended by participants across conditions at 12 months post-enrollment was assessed using independent sample t-tests. Two participants in E-TAU who primarily received residential treatment were not included in these analyses. Those randomized to I-CBT (n = 19) relative to E-TAU (n= 15), attended significantly more individual, I-CBT: M = 22.53, SD = 8.44, Range = 5–37; E-TAU: M = 15.53, SD = 10.69, Range = 3–45, t(32) = 2.13, p = .04, d = .75, family, I-CBT: M = 8.53, SD = 4.34, Range = 2–18; E-TAU: M = 4.13, SD = 5.15, Range = 0–15, t(32) = 2.70, p = .01, d = .95, parent training, I-CBT: M = 14.63, SD = 6.51, Range = 3–27; E-TAU: M = 2.07, SD = 4.42, Range = 0–17, t(32) = 6.40, p = .00, d = 2.26, and total number, I-CBT: M = 45.68, SD = 15.67, Range = 11–72; E-TAU: M = 24.60, SD = 13.21, Range =3–47, t(32) = 4.17, p = .00, d = 1.47, of therapy sessions. Unlike I-CBT, some participants in E-TAU also received group sessions, M = 2.87, SD = 4.42, Range =0–12. Further, those in I-CBT relative to E-TAU were more likely to have received 18 out the 24 CBT techniques assessed with the PTI in the context of their treatment. The greatest differences across groups were found in rates of family based CBT techniques, including family pleasant events/interactions, 100% vs. 29.4%, χ2(1, N = 36) = 20.12, p = .00, h = 2.01, problem-solving, 100% vs. 35.3%, χ2(1, N = 36) = 17.70, p = .00, h = 1.88, and behavioral contracting, 100% vs. 47.1%, χ2(1, N = 36) = 13.41, p = .00, h = 1.63, as well as adolescent affect regulation (e.g., progressive muscle relaxation), 94.7% vs. 35.3%, χ2(1, N = 36) = 14.27, p = .00, h = 1.43, and cognitive restructuring,100% vs. 64.7%, χ2(1, N= 36) = 8.05, p = .005, h = 1.27, techniques.
Medication Protocols Employed Across Conditions
At study entry, 77.8% (n = 28) of adolescents were prescribed psychiatric medication. Specifically, 42.9% (n = 12) of adolescents were prescribed an anti-depressant only, 10.7% (n = 3) a mood stabilizer only, 7.1% (n = 2) two antidepressants, 3.6% (n = 1) an anti-depressant and mood stabilizer, 14.3% (n = 4) an anti-depressant and anti-psychotic, 10.7% (n = 3) an anti-depressant and stimulant, and 10.7 % (n = 3) two anti-depressants and a stimulant. These medication protocols were common across follow-up periods. There were no significant differences on number of youth prescribed medication across the I-CBT and E-TAU conditions, respectively, at baseline, 68.4% vs. 88.2%, χ2(1, N = 36) = 2.04, p = .15, h = .50; 3 months, 66.7% vs. 82.4%, χ2(1, N = 35) = 1.13, p = .29, h = .35; 6 months, 64.7% vs. 70.6%, χ2(1, N = 35) =.13, p = .71, h = .13; 12 months, 56.3% vs. 47.1%, χ2(1, N = 33) = .28, p = .60, h =.18; or 18 months, 40.0% vs. 47.1%, χ2(1, N = 32) = .16, p = .69, h = .14. Rates of full adherence to prescribed medication were also comparable across conditions, respectively, at 3 months, 75.0% vs. 78.6%, χ2(1, N = 26) = .05, p = .83, h = .10; 6 months, 72.7% vs. 83.3%, χ2(1, N = 23) = .38, p = .54, h = .24; 12 months, 66.7% vs. 50.0%, χ2(1, N = 17) = .49, p = .49, h = .35, and 18 months, 66.7% vs. 62.5%, χ2(1, N = 14) = .03, p = .87, h = .08.
Alcohol/Marijuana Consumption and Problems
Drug use other than marijuana was uncommon during follow-up. There were 39 cases of positive urine screens during follow-ups, only 4 of which did not involve marijuana. A total of 4 out of 47 self-reports of abstinence from marijuana and alcohol across the 3, 6, 12, and 18 months follow-ups were disconfirmed by urine drug screens positive for marijuana and were recoded to non-abstinence. For the analysis of number of marijuana use days, those 4 cases were set to missing as the number of days of use were not known.
As can be seen in Table 2, for days of alcohol use, the effect of treatment and the time X treatment interaction were both non-significant. For days of heavy alcohol use, the effect of treatment was non-significant but the time X treatment interaction was significant, indicating that I-CBT was associated on average with a more than 50% reduction in the expected number of heavy drinking days and that this effect became stronger at later follow-ups. For days of marijuana use, both the main effect of treatment and the time X treatment interaction were significant, indicating a more than 60% reduction in the expected number of marijuana use days in I-CBT compared to E-TAU, with the effect significantly stronger at later follow-ups compared to earlier follow-ups. When abstinence from alcohol and marijuana was considered as a binary dependent variable, there was no main effect of I-CBT or time X treatment interaction. For alcohol problems, the effect of treatment and the time X treatment interaction were both non-significant. For marijuana problems, there was no main effect of treatment, but there was a significant time X treatment interaction, indicating that marijuana problems reduced more over time in the I-CBT condition compared to the E-TAU condition.
Table 2.
Summary of Results from GEE Analyses Used To Examine Treatment Effects
| Treatment | Treatment X Time | p | ||||
|---|---|---|---|---|---|---|
| exp(B)/B | 95% CI | p | exp(B)/B | 95% CI | ||
| Main Outcomes | ||||||
| TLFB drinking days1 | 0.61 | 0.29, 1.32 | .21 | 0.87 | 0.56, 1.36 | .54 |
| TLFB heavy drinking days1 | 0.43 | 0.16, 1.15 | .09 | 0.54 | 0.35, 0.85 | .007 |
| TLFB days marijuana use1 | 0.39 | 0.19, 0.77 | .007 | 0.65 | 0.47, 0.90 | .009 |
| TLFB abstinence2 | 1.03 | 0.73, 1.44 | .87 | 1.01 | 0.89, 1.15 | .88 |
| RAPI3 | −0.29 | −0.67, 0.10 | .15 | −0.27 | −0.57, 0.02 | .07 |
| RMPI3 | −0.02 | −0.42, 0.37 | .91 | −0.29 | −0.58, −0.003 | .048 |
| CIS – Teen3 | −0.29 | −0.69, 0.11 | .15 | −0.23 | −0.44, −0.02 | .03 |
| CIS – Parent3 | −0.49 | −0.88, −0.09 | .02 | −0.08 | −0.31, 0.14 | .49 |
| SIQ3 | −0.31 | −0.78, 0.15 | .19 | 0.01 | −0.22, 0.24 | .90 |
| Exploratory Outcomes | ||||||
| RADS-23 | −0.13 | −0.97, 0.72 | .77 | −0.15 | −0.70, 0.40 | .60 |
| SCARED 3 | −0.17 | −0.57, 0.23 | .41 | −0.18 | −0.34, −0.02 | .03 |
| BASC-Depression3 | −0.51 | −0.91, −0.10 | .01 | 0.08 | −0.29, 0.13 | .47 |
| BASC-Anxiety3 | −0.38 | −0.84, 0.08 | .10 | −0.10 | −0.33, 0.13 | .40 |
| BASC-Conduct Problems3 | −0.73 | −1.47, 0.02 | .06 | −0.19 | −0.71, 0.34 | .40 |
Note. TLFB = Timeline Followback 30 day recall; RAPI = Rutgers Alcohol Problem Inventory; RMPI = Rutgers Marijuana Problem Inventory; CIS = Columbia Impairment Scale; SIQ = Suicide ideation Questionnaire; RADS- 2 = Reynolds Adolescent Depression Scale – 2; SCARED = Screen for Child Anxiety Related Emotional Disorders; BASC = Behavioral Assessment Scale for Children.
Count variables with a negative binomial distribution. The coefficients reported are incidence rate ratios (IRR). A rate of 1 indicates an equal expected number of events in each group.
Dichotomous dependent variable. The coefficient reported is the odds ratio.
Continuous dependent variables that have been standardized. The coefficients reported for treatment represents the standardized difference between treatment and control, i.e., effect size d.
Impairment and Suicidal Ideation
As can be seen in Table 2, the effect of I-CBT on participants’ self reported ratings of impairment was non-significant but the time X treatment interaction was significant, indicating greater reductions over time in I-CBT compared to E-TAU. For parent ratings, the main effect of treatment was significant but the time X treatment interaction was non-significant. For suicidal ideation, the main effect of treatment and the time X treatment interaction were non-significant.
Suicide Attempts and Other Adverse Psychiatric/Legal Outcomes
As can be seen in Table 3, over the course of 18 months, significantly fewer participants in I-CBT relative to E-TAU made a suicide attempt, were hospitalized on a psychiatric inpatient unit, received emergency department evaluations, and were arrested. Reasons for the arrests included drug possession, DUI, breaking and entering, shoplifting, assault and battery, resisting arrest, domestic disturbance, and larceny. No participants in I-CBT were placed in residential treatment compared to three in E-TAU. Though in the expected direction, a significant difference in rates of partial hospitalization nor running away from home was found across groups.
Table 3.
Summary of Suicide Attempts and Other Adverse Psychiatric/Legal Outcomes
| I-CBT (n = 19) | E-TAU (n = 17) | χ2 | p | Cohen’s h | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Suicide attempt | 1 | 5.3 | 6 | 35.3 | 5.17 | .023 | 0.82 |
| Inpatient hospitalization | 3 | 15.8 | 9 | 52.9 | 5.57 | .018 | 0.81 |
| Partial hospitalization | 1 | 5.3 | 4 | 23.5 | 2.50 | .114 | 0.57 |
| Residential placement | 0 | 0 | 3 | 17.6 | --- | --- | --- |
| Emergency dept. visit | 3 | 15.8 | 10 | 58.8 | 7.20 | .007 | 0.93 |
| Arrest | 1 | 5.3 | 7 | 41.2 | 6.70 | .01 | 0.94 |
| Ran away | 1 | 5.3 | 5 | 29.4 | 3.77 | .052 | 0.69 |
Note.
Effect size range (h): .20 = small, .50 = medium, and .80 = large effect size.
Mental Health Symptoms and Psychiatric Diagnosis
As can be seen in Table 2, for the RADS-2, neither the main effect of treatment nor the time X treatment interaction were significant. For the SCARED, there was no main effect of treatment but there was a significant time X treatment interaction, indicating a greater effect on anxiety over time in the I-CBT condition than E-TAU. For parent report on the BASC, there was a significant main effect of treatment on depressive symptoms, but no time X treatment interaction. For parent report of adolescent anxiety and conduct problems on the BASC, there was no main effect of treatment nor time X treatment interaction.
With regard to change in rate of psychiatric diagnoses from baseline to 18 month follow-up, I-CBT relative to E-TAU was associated with lower rates of any substance use disorder, 26.7% vs. 76.5%, χ2(1, N = 32) = 7.94, p = .005, h = 1.10. Rates of mood, 6.7% vs. 31.3%, χ2(1, N = 31) = 3.00, p = .08, h = .65, disruptive behavior, 0% vs. 40.0%, χ2(1, N = 15) = 2.73, p = .099, h = 1.31, anxiety, 30.0% vs. 66.7%, χ2(1, N = 19) = 2.55, p = .11, h = .76, alcohol, 25.0% vs. 53.8%, χ2(N = 21) = 1.68, p = .195, h = .60, and cannabis, 30.8% vs. 60.0%, χ2(1, N = 28) = 2.39, p = .12, h = .59, disorders were not statistically different across I-CBT and E-TAU conditions, respectively, though a medium to large effect size was found in favor of I-CBT.
Discussion
Though interventions that target co-occurring suicidality and AODs have been tested with adults (Linehan et al., 1999; 2002), this is the first study, to our knowledge, to assess the efficacy of an integrated treatment for adolescents with these problems. I-CBT relative to E-TAU was associated with greater reductions in heavy drinking days, days of marijuana use, and marijuana related problems over the course of treatment relative to E-TAU. Further, youth who received I-CBT reported less global impairment as well as fewer suicide attempts, psychiatric hospitalizations, emergency department visits, and arrests than those in the E-TAU condition. These results were achieved in a sample of adolescents with significant psychopathology who had an average of three years of prior mental health treatment provided by an average of two therapists before study entry. Given the acuity of the sample, it also noteworthy that these families could be enrolled in a clinical trial, and that 74% of the families in the I-CBT condition were retained for an intensive 6 month protocol that averaged 34 sessions per family.
Ultimately, the definition of a clinically significant effect depends on the condition being treated and the emotional costs to the individual and family if the treatment is unsuccessful. From this perspective, the effect that the I-CBT protocol had on suicidal behavior and service utilization, including repeat ED visits and hospitalizations, is particularly noteworthy. There were six adolescents who attempted suicide in the E-TAU condition compared to one adolescent in the I-CBT condition, and this latter participant dropped out of the I-CBT protocol prematurely. The results are even more impressive considering that three of the adolescents in the E-TAU condition were in residential treatment for most of the study period (241, 439, and 540 days).
Differences between groups in rates of attempted suicide in a psychiatric adolescent population have been found in only one other study. Huey et al. (2004) randomized adolescents presenting with psychiatric emergencies to either psychiatric hospitalization or multisystemic therapy (MST). MST is a family-focused behaviorally oriented home-based intervention. Controlling for prior history of suicide attempts, adolescents in the MST group reported fewer suicide attempts than the hospitalized adolescents. However, in the Huey et al. (2004) study, only 51% of youth were classified as suicidal so the samples are somewhat different. Notably though, in both the Huey et al. (2004) and the present study, numerous parent training and family sessions were provided in addition to individual adolescent sessions. Moreover, in our prior open pilot trial (Esposito-Smythers et al., 2006) that included a few family and no parent training sessions, 33.3% (2 out of 6) of adolescents attempted suicide while enrolled in the study in comparison to 5.3% (1 out of 19) of adolescents in the present study. These results suggest that work with the adolescent and their parents may yield the most promising results. Future research that compares individual work with suicidal youth with and without a significant parent training and/or family component may be warranted to empirically examine this question.
In comparison to family intensive studies for suicidal youth, those that have tested primarily individual interventions or treatment as usual plus a few family sessions (Donaldson et al., 2005; Harrington et al., 1998) have not affected suicide attempt rates. Further, there is mixed evidence in studies that examine group interventions for suicidal behavior. Wood, Trainor, Rothwell, Moore, and Harrington (2001) found that adolescents who received group therapy plus routine care, compared to routine care alone, were less likely to engage in 2 or more acts of deliberate self-harm (with or without suicidal intent) at 7 months post-treatment initiation follow-up (6% vs. 32%). No data was presented on rates of any deliberate self-harm. In a replication study (Hazell et al., 2009), youth in the group therapy plus routine care condition, versus routine care alone, were more likely to engage in some form of self-harm by 6 months post-treatment initiation (88% vs. 68%). No differences were found in rate of repetitive self-harm.
The limited number of studies that have found an effect on suicidal behavior makes the present study particularly noteworthy, albeit with the caveat that the stability of our findings are tempered by our small sample size. Nonetheless, the consistency of our findings across suicide attempts, emergency department visits, and inpatient psychiatric hospitalizations adds confidence to our results. In addition, I-CBT had equally strong effects on legal problems, specifically arrest rates, which bolsters our conclusions and draws attention to the need to treat both internalizing and externalizing problems in these multi-problem youths.
With respect to substance use, there were consistently greater reductions in the I-CBT condition relative to E-TAU on heavy volume alcohol use, marijuana use, and marijuana related problems. There were no significant effects on drinking days or alcohol problems. These results may reflect the greater emphasis that we placed on decreasing volume of alcohol intake relative to abstinence given that risk for suicidal behavior increases when adolescents are intoxicated (Esposito-Smythers & Spirito, 2004). Greater systematic monitoring of substance use (via self-report and urine drug screens), in combination with more adolescent, family, and parent training sessions that specifically addressed substance use in I-CBT relative to E-TAU, may underlie the positive findings on substance use. Indeed, a number of studies have found that interventions that combine individual therapy with a significant family component may yield greater reductions in adolescent substance use than individual or group based interventions (e.g., Latimer, Winters, Zurillo, & Nichols, 2003; Waldron et al., 2001).
Other possible reasons for the superiority of the I-CBT protocol relative to E-TAU for both suicidal behavior and substance use may have been the greater emphasis on cognitive behavioral techniques and adherence to the treatment protocol, as well as the potential synergistic effects of treating both conditions simultaneously using the same treatment modality. Indeed, participants in the I-CBT group reported receiving more cognitive behaviorally oriented treatment sessions than those in the E-TAU group. Number of sessions attended did not account for differences in treatment outcome across conditions.
In contrast to the consistently strong effects on behavioral outcomes, the effects on mental health symptoms were less impressive. There were no differences between groups on adolescent self-report of suicidal ideation or depressed mood, although both groups improved. There was a significant difference in adolescent self-report of anxiety favoring the I-CBT protocol over E-TAU. The lack of differences across groups in self-report of depressed mood and suicidal ideation, a symptom of depression, may reflect the fact that adolescents with the most severe depressive symptoms across study arms received psychiatric medications prescribed by the same board certified child psychiatrist. Indeed, comparable reductions in depressive symptoms and suicidal ideation have been found in prior work that has compared antidepressant medication alone to medication plus cognitive-behavioral therapy (e.g., Brent et al., 2008).
Though study results are of potential significance, the present study is subject to the limitations of Stage I behavior therapies development research (Rounsaville et al., 2001), including a small sample size and limited generalizability. The small sample size affects the stability of our findings and limited power to detect differences. Moreover, due to limited power and the importance of minimizing Type II error given the early state of research in this area, statistical correction was not applied to data analyses. Therefore, study results are limited by the potential of Type I error. Further, the study sample represents a small percentage of primarily White youth admitted to a psychiatric inpatient unit. Most hospitalized youth were screened out of participation because they did not endorse substance use during their hospital intake interview which was not kept confidential. Given that validity of adolescent self-report of substance use is enhanced when confidentiality is guaranteed (Needle, McCubbin, Lorence, & Hochhauser, 1983), it is likely that many eligible youth failed to disclose their use and were missed during screening. Indeed, many studies conducted with psychiatrically hospitalized adolescents yield much higher rates of co-occurring AOD and suicidality when confidentiality is guaranteed (e.g., D’Eramo et al., 2004; Brent et al., 1993). We also chose to screen out youth diagnosed with bipolar disorder and dependence on drugs other than alcohol or marijuana. This decision was made because the inpatient treatment team deemed them inappropriate for weekly therapy and referred them to more intensive treatment settings upon discharge (i.e., residential, day treatment, intensive outpatient). However, once stabilized in more intensive settings, such youth could potentially benefit from this protocol. Adolescents with co-occurring suicidality and AODs seen in other treatment settings (i.e., partial hospitalization, day treatment, intensive outpatient, emergency departments) would also be appropriate for this protocol.
In addition to the aforementioned limitations, we were unable to control medication use in this study for clinical and ethical reasons. However, we did have one study psychiatrist prescribe medications in an effort to control variability across conditions, and study results suggest relatively consistent prescribing practices across conditions. Prescribing algorithms would be difficult to implement with these multi-problem adolescents given their substantial past treatment history and the host of comorbid diagnoses. Another limitation is that substance use self-report data were not corroborated by either parents or peers. However, self-report of substance use was corroborated with urine toxicology screens and there is no reason to believe that any inaccurate reporting differed as a function of treatment condition. Relatedly, on occasion, the research assistants learned about participant treatment assignment. However, the only main outcome assessment that required research assistant guidance was the TLFB, and marijuana and abstinence related results of the TLFB were corroborated with toxicology screens.
Consistent with Stage I pilot trial work (Rounsaville et al., 2001), only the treatment development team conducted independent fidelity checks which is another limitation of this study. However, though extensive psychometric work has not been conducted on the revised Psychosocial Treatment Interview, it yielded data which suggests that adolescent’s learned CBT techniques consistent with the I-CBT protocol in treatment. Finally, we cannot say for certain whether the I-CBT protocol accounted for the positive effects or whether other integrated treatments based on different models, e.g. interpersonal therapy, delivered under similar conditions, would work equally well. We chose CBT as our model due to its applicability to both mental health and substance use problems.
Clinical Implications
Further testing of integrated CBT protocols for adolescent suicidality and AODs, as well as other potentially promising therapies for high risk behaviors (e.g., DBT), appears warranted. By addressing both suicidality and AODs in one protocol, the therapist is able to simultaneously monitor both conditions, obtain an understanding of their functional relationship for each client, and intervene accordingly. Some CBT techniques were reportedly used by therapists in the E-TAU condition. Therefore, it may not simply be the use of CBT techniques that is useful, but a comprehensive protocol, with repeated skill training, that may be necessary to affect change in this population. Moreover, the use of a consistent cognitive-behavioral conceptualization and orientation for both conditions yields a simpler treatment plan, allows for a consistent treatment message for clients, and provides clients with more practice with the same basic set of cognitive behavioral skills to facilitate skill mastery and generalization.
Acknowledgments
This research was supported by a grant from the National Institute of Alcohol Abuse and Alcoholism (R01 AA014191).
Contributor Information
Christianne Esposito-Smythers, George Mason University.
Anthony Spirito, Alpert Medical School of Brown University.
Christopher W. Kahler, Brown University Center for Alcohol & Addiction Studies/Alcohol Research Center on HIV
Jeffrey Hunt, Alpert Medical School of Brown University.
Peter Monti, Brown University Center for Alcohol & Addiction Studies.
References
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall; Saddle River, NJ: 1986. [Google Scholar]
- Bird HR, Shaffer D, Fisher P, Gould MS, Staghezza B, Chen JY, Hoven C. The Columbia Impairment Scale: Pilot findings on a measure of global impairment for children and adolescents. International Journal Of Methods in Psychiatric Research. 1993;3:167–176. [Google Scholar]
- Birmaher B, Brent D, Chiapetta L, Bridge J, Suneeta M, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Zelaney J. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. Journal of the American Medical Association. 2008;299:901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Wartella ME, Boylan MB, Moritz G, Baugher M, Zelenak J. Adolescent psychiatric inpatients’ risk of suicide attempt at 6-month follow up. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;21:95–105. doi: 10.1097/00004583-199301000-00015. [DOI] [PubMed] [Google Scholar]
- Burns B, Angold A, Magruder-Habib K, Costello E, Patrick M. Child and Adolescent Services Assessment (version 4.2) Durham, NC: Duke University; 1997. [Google Scholar]
- Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Donaldson D, Spirito A, Esposito-Smythers C. Treatment for adolescents following a suicide attempt: Results of a pilot trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:113–120. doi: 10.1097/00004583-200502000-00003. [DOI] [PubMed] [Google Scholar]
- Esposito-Smythers C, Walsh A, Spirito A, Rizzo C, Goldston D, Kaminer K. Working with the suicidal client who also abuses substances. Cognitive and Behavioral Practice. Advance online publication. 2011 doi: 10.1016/j.cbpra.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A. Adolescent substance use and suicidal behavior: A review with implications for treatment research. Alcoholism: Clinical and Experimental Research. 2004;28:77S–88S. doi: 10.1097/01.alc.0000127417.99752.87. [DOI] [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A, Uth R, LaChance H. Cognitive behavioral treatment for suicidal alcohol abusing adolescents: Development and pilot testing. American Journal of Addiction. 2006;15:126–130. doi: 10.1080/10550490601003631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer EMZ, Angold A, Burns BJ. Reliability of self-reported service use: Test-retest consistency of children’s responses to the Child and Adolescent Services Assessment (CASA) Journal of Child and Family Studies. 1994;3:307–325. [Google Scholar]
- Goldston D. Conceptual issues in understanding the relationship between suicidal behavior and substance abuse during adolescence. Drug and Alcohol Dependence. 2004;76S:S79–S91. doi: 10.1016/j.drugalcdep.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Erkanli A, Reboussin BA, Mayfield A, Frazier PH, Treadway L. Psychiatric diagnoses as contemporaneous risk factors for suicide attempts among adolescents and young adults: Developmental changes. Journal of Consulting and Clinical Psychology. 2009;77:281–290. doi: 10.1037/a0014732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned MS, Murray A, Comtois KA, Linehan MM. Treating co-occurring Axis I disorders in recurrently suicidal women with borderline personality disorder: A 2-year randomized trial of dialectical behavior therapy versus community treatment by experts. Journal of Consulting and Clinical Psychology. 2008;76:1068–1075. doi: 10.1037/a0014044. [DOI] [PubMed] [Google Scholar]
- Hazell PL, Martin G, McGill K, Kay T, Wood A, Trainer G, Harrington R. Group therapy for repeated deliberate self-harm in adolescents: Failure of replication of a randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:662–670. doi: 10.1097/CHI.0b013e3181aOacec. [DOI] [PubMed] [Google Scholar]
- Hawkins EH. A tale of two systems: Co-occurring mental health and substance abuse disorders treatment for adolescents. Annual Review of Psychology. 2009;60:197–227. doi: 10.1146/annurev.psych.60.110707.163456. [DOI] [PubMed] [Google Scholar]
- Huey S, Henggeler SW, Rowland MD, Halliday-Boykins CA, Cunningham PB, Pickrel SG, Edwards J. Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:183–190. doi: 10.1097/00004583-200402000-00014. [DOI] [PubMed] [Google Scholar]
- Johnson V, White HR. An investigation of factors related to intoxicated drinking behaviors among youth. Journal of Studies on Alcohol. 1989;50:320–330. doi: 10.15288/jsa.1989.50.320. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Bormaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for affective disorders and schizophrenia for school-aged children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test Manual. Circle Pines, MN: American Guidance Service; 1990. [Google Scholar]
- Latimer WW, Winters KC, D’Zurilla T, Nichols M. Integrated family and cognitive-behavioral therapy for adolescent substance abusers: A Stage I efficacy study. Drug and Alcohol Dependence. 2003;71:303–317. doi: 10.1016/s0376-8716(03)00171-6. [DOI] [PubMed] [Google Scholar]
- Liang K, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Linehan MM, Schmidt H, Dimeff LA, Craft C, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. The American Journal on Addictions. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Dimeff LA, Reynolds SK, Comtois AC, Welch SS, Heagerty P, Kivlahan DR. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug and Alcohol Dependence. 2002;67:13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- Needle R, McCubbin H, Lorence J, Hochhauser M. Reliability and validity of adolescent self-reported drug use in a family based study: a methodological report. International Journal on Addictions. 1983;18:901–912. doi: 10.3109/10826088309033058. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Reynolds Adolescent Depression Scale. 2. Lutz, FL: Psychological Assessment Resources; 2002. [Google Scholar]
- Reynolds WM, Kamphaus RW. Behavioral Assessment Scale for Children. Circle Pines, MN: American Guidance Service; 1992. [Google Scholar]
- Reynolds WM. Suicidal Ideation Questionnaire. Odessa, FL: Psychological Assessment Resources; 1985. [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies development research: Getting started and moving on from Stage I. Clinical psychology Science and Practice. 2001;8:133–142. [Google Scholar]
- SAS Institute Inc. SAS for Windows [Computer software] Cary, NC: SAS; 1997. [Google Scholar]
- Simons-Morton B, Haynie DL, Crump AD, Saylor KE, Eitel P, Yu K. Expectancies and other psychosocial factors associated with alcohol use among early adolescent boys and girls. Addictive Behaviors. 1999;24:229–238. doi: 10.1016/s0306-4603(98)00095-1. [DOI] [PubMed] [Google Scholar]
- Steketee G, Perry JC, Goisman RM, Warshaw MG, Massion AO, Peterson LG, Keller MB. The psychosocial treatments interview for anxiety disorders. A method for assessing psychotherapeutic procedures in anxiety disorders. Journal of Psychotherapy Research and Practice. 1997;6:194–210. [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol Timeline Followback Users’ Manual. Toronto, Canada: Addiction Research Foundation; 1995. [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Vallis TM, Shaw BF, Dobson KS. The Cognitive Therapy Rating Scale: Psychometric properties. Journal of Consulting and Clinical Psychology. 1986;54:381–385. doi: 10.1037//0022-006x.54.3.381. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcome for adolescent substance abuse at 4 and 7 month assessments. Journal of Consulting and Clinical Psychology. 2001;69:802–813. [PubMed] [Google Scholar]
- White HR, Lobouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Wood A, Trainor G, Rothwell J, Moore A, Harrington R. Randomized trial of group therapy for repeated deliberate self harm in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1246–1253. doi: 10.1097/00004583-200111000-00003. [DOI] [PubMed] [Google Scholar]
- Young J, Beck AT. Unpublished manuscript. University of Pennsylvania; Philadelphia: 1980. Cognitive Therapy Rating Scale manual. [Google Scholar]