Abstract
Juvenile ossifying fibroma is an uncommon, benign, bone-forming neoplasm with aggressive local growth that is distinguished from other fibro-osseous lesions primarily by its age of onset, clinical presentation and aggressive behavior. Although a benign entity, juvenile ossifying fibroma is known to be locally aggressive and has a high tendency to recur. Two distinctive microscopic patterns have been described: A trabecular variant and a psammomatoid variant. This latter variant is predominantly a craniofacial lesion and occurs rarely in the jaws. We present herein two cases of psammomatoid juvenile ossifying fibroma involving the jaws. The first case was a mandibular lesion in a 31-year-old female whereas the second case presented with maxillary involvement in a 46-year-old female. In addition, the pathology of the lesion was analyzed with confocal laser scanning microscopy.
Keywords: Confocal microscopy, fibro-osseous lesions, juvenile ossifying fibroma, psammomatoid
INTRODUCTION
Ossifying fibroma (OF) is a benign neoplasm of bone that has the potential for excessive growth, bone destruction, and recurrence.[1] Juvenile ossifying fibroma (JOF) is an uncommon lesion that has been distinguished from larger group of ossifying fibromas on the basis of age of the patients, most common site of involvement, and clinical behavior.[2] It is highly aggressive and has a strong tendency to recur.[3]
The term JOF is used in the literature to describe two distinct histopathologic variants of ossifying fibroma of the craniofacial skeleton namely psammomatoid juvenile ossifying fibroma (PsJOF) and trabecular juvenile ossifying fibroma (TrJOF). PsJOF was first reported by Benjamins, in 1938, who gave it the designation osteoid fibroma with atypical ossification of the frontal sinus. It was later termed psammomatoid ossifying fibroma of the nose and paranasal sinuses by Gögl, in 1949 and as juvenile active ossifying fibroma by Johnson et al. in 1952. Makek, in his review of 86 cases, considered the lesion to be a variant of osteoblastoma and termed it psammous desmo-osteoblastoma. Margo et al. in 1985 introduced the term psammomatoid juvenile ossifying fibroma.[4] Other names that have been used synonymously include psammo-osteoid-fibroma, psammous desmo-osteoblastoma, juvenile psammomatoid ossifying fibroma, and juvenile aggressive psammomatoid ossifying fibroma. Distinctive features of PsJOF include a predilection for the sinonasal complex and orbit of young people, an aggressive, infiltrative growth pattern, and a propensity for recurrence.[5] Here we report two cases of PsJOF, the first involving the maxilla and the second case involving the mandible. The histopathology of the lesion was also analyzed with the aid of confocal laser scanning microscopy as an attempt to view the psammoma bodies at higher resolution.
CASE REPORTS
Case 1
A 31-year-old female reported with a complaint of a swelling in the molar region of left mandible for past 2 years. Past history revealed that she had undergone treatment for a similar complaint at the same site 10 years back which was diagnosed as fibrous dysplasia. Intraoral examination revealed a diffuse, bony hard, nontender swelling of the left mandibular buccal cortex extending from mesial aspect of 35 to distal aspect of 37, superiorly from alveolar ridge in relation to missing 36 and cervical margin of 37 and inferiorly obliterating the vestibule. The swelling obliterated the buccal vestibule. An orthopantomograph showed a well-demarcated unilocular radiolucent lesion interspersed with areas of radiopacity extending anteriorly from mesial aspect of missing 35 up to distal aspect of 37 posteriorly [Figure 1]. Differential diagnosis of the lesion included fibrous dysplasia and ossifying fibroma. An incisional biopsy was done and the tissue was sent for histopathological examination.
Figure 1.
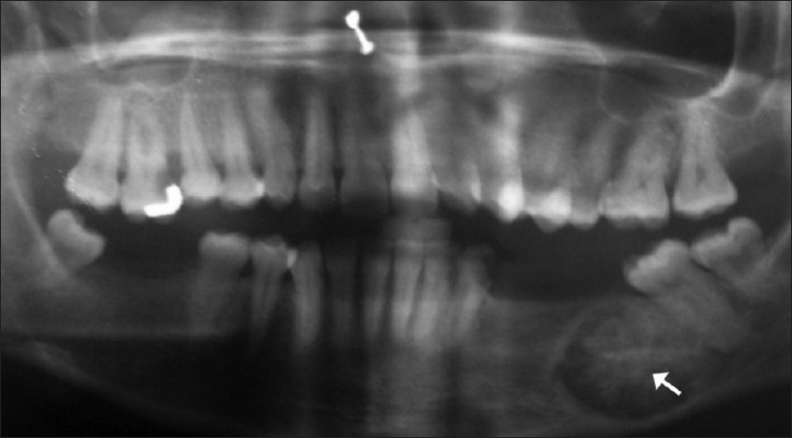
Orthopantamograph showing a unilocular radiolucent lesion interspersed with radiopaque areas in relation to 36, 37 (Case 1)
Case 2
A 46-year-old female presented with a growth in relation to right maxillary posterior tooth region for past 2 years. Past history revealed that the lesion was present for past 2 years, was slow growing, and showed a progressive increase in size for past 6 months. On intraoral examination, a diffuse proliferative mass was present in the right maxilla extending anteriorly from right permanent maxillary central incisor and posteriorly up to the maxillary tuberosity, laterally obliterating the mucobuccal sulcus and medially up to the midline of the palate. The lesion was soft, nontender and measured 4 cm × 3 cm × 2 cm approximately [Figure 2]. Radiographic examination showed a unilocular radiolucent lesion with areas of radiopacity extending from 11 anteriorly up to the maxillary tuberosity region posteriorly. The lesion did not show involvement of maxillary sinus. A provisional diagnosis of ossifying fibroma was made. Partial maxillectomy was done under general anesthesia and specimen was sent for histopathological examination. On macroscopic examination, the resected right maxillary segment along with 13 and root stump of 14 measured about 4 × 3 × 2 cm approximately, brownish white in color and varied from firm to hard in consistency [Figure 3].
Figure 2.
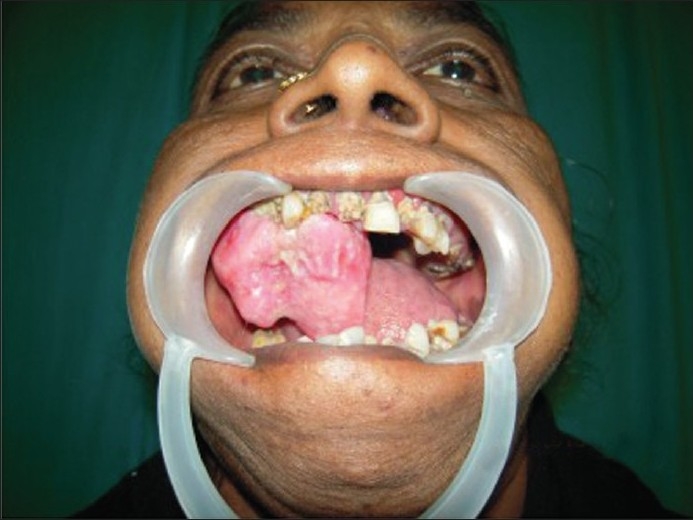
Intraoral view of the lesion (Case 2)
Figure 3.
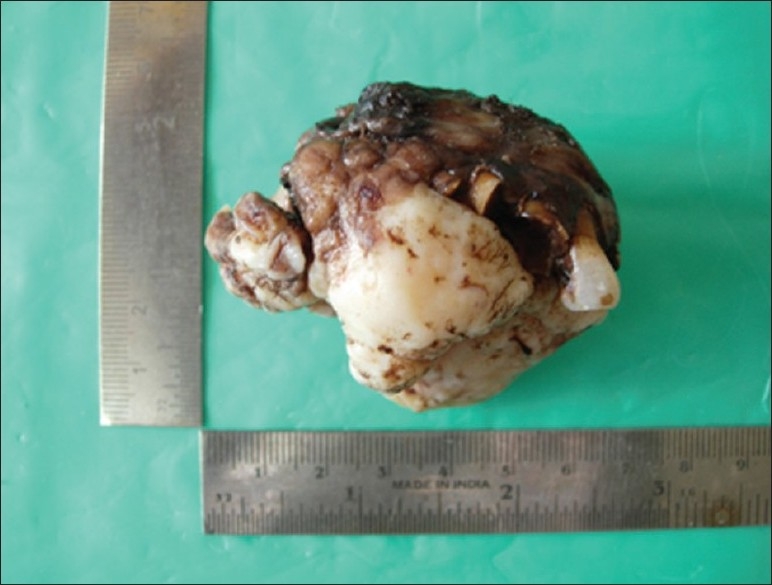
Macroscopic view of resected half of the maxilla (Case 2)
Microscopic examination of the lesional tissue in both the cases revealed cellular fibroblastic stroma containing spherical and curved ossicles [Figure 4]. Concentric lamellated ossicles resembling psammoma bodies were present [Figure 5]. Periphery of these ossicles showed a brush border which was blending into the surrounding stroma [Figure 6]. Confocal laser scanning microscopic examination of the tissue stained with alizarin red revealed the varying densities of calcifications in the psammoma bodies and brush borders in high resolution [Figures 7–9].
Figure 4.
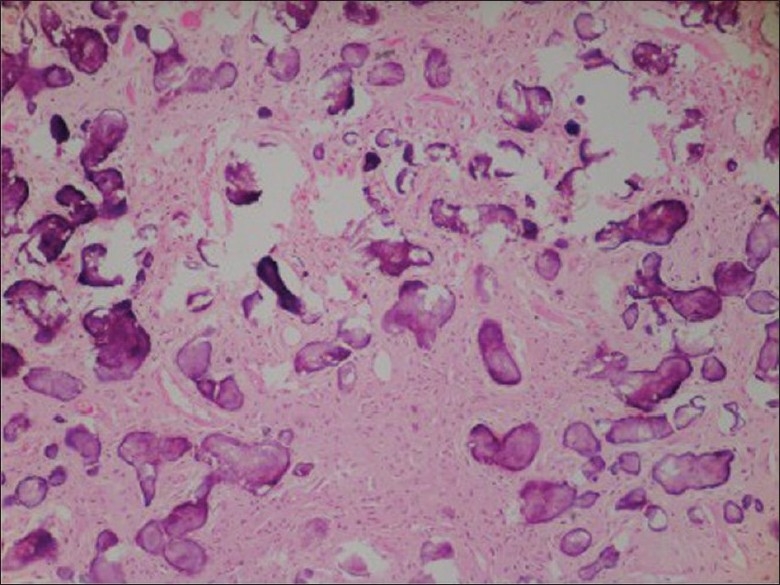
Photomicrograph showing cellular fibroblastic stroma containing spherical and curved ossicles (H and E, 10× – Case 1)
Figure 5.
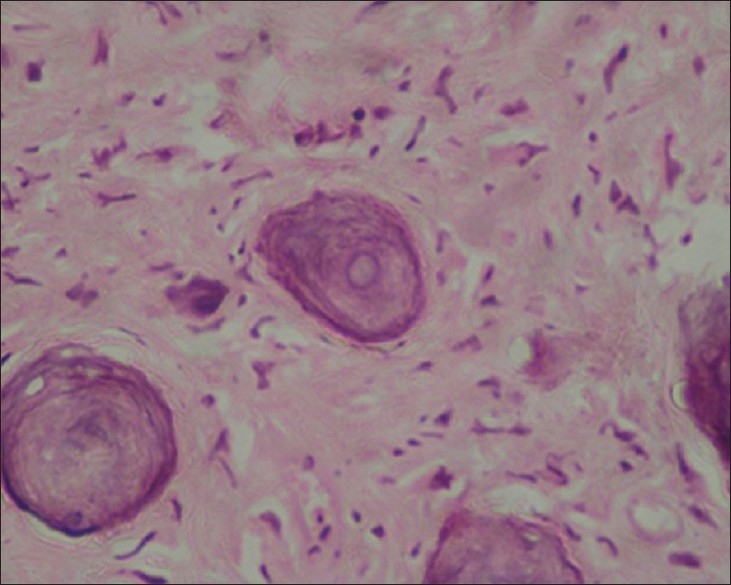
Photomicrograph showing concentric lamellated ossicles resembling psammoma bodies (H and E, 40× – Case 1)
Figure 6.
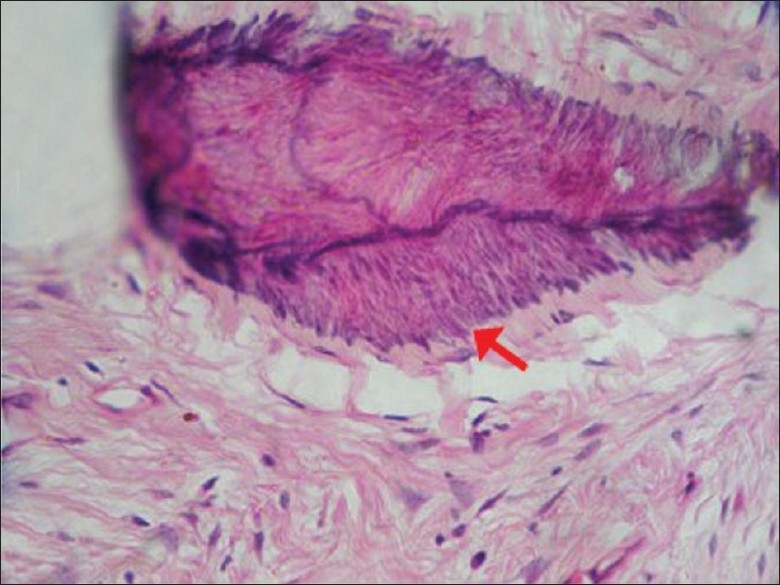
Photomicrograph showing periphery of these ossicles with a brush border which was blending into the surrounding stroma (H and E, 40× – Case 2)
Figure 7.
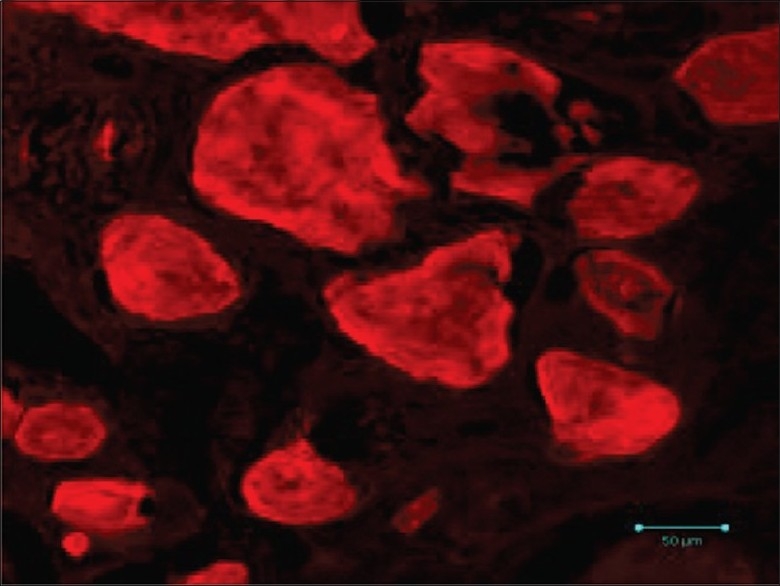
Confocal microscopic view of the psammoma bodies exhibiting varying densities of calcifications (alizarin red, ×40 – Case 1)
Figure 9.
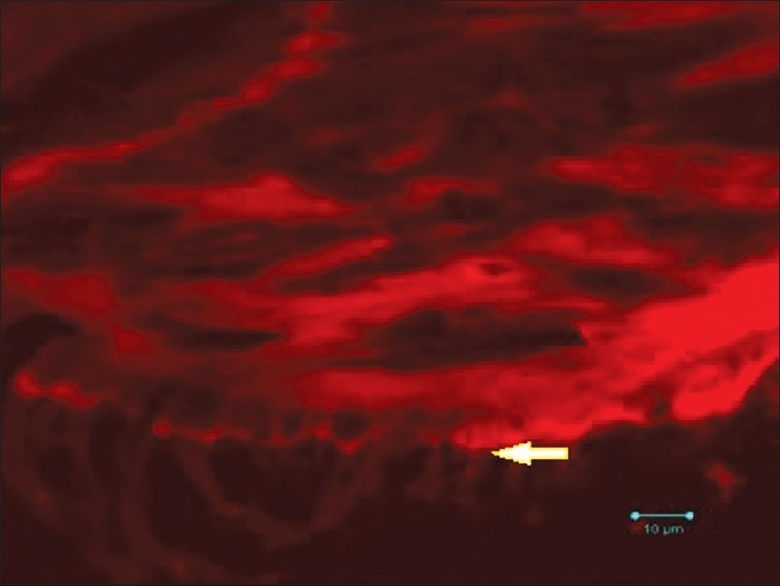
Confocal microscopic view (high power) of the psammoma bodies exhibiting varying densities of calcifications and brush border (Alizarin red, ×100 – Case 2)
Figure 8.
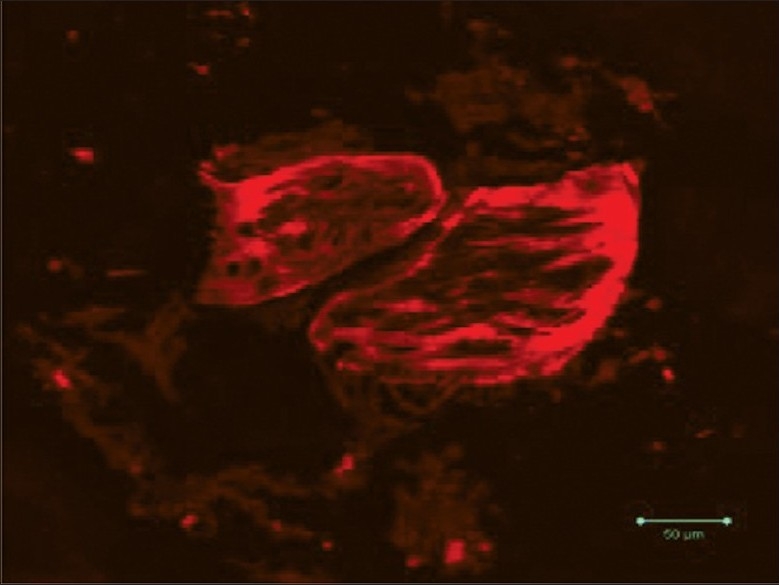
Confocal microscopic view of the psammoma bodies exhibiting varying densities of calcifications and brush border (alizarin red, ×40 – Case 2)
DISCUSSION
The spectrum of fibro-osseous lesions includes a variety of developmental, reactive or dysplastic lesions, and neoplastic entities.[6] Ossifying fibroma [ICD-O code-9262/0] is a well-demarcated lesion composed of fibrocellular tissue and mineralized material of varying density.[7] Juvenile ossifying fibromas are benign, potentially aggressive fibro-osseous lesions of the craniofacial bones. In addition to its aggressive behavior, it has a strong tendency to recur.[6] Recurrence and aggressive, infiltrative growth pattern which are characteristic of JOF were typically present in cases 1 and 2 respectively. The most characteristic feature of JOF, as the name suggests, is its higher incidence in children and young adults. However, its occurrence in the older age group has also been reported. Johnson et al. have reported JOFs occurring at any age between 3 months and 72 years.[3] The age of the patients in our report was 31 years and 46 years in cases 1 and 2 respectively.
Slootweg et al. classified JOF into two distinct groups, the JOF-WHO type and JOF-PO (psammoma-like ossicles) type, based on the difference in the age of occurrence; the mean age of JOF-WHO type is 11.8 years and that of JOF-PO is 22.6 years. Mofty identified two categories, trabecular JOF (TrJOF) and PsJOF, based on histologic criteria and predilection for specific age groups, the average age of occurrence of TrJOF being 81/2-12 years, whereas that of PsJOF being 16-33 years.[3]
Approximately 75% of PsJOFs develop in the orbit, paranasal sinuses, and calvaria, whereas only about 25% of all cases involve the maxilla or mandible.[8] PsJOF occurs overwhelmingly in the sinonasal and orbital bones of the skull, whereas TrJOF is predominantly a gnathic lesion affecting the jaws, with a predilection for the maxilla.[4] In our reported cases, case 1 involved the mandible whereas second case involved the maxilla. Multiple sites of origin have also been reported and these tumors behave aggressively.[9] The pathogenesis for these jaw lesions are related to the maldevelopment of basal generative mechanism that is essential for root formation.[6] The presence of nonrandom chromosomal breakpoints at Xq26 and 2q33 resulting in (x, 2) translocation have been reported.[2]
PsJOF is reported more frequently and in larger case series than is TrJOF. In a comprehensive review of the literature, the total number of cases of PsJOF reported exceeded that of the TrJOF by a ratio of more than 4 to 1 (230 vs. 55). Both the types showed predilection for males.[4] In our report, both the patients were females.
JOF manifests as an asymptomatic bony-hard swelling, the duration and extent of which may vary depending on the site and aggressiveness of the lesion; however it does not demonstrate the chronic, long-standing evolution of other fibro-osseous lesions.[3] TrJOF is characterized by a progressive and sometimes rapid aggressive growth.[4] Complications arising secondary to the neoplasm are typically result of the impingement on neighboring structures with persistent growth. Intracranial extension has been discovered in neoplasms arising adjacent to the cribriform plates.[2] Radiographically, the lesion can be radiolucent, mixed or radiopaque, depending on the degree of calcification. A “ground-glass” appearance on radiographs has been reported.[3]
Microscopically the lesion is characterized by a fibroblastic stroma containing small ossicles resembling psammoma bodies.[7] Gögl was the first to term these unique spherical structures as “psammoma-like bodies.”[6] The word “psammoma” is derived from a greek word “psammos” meaning “sand.”[10] Ultrastructurally, psammoma-like bodies in PsJOF were found to possess a dark rim of crystals from which small spicules and needle-like crystalloids project toward the periphery.[6] The stroma varies from being loose and fibroblastic to intensely cellular with minimum intervening collagen. The mineralized material consists of spherical or curved ossicles that are acellular or show sparsely distributed cells. Sometimes, PsJOF contains deeply basophilic concentrically lamellated particles as well as irregular thread-like or thorn-like calcified strands in a hyalinized background. Other features such as trabeculae of woven bone as well as lamellar bone, pseudocystic stromal degeneration, and hemorrhages result in areas similar to an aneurysmal bone cyst.[7]
PsJOF has to be distinguished from extracranial meningioma with psammoma bodies, which demonstrates EMA positivity. Moreover, the psammomatoid ossicles in PsJOF are clearly different from the acellular spherical true psammoma bodies.[7]
The clinical management and prognosis of JOF is uncertain. Smaller lesions can be simply excised with surrounding marginal bone. Larger lesions however warrant more aggressive surgical management. The recurrence rate for this lesion is about 30–60%.[10] Malignant transformation has not been documented.[2] Early detection and complete surgical excision followed by long-term follow-up bears importance in clinical management due to their aggressive nature and high recurrence rate.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Regezi JA, Sciubba JJ, Jordan RCK. Oral Pathology - Clinical Pathologic Correlations. 5th ed. India: Elsevier Publishers; 2009. p. 283. [Google Scholar]
- 2.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 3rd ed. India: Elsevier Publishers; 2009. p. 648. [Google Scholar]
- 3.Thankappan S, Nair S, Thomas V, Sharafudeen KP. Psammomatoid and trabecular variants of juvenile ossifying fibroma - two case reports. Indian J Radiol Imaging. 2009;19:116–9. doi: 10.4103/0971-3026.50832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Mofty S. Psammomatoid and trabecular juvenile ossifying fibroma of the craniofacial skeleton: Two distinct clinicopathologic entities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:296–304. doi: 10.1067/moe.2002.121545. [DOI] [PubMed] [Google Scholar]
- 5.Nwizu NN, George MD, Chen F. An agressive psammomatoid ossifying fibroma presenting as a sphenoethmoidal mass. N Am J Med Sci. 2010;3:24–27. [Google Scholar]
- 6.Solomon MC, Khandelwal SAR, Carnelio S. Psammomatoid juvenile ossifying fibroma of the mandible – A histochemical insight! Internet J Dent Sci. 2009;7 [Google Scholar]
- 7.Barnes L, Eveson WJ, Reichart P, Sidransky D. WHO Classification of Tumours - Pathology and Genetics - Head and Neck tumours. France: IARC press; 2005. [Google Scholar]
- 8.Alawi F. Benign fibro-osseous diseases of the maxillofacial bones - A review and differential diagnosis. Am J Clin Pathol. 2002;118(Suppl):S50–70. doi: 10.1309/NUXA-JUT9-HA09-WKMV. [DOI] [PubMed] [Google Scholar]
- 9.Syarifah NT, Roselinda AR, Irfan M. Juvenile Ossifying Fibroma of the Maxilla: A Case Report. Banglad J Med Sci. 2010;9:49–52. [Google Scholar]
- 10.Tamgadge SA, Tamgadge AP, Bhatt DM, Bhalerao S, Periera T, Gotmare S. Juvenile ossifying fibroma (Psammomatoid Type) of the maxilla. Scientific Journal. 2009;3:14–16. [Google Scholar]


