Abstract
Aims:
This study evaluated the effect of 2% chlorhexidine cavity disinfectant on microleakage in class II cavities restored with light cured composites using a single bottle adhesive in an in vitro model.
Materials and Methods:
Proximal box cavities were prepared on mesial and distal surfaces of 40 non carious mandibular third molars, resulting in total of 80 cavities. Forty cavities on were rinsed with normal saline and 40 cavities were rinsed with 2% chlorhexidine cavity disinfectant. All cavities were restored with a single bottle adhesive and nano hybrid composite resin. Microleakage was evaluated at the gingival margin using methylene blue dye penetration method.
Results and Conclusion:
Chlorhexidine cavity disinfectants produced significantly higher microleakage while restoring the cavities using a self-etching single bottle adhesive.
Keywords: Cavity disinfection, chlorhexidine, microleakage, self-etching adhesives
INTRODUCTION
Polymerization shrinkage appears to be the most significant problem with the composite restorations, as it has the potential to initiate gap formation at the tooth-composite interface,[1] which can lead to microleakage,[2] secondary caries,[3] and eventually leading to failure of the bond.[4] Although various generations of dentin bonding agents have been developed to reduce the effects of polymerization shrinkage, microleakge remains a problem of clinical significance.[2] The problems associated with microleakage can be magnified by the presence of viable microorganisms remaining after cavity preparation, which can result in secondary or residual caries.[5] Histologic and bacteriologic studies have shown that only a small portion of teeth is sterile after cavity preparation.[6] Anderson and Charbeneau (1985) found that even when the dentin enamel junction was cleared of all discoloration attributable to caries and was judged with an explorer to be sound, after using fuchsin stain to disclose caries, 59% of the teeth demonstrated staining at the dentin-enamel junction.[7] Various studies have shown that bacteria left in the cavity preparation can remain viable for a long duration.[8–10]
Based upon these evidences, the use of an antibacterial cavity cleanser has been recommended after cavity preparation to eliminate the potential risks due to bacterial activity.[6–8] Chlorhexidine has been recommended by various authors an effective agent to disinfect dentin.[11,12] It is also effective in reducing the levels of S. mutans found on exposed carious root surfaces.[11] It has been recently shown that Chlorhexidine preserves dentin bond strength by inhibiting host derived matrix metalloproteinases (MMPs).[13] However, any positive benefits would be negated if the solution affects the composite resin bond to dentin. The bond strength may be decreased by altering the ability of the hydrophilic resin to seal dentin.[14] This effect is more pronounced in single bottle adhesives than etch and rinse adhesives.[15]
The purpose of this study was to evaluate the effect of 2% chlorhexidine cavity disinfectant (Consepsis Ultradent) on microleakage at the gingival margins in cavities restored with single bottle adhesive (Adper Easy One 3M ESPE).
MATERIALS AND METHODS
Forty freshly extracted caries free, human permanent mandibular 3rd molars were used. Teeth were cleaned of debris and were stored in normal saline for a maximum period of one month. Proximal box-only cavities of standard dimensions were prepared on both proximal surfaces in all 40 samples resulting in 80 cavities. The occlusal portion of the preparation had a facio-lingual width of 1.5 mm. The gingival floor of the proximal box was kept 0.8–1.0 mm below the cemento enamel junction (CEJ) to keep the gingival margins in dentin. Each preparation was rinsed for 20 seconds with distilled water and dried with a blast of compressed air for 5 seconds. Caution was taken not to over dry the preparation. The samples were distributed into two experimental groups, each consisting of 40 cavities each. All the cavities were restored as given below.
Group I: Adper Easy One (3M ESPE) was applied according to manufacturer's instructions with a saturated micro brush and rubbed for 15 seconds. A gentle stream of air was applied to create a shiny film and was followed by a 10 second polymerization. A clear plastic matrix strip was placed. A nanohybrid restorative resin (Z 350 3M ESPE) was placed in the cavity in 2 mm increments. Each increment was cured for 20 seconds by a QTH (Vivadent) light cure unit. Curing was done initially from the occlusal direction and then from the buccal and lingual directions. After curing, the matrix strip was removed and gingival margins contoured with Composite polishing kit (Shofu Co., Japan).
Group II: A 2% chlorhexidine cavity disinfectant (Consepsis Ultradent) was applied with a sterile brush applicator. Consepsis solution consists of Chlorhexidine gluconate and ethyl alcohol with a pH of 6.0. The disinfectant stayed in contact with each tooth for 20 seconds followed by blast of compressed air for 5 seconds. Caution was taken not to over dry the preparation. After cavity disinfection, cavities were restored as in group I.
All teeth were stored in distilled water at 37°C for 24 hrs. The teeth were covered with two coats of nail varnish to within approximately 1.0 mm of gingival margin, after the root apices were sealed with modeling wax. The specimens were immersed in methylene blue dye in separate sealable vials at 37°C for 24 hrs. After staining the teeth were rinsed off to remove residual dye. The radicular parts of the teeth were cut 6 mm below the CEJ. Coronal parts were sectioned mesiodistally in the approximate center of the restorations with a diamond disks (Horico H557F220) in a straight air motor handpiece. Microleakage was assessed for gingival margins at ×30 magnification by two examiners according to the following scale.
0 – No dye penetration
1 – Up to 1/3rd of length of gingival margin
2 – Up to 2/3rd of length of gingival margin
3 – Covering full length of gingival margin
A nonparametric analysis of variance was used to determine whether there were significant differences among groups. Since the values for microleakage were described as categorical variables, group wise comparisons were made using categorical two way tables using proportions.
RESULTS
Since the data had categorical variables, the groups were compared using the proportions of samples with a particular score in each group. Two way tables of proportions were calculated and used for statistical evaluation using Kruskal-Wallis test [Table 1]. In 65% of cavities, which were restored without using chlorhexidine disinfectant, there was no microleakage, but number decreased to 35% after Chlorhexidine disinfectant application (P < 0.05). Moreover, chlorhexidine disinfectant application increased microleakage in all remaining 65% of samples [Figure 1]. Hence it was observed that Chlorhexidine disinfectant application increased microleakage in additional samples, where none existed and increased the microleakage in remaining samples.
Table 1.
Categorical two way proportions of samples showing microleakage in both the groups
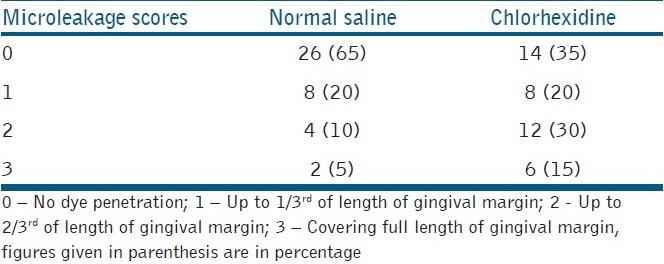
Figure 1.
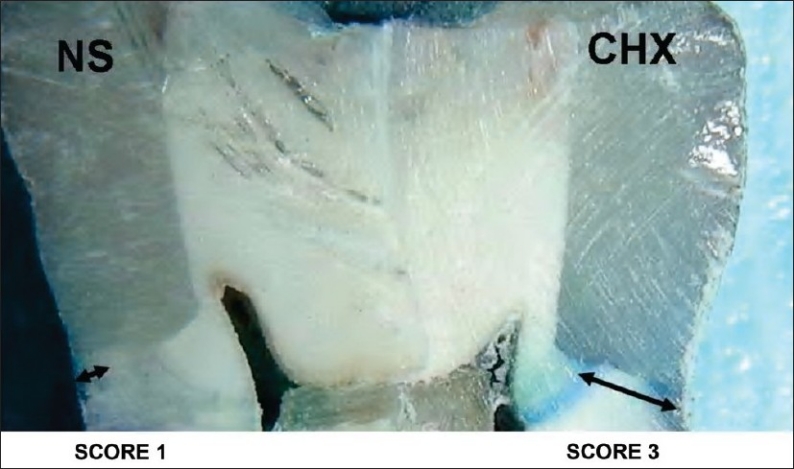
A ×30 magnification showing dye penetration covering the full length of gingival floor in chlorhexidine group and upto 1/3rd in normal saline group
DISCUSSION
A major cause of secondary caries is the presence of bacteria in the smear layer, after cavity preparation, which can remain viable for long periods of time.[5] An alternative approach to reduce residual bacteria is treatment with a cavity disinfectant.[6–8] Various cavity disinfectants have been used in the recent past including chlorhexidine,[11–13] fluoride gels, sodium hypochloride, and benzalkonium-based solutions,[16] but studies have reported adhesion could be impaired by a series of previous dentin treatments. Results of these studies are controversial with regard to whether the use of disinfectants in cavity preparations affects adhesion.[8,11,12,16]
Chlorhexidine is a broad spectrum antiseptic, and its use has been generalized over the past two decades for chemical control of bacterial plaque; the disinfection of therapeutic cavities has been adopted as a positive control for studies on bacterial growth or antibacterial activity. Previous studies have demonstrated that chlorhexidine application prior to acid-etching in etch and rinse adhesives, has no adverse effects on immediate composite-adhesive bonds in dentin,[17] enamel,[18] or with resin-reinforced glass-ionomer cements.[19] Recent studies have examined the use of chlorhexidine after acid-etching, demonstrating initial bond strengths comparable with those of the controls.[16,20–22] Also, some in vitro[20] as well as an in vivo[13] study demonstrates preservation of hybrid layers with chlorhexidine treatment after acid-etching.
However, it is still controversial whether the application of a chlorhexidine solution in a cavity preparation influences the effectiveness of a self etching adhesive and ultimately the marginal microleakage of resin composite restorations.[8,15,20] Self-etching primers combine dentin conditioning and a bonding agent in a single step. In such adhesive systems the acidic component of the primer dissolves the smear layer and incorporates it into the mixture as it demineralizes dentin and encapsulates collagen fibers and hydroxyappetite.[23–25]
Results of the present study have shown that use of 2% chlorhexidine disinfectant application increased microleakage in single bottle self etching adhesives. Self-etching adhesives have a pH relatively higher than phosphoric acid etchants. Scanning electron microscope examination by Meiers and Kresin[8] showed that cavity disinfectants applied to dentin surfaces were resistant to acidic conditioning. This acid-resistant layer might inhibit the ability of the weak acidic primers to effectively demineralize the dentin and hydrophilic resin to impregnate the dentinal surface.
Results of the present study differed from the conclusions obtained by some previous studies using carbide burs or lasers for cavity cutting. Various authors have concluded that a diamond stone produce more smear layer on the dentinal surfaces than the carbide burs and produces a surface, which is less conducive for bonding with self etching primers.[26,27]
Chlorhexidine is water soluble and dissociates at physiologic pH. It inhibits bacteria adherence to surfaces by competing with calcium for retention sites.[20] It also gets adsorbed by the smear layer and makes the dentinal surface acid resistant.[8] Our study indicates that the self etching primers might not effectively demineralize the acid-resitant dentinal tubules and subsequently incorporate the chlorhexidine adsorbed smear layer into them.
It is well documented that use of chlorhexidine as a cavity disinfectant has a definite beneficial role in etch and rinse adhesives, but it might adversely affect the resin dentin interface in single bottle self etching adhesives. Further clinical studies need to be conducted to verify the results obtained by the present study.
CONCLUSIONS
Within the limitations of this in vitro study, it can be concluded that use of 2% chlorhexidine cavity disinfectant increases the microleakage in cavities restored with light cured composites using a single bottle self-etching adhesives.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Asmussen E, Jorgensen KD. A microscopic investigation of the adaptation of some plastic filling materials to dental cavity walls. Acta Odontol Scand. 1972;30:3–21. doi: 10.3109/00016357209004588. [DOI] [PubMed] [Google Scholar]
- 2.Cheung GS. Reducing marginal leakage of posterior composite resin restorations: A review of clinical techniques. J Prosthet Dent. 1990;63:286–8. doi: 10.1016/0022-3913(90)90196-j. [DOI] [PubMed] [Google Scholar]
- 3.Retief DH. Do adhesives prevent microleakage? Int Dent J. 1994;44:19–26. [PubMed] [Google Scholar]
- 4.Lai JH, Johnson AE. Measuring polymerization shrinkage of photo activated restorative materials by a water-filled dilatometer. Dent Mater. 1993;9:139–43. doi: 10.1016/0109-5641(93)90091-4. [DOI] [PubMed] [Google Scholar]
- 5.Say EC, Koray F, Tarim B, Soyman M, Gulmez T. In vitro effect of cavity disinfectants on the bond strength of dentin bonding systems. Quintessence Int. 2004;35:56–60. [PubMed] [Google Scholar]
- 6.Brannstrom M. The cause of postoperative sensitivity and its prevention. J Endod. 1986;12:475–81. doi: 10.1016/S0099-2399(86)80202-3. [DOI] [PubMed] [Google Scholar]
- 7.Anderson MN, Charbeneau GT. A comparison of digital and optical criteria for detecting carious dentin. J Prosthet Dent. 1985;53:643–6. doi: 10.1016/0022-3913(85)90011-3. [DOI] [PubMed] [Google Scholar]
- 8.Meiers JC, Kresin JC. Cavity disinfectants and dentin bonding. Oper Dent. 1996;21:153–9. [PubMed] [Google Scholar]
- 9.Crone FL. Deep dentinal caries from a microbiological point of view. Int Dent J. 1968;18:481–8. [PubMed] [Google Scholar]
- 10.Leung RL, Loesche WJ, Charbeneau GT. Effect of dycal on bacteria in deep carious lesions. J Am Dent Assoc. 1980;100:193–7. doi: 10.14219/jada.archive.1980.0056. [DOI] [PubMed] [Google Scholar]
- 11.Fure S, Emilson CG. Effect of chlorhexidine gel treatment supplemented with chlorhexidine varnish and resin on Mutans Streptococci and Actinomyces on root surfaces. Caries Res. 1990;24:242–7. doi: 10.1159/000261275. [DOI] [PubMed] [Google Scholar]
- 12.Ersin NK, Aykut A, Candan U, Onçağ O, Eronat C, Kose T. The effect of a chlorhexidine containing cavity disinfectant on the clinical performance of high viscosity glass-ionomer cement following ART: 24-month results. Am J Dent. 2008;21:39–43. [PubMed] [Google Scholar]
- 13.Hebling J, Pashley DH, Tjaderane L, Tay FR. Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res. 2005;84:741–6. doi: 10.1177/154405910508400811. [DOI] [PubMed] [Google Scholar]
- 14.Gurgan S, Bolay S, Kiremitc A. Effect of disinfectant application methods on the bond strength of composite to dentin. J Oral Rehabil. 1999;26:836–40. doi: 10.1046/j.1365-2842.1999.00458.x. [DOI] [PubMed] [Google Scholar]
- 15.Meiers JC, Shook LW. Effect of disinfectants on the bond strength of composite to dentin. Am J Dent. 1996;9:11–4. [PubMed] [Google Scholar]
- 16.Bocangel JS, Kraul AO, Vargas AG, Demarco FF, Matson E. Influence of disinfectant solutions on the tensile bond strength of a fourth generation dentin bonding agent. Pesquisa Odontolóica Brasileira. 2000;14:107–11. [Google Scholar]
- 17.Perdigão J, Denehy GE, Swift EJ., Jr Effects of chlorhexidine on dentin surfaces and shear bond strengths. Am J Dent. 1994;7:81–4. [PubMed] [Google Scholar]
- 18.Filler SJ, Lazarchik DA, Givan DA, Retief DH, Heaven TJ. Shear bond strengths of composite to chlorhexidine-treated enamel. Am J Dent. 1994;7:85–8. [PubMed] [Google Scholar]
- 19.Cunningham MP, Meiers JC. The effect of dentin disinfectants on shear bond strength of resin-modified glass-ionomer materials. Quintessence Int. 1997;28:545–51. [PubMed] [Google Scholar]
- 20.Soares CJ, Pereira CA, Pereira JC, Santana FR, do Prado CJ. Effect of chlorhexidine application on microtensile bond strength to dentin. Oper Dent. 2008;33:183–8. doi: 10.2341/07-69. [DOI] [PubMed] [Google Scholar]
- 21.Brackett WW, Tay FR, Brackett MG, Dib A, Sword RJ, Pashley DH. The effect of chlorhexidine on dentin hybrid layers in vivo. Oper Dent. 2007;32:107–11. doi: 10.2341/06-55. [DOI] [PubMed] [Google Scholar]
- 22.Korkmaz Y, Baseren M. Effect of antibacterial varnishes applied to root dentin on shear bond strength of tooth-colored restorative materials. Oper Dent. 2008;33:65–71. doi: 10.2341/07-38. [DOI] [PubMed] [Google Scholar]
- 23.Chigira H, Yukitani W, Hasegawa T, Manabe A, Itoh K, Hayakawa T, et al. Self-etching dentin primers containing Phenyl-P. J Dent Res. 1994;73:1088–95. doi: 10.1177/00220345940730051101. [DOI] [PubMed] [Google Scholar]
- 24.Watanabe I, Nakabayashi N, Pashley DH. Bonding to ground dentin by a phenyl- P self-etching primer. J Dent Res. 1994;73:1212–20. doi: 10.1177/00220345940730061301. [DOI] [PubMed] [Google Scholar]
- 25.Tay FR, Pashley DH, Suh BI, Carvalho RM, Itthagarun A. Single-step adhesives are permeable membranes. J Dent. 2002;30:371–82. doi: 10.1016/s0300-5712(02)00064-7. [DOI] [PubMed] [Google Scholar]
- 26.Dias WR, Pereira PN, Swift EJ., Jr Effect of bur type on microtensile bond strengths of self-etching systems to human dentin. J Adhes Dent. 2004;6:195–203. [PubMed] [Google Scholar]
- 27.Barros JA, Myaki SI, Nor JE, Peters MC. Effect of bur type and conditioning on the surface and interface of dentine. J Oral Rehabil. 2005;32:849–56. doi: 10.1111/j.1365-2842.2005.01507.x. [DOI] [PubMed] [Google Scholar]


