Abstract
Background:
Interbody fusion surgery has been considered by many to be a treatment of choice for instability in lumbar degenerative disc disease. A posterior lumbar interbody fusion (PLIF) has the advantages of spinal canal decompression, anterior column reconstruction, and reduction of the sagittal slips from a single posterior approach. The PLIF using double cage was a standard practice till many studies reported comparable results and lesser complications with single cage. Iliac crest was considered as an appropriate source of bone graft until comparable spinal fusion rates using local bone graft and cage emerged. Till date, there has been no report of corticocancellous laminectomy bone chips alone being used for spinal fusion. In this paper, we present radiologic results of single level instrumented PLIF, where in only corticocancellous laminectomy bone chips were used as a fusion device.
Materials and Methods:
It is a retrospective cohort study of 35 consecutive patients, who underwent single level instrumented PLIF surgery, wherein only locally obtained bone chips was used for spinal fusion. The average follow-up was 26 months. The indications for the surgery were as follows: 19 patients had disc herniations, with back pain of instability type, normal disc height on radiology. Ten patients had grade 1 spondylolisthesis, with significant back pain and translational instability on radiography. Three patients were redo spine surgeries, and three patients had healed spondylodiscitis with significant back pain and instability. All patients were regularly followed up and decision of spinal fusion or no fusion was taken at 2 years using modified criteria of Lee.
Results:
Of total 35 patients, there were 24 males and 11 females, with a mean age of 41 years. There were 16 patients with definitive fusion, 15 patients with probable fusion, 04 patients with possible pseudoarthrosis, and no patient had definitive pseudoarthrosis. The mean time for fusion to occur was 18 months. The average loss of disc height, over 2 year follow up, was only 3 mm in 8 patients. Three patients had a localized kyphosis of more than 3° at the fusion level. The average blood loss was 356 ml and average operating time was 150 min.
Conclusion:
Corticocancellous laminectomy bone chips alone can be used as a means of spinal fusion in patients with single level instrumented PLIF. This has got a good fusion rate.
Keywords: Corticocancellous laminectomy bone chips, Interbody cage, posterior lumbar interbody fusion
INTRODUCTION
Interbody fusion surgery has been considered by many to be a treatment of choice for instability in lumbar degenerative disc disease.1 This is especially true with advent of pedicle screws for spinal fusion. A posterior lumbar interbody fusion (PLIF) has the advantages of spinal canal decompression, anterior column reconstruction, decompression of foraminal stenosis, and reduction of the sagittal slips from a single posterior approach.2 The PLIF using double cage has been a standard practice till recently. However, there are many studies now with PLIF using single cages with comparable results and lesser complications.3
With time there has also been an evolution in the type and techniques in bone grafting in the spinal fusion. Since the introduction of the PLIF procedure by Ralph Cloward, iliac crest has been considered as an appropriate source of bone graft, in terms of quality and quantity.4 However, many recent papers show comparable spinal fusion rates of iliac crest bone graft harvest with that of local bone graft and cage.5
Till date, there has been no report of corticocancellous laminectomy bone chips alone being used for spinal fusion. We present radiologic results of spinal fusion in patients with single-level instrumented PLIF, where in only corticocancellous laminectomy bone chips (no cage) were used to achieve fusion.
MATERIALS AND METHODS
It is a retrospective cohort study of 35 consecutive patients (24 males and 11 females), with an average age of 41.44 years (ranging from 21–62 years), who underwent single level instrumented PLIF surgery. The average follow-up period was 26 months (ranging from 12 to 55 months). All patients, with single level instrumented PLIF surgery, wherein only local bone pieces were used for spinal fusion in place of cage were included in the study. These local bone chips were obtained by laminectomy and medial half facetectomy, during spinal decompression and were devoid of all soft tissue attachments. After discectomy the endplates were cleared of the cartilage. The local bone chips were prepared into the size of 3–5 mm in all dimensions and were inserted into anterior two-third of the disc space. The bone graft was impacted well using a bone graft impactor. The screw rod assembly was tightened and held in compression. Before wound closure, any free bone graft fragment pressing on neurological structures was removed. Of total, 19 patients had the pathology at the L4-L5 level, and 16 patients had pathology at the L5-S1 level [Figures 1–3]. The indications for surgery included, spinal instability due to the following pathologies. Of these, there were 19 patients who had disc herniations (02 were recurrent discs) with back pain of the instability type, normal disc height, and spinal instability on radiology. Ten patients had significant back pain and grade 1 translational instability on radiography (three were degenerative spondylolisthesis), three cases were redo spine surgeries who underwent spinal fusion for instability following previous surgery and three patients had healed spondylodiscitis (one was healed TB) with severe back pain of instability type as an etiology for PLIF.
Figure 1.
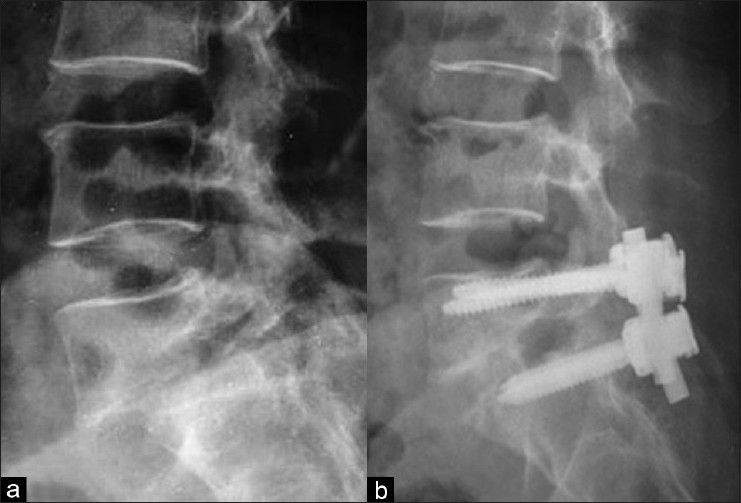
(a) Preoperative X-ray of lumbar spine (lateral view) showing Grade 2 lytic listhesis. (b) X-ray lumbosacral spine (lateral view) showing grade 1 fusion after instrumented laminectomy bone chip PLIF
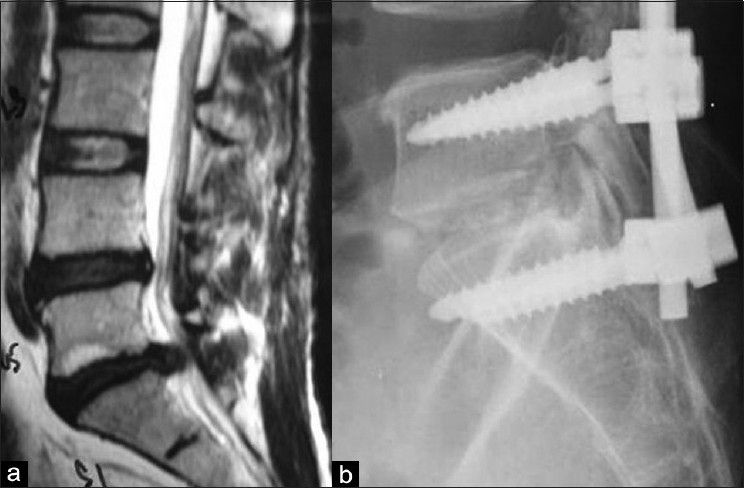
Figure 3.
(a) T2W sagittal MRI showing L5-S1 prolapsed intervertebral disc. (b) X-ray of lumbar spine (lateral view) showing grade 3 fusion after instrumented laminectomy bone chip PLIF
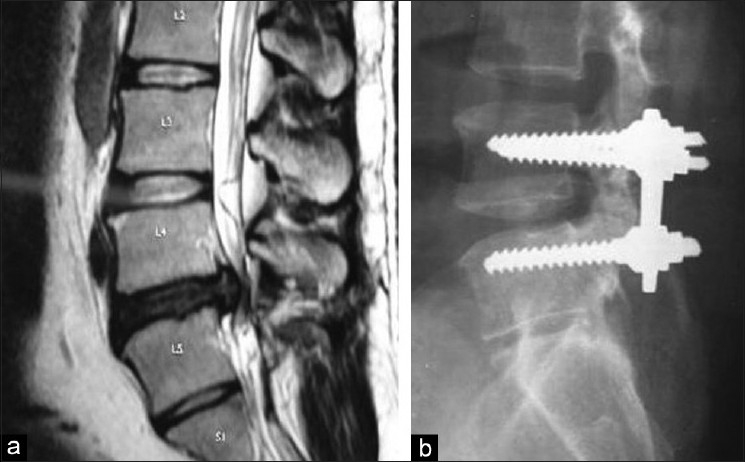
Figure 2.
(a) T2W sagittal MRI of lumbosacral spine showing L5-S1 prolapsed intervertebral disc. (b) X-ray of lumbar spine (lateral view) showing grade 2 fusion, after instrumented laminectomy bone chip PLIF
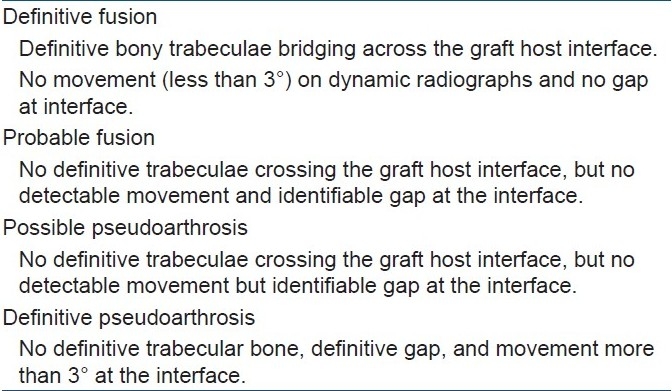
All patients were mobilized out of bed on their second or third postoperative day depending on pain compliance. Bending, sitting squatting, and lifting weights were allowed at 3 months. All these patients were followed up at regular intervals, three monthly for the first 6 months, followed by at 6 months in the first year and then yearly. Decision of fusion or no fusion was taken at 2 years following surgery. At each follow-up, all patients were assessed for spinal fusion by an independent observer using modified criteria of Lee et al.6 as shown in Table 1.
Table 1.
Modified Lee's criteria of fusion
RESULTS
Of total 35 patients, there were 24 males and 11 females, with a mean age of 41.44 years (range 21-62 years). Twenty-six patients presented with radicular leg pain and 19 patients had low back pain as significant complaint, which failed to conservative treatment required surgical fusion. Modified Lee's radiological criteria were used to assess the spinal fusion. There were 16 patients with definitive fusion, 15 patients with possible fusion, 4 patients with possible pseudoarthrosis, and no patient with definitive pseudoarthrosis. At 2 years follow-up, the average loss of disc height was only 3 mm in eight patients. In 10 patients with grade 1 spondylolisthesis, central decompression and root canal stenosis release were attempted; however, we did not aim reduction of the slip and correction of the slip angle. Of these, three patients at last follow-up had a localized kyphosis of more than 3° at the fusion level. The mean time for fusion to occur was 18 months. There was no patient with the pedicle screw loosening and implant failure in this series.
Five patients presented with preoperative neurologic deficits (MRC grade 4/5, n=04, 3/5n=1). Stainless steel variable screw placement (VSP) plates and screws were used in six patients for spinal instrumentation. In remaining patients, standard poly axial 6 mm pedicle screws of various brands were used for spinal instrumentation. The average blood loss was 356 ml (range 200-750 ml). The average operating time was 150 min (range 90-240 min).
DISCUSSION
The concept of using cages for interbody fusion evolved with the aim of restoring disc height in situations of collapsed degenerated discs and to afford immediate anterior load sharing construct without the morbidity of iliac crest site bone grafts.7 However, cages have many intrinsic disadvantages. The addition of a nonbiological “bulk” to the fusion area reduces the contact area available for bony fusion. Studies prove that the surface area of the end plate in contact with the local bone should be more than 30% of local bone.8 Also in the presence of interbody cage, visualization and assessment of spinal fusion status become difficult.9 The cage being a foreign body, thus makes their use controversial in patients with active infections and even in healed spondylodiscitis due to fear of re-infection.10 The differing modulus of elasticity of cages and the local bone it holds creates an unfavorable situation, making way for possible conflict with the adjacent weight bearing end plates and cage.11 Lastly, the high cost of cages remains an obvious disadvantage.
Using bone graft instead of a cage would offset most of the above disadvantages. Tricortical iliac crest graft has the comparative quality of a cage in terms of restoring disc height and affording instant anterior column support. The fusion rates achieved with iliac crest bone is as high as 90–100%.12 On the other hand, donor site, morbidity, and a possible second surgical incision are the obvious disadvantages. This surgery increases the operative time and blood loss. Iliac crest bone graft harvesting is associated with the donor site complication rate of 1–39%.13 Many of these complications are major requiring reinterventions and minor complications lasting for many months. Both these disadvantages can be circumvented by use of corticocancellous bone chips from the laminectomy performed.
The obvious advantages and disadvantages of using bone chips instead of a tricortical graft are as follows: Compared to tricortical bone, cortico-cancellous bone chips do not provide immediate anterior column support. However, in the presence of pedicle screws, the fixation becomes a fairly rigid construct. Given the current strength of the metals used in manufacturing pedicle screws, fatigue-related screw breakage is unlikely to occur within the first year.14 This time seems to be usually adequate for spinal fusion to occur.
This is especially true in this technique, where there is ample quantity of healthy corticocancellous autograft is in contact with large bone graft bed. This fact is exemplified in our series where we had no implant failures. Of course, one may want to be cautious in using this technique in cases with overt three column segmental instability like fractures or high grade/dysplastic listhesis. Restoration of disc height is not possible when using corticocancellous bone chips. This can, however, be easily achieved in most cases using the pedicle screws to maneuver the disc space as appropriate. A proper surgical technique with adequate discectomy and optimum lateral and facet release would contribute greatly to restoring the best possible disc height. In our series, the average loss of disc height, over a 2-year follow-up, was only 3 mm in 8 patients, further justifying this argument.
The best indications for this procedure would be (1) Primary fusion for degenerated discs with instability, where there is usually a lesser disc height loss. (2) Discitis, where cages might add to the problems of infection control. (3) Patients with osteoporotic vertebral bones, where the modulus of elasticity of the graft would best match than that of the vertebral bodies and cage. (4) The more demanding indications would naturally be spondylolisthesis where anterior load sharing and disc height restoration are more significant issues.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976) 1997;22:210–9. doi: 10.1097/00007632-199701150-00016. [DOI] [PubMed] [Google Scholar]
- 2.Sudo H, Oda I, Abumi K, Ito M, Kotani Y, Minami A. Biomechanical study on the effect of five different lumbar reconstruction techniques on adjacent-level intradiscal pressure and lamina strain. J Neuro Surg Spine. 2006;5:150–5. doi: 10.3171/spi.2006.5.2.150. [DOI] [PubMed] [Google Scholar]
- 3.Fogel GR, Toohey JS, Neidre A, Brantigan JW. Is one cage enough in posterior lumbar interbody fusion: A comparison of unilateral single cage interbody fusion to bilateral cages. J Spinal Disord Tech. 2007;20:60–5. doi: 10.1097/01.bsd.0000211251.59953.a4. [DOI] [PubMed] [Google Scholar]
- 4.Molinari RW, Sloboda J, Johnstone FL. Are 2 cages needed with instrumented PLIF.A comparison of 1 versus 2 interbody cages in a military population? Am J Orthop (Belle Mead NJ) 2003;32:337–43. [PubMed] [Google Scholar]
- 5.Ito Z, Matsuyama Y, Sakai Y, Imagama S, Wakao N, Ando K, et al. Bone union rate with autologous iliac bone versus local bone graft in posterior lumbar interbody fusion. Spine (Phial Pa 1976) 2010;35:E1101–5. doi: 10.1097/BRS.0b013e3181de4f2e. [DOI] [PubMed] [Google Scholar]
- 6.Lee CK, Vessa P, Lee JK. Chronic disabling low back pain syndrome caused by internal disc derangements. The results of disc excision and posterior lumbar interbody fusion. Spine (Phila Pa 1976) 1995;20:356–61. doi: 10.1097/00007632-199502000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Okuyama K, Kido T, Unoki E, Chiba M. PLIF with a titanium cage and excised facet joint bone for degenerative spondylolisthesis in augmentation with a pedicle screw. J Spinal Disord Tech. 2007;20:53–9. doi: 10.1097/01.bsd.0000211243.44706.2b. [DOI] [PubMed] [Google Scholar]
- 8.Closkey RF, Parsons JR, Lee CK, Blacksin MF, Zimmerman MC. Mechanics of interbody spinal fusion. Analysis of critical bone graft area. Spine (Phila Pa 1976) 1993;18:1011–5. doi: 10.1097/00007632-199306150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Sprit M, Meijers H, Obradov M, Anderson PG. CT density measurement of bone graft within an intervertebral lumbar cage: Increase of hounsfield units as an indicator for increasing bone mineral content. J Spinal Disord Tech. 2004;17:232–5. doi: 10.1097/00024720-200406000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Carmouche JJ, Molinari RW. Epidural abscess and discitis complicating instrumented posterior lumbar interbody fusion: A case report. Spine (Phila Pa 1976) 2004;29:E542–6. doi: 10.1097/01.brs.0000146802.38753.38. [DOI] [PubMed] [Google Scholar]
- 11.Adam C, Pearcy M, Mc Combe P. Stress analysis of interbody fusion–finite element modelling of intervertebral implant and vertebral body. Clin Biomech (Bristol, Avon) 2003;18:265–72. doi: 10.1016/s0268-0033(03)00022-6. [DOI] [PubMed] [Google Scholar]
- 12.Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM. Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: Two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine (Phila Pa 1976) 2000;25:1437–46. doi: 10.1097/00007632-200006010-00017. [DOI] [PubMed] [Google Scholar]
- 13.Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma. 1989;3:192–5. doi: 10.1097/00005131-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Gaines RW., Jr The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82-A:1458–76. doi: 10.2106/00004623-200010000-00013. [DOI] [PubMed] [Google Scholar]


