Abstract
Background:
Standard treatment of chronic infected total knee arthroplasty (TKA) is a two-stage revision, the first step being placement of an antibiotic-impregnated cement spacer. Here we describe the results of a new technique (modification of the Goldstien's technique) for intraoperative manufacture of a customized articulating spacer at minimal cost and with relatively good conformity and longevity.
Materials and Methods:
Thirty-six infected knees underwent this procedure from June 2002 to May 2007. The technique consists of using the freshened femur and tibia interface as molds wrapped in a tin foil for manufacturing the two components of the spacer with antibiotic-impregnated methyl methycrylate cement. We used the spacer and the femoral component of the trial set of a TKA system to mold them to perfect articulation. We also reinforced the spacer with a K-wire scaffold to prevent fracture of the cement mantle in the last 21 cases.
Results:
All 36 knees showed excellent results in terms of infection control, mobility, and stability. There was significant improvement in the WOMAC and Knee Society Scores (20 and 39 points respectively). There were two fractures of the spacers in the initial 15 cases that did not have K-wire scaffolding but none in the last 21 that had reinforcement.
Conclusion:
This technique provides a more conforming spacer, with good range of motion and stability. The reinforcement helps in preventing the fracture of the cement mantle and is cost effective.
Keywords: TKA, antibiotic spacers, articulating cement spacer
INTRODUCTION
Total joint arthroplasty is one of the most frequently done and successful surgeries in recent times. Infection after total joint arthroplasty when occurs has devastating results. With the increasing incidence of total knee arthroplasty (TKA), the incidence of infected TKA is also on the rise. Infection at the site of a total knee arthroplasty can be classified into four basic categories: type I (early postoperative), type II (late chronic), type III (acute hematogenous), and type IV (positive intraoperative cultures but clinically unapparent infection). The current standard of care for late chronic infection is considered to be two-stage revision arthroplasty, including removal of the prosthesis and cement, thorough debridement, placement of an antibiotic impregnated cement spacer, a course of intravenous antibiotics, and a delayed second stage revision arthroplasty.1–6 The different types of spacers available are either articulating or non-articulating, pre-fabricated or custom-made, and those made on table with or without moulds.
Articulating spacers are better than non-articulating ones as they provide mobility to the knee besides controlling infection. The cost of the commercially available articulating spacers is quite high. Pre-fabricated spacers are a costly alternative for an already burdened patient. Here we describe a new technique (a modification of Goldstein's technique7) for intraoperative manufacture of a custom-made antibiotic impregnated articulating spacer, with minimal cost and good conformity. We assess the results of this technique in a larger series of patients than in the original series7 and also assess the effect of the modification that we have introduced.
MATERIALS AND METHODS
This is a retrospective study which conducted on twenty eight patients with thirty six infected total knee arthroplasty (eight were bilateral) from June 2002 to May 2007. Eighteen of the 28 patients were females. The average age of the patients was 62 years (range:50–76 years). Of the 36 knees, 26 were cases of primary osteoarthritis, while the other 10 were rheumatoid knees. We included only type II (late chronic) infections for this study. The diagnosis was made on basis of clinical examination, labotary investigations and radiographic evaluation. The clinical findings included pain, warmth, redness, severe restriction of movement and frank discharging sinuses. Laboratory values showed elevated total counts with neutrophilia, along with persistent elevated ESR and CRP. All these patients had taken conservative trial of debridemnt and antibiotics and this operation was only suggested once there was radiographic evidence of loosening of the implants. The average time between the original surgery and this surgery was 10 months 8 days (range: 7 months to 1 year 4 months). The new technique is a modification of the original technique described by Goldstein et al.7 All these operations were performed by the same main surgeon (PG) in the same institute. Assessment was done on the basis of the following parameters: 1) wound healing and infection subsidence (on the basis of clinical examination and serial ESR and CRP); 2) functional results and patient satisfaction (on the basis of range of motion, Knee Society Score and WOMAC score); and 3) cost-effectiveness.
Operative procedure
Step 1 – Removal of implants and debridement
The prosthesis and all foreign material was removed and a thorough synovectomy was performed. The fluid and tissue obtained from the joint was sent for culture. The copious lavage with saline solution was done.
Step 2 – Preparation of the cement
The two packets of polymethyl methacrylate high viscosity cement (40 gm each), one each for the femoral and tibial component, were used for every case. Hand mixing was done. 5 ml of dextran was added for porosity as this leads to better elution of the antibiotics.8 2.4 gm of tobramycin, 2 gm of vancomycin, and 1.5 gm of cefuroxime in powder form was added because of heat resistant.9
Step 3 – Preparation of the femoral component
Aluminium foil of 0.05-mm thickness was autoclaved and then carefully wrapped around the freshened femur condyles so as to create all the defects and projections on the surface. The foil was then coated with a sterile lubricant (lignocaine jelly) in order to prevent it from sticking to the cement. Finally, the prepared cement was molded over the foil in uniform manner. A sterile trial plastic spacer or monoblock was used as a mold to give anatomical shape to the distal articulating part of the femoral spacer. The upper surface of the spacer is the surface that this component is finally going to articulate with, and this simple technique provides an exact conformation of the distal articulating surface. Also, the smooth surface of the spacer provides a smooth finish to the cement, preventing the rough surfaces and the friction and wear seen with the normal hand-moulded spacers. A groove on the anterior surface of the spacer can also be made with the femoral component at the same time for better alignment of the patella, though this is not a necessary step. Once the cement hardens, it is removed and the foil is taken out; the spacer is then reapplied on the femur [Figure 1]. It sits well on the condyles because of exact conformity, giving it inherent stability. In all the operated knees a bone block was used for the femoral medullary canal and so we found no opening for it in any of our cases; we did not recreate the canal as it could be a potential site of infection.
Figure 1.
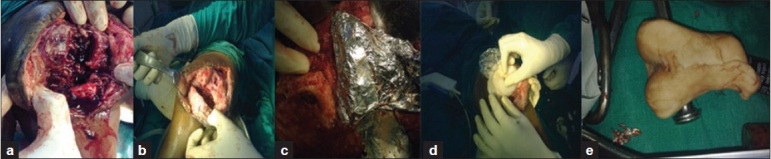
Intraoperative photograph showing (a) an infected knee after taking out the implants. (b) The same knee after extensive debridement. (c) Aluminium foil applied to femoral side. (d) Cement applied and molded with the spacer implant to prepare the femoral component. (e) The final prepared femoral component
Step 4 – Preparation of the tibial tray
Preoperative measurement of the tibial thickness is required for adequate soft tissue stretching. The tibial tray is prepared in a manner similar to the femoral side, with the aluminium foil and jelly covering the tibia now, using the sterile trial metallic femoral component of the same system to mould and shape the articulating surface giving a lock-and-key arrangement to the assembly. This is crucial step as it provides modularity to the spacers in terms of thickness. It is essential to maintain the needed thickness of the tibial component, which is determined preoperatively and confirmed peroperatively before this step [Figure 2].
Figure 2.
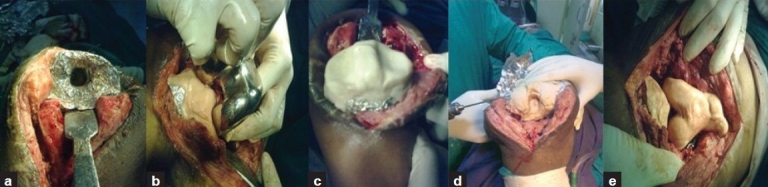
Intraoperative photograph showing (a) aluminium foil applied to the tibial side. (b) Moulding of the tibial component using the femoral implant. (c) final prepared tibial component. (d) modification: K-wire being drilled into the components before setting of the cement and then embedded within. (e) final component articulated and placed in position fit like a lock and key
Nine patients, five with unilateral affection could not afford a revision surgery. Three out of the five patients opted for arthrodesis. While rest two patients insisted on the spacer option The two bilateral patients also took this spacer option. To make the cement spacers last longer we reinforced the cement mantle with K-wires just before it hardens. At least one K-wire each is to be drilled, with the keel of the tibia and the intercondylar junction of the femoral component as they are the ones most prone to breakage. Additional more than one K-wire can be drilled parallel or perpendicular to the first K-wire. Care is to be taken to fully embed the k wire in the cement mantle.
Step 5 – Articulation and closure
The stability and mobility are checked by flexing and extending the knee joint once both the components are placed. Patellar tracking is also tested at the same time by the ‘no thumbs’ technique. The wound is closed in layers and the patient kept on IV cefuroxime till reports of cultures are available. Later on antibiotic was changed as guided by culture and sensitivity. The total duration for which antibiotics are given is usually 10–12 weeks. Serial ESR and CRP are done to evaluate the healing process. Immediate rehabilitation, with knee bending with partial weight bearing, was started so that maximum mobility can be attained. For the first 2 weeks the patients were allowed to walk with the help of a walker, after which they used a walking stick; the patients were weaned off the walking aids over a period of 4–8 weeks. Assessment was done on the basis of the following parameters: 1) wound healing and infection subsidence (on the basis of clinical examination and serial ESR and CRP); 2) functional results and patient satisfaction (on the basis of range of motion, Knee Society Score and WOMAC score); and 3) cost-effectiveness. Revision surgery was offered to the patients 3 months after complete subsidence of infection. Finally 29 patients opted for revision surgery while the rest could not afford a revision surgery.
RESULTS
All the knees were examined by the same surgeon, who was not a part of the operating team. All the patients were administered a questionnaire before the operation and 6 weeks after the operation and the results were evaluated.
Clinical evidence of wound healing and infection subsidence was evident in all 36 knees within a mean period of 3.5 weeks. The 10 rheumatoid knees took slightly longer than the other knees to heal (average: 4 weeks). Subsidence of infection was confirmed using serial CRP and ESR; these values coincided with clinical healing in all cases.
The average follow-up was 5 years and 2 months [Table 1]. Range of motion was increased by an average of 33°. The WOMAC function, pain, and stiffness scores also increased; the average increase of the combined WOMAC scores was 20 points. The Knee Society Score (clinical + functional) increased by an average of 39 points. We specifically questioned the patients for any feeling of stickiness or any scratching or grating sound caused due to the conventional rough surface of the hand-molded spacer, or any locking episodes due to the wear particles; none of the patients had any such symptoms.
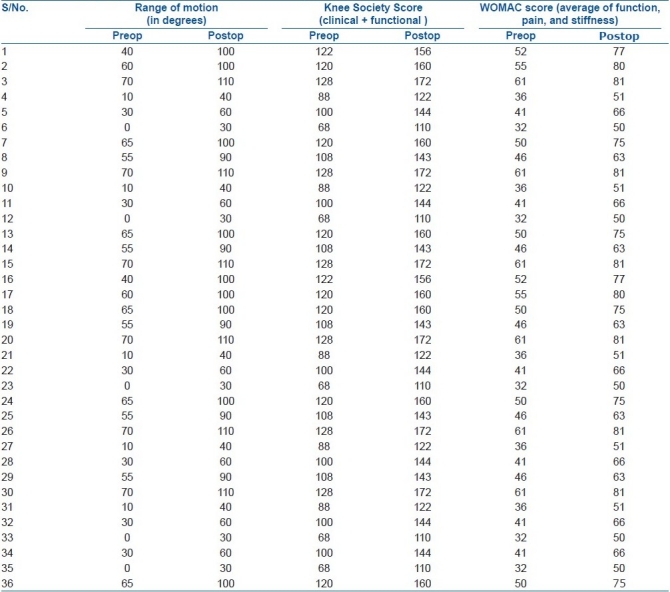
Table 1.
Pre and postoperative range of motion, Knee Society Score and WOMAC score
There were two cases of fracture of cement spacer in the first 15 cases that we operated without augmentation. The first case had a fracture 4 mo postoperatively while the second at 3 mo followup. In both cases it was the femoral component that fractured, leading to severe restriction of movement. Fortunately, the infection in both these cases had healed by this time and we could safely remove the spacer. We added a K-wire scaffold in the last 21 knees to prevent this complication. There was one case of a minor fracture of the tibial component in one of these 21 cases but it did not restrict motion and the patient continued motion and weight bearing. There was no major fracture in these 21 cases. We also had an intraoperative fracture of the cement cast when we drilled a K-wire into the bone rather than only through the cement. We had to use extra cement to re-prepare the spacer. The ability to change, reshape, or rebuild with just another extra packet of cement is a major advantage of this technique.
We compared the cost of the standard spacers used [Table 2]. Comparing the long-term costs (with regard to antibiotic usage and re-operations), since we got eradication of infection in all our cases without any re-operations, long-term cost effectively remain same or even better than other procedures.
Table 2.
Comparison of the cost of various spacers available
![]()
Out of the 36 knees, 29 went for a revision surgery after an average of 1.5 years (range: 6 months to 3.5 years). In all 29 cases, there was no difficulty in removing the spacer and there was minimum bone loss. There were no cases of reinfection in any of these cases. One bilateral case and three unilateral cases (five knees) did not go for revision due to financial constraints. All of them are still walking with the spacer, without any problems till last follow up. The average follow up of these 5 cases is 4 yrs [Figures 3 and 4] (range 3 years to 5.5 years) There was one death but this was 4 years after the patient underwent the spacer operation. One patient changed her address 4.5 years after the spacer operation and she was lost to follow-up.
Figure 3.
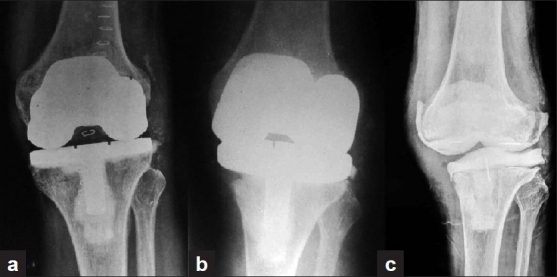
X-rays of knee joint showing (a) Infected TKA (anteroposterior view). (b) infected loose implants (lateral view). (c) X ray of same patient (lateral view) with spacer in for 4 years now and patients walking
Figure 4.

X-rays of knee joint showing (a) Primary TKA (anteroposterior view). (b) Spacer done after TKA became infected (anteroposterior view). (c) Patient walked with this spacer for an year (lateral view). (d) Patient had a revision TKA done with bone graft augmentation (anteroposterior view)
DISCUSSION
Two-stage exchange arthroplasty with an antibiotic-impregnated cement spacer remains the standard treatment for patients with an infected total knee arthroplasty.8 Static spacers not only reduce the range of motion of the knee joint but also cause capsular and quadriceps scarring and shortening, with subsequent difficulty in exposure at the second stage and the possibility of additional bone loss. Attempts to overcome these problems led to the development of prefabricated articulating spacer blocks. These had inherent problems like size discrepancy leading to early loosening, unsatisfactory antibiotic impregnation, inability to modify and redo the procedure on table and, most of all, high cost. These spacers lack modularity to increase or decrease the thickness of the spacers according to the bone loss and joint laxity.
Articulating spacers used in studies by Hoffman10 and Haddad11 and also the popular Prostalac® spacer have the inherent disadvantage of leaving some metallic component in the knee joint. We concur with Goldstein's thinking that any metal in the joint can act as a foreign body and as a potential surface for biofilm formation and bacterial proliferation.7
To make up for these disadvantages, intraoperative custom-made cement spacers were conceived. McPherson et al.12 and Ha et al.13 created spacers using only cement components, preparing them on the table and moulding them on the cut surfaces of the bones. The method does away with all metallic components and provides good conformation to the underlying bone. However, this approach requires technical perfection, as premature cement placement could result in interdigitation of the cement into the cancellous bone and, on the other hand, waiting until the cement is sufficiently thick may result in poor conformity of the implant and a loose fit. Only with a perfect cementing technique is bone loss minimized. Ha used Hohmann retractors and osteotomes for moulding the spacers, but we did not find this very convenient for creating good articulating surfaces. There are also cement spacers that can be made intraoperatively using moulds, which cost a little less than the prefabricated spacers, but most of the above mentioned problems still persist in these spacers.14
Our technique was devised to solve some of these problems. Using the aluminium foil prevents the danger of interdigitations of cement with bone. It also gives us sufficient time to mould, modify, or change the block and shape it perfectly for articulation. We think that using the cleaned prosthesis to mould the surfaces is the easiest and the most conforming way to produce good articulation. We would like to stress here that no matter what technique is used the most important step of these operations is complete and thorough debridement of the infected tissues. If this step is compromised then all techniques will fail as the primary objective of this operation is control of infection.
The original technique described by Goldstein is what we followed in our first few cases. But soon we had a complication in the form of fracture of the femoral component. This is an inevitable consequence if we use a cement-only spacer and advice weight-bearing to the patient. Usually, this complication is not of much consequence as pointed out by the study of Meek et al.,6 but the study does not state how many of their patients took to full weight-bearing.
To overcome this problem we added K-wires to the spacers, drilled while the cement was setting. The K-wires provide a structural support and will go a long way in preventing fractures of the cement. Even if there is a break, our K-wire inlay keeps the major fragments together, giving a satisfactory result.
We advised second stage revision surgery once infection was controlled, usually 3 months after debridement and spacer. 29 did undergo revision anytime after 6 months. However, 5 which could be followed still continuing on spacer without fracture of cement spacer.
In our study we had two cases of fractures in the first 15 nonaugmented spacers we performed. In contrast, there were no significant fractures in the other 21 K-wire-augmented spacers. This clearly proves the advantage of using the K-wire framework to provide longevity to the spacer. On the downside, intraoperative fracture of the cement mantle due to anchorage of K-wire in bone is a possible complication. Also, drilling the K-wires in that short span of cement-setting time, along with the shaping of the spacer, is a difficult procedure and should be attempted only after the surgeon is familiar and practiced with the plain spacer.
One of our major concerns, and the reason for using this technique, was the cost. Infection in any arthroplasty is a huge financial burden for the patient and it is difficult to accept that the patient should pay more for an interim procedure like this than he/she did for the original procedure. The commonly used prefabricated spacer costs approximately 18 times the cost of our technique, while the local versions of the same cost around six times. This is a huge relief for the patients and an attractive option for some patients who would otherwise go for arthrodesis or amputation due to economic constraints. Some patients cannot ever afford a revision operation, and this system (especially the K-wire-augmented system, with its longevity) provides a mobile and effective solution for them. Since we achieved eradication of infection in all our cases without any re-operations, the long-term cost (which includes cost of antibiotics and re–operations) with our technique was effectively the same or even lower than with other techniques. Other factors like range of motion, patient satisfaction, and infection healing were comparable with that seen with any other types of spacer and depended more on the previous state of the knees. Theoretically, this technique does provide more conformation and therefore more stability to the knee, but this could not be measured objectively.
Overall, this is a simple technique that places only a minimal economic burden on the already burdened patient. It primarily serves to control infection, along with preservation of motion. With our modification it can last longer with lesser complications. On the strength of the excellent results achieved in this study we recommend this technique for all infected total knee cases to control infection before the final revision surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Insall JN, Thompson FM, Brause BD. Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am. 1983;65:1087–98. [PubMed] [Google Scholar]
- 2.Hsieh PH, Chen LH, Chen CH, Lee MS, Yang WE, Shih CH. Two-stage revision hip arthroplasty for infection with a custom-made, antibiotic-loaded, cement prosthesis as an interim spacer. J Trauma. 2004;56:1247–52. doi: 10.1097/01.ta.0000130757.53559.bf. [DOI] [PubMed] [Google Scholar]
- 3.Deshmukh RG, Thevarajan K, Kok CS, Sivapathasundaram N, George SV. An intramedullary cement spacer in total hip arthroplasty. J Arthroplasty. 1998;13:197–9. doi: 10.1016/s0883-5403(98)90099-7. [DOI] [PubMed] [Google Scholar]
- 4.Nazarian DG, de Jesus D, McGuigan F, Booth RE., Jr A two-stage approach to primary knee arthroplasty in the infected arthritic knee. J Arthroplast. 2003;18(7 Suppl 1):16–21. doi: 10.1016/s0883-5403(03)00343-7. [DOI] [PubMed] [Google Scholar]
- 5.Pitto RP, Spika IA. Antibiotic-loaded bone cement spacers in two-stage management of infected total knee arthroplasty. Int Orthop. 2004;28:129–33. doi: 10.1007/s00264-004-0545-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meek RM, Masri BA, Dunlop D, Garbuz DS, Greidanus NV, McGraw R, et al. Patient satisfaction and functional status after treatment of infection at the site of a total knee arthroplasty with use of the PROSTALAC articulating spacer. J Bone Joint Surg Am. 2003;85:1888–92. doi: 10.2106/00004623-200310000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Goldstein WM, Kopplin M, Wall R, Berland K. Temporary articulating methylmethacrylate antibiotic spacer (TAMMAS): A new method of intraoperative manufacturing of a custom articulating spacer. J Bone Joint Surg Am. 2001;83(Suppl 2 Pt 2):92–7. [PubMed] [Google Scholar]
- 8.Kuechle DK, Landon GC, Musher DM, Noble PC. Elution of vancomycin, daptomycin, and amikacin from acrylic bone cement. Clin Orthop Relat Res. 1991;264:302–8. [PubMed] [Google Scholar]
- 9.Raker DM, Vansow PC. Antibiotic elution from acrylic bone cement in clinical setting for spacers in knee and hip. Clin Orthop Relat Res. 1993;153:163–7. [Google Scholar]
- 10.Hofmann AA, Kane KR, Tkach TK, Plaster RL, Camargo MP. Treatment of infected total knee arthroplasty using an articulating spacer. Clin Orthop Relat Res. 1995;321:45–54. [PubMed] [Google Scholar]
- 11.Haddad FS, Masri BA, Campbell D, McGraw RW, Beauchamp CP, Duncan CP. The PROSTALAC functional spacer in two-stage revision for infected knee replacements. Prosthesis of antibiotic-loaded acrylic cement. J Bone Joint Surg Br. 2000;82:807–12. doi: 10.1302/0301-620x.82b6.10486. [DOI] [PubMed] [Google Scholar]
- 12.McPherson EJ, Lewonowski K, Dorr LD. Techniques in arthroplasty: Use of an articulated PMMA spacer in the infected total knee arthroplasty. J Arthroplasty. 1995;10:87–9. doi: 10.1016/s0883-5403(05)80105-6. [DOI] [PubMed] [Google Scholar]
- 13.Meek T, Muncie M, Tarbox TR, Higgins LL. Comparison of a static with a mobile spacer in total knee infection. Clin Orthop Relat Res. 2002;404:132–8. doi: 10.1097/00003086-200211000-00023. [DOI] [PubMed] [Google Scholar]
- 14.Kohl S, Krueger A, Roeder C, Hartel M, Kohlhof H, Schneider C, et al. An aluminium mould for intraoperative production of antibiotic-loaded PMMA knee prostheses. Acta Orthop. 2009;80:389–91. doi: 10.3109/17453670902876771. [DOI] [PMC free article] [PubMed] [Google Scholar]


