Abstract
Background:
Tendon transfer for radial nerve paralysis has a 100 years history and any set of tendons that can be considered to be useful has been utilized for the purpose. The pronator tress is used for restoration of wrist dorsiflexion, while the flexor carpi radialis, flexor carpiulnaris, and flexor digitorum superficialis are variably used in each for fingers and thumb movements. The present study was a retrospective analysis, designed to compare three methods of tendon transfer for radial nerve palsy.
Materials and Methods:
41 patients with irreversible radial nerve paralysis, who had underwent three different types of tendon transfers (using different tendons for transfer) between March 2005 and September 2009, included in the study. The pronator teres was transferred for wrist extention. Flexor carpi ulnaris (group 1, n=18), flexor carpi radialis (group 2, n=10) and flexor digitorum superficialis (group 3, n=13) was used to achieve finger extention. Palmaris longus was used to achieve thumb extention and abduction. At the final examination, related ranges of motions were recorded and the patients were asked about their overall satisfaction with the operation, their ability, and time of return to their previous jobs, and in addition, disabilities of the arm, shoulder and hand (DASH) Score was measured and recorded for each patient.
Results:
The difference between the groups with regard to DASH score, ability, and time of return to job, satisfaction with the operation, and range of motions was not statistically significant (P>0.05). All of the patients had experienced functional improvement and overall satisfaction rate was 95%. No complication directly attributable to the operation was noted, except for proximal interphalangeal joint flexion contracture in three patents.
Conclusion:
The tendon transfer for irreversible radial nerve palsy is very successful and probably the success is not related to type of tendon used for transfer.
Keywords: DASH score, radial nerve palsy, tendon transfer
INTRODUCTION
The grip is severely impaired following loss of radial nerve function as a result of loss of extention of wrist, metacarpophalangeal joint and thumb. If radial nerve does not show neural recovery following conservative or surgical repair, tendon transfer is considered the standard treatment. Tendon transfer for radial nerve paralysis has a 100 years history and any set of tendons that can be considered to be useful has been utilized for the purpose!1 However, a few of these sets of tendon transfers are in common usage nowadays. In summary, in all of them, the pronator tress (PT) is used for restoration of wrist dorsiflexion, while the flexor carpi radialis (FCR), flexor carpi ulnaris (FCU), and flexor digitorum superficialis are variably used in each for fingers and thumb movements (1 and 2). We could not find any studies comparing different sets of tendon transfer and only the results have been described for each. The present study compares the three methods that are routinely performed at our centers.
MATERIALS AND METHODS
41 patients who had undergone tendon transfers for isolated radial nerve paralysis between March 2005 and September 2009 entered the study. The proposal was approved by neuroscience research center and got a reference number by the ethics committee. The inclusion criteria were: a) Female who had undergone tendon transfer more than 6 months ago, b) Informed consent.
Absence of any other musculoskeletal disorder affecting the upper limb(s).
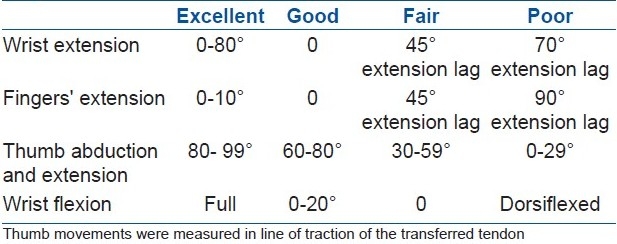
All of the surgeons were hand surgeons with especial interest in tendon transfer surgery and with at least 3 years of work experience. They had operated on the patients based on their education and experience and indeed each used one of the techniques for every patient. At the end of the follow-up period, the patients could be divided into the following three groups: The FCU group (group 1), the FCR group (group 2), and the flexor digitorum superficialis group (group 3). In all of the three groups, when necessary, restoration of wrist extension was restored by transferring PT to extensor carpi radialis brevis. In group 1, the FCU was used to restore fingers extension and in group 2, the FCR was utilized for the same purpose. In both groups, the palmaris longus was sutured to the rerouted extensor Pollicis longus to restore thumb abduction and extension. In group 3, the FDS of 3rd ray was used for fingers extension and FDS of 4th ray for thumb extension and abduction. For a note of clarification, it must be emphasized that patients in whom palmaris longus was absent and FCR or FCU had been transferred were excluded from the study. All of the tendons were passed subcutaneously to the target. After observing proximal interphalangeal (PIP) joint contraction in three of the patients in group 3, in whom the FDS tendon had been removed from the palm, just proximal to the A1 pulley, the surgeon modified the operation by making incision just proximal to the distal flexion crease of the wrist and removing the FDS tendons from there. For clearance, it must be notified that we did not perform Boy's Transfer, as in this technique, the FDS tendons are severed in the palm, are passed through the interosseous membrane and thumb extension and abduction are restored separately with FDS and FCR, respectively.1,2 No complications, including shortness of the tendons to reach the target, were observed. After the operation, a short arm splint with the wrist and fingers in extension was used for 4 weeks and then for 3 months at nights. All of the patients had undergone physiotherapy for one month after fulltime splint removal and after that, they were instructed to use their limbs as a practice without physiotherapy. At the final follow-up, the patient was interviewed and physical examination was performed. S/he was asked about overall satisfaction with the operation (yes/no), whether s/he would be willing to undergo the same operation on the opposite limb provided the same occurred to that, whether s/he has been able to return to her/his job, and finally when s/he had been able to use the limb usefully for daily activity (the time to maximum recovery). On physical examination, the related ranges of motion were recorded and the DASH Score was measured too. The ranges of motions were arbitrarily divided into four categories from simplicity of calculations: Excellent, good, fair, and poor [Table 1]. At the end, the data were analyzed with computer Pentium 4, using SPSS 16 software and by Analysis of variance, Chi square Kruskal-Wallis, and exact Chi square tests.
Table 1.
The criteria for range of motion of wrist, thumb, and fingers
RESULTS
A total of 41 patients were finally enrolled in the study, 18 in group 1 (14 men and 4 women), 10 in group 2 (9 men and 1 woman), and 13 in group 3 (10 men and 3 women). The mean age of the patients in the 3 groups did not show statistically significant difference (26.3 ± 9.7, 27.2 ± 9.1, and 27.3 ± 8.2 in the groups 1 to 3, respectively, P = 0.4) and so was about the sex distribution (P = 0.256). The mean follow-up period was 20 months, (range 6-36 mos). In 17 patients (41.5%), the dominant limb was involved in 24 (58.5%), the nondominant one. In eight patients, wrist extension was not affected, 2 in group 1, and 3 in groups 2 and 3, respectively. Statistical analysis revealed no significant difference between the three groups with regard to the ranges of motion of fingers, thumb, and wrist [Table 2]. Mean Dash score was 35, 38, and 30 and the mean time to job return was 4, 4.5, and 4 months for groups 1 to 3, respectively (P = 0.45). All of the patients had subjectively improved with the operation. 95% expressed willingness to undergo similar operation in opposite limb for similar clinical problem.
Table 2.
Range of motion of fingers, thumb and wrist in the three groups
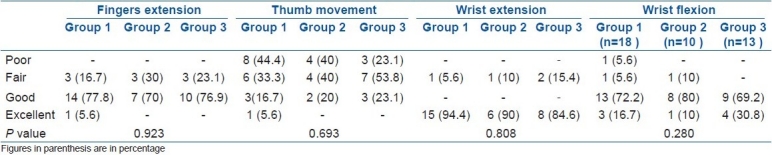
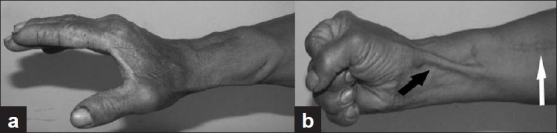
The ability to simultaneously extend the fingers and the wrist was observed only in four patients, all of group 3 [Table 3]. No complication directly attributable to operation was observed, except for PIP flexion contracture in the three patients of group 3. Forearm pronation was adequate in all of the patients. No patient complained of decreased wrist flexion, though actually it was found in many. All of the patients could make a fist without difficulty and none complained of decreased grip power, but grip power was not measured because of lack of equipment. We did not observe any cases of significant radial deviation of wrist in group 1 patients, even the two patients with low radial nerve palsy [Figures 1–3].
Table 3.
The ability of job return in the 3 groups
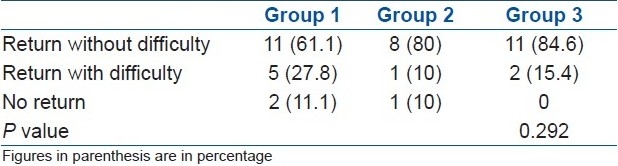
Figure 1.

Clinical photograph showing (a) clinical result of a patient with FCR transfer. Note that the fingers cannot be extended with the wrist extended. Note also the incision for PT transfer. (b) A patient with FCR transfer uses the tenodesis effect of the wrist flexion for fingers’ extension
Figure 3.
Clinical photograph showing (a) FDS transfer. Note excellent control of the thumb and fingers with the wrist in extension. (b) note the route of thumb extensor and abductor (black arrow) and the incision for PT transfer (white arrow)
Figure 2.

Clinical photograph showing incisions used for FCU transfer. Note the relatively large incision necessary for transfer
DISCUSSION
Drobnik (1894) the Polish surgeon performed the first transfer of the extensor carpi radialis longus to extensor digitorum communis tendon in a 4.5-year-old girl for radial nerve palsy.3 Many combination of tendon transfer are proposed since then. The tendon transfers are among the most successful surgical operations in the upper limb,1 and a review of literature may confirm the very satisfactory results with this operations, in concordance with the present one.4–12
At first glance, it may seem that a comparison between a synergistic (FCR, FCU) and a nonsynergistic (FDS) transfer is not a correct one. But all of them are standard transfers for radial nerve paralysis and the nonsynergistic transfer works well.1,10,11 The aim of the present study was to compare the results, regardless of the method and mechanism.
The use of FDS tendons for restoration of fingers and thumb movements was proposed by Boyes and later by Chuinard et al.10 Their major proof was the fact that amplitude of action and power of wrist flexors is too small to allow simultaneous extension of the wrist and fingers. Although theoretically this seems logical, in our and others’1,11 experience, this will not be achieved in all of the patients. Theoritically the FDS tendons have a common origin and removing one or two of them may “confuse” the muscle (in fact these patients may require more aggressive physiotherapy7 and this was our experience too that good control of fingers and thumb was achieved later in this group, though at the last follow-up, there was no difference) and second removing FDS tendons from a hand with previously weakened grip is not desirable. Further studies are necessary to answer these questions.
In group 3 patients of the present study, the FDS tendons were passed subcutaneously, the main reason being the fear of surgeon of “aggressiveness” of the operation and median nerve injury, which has been the concern of others too.13 We could not find a written reason for choosing the interosseous route for transfer of tendons, except probably for a better line of traction and again we do not see any clear proof that a tendon passed subcutaneously would not act as good as the one passed from the interosseous space, given the reverse is not true.2 Nevertheless, this emphasizes the need for studies in which “classic” FDS transfer has been performed.
PIP joint flexion contracture was observed in three patients in whom the FDS had been removed from the palm. This has been noticed by other surgeons too14–16 and some have advised preventive methods, such as full daily passive extension of the fingers14 and removing the tendon between A1 and A2 pulleys.16 In our experience, though not a vast one, if the tendon is going to be sacrificed for radial nerve palsy treatment, it can be removed from the wrist. Here again, we could not find a explanation for removing the tendon from the palm, as some length will be unnecessary.
The range of motion of thumb was similar in the three groups. It means that PL and FDS worked similarly in this regard. We cannot explain this finding as the amplitude of action of FDS is obviously greater. This may be compared with the point that many patients with FDS to EDC transfer will not achieve simultaneous wrist and fingers extension despite the theoretical fact. A noticeable finding of the present study is the absence of significant radial deviation in all of the patients in whom FCU was transferred. Again, we cannot explain this finding, except for probably the small sample size in this group or the small follow-up period, though it has been the finding of others too.5
At a glance, the best results have been of wrist extension reconstruction, so that 90% of the patients could extend their wrist at least to neutral. As the PT was used in all of the three patient groups, probably it may be concluded that the most successful result in radial nerve paralysis treatment by tendon transfers will be the wrist extension. In fact, neutral is the functional position and the one that has been proposed for wrist arthrodesis.17,18 Limitation of wrist flexion was noted in most of our patients, though actually none had any complaints of it. This must be due to the fact that less wrist flexion is necessary than extension in daily activities and fewer activities need it.18 Loss of wrist flexion was noted in both active and passive range of motions and must have been due to excessive tension on the transferred PT by the surgeons or less likely to prolonged immobilization after the operation.
The ability to return to previous job without difficulty was observed overall in 73.2% of the patients in the present study, while 19.5% had experienced some difficulties and 7.3% could not return at all, the distribution being even in the three groups. For simplicity and because of the relatively small sample size in each group, we did not provide “job groups,” but as we compared percents and ratios, probably this is not of much importance. All of the patients who had not returned to their job declared that they “had experienced difficulties with it,” which we could not find a good reason, probably insurance and workers’ compensation problems were involved too.
We did not measure the power of the grip because of lack of equipment. Though surely this is a limitation of the study, it may be considered that power of grip differs among individuals, and even between the two hands in the same individual, both sides cannot be of equal strength, so grip is not a good parameter for comparison. The fact that none of our patients had any complaints of a reduced power of grip may be due to their accommodation to the procedure or to the improvement in grip strength they experienced as a result of surgery. Despite this, we admit that FCU transfer may cause a decrease in grip power and some activities such as hammering and dart throwing are impossible without it and this is a limitation of the study. Perhaps, the most important limitation would be the fact that we did not measure the more detailed and specific scores of hand function such as “Jebsen-Taylor” test. In fact, we aimed to assess overall function of the upper extremity and not a detailed one. The other limitation is the failure to perform randomization, as the study was a retrospective one, and finally, the fact that we did not perform the classic Boyes tendon transfer for our patients.
The tendon transfer(s) is a very successful treatment for irreversible radial nerve paralysis and also probably is not dependent on the combination of tendon transferred.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Green DP. Radial nerve palsy. In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, editors. Green's operative hand surgery. 4th ed. Vol. 1. Philadelphia, Pensylvania: Churchil Livingston; 2003. pp. 1113–30. [Google Scholar]
- 2.Calandruccio JH, Jobe MT. Paralytic hand. In: Canale ST, editor. Campbell's operative orthopedics. 11th ed. Vol. 1. Philadelphia, Pensylvania: Mosby; 2008. pp. 4125–72. [Google Scholar]
- 3.Korteweg SF, van de Graaf RC, Werker PM. Who was the first in history to treat radial nerve palsy by tendon transfer? Plast Reconstr Surg. 2010;125:756–7. doi: 10.1097/PRS.0b013e3181c87b58. [DOI] [PubMed] [Google Scholar]
- 4.Ropars M, Dréano T, Siret P, Belot N, Langlais F. Long-term results of tendon transfers in radial and posterior interosseous nerve paralysis. J Hand Surg Br. 2006;31:502–6. doi: 10.1016/j.jhsb.2006.05.020. [DOI] [PubMed] [Google Scholar]
- 5.Raskin KB, Wilgis EF. Flexor carpi ulnaris transfer for radial nerve palsy: Functional testing of long-term results. J Hand Surg Am. 1995;20:737–42. doi: 10.1016/s0363-5023(05)80423-x. [DOI] [PubMed] [Google Scholar]
- 6.Chotigavanich C. Tendon transfer for radial nerve palsy. Bull Hosp Jt Dis Orthop Inst. 1990;50:1–10. [PubMed] [Google Scholar]
- 7.Kruft S, von Heimburg D, Reill P. Treatment of irreversible lesion of the radial nerve by tendon transfer: Indication and long-term results of the Merle d’Aubigné procedure. Plast Reconstr Surg. 1997;100:610–6. doi: 10.1097/00006534-199709000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Altintas AA, Altintas MA, Gazyakan E, Gohla T, Germann G, Sauerbier M. Long-term results and the disabilities of the arm, Shoulder, and hand score analysis after modified Brooks and D’Aubigne tendon transfer for radial nerve palsy. J Hand Surg Am. 2009;34:474–8. doi: 10.1016/j.jhsa.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Skoll PJ, Hudson DA, de Jager W, Singer M. Long-term results of tendon transfers for radial nerve palsy in patients with limited rehabilitation. Ann Plast Surg. 2000;45:122–6. doi: 10.1097/00000637-200045020-00004. [DOI] [PubMed] [Google Scholar]
- 10.Chuinard RG, Boyes JH, Stark HH, Ashworth CR. Tendon transfers for radial nerve palsy: use of superficialis tendons for digital extension. J Hand Surg Am. 1978;3:560–70. doi: 10.1016/s0363-5023(78)80007-0. [DOI] [PubMed] [Google Scholar]
- 11.Krishnan KG, Schackert G. An analysis of results after selective tendon transfers through the interosseous membrane to provide selective finger and thumb extension in chronic irreparable radial nerve lesions. J Hand Surg Am. 2008;33:223–31. doi: 10.1016/j.jhsa.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 12.Gousheh J, Arasteh E. Transfer of a single flexor carpi ulnaris tendon for treatment of radial nerve palsy. J Hand Surg Br. 2006;31:542–6. doi: 10.1016/j.jhsb.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Thomsen M, Rasmussen KB. Tendon transfers for defective long extensors of the wrist and fingers. Scand J Plast Reconstr Surg. 1969;3:71–8. doi: 10.3109/02844316909036698. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs B, Thompson TC. Opposition of the thumb and its restoration. J Bone Joint Surg Am. 1960;42:1015–40. [Google Scholar]
- 15.Richer RJ, Peimer CA. Flexor superficialis abductor transfer with carpal tunnel release for thenar palsy. J Hand Surg Am. 2005;30:506–12. doi: 10.1016/j.jhsa.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 16.North ER, Littler JW. Transferring the flexor superficialis tendon: technical considerations in the prevention of proximal interphalangeal joint disability. J Hand Surg Am. 1980;5:498–501. doi: 10.1016/s0363-5023(80)80084-0. [DOI] [PubMed] [Google Scholar]
- 17.Dabov GD. Arthrodesis of the shoulder, elbow and wrist. In: Canale ST, editor. Campbell's operative orthopedics. 11th ed. Vol. 1. Philadelphia, Pensylvania: Mosby; 2008. pp. 244–31. [Google Scholar]
- 18.Hastings H. (wrist) arthrodesis (Partial and Complete) In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, editors. Green's operative hand surgery. 4th ed. Vol. 1. Philadelphia, Pensylvania: Churchil Livingston; 2003. pp. 489–534. [Google Scholar]


