Abstract
The myositis ossificans around shoulder in military recruits are not reported yet. Three young male soldiers presented with complaints of palpable mass at the anterior aspect of shoulder; tenderness around the superior part of deltopectoral groove close to acromioclavicular joint; and restriction of shoulder motion. They also noticed ecchymosis and pain around the coracoid process and anterior shoulder region during regular firing exercises. Plain X-rays and computerized tomography showed extra-capsular, dense, irregular structure in the space between pectoralis and deltoid muscles which correlated with heterotopic bone. One patient refused surgical intervention because of the completion of his military serving period. Surgical excision was performed for the other two patients. During surgical exploration, both ossified masses were found in deltopectoral region and mostly in fibers of clavicular and acromial parts of deltoid muscle. Pathological reports confirmed the structure of masses as mature trabecular bone. Postoperatively indomethacin treatment and active shoulder exercises were started until the full range of motion was regained. Mini soft bag was used on the rifle contact area of the shoulder. No complications or recurrences were observed during the 24 months of followup period.
Keywords: Heterotopic ossification, military exercises, shoulder
INTRODUCTION
Heterotopic ossification is a well-recognized complication of spinal cord injury, closed head injury, total hip arthroplasty, burns and other traumas. It may be observed in various tissues, such as muscles, tendons, ligaments and menisci.1 Shoulder region is infrequently involved by heterotopic ossification, and most of the cases are related with neurologic diseases (coma, encephalitis, head and spinal injury).1–3 Ectopic bone formation with direct trauma to surrounding tissues of shoulder (by iatrogenic, e.g., surgical interventions; or non-iatrogenic, e.g., fracture, dislocation, soft tissue trauma) is rare.4,5 The term myositis ossificans describes heterotopic ossification that forms in muscle as a result of direct trauma.4 In the english language literature, there is no study about myositis ossificans at the shoulder region related to military arm exercises to the best of our knowledge. We report occurrence of myositis ossificans at the shoulder region of three soldiers, seen after execution of shoulder-arm exercises.
CASE REPORTS
Three young male soldiers, all aged 20 years, presented with anterior shoulder pain and palpable mass in the superior part of the deltopectoral groove close to acromioclavicular joint on left shoulder, since a couple of months prior to presentation. All the patients served in elite commando company drill team. They performed military demonstrations with or without rifle in ceremonies and military shows. Thus they underwent intense military training program, including rifle drill exercises for about eight hours a day and ordinary duty for four hours a day with a rifle as well, throughout the serving period. Mean military serving period was 10 months (range, 7-12 months).
History of the patients revealed they underwent repetitive trauma and overuse of their shoulders due to military exercises. As members of the army drill team, they mainly performed rifle drills, exhibition drills, military parade, and related exercises like left shoulder–arm orders from the beginning of their serving period. Left shoulder–arm exercises were performed with G-3 assault rifle (7.63 mm, Heckler and Koch, Germany), and each soldier performed the regular firing exercises twice and fired five rounds each time, in the first two months of their serving period.
The patients complained of mild tenderness, pain in the region of the mass, discomfort on movements of the shoulder and difficulties when participating in military exercises. During the serving period, they reported gradually increasing pain; and thereafter, ecchymosis around the contact area of rifle on the shoulder. Later a firm, rigid mass gradually developed in the same region while ecchymosis faded.
Physical examination revealed a firm, solid, irregular mass in the superior part of deltopectoral groove close to acromioclavicular joint of the shoulder [Figure 1]. On palpation, masses were detected in the muscle belly of deltoid muscle close to distal part of clavicle and anterior part of acromion, which then extended to deltopectoral groove. Masses were not fixed to bony structures. They were in soft tissue and located intramuscularly along the deltoid muscle. Size of each mass was approximately 5 × 3 cm. The structure of masses was irregular, rigid and hard. Described locations had a direct contact with the rifle during the shoulder-arm exercises and firing of arms. The range of motion was between 140° and 150° forward flexion, 140° and 150° abduction, 45° extension, 75° of external rotation and 75°-90° internal rotation. Neurovascular examinations were unremarkable. Plain radiography of the shoulder revealed hyper-dense irregular masses in the anterior aspect. No radiological abnormalities were seen in the adjacent bony structures [Figure 2a]. Computerized tomography scan (coronal view) showed extracapsular, dense, irregular structure between pectoralis and deltoid muscles which was correlated with heterotopic bone [Figure 2b]. No erosion, or invasion of, adjacent bony structure was reported. Proximity of mass to clavicle, acromion and coracoids process was obvious without bridging. Complete blood count and biochemical parameters of the patients were normal.
Figure 1.
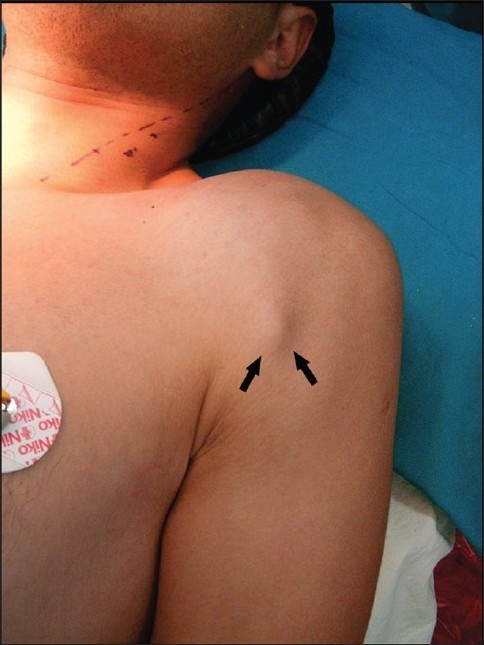
Clinical photograph showing ossified mass
Figure 2.
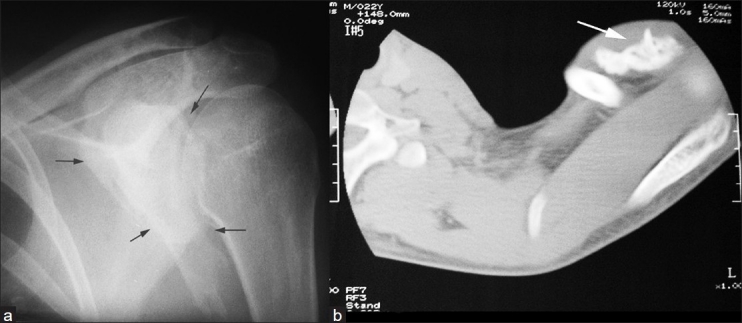
(a) X-ray of shoulder joint (anteroposterior view) showing appearance of ossified mass (black arrows) (b) Computerized tomography images (coronal view) showing heterotopic bone in the deltopectoral groove (white arrow)
Patients were diagnosed as suffering from myositis ossificans of the shoulder.
One patient refused surgical intervention because of completion of his military serving period. Others were operated with interscalene block anesthesia. Deltopectoral incisions were used, and masses were bluntly dissected from the surrounding soft tissues. Well-demarcated ossified masses were easily dissected from the soft tissues and removed completely [Figure 3].
Figure 3.

Gross appearance of excised mass
Gross appearances and pathological reports confirmed the structure of the mass as a mature trabecular bone. Postoperatively, indomethacin (75 mg, OD) treatment (6 months) and active shoulder exercises were initiated and continued till the full range of motion was regained. After the convalescence period, the patients were ordered to use mini soft bag on the rifle contact area of shoulders.
No complications or recurrences were observed during the 24 months of followup [Figure 4] period including full participation in military training and exercise activities.
Figure 4.
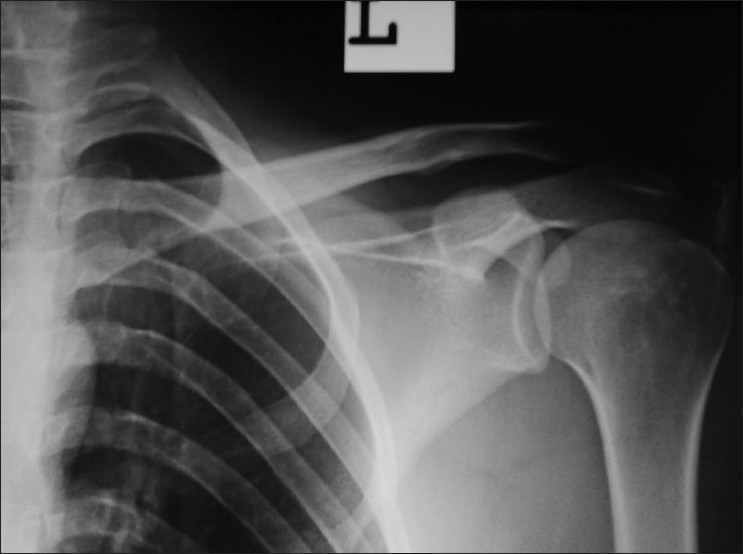
X-ray of left shoulder (anteroposterior view) at 2 years followup showing no recurrence of heterotopic ossification
DISCUSSION
The myositis ossificans usually involves young people and athletes because of high level of athletic activities and extensive muscle usages. Direct trauma to muscle may induce hemorrhagic injury and diffuse ossification in soft tissue. Detailed history of our patients reveal the etiological factor to be shoulder-arm or firing exercises. Myositis ossificans may adhere to adjacent bony structures in deeper muscular plane. Shoulder region is predisposed to heterotopic bone formation because of its extensive muscle coverage.5 The proposed theory in the case of our patients is the ossification of muscle owing to trauma and hematoma during shoulder exercises and firing.
Millions of soldiers are performing shoulder-arm exercises and undergoing marksmanship training all over the world. In the course of performing shoulder-arm exercises, the last phase transfers the kinetic energy of rifle to the shoulder via the rifle's barrel to the deltopectoral region. Repetition of this activity causes hemorrhagic injury in the muscle belly. Although we have herein reported, to the best of our knowledge, the first few cases of musculoskeletal injury related with these activities, but we think the exact unpublished incidence is evidently much higher than this. Not only shoulder exercises but also backfire effect while firing of arms, contributes to the stress on the shoulder region as well as deltopectoral region. We consider the main cause of injury to be shoulder-arm exercises; also, the backfire effect may have contributed too.
Treatment modalities should be chosen according to the patient's demands and lesions. Indications for removal are — restriction of motion, pressure symptoms on nerves or blood vessels, pain and limitation of athletic, occupational or daily activities.7 Treatment of heterotopic ossification of the shoulder is mainly surgical excision.1,2 Close manipulation, radiation therapy and medication are also treatment options.6 Complete excision via classic deltopectoral incision with proper care of neurovascular bundle and prophylactic medication led us to achieve the desired goal of treatment. Furthermore, protecting the shoulder by mini soft bag or a towel during the exercises, also prevent development of myositis ossificans.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Garland DE. Surgical approaches for resection of heterotopic ossification in traumatic brain injured adults. Clin Orthop Relat Res. 1990;263:59–70. [PubMed] [Google Scholar]
- 2.Warner JJ, Ejnisman B, Akpinar S. Surgical mamagement of heterotopic ossification of the shoulder. J Shoulder Elbow Surg. 1999;8:175–8. doi: 10.1016/s1058-2746(99)90015-0. [DOI] [PubMed] [Google Scholar]
- 3.Wenner SM. Heterotopic ossification of the shoulder following head injury: A case report. Clin Orthop Relat Res. 1985;212:231–6. [PubMed] [Google Scholar]
- 4.Boynton MD, Enders TJ. Severe heterotopic ossification after arthroscopic acromioplasty: A case report. J Shouler Elbow Surg. 1999;8:495–7. doi: 10.1016/s1058-2746(99)90083-6. [DOI] [PubMed] [Google Scholar]
- 5.Erggelet C, Eggensperger G, Steinwachs M, Lahm A, Reichelt A. Postoperative ossifications of the shoulder. Arch Orthop Trauma Surg. 1999;119:168–70. doi: 10.1007/s004020050383. [DOI] [PubMed] [Google Scholar]
- 6.Berg EE, Ciullo JV. Heterotopic ossification after acromioplasty and distal clavicle resection. J Shoulder Elbow Surg. 1995;4:188–93. doi: 10.1016/s1058-2746(05)80050-3. [DOI] [PubMed] [Google Scholar]
- 7.Ring D, Jupiter JB. Operative release of complete ankylosis of the elbow due to heterotopic bone im patients without severe injury of the central nervous system. J Bone Joint Surg Am. 2003;85:849–57. doi: 10.2106/00004623-200305000-00012. [DOI] [PubMed] [Google Scholar]


