Abstract
Objectives
To look retrospectively at patients undergoing elective, ultrasound indicated and rescue cervical cerclage, examine the immediate pregnancy outcomes and compare them.
Design
This was a retrospective observational study using the maternity and neonatal databank to identify patients having cervical cerclage between 1985 and 2009 inclusive. Data extracted included patient demographics, gestation of suture insertion, gestation at delivery, mode of delivery and initial pregnancy outcome. Further information on selected patients having cerclages over 16 weeks gestation was collected from case-notes.
Setting
Aberdeen Maternity Hospital, North East Scotland.
Participants
All patients having cervical cerclage between 1985 and 2009.
Main outcome measures
Gestation at delivery, live birth rate and birth weight.
Results
A total of 177 sutures were inserted – 116 electively and 61 as an emergency procedure. Time trends of cervical cerclage revealed a bimodal distribution and in the last four years there has been a general increase in the number of emergency sutures while the number of elective cerclages has remained relatively constant. There was little difference in the gestation at delivery between the elective and emergency cerclage groups (35 and 33 weeks, respectively), live birth rate (93% and 92%, respectively) and the difference in mean birth weight did not reach statistical significance. Case-notes were obtained for 25 patients undergoing ultrasound indicated cerclage and nine patients undergoing rescue cerclage. There was a higher suture associated complication rate in the rescue cerclage group (33% vs. 12% in the ultrasound indicated cerclage group) and the mean gestation of delivery was lower (26 weeks vs. 32 weeks). The birth weight was significantly lower and the neonatal death rate higher in the rescue cerclage group.
Conclusions
Elective and ultrasound indicated cervical cerclage appear to have low complication rates and high live birth rates. Rescue cerclage has a high complication rate and is therefore associated with poor outcome.
Introduction
The use of cervical cerclage in the prevention of preterm delivery was described by Shirodkar in 1955 and then by McDonald two years later. It is not clear why dilatation and effacement of the cervix occurs prematurely, but it is thought that the forced mechanical closure of an ‘incompetent’ cervix with a suture maintains the cervical length as well as the mucus plug – both of which have a role in preventing labour. However, there is a lack of good large randomized controlled trials to help clinicians and patients decide whether or not to insert a cervical suture – the three main randomized controlled trials having conflicting results.1–3 Cervical cerclage may be performed prophylactically in the first trimester when the clinical history suggests risk of mid-trimester loss or when cervical resistance studies confirm low cervical resistance. It may also be performed when there is evidence of a short cervix (<25 mm) or cervical shortening on ultrasound. More rarely, a rescue cervical suture may be inserted when the patient presents with a cervix that is already dilated with the membranes bulging into the vagina but no signs of labour, infection or heavy vaginal bleeding. The aim of this study was to look retrospectively at the patients undergoing elective, ultrasound indicated and rescue cervical cerclage, examine the immediate pregnancy outcomes and compare them. This information may help the patient and her carer make an informed decision about whether to undergo cervical cerclage – either electively or as an emergency procedure.
Methods
The study was based at Aberdeen Maternity Hospital in the North East of Scotland. This tertiary referral centre covers a wide geographical area and includes the islands of Orkney and Shetland. The Aberdeen Maternity and Neonatal Databank (AMND) was used to identify all patients who had a cervical cerclage inserted during pregnancy between 1985 and 2009. Information such as patient age, parity, gestation of suture insertion, gestation at delivery, mode of delivery, initial pregnancy outcome (including Apgar scores at 1 minute and birth weight) were extracted from the AMND. If the suture was inserted after 16 weeks gestation, further information on the patient was obtained from the case-notes. Sixteen weeks was chosen as the cut-off because sutures inserted after this gestation were less likely to have been inserted electively. Information gathered included past obstetric history, any cervical length scan result (whether transabdominal, transvaginal or both), the findings at any vaginal examination, the type of suture inserted and by whom, any complication deemed to be as a direct result of suture insertion, and whether the suture was removed antenatally or intrapartum. These findings were recorded on a standardized pro forma. Statistical analysis was done using Microsoft Excel and Statistical Package for Social Scientist (SPSS version 17, Chicago Illinois). Time trends of the different types of cervical sutures were constructed. Sociodemographic characteristics and outcomes of pregnancy were compared across the groups using Anova for continuous variables and chi-square test for categorical variables.
Results
All cervical sutures
A total of 177 sutures were inserted between August 1985 and November 2009. Of the 63 patients having sutures beyond 16 weeks, 36 case-notes were obtained thus in the remaining 27 cases it was impossible to determine whether the cerclage was ultrasound indicated or rescue in nature. Of the 36 cases available for review, two patients were from the islands and had an elective cervical suture; the data from these patients were thus added to the elective cerclage group. Twenty-five of the remaining 34 patients (74%) had ultrasound indicated cervical cerclage while nine patients had rescue cervical cerclage.
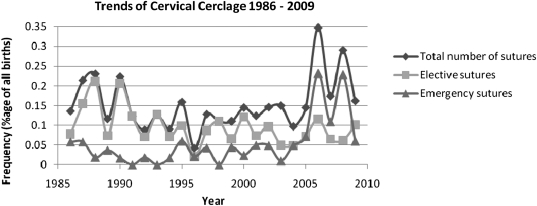
Time trends: The number of sutures inserted per year ranged from two (1996) to 15 (2006) with an average of seven sutures per year. Figure 1 demonstrates the annual frequency of all the cervical sutures inserted as a percentage of all births for that year, as well as the frequency of elective and emergency cerclage insertions.
Figure 1.
Trends of cervical cerclage 1986–2009
The frequency of cervical cerclage insertion over the years shows a bimodal distribution and between 2005 and 2008, the number of emergency cervical cerclages exceeded the number of elective procedures. The number of elective cervical cerclages has stayed fairly constant since 1992 yet since 2004 the number of sutures inserted after 16 weeks has generally risen.
A total of 114 sutures (64%) were inserted at <17 weeks. There were a large number of pregnancy losses in the 38 patients who had had multiple cervical sutures – eight of the 17 pregnancy losses (47%) occurring in patients who had had more than one suture.
Eleven patients (6%) delivered at 41 weeks and beyond – eight had had early cervical sutures.
Elective cervical sutures
There were 116 elective (also described as history indicated) cervical sutures carried out at a mean gestation of 14 weeks. The vast majority of the elective cervical sutures were inserted in multiparous women, with an average age of 31 years. The mean suture to delivery interval was 21 weeks with 76% of patients delivering vaginally at an average gestation of 35 weeks. There were 107 live births, 12 mid-trimester losses and one neonatal death.
Ultrasound indicated cervical sutures
There were 25 patients who had a cervical suture inserted on the basis of cervical length scans – this included three sets of twins and one triplet pregnancy. Twenty-one patients (84%) had a past history of at least one mid-trimester loss. Twelve scans (46%) were transabdominal (TA), eight scans (35%) transvaginal (TV) and the remaining five patients had both TA and TV scans. The sonographic cervical length varied between 6 mm and 40 mm (mean 25 mm) and funnelling (dilatation of the internal os) was noted on 12 (46%) of the scans. The consultant inserted the majority of the sutures (74%) while the trainees inserted the remainder. The type of suture inserted was poorly documented but there was one modified Shirodkar (high vaginal) suture inserted and 11 McDonald sutures. There were two complications (8%) – excessive vaginal bleeding and ruptured membranes within 24 hours, both necessitating suture removal. In these cases, the suture to delivery intervals were 4 and 10 weeks, respectively. Fifteen sutures (60%) were removed in labour. There were two pregnancy losses (8%) at 20–23 weeks gestation. The suture to delivery interval ranged between 1–23 with a mean duration of 10 weeks. The average gestation of delivery was 32 weeks with 54% of patients delivering vaginally.
Rescue cervical cerclage
Of the nine patients known to have undergone rescue cervical cerclage, there were four sets of twins. The cervical dilatation noted on examination was between 3–9 cm. The consultant inserted the majority of the sutures (89%) and the type of suture was also poorly documented (two McDonald sutures and one Shirodkar). The complication rate was 33% – ruptured membranes in all cases. The suture to delivery interval was 0–14 weeks with a mean of 6 weeks (modal duration was 1 week). The vaginal delivery rate was 73% with a mean birth weight of 900 g. There were nine neonatal deaths (64% of live births). Three sutures were inserted at 9 cm of cervical dilatation. In these pregnancies, the maximum number of weeks gained was 1; one suture was associated with a complication and all resulted in losses (one stillbirth and two neonatal deaths).
Tables 1–4 summarize the results for ease of comparison. The data shown from the non-elective cervical cerclage column include all 61 patients having a non-elective cervical suture beyond 16 weeks.
Table 1.
Demographic factors
| Elective cervical cerclage | All non-elective cervical cerclage | P value | |
|---|---|---|---|
| Pregnancies (n) | 116 | 61 | |
| Mean age (years) (range in brackets) | 31 (18–41) | 30 (22–41) | 0.30 |
| Percentage primiparous | 1 | 21 | <0.05 |
| Percentage multiparous | 99 | 79 | <0.05 |
| Multiple pregnancies (percentage of total in brackets) | 3 (3%) | 12 (20%) | <0.05 |
| Gestation of suture insertion (weeks) (range in brackets) | 14 (6–19) | 23 (17–29) | <0.05 |
Table 4.
Outcomes – non-elective subgroups
| USS indicated cervical cerclage | Rescue cervical cerclage | P value | |
|---|---|---|---|
| Mean suture to delivery interval (weeks) (range in brackets) | 10 (1–23) | 3 (0–14) | 0.33 |
| Immediate complication (percentage of total in brackets) | 3 (12) | 3 (33) | 0.15 |
| Suture removed in labour (percentage of total in brackets) | 15 (60) | 3 (33) | 0.17 |
| Mean gestation at delivery (range in brackets) | 32 (20–40) | 26 (22–36) | 0.24 |
| Vaginal delivery rate (%) | 54 | 73 | 0.14 |
| Live births (percentage of babies born in brackets) | 26 (93) | 14 (93) | 0.98 |
| Mean birth weight (g) | 2112 | 900 | <0.05 |
| Mean Apgar at 1 minute | 7 | 4 | 0.28 |
| Admissions to the neonatal unit (as percentage of live births within group) | 65 | 43 | 0.14 |
Table 2.
Demographic factors – non-elective subgroups
| USS indicated cervical cerclage | Rescue cervical cerclage | P value | |
|---|---|---|---|
| Pregnancies (n) | 25 | 9 | |
| Mean age (years) (range in brackets) | 27 (18–38) | 31 (21–39) | 0.9 |
| Percentage primiparous | 12 | 44 | <0.05 |
| Percentage multiparous | 88 | 56 | <0.05 |
| Multiple pregnancies (percentage of total in brackets) | 3 (12%) | 5 (56%) | <0.05 |
| Gestation of suture insertion (weeks) (range in brackets) | 22 (17–28) | 23 (20–24) | <0.05 |
Table 3.
Outcomes
| Elective cervical cerclage | All non-elective cervical cerclage | P value | |
|---|---|---|---|
| Mean suture to delivery interval (weeks) (range in brackets) | 21 (2–30) | 10 (0–24) | <0.05 |
| Mean gestation at delivery (range in brackets) | 35 (16–41) | 33 (20–41) | 0.39 |
| Vaginal delivery rate (%) | 76 | 77 | 0.96 |
| Live births (percentage of babies born in brackets) | 107 (92) | 69 (93) | 0.26 |
| Mean birth weight (g) | 2696 | 1987 | 0.87 |
| Mean Apgar at 1 minute | 7 | 7 | – |
| Admissions to the neonatal unit (as percentage of births within group) | 35 | 55 | 0.22 |
| Neonatal deaths (percentage of live births in brackets) | 1 (1) | 15 (22) | – |
Comments
Time trends of cervical cerclage reveal a bimodal distribution and in four years there has been a general increase in the number of emergency sutures inserted. This probably reflects the vogue for each year – itself a reflection of newly available literature – but it may also be the result of staff changes within the maternity unit.
There was little difference in the gestation at delivery between the elective and emergency cerclage groups and no statistical difference between live-birth rate, mean birth weight, Apgars at 1 minute and neonatal unit admission.
Infection and ensuing chorioamnionitis, ruptured membranes and bleeding are the most concerning complications associated with cervical cerclage – all of which may result in early delivery. Although there are no figures available for the elective cerclage group, the complication rate is likely to be relatively low because the average suture insertion to delivery interval and the gestation of delivery are both high. Rescue cerclage carried the highest complication rate (33% compared with 12% for ultrasound indicated cervical sutures in this study). The suture to delivery interval was far longer in the ultrasound indicated cervical cerclage group compared to the rescue cerclage group – the latter group delivering at a much earlier gestation; however this did not reach statistical significance.
While on the face of it the live-birth rate was high for rescue cerclage and comparable to the ultrasound indicated cerclage group, there were a large number of neonatal deaths (most probably attributed to extreme prematurity) – with only two of the nine pregnancies ending in the third trimester. The lack of a control group makes it difficult to determine whether rescue cervical cerclage was detrimental or not. Patients undergoing rescue cerclage delivered babies with a significantly lower birth weight than those babies born after ultrasound indicated cervical cerclage and had poorer Apgar scores at 1 minute – although the latter did not reach statistical significance. Evidence for inserting sutures at advanced dilatation is mostly in the form of case reports4,5 – and including such patients have skewed the results towards a poor outcome. However, it has been suggested that cerclage should be considered as despite the poor prognosis, successful outcomes sometimes occur.4
Because the study used retrospective data over 24 years, there are limitations. During this time period ultrasound practices have changed and neonatal care has improved dramatically. In addition, the study did not have the power to detect small differences in rare outcomes like pregnancy loss.
The increased pregnancy loss rate associated with patients who have had cerclages in several pregnancies could indicate that the patients had true cervical incompetence for which cervical cerclage proved limited benefit. Interestingly, a study by Pelham et al. in 2008 noted that repeat cervical suture for an indication other than true cervical incompetence was of no benefit.6
In our unit, all patients with a multiple pregnancy have a cervical length scan at 24 weeks which allows for appropriate counselling of the risk of preterm labour (and prophylactic steroid administration) – cervical cerclage may be offered if the cervix measures less than 25 mm. TV ultrasound assessment of the cervix is the gold standard – the full bladder needed for TA assessment may artificially lengthen the cervix leading not only to under-intervention but also decreasing the perceived risk of suture insertion with resultant inappropriate counselling of the patient. The fact that just over half of patients having ultrasound indicated cervical cerclage had a transvaginal scan, may have skewed our results. The patients undergoing ultrasound-based cervical cerclage are an interesting group as a short cervix predicts risk of preterm delivery but cerclage resulting in a complication can shorten the gestation further. Ultrasound surveillance of cervical length is certainly beneficial – a study showed that ultrasound surveillance of cervical length versus elective cervical cerclage reduced cervical cerclage rates without compromising pregnancy outcome.7 Other studies have found that insertion of a suture if the cervix is 15–25 mm and the patient has no other risk factors for preterm delivery, offers no benefit.8,9
The benefit of cervical cerclage in patients with multiple pregnancies compared to bedrest is also in doubt with studies showing no benefit8,10 or even a deleterious effect.8,11,12
It is difficult to know whether the procedure itself led to the complications in rescue cerclages or whether the presumed complication is the result of cervical dilatation. There has only been one randomized controlled trial looking at rescue cervical cerclage and the average suture to delivery interval was 54 days.13 Our findings concur – although the numbers are small and the mean interval is skewed by the fact that two of the nine pregnancies achieved an interval of 14 weeks (one patient being delivered for a non-obstetric indication). Other studies have found longer mean suture to delivery intervals of 71 days and 8.8 weeks, respectively.14,15
There are some implications for the future. The use of TV ultrasound in cervical length assessment needs to be standardized. There is also a definite need for a good randomized controlled trial in patients undergoing serial cervical length ultrasound assessment – perhaps including other therapies such as progesterone and especially in multiple pregnancies.
Conclusions
Elective and ultrasound indicated cervical cerclage appear to have low complication rates and high live-birth rates. It is difficult to predict those who may require rescue cervical cerclage although multiple pregnancies are at risk. Rescue cerclage has a very high complication rate and is associated with a high loss rate but a large randomized controlled study is required to determine whether this intervention actually prolongs pregnancy.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Not applicable
Guarantor
AL
Contributorship
All authors contributed equally
Acknowledgements
The authors thank The Steering Committee for granting access to the Aberdeen Maternity and Neonatal Database
Reviewer
Jonathan Baum
References
- 1.Lazar P, Gueguen S, Dreyfus J, Renaud R, Pontonnier G, Papiernik E Multicentred controlled trial of cervical cerclage in women at moderate risk of preterm delivery. Br J Obstet Gynaecol 1984;91:731–5 [DOI] [PubMed] [Google Scholar]
- 2.Rush RW, Isaacs S, McPherson K, Jones L, Chalmers I, Grant A A randomised controlled trial in women at high risk of spontaneous preterm delivery. Br J Obstet Gynaecol 1984;91:724–30 [DOI] [PubMed] [Google Scholar]
- 3.Final report of the Medical Research Council/Royal College of Obstetricians and Gynaecologist multicentred randomised trial of cervical cerclage MRC/RCOG Working Party on Cervical Cerclage. Br J Obstet Gynaecol 1993;100:516–23 [DOI] [PubMed] [Google Scholar]
- 4.Groom KM, Bennett PR, Golara M, Maxwell DJ, Shennan A Successful cerclage at advanced dilatation in the second trimester. Br J Obstet Gynaecol 2001;108:1005–7 [DOI] [PubMed] [Google Scholar]
- 5.Takai N, Nishida M, Urata K, Yuge A, Miyakawa I Successful cerclage in two patients with advanced cervical dilatation in the second trimester. Arch Gynaecol Obstet 2003;268:102–4 [DOI] [PubMed] [Google Scholar]
- 6.Pelham JJ, Lewis D, Berghella V Prior cerclage to repeat or not to repeat. That is the question. Am J Perinatol 2008;25:417–20 [DOI] [PubMed] [Google Scholar]
- 7.Groom KM, Bennett PR, Golara M, Thalon A, Shennan A Elective cervical cerclage versus serial ultrasound surveillance of cervical length in a population at high risk for preterm delivery. Eur J Obstet Gynaecol Reprod Biol 2004;112:158–61 [DOI] [PubMed] [Google Scholar]
- 8.Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient – level data. Obstet Gynaecol 2005;106:181–9 [DOI] [PubMed] [Google Scholar]
- 9.To MS, Alfirevic Z, Heath VC, Cicero S, Williamson PR, Nicolaides KH Cervical cerclage for prevention of preterm delivery in women with a short cervix – randomised controlled trial. Lancet 2004;363:1849–53 [DOI] [PubMed] [Google Scholar]
- 10.Roman AS, Rebarber A, Pereira L, Sfakianaki AK, Mulholland J, Berhella V The efficacy of sonographically indicated cerclage in multiple gestations. J Ultrasound Med 2005;24:763–8 [DOI] [PubMed] [Google Scholar]
- 11.Strauss A, Heer IM, Janßen U, Dannecker C, Hillemanns P, Müller-Eglof S Routine cervical cerclage in higher order multiple gestation – does it prolong the pregnancy? Twin Res 2002;5:67–70 [DOI] [PubMed] [Google Scholar]
- 12.Newham R, Krombach R, Myers M, McGee D Effect of cerclage on obstetrical outcome in twin pregnancies with a shortened cervical length. Am J Obstet Gynecol 2002;186:634–40 [DOI] [PubMed] [Google Scholar]
- 13.Althusius SM, Dekker GA, Hummel P, van Geijn HP Cervical incompetence prevention randomized cerclage trial: emergency cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol 2003;189:907–10 [DOI] [PubMed] [Google Scholar]
- 14.Gupta M, Emary K, Impey L Emergency cervical cerclage: predictors of success. J Matern Fetal Neonatal Med 2010;23:670–4 [DOI] [PubMed] [Google Scholar]
- 15.Daskalakis G, Papantoniou N, Mesogitis S, Antsaklis A Management of cervical insufficiency and bulging fetal membranes. Obstet Gynecol 2006;107:221–6 [DOI] [PubMed] [Google Scholar]