Abstract
Objectives
The study hypothesis is to assess correlation of breast specimen weight versus volume.
Design
Consecutive patients undergoing breast surgery at a single tertiary referral centre during a 6-month period were included. Specimen weight was measured in grams. Direct volume measurements were performed using water displacement. Data including side of the breast, age and menstrual status of the patient were noted.
Setting
Knowledge of breast volume provides an objective guide in facilitating the achievements of balance in reconstructive operations. Surgeons use intraoperative weight measurements from individual breasts to calculate the breast volume assuming that weight is equal to the volume of the specimen. However, it is unclear whether weight accurately reveals the true volume of resection.
Participants
Forty-one patients were included in the study with 28 having bilateral surgeries, 13 having unilateral procedures giving a total of 69 breast specimens.
Main outcome measures
Breast specimen weight correlation to breast specimen volume.
Results
The mean age of the group was 42.4 years. Fifty-two specimens were from premenopausal patients and 17 were of postmenopausal. Thirty-five were left-sided. Twenty-six patients had bilateral breast reduction, two had bilateral mastectomy, nine had a unilateral mastectomy and four patients had a unilateral breast reduction. The difference between weight and volume of these breasts was 36.4 units (6.6% difference). The difference in measurement of weight and volume in premenopausal was 37.6 units compared to 32.6 units in postmenopausal women. The density was 1.07 and 1.06, respectively. This was statistically not significant.
Conclusions
No significant difference between volume and weight was seen in this series. Furthermore, we are unable to support the notion that premenopausal patients have a significant difference in the proportion of fatty and glandular tissue as there was little difference between the weight and the volume. An easy, clinically proper formula for the quantification of actual breast volume has yet to be derived.
Introduction
For many years breast and plastic surgeons have pondered about achieving symmetry and natural-looking breast shapes after reduction mammaplasty. Indeed, many surgeons still try to achieve breast symmetry, by volume, mainly using intraoperative comparative weight measurements between specimens excised from individual breasts. Many surgeons advocate that the knowledge of breast volume provides an objective guide in asymmetry procedures and facilitates the achievement of balance especially in reduction and reconstructive surgery. The question many breast surgeons have pondered is, does weight of excised specimens really reveal the volume of the resection?
By performing this simple prospective study our aim was to shed some light on the years of debate between surgeons advocating the use of volume and surgeons using weight as an intraoperative guide to facilitate breast resection.
Materials and methods
Consecutive patients undergoing breast surgery at a single tertiary centre during a period of 6 months were included. Specimen weight was measured in grams on electronic weighing scales. Direct volume measurements were performed by using a water displacement technique undertaken by the same team member (senior breast care nurse) on each occasion. The excised breast tissue was placed in a cylinder of known volume. The specimen was then submerged in the cylinder and the volume of the displaced water was measured. This volume measurement was measured by a simple device based on Archimedes' principle. Archimedes' principle is a physical law of buoyancy, which states that any body completely or partially submerged in a fluid is acted upon by an upward force equal to the weight of the fluid displaced by the body.1 The validity and reproducibility of this method was confirmed by submerging breast implants of known volume into the cylinder and assessing the water volume displaced.
Data including breast laterality, age and menstrual status of the patient were also noted.
Results
Forty-one patients participated in this study, yielding 69 specimens. Twenty-six patients had bilateral breast reduction mammoplasty while two patients had bilateral breast mastectomies for breast cancer treatment. The remaining 13 patients had single breast mastectomy (n = 9) and single breast reduction mammaplasty (n = 4).
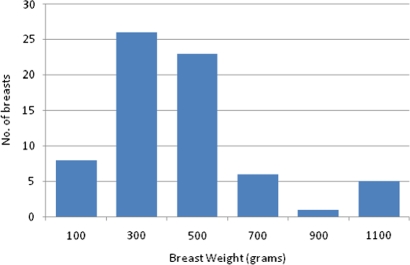
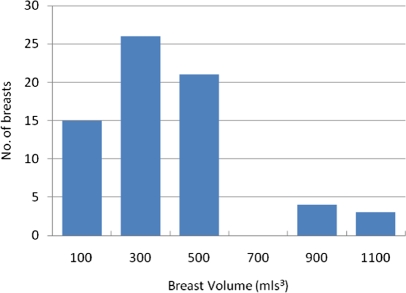
Median patient age was 42 years, with a range of 18–81 years. The volume and weight data for all 69 breasts conformed to a normal distribution (Figures 1 and 2). The mean weight was 545.4 g while the mean volume was 509 mL3, a difference of 36.4 units (7%). The mean difference in weight and volume of the left breast (n = 35) was 33.3 units, compared to 39.6 units on the right (n = 34) (Mann Whitney P = 0.39 and P= 0.39, respectively). The mean volumes of the right and left breasts were statistically similar at 504 mL3 and 513 mL3, respectively (unpaired student T-test P = 0.88). The mean weight of the right and left breasts were also statistically similar at 544 g and 547 g, respectively (unpaired student T-test P = 0.96). This is summarized in Table 1.
Figure 1.
Histogram showing normally distributed data depicting number of breast specimens against breast weight (in grams)
Figure 2.
Histogram showing normally distributed data depicting number of breast specimens against breast volume (in mL3)
Table 1.
Comparison between mean weight and volume for all patients. Significance denoted by P < 0.05
| Bilateral | Mean | Statistics | ||
|---|---|---|---|---|
| Mean weight (g) (n = 69) |
545.4 | Right (n = 34) | 544 | Unpaired student T-test P = 0.96 |
| Left (n = 35) | 547 | |||
| Mean volume (mL3) (n = 69) |
509 | Right (n = 34) | 504 | Unpaired student T-test P = 0.88 |
| Left (n = 35) | 513 | |||
| Difference | 36.4 (P = 0.30) | Right (n = 34) | 39.6 | Mann-Whitney P = 0.39 |
| Left (n = 35) | 33.3 | Mann-Whitney P = 0.39 |
When considering the menopausal status of our patients we found that the majority were premenopausal (n = 29) versus 12 postmenopausal patients. Of these, five premenopausal patients and seven postmenopausal patients had unilateral procedures. When considering the difference between weight and volume in premenopausal and postmenopausal excised breast tissue, the mean difference was 37.6 units and 32.6 units, respectively. This was still found to be statistically not significant (Mann Whitney P = 0.39 and 0.47, respectively) When comparing pre- to postmenopausal weight and volume we found results to be statistically insignificant (unpaired student T-test P = 0.40, SD –58.69 ± 69.90 and P = 0.45, SD –53.68 ± 70.26, respectively). This is summarized in Table 2. We also calculated the density of the pre- and postmenopausal breasts using the formula mass/volume. The premenopausal breasts had a mean density of 1.07 g/mL while the postmenopausal breast had a mean density of 1.06 g/mL (unpaired student T-test P = 0.36, SD 0.03 ± 0.03).
Table 2.
Comparison between mean weight and volume in pre- and postmenopausal patients. Significance denoted by P < 0.05
| Mean | Statistics | ||
|---|---|---|---|
| Premenopausal (n = 52) | Weight (g) | 560 | Mann Whitney P = 0.30 |
| Volume (mL3) | 522 | ||
| Postmenopausal (n = 17) | Weight (g) | 501 | Mann Whitney P = 0.47 |
| Volume (mL3) | 467 | ||
| Pre vs. postmenopasual | Weight (g) | 560 | Unpaired student T-test P = 0.40 |
| Weight (g) | 501 | ||
| Pre vs. postmenopasual | Volume (mL3) | 522 | Unpaired student T-test P = 0.45 |
| Volume (mL3) | 467 |
Discussion
From the viewpoint of the operating surgeon, determination of breast volume would be helpful and desirable to facilitate the complex planning and difficult execution of many surgical breast interventions, including correction of breast asymmetry, restoration of an ablated breast, and volume-changing aesthetic intervention.2–12 The desire for improved breast volume calculation methods is reflected by over 50 publications in the last four decades on the topic. Unfortunately, the various breast volume measurement techniques that have been proposed in such articles exhibit variable reliability. Moreover, these techniques involve a level of detail that can be difficult to execute, are of limited practicability, are often cost-intensive, and are not always accepted by the patient. For these reasons, these techniques have found only limited application in everyday breast surgery as well as plastic and reconstructive surgery, and in only exceptional cases does breast volume measurement occur before surgery. Generally, these methods of breast volume assessment fall into one of five different categories. The anthropomorphic method attempts to derive a correlation between breast volume data obtained by other methods and standardized end-to-end measurements of the thorax region.13,14 Volume methods based on 2D images such as mammograms and ultrasound are somewhat comparable to modified anthropomorphic measurement with the help of 2D photography.15,16 Archimedean methods of breast volume measurement are based on Archimedes' principle of water displacement.17 Here the female patient bends over a water-filled vessel, lowering her breast into the water, and breast volume is calculated based on displaced water. Alternatively, modified methods use calibrated measurement cylinders placed against the thorax wall; the rigid thorax wall forms the rear demarcation of the breast and the ventral tissue portions are measured as the displaced ‘breast volume’.18–20 Another method is the use of plaster and thermoplastic materials to generate a three-dimensional (3D) negative cast of the breast.21,22 The cast materials are placed on the upright, seated patient and left to harden. The resulting 3D shell model is filled with water or sand in order to determine breast volume. Modern imaging procedures such as computed tomography (CT) and nuclear magnetic resonance imaging (MRI) offer an alternative means of modelling the breast in 3D.23,24 The patient is placed in the scanner in a prone position, and the breast volume is calculated by the summation of segmented monolayers. An alternative to these classical methods is 3D body surface imaging. With the help of different 3D imaging devices, a non-invasive recording in a standing position and the creation of a virtual 3D model of the breast region are possible. Furthermore, the 3D technology provides the ability to quantitatively evaluate symmetry, volume, shape, contour, surface and distance measurements.
All the above techniques are mainly used for the assessment of breast volume in a preoperative setting. In our study, we aimed to shed some light on the debate between the use of weight or volume in breast surgery intraoperatively. Few publications tackle the subject of weight or volume use in an intraoperative setting.25,26 In our study we have found no statistical significance when comparing the use of measurement by weight or volume. We also found no significance when comparing the weight or volume by breast laterality. Right- and left-sided specimens were also compared for volume and weight measurements. Here still no significant difference was found. We also explored the general belief that premenopausal and postmenopausal patients have significant different proportions of glandular and fatty tissue contributing to the difference in the weight and volume. Here we compared premenopausal and postmenopausal patient breast weight versus volume measurements and also premenopausal versus postmenopausal weight and volume and found no statistical significance. Furthermore, no significance was found when calculating breast density for pre- and postmenopausal women, although we must point out that this study is limited by a relatively small patient cohort. Thus, we recommend that a larger blinded study is necessary to correlate weight and volume between pre- and postmenopausal women.
There is little evidence in the literature pertaining to this subject, but our findings reflect experimental work by Sommer et al.,25 Lejour et al.26 and Aslan et al.27 They state that in preliminary studies they conducted, they have shown that the amount and pattern of breast fat and glandular tissue may have many personal variations and may also differ between breasts from the same patient. They go on to conclude that as the specific gravity of water is 1.00 and that of fat is 0.92, breast tissue with its fibrous and glandular structure is a mixture of the two, hence it is good practice to assume that weight equals volume as the overall specimen density approaches 1.0 g/cm3. All studies conducted similar experimental work. They all go on to state that although clinically it is claimed that the glandular tissue of a particular breast is more than the fat component in both pre-and postmenopausal women, this has been proved to be the contrary. There is a high probability that the majority of specimens will be fatty tissue dominant.
We can thus conclude that this enables the clinician to use intraoperative specimen weight as a close comparison of resected breast volume, both in pre- and postmenopausal women.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Not applicable
Guarantor
LM
Contributorship
CP devised the study concept; MW is the primary author; SP and JN collected data; CP, MW, and SP finalised the draft; LM was the consultant responsible for the patients
Acknowledgements
None
Reviewer
Bernard Robertson
References
- 1.Schultz RC, Dolezal RF, Nolan J Further applications of Archimedes' principle in the correction of asymmetrical breasts. Ann Plast Surg 1986;16:98 [DOI] [PubMed] [Google Scholar]
- 2.Hudson DA Factors determining shape and symmetry in immediate breast reconstruction. Ann Plast Surg 2004;52:15–21 [DOI] [PubMed] [Google Scholar]
- 3.Kovacs L, Zimmermann A, Papadopulos NA, et al. Re: factors determining shape and symmetry in immediate breast reconstruction. Ann Plast Surg 2004;53:192–4 [DOI] [PubMed] [Google Scholar]
- 4.Qiao Q, Zhou G, Ling Y Breast volume measurement in young Chinese women and clinical applications. Aesthetic Plast Surg 1997;21:362–8 [DOI] [PubMed] [Google Scholar]
- 5.Brown RW, Cheng YC, Kurtay M A formula for surgical modifications of the breast. Plast Reconstr Surg 2000;106:1342–5 [DOI] [PubMed] [Google Scholar]
- 6.Galdino GM, Nahabedian M, Chiaramonte M, et al. Clinical applications of three-dimensional photography in breast surgery. Plast Reconstr Surg 2002;110:58–70 [DOI] [PubMed] [Google Scholar]
- 7.Kovacs L, Eder M, Papadopoulos NA, et al. Re: validating three-dimensional imaging of the breast. Ann Plast Surg 2005;55:695–6 [DOI] [PubMed] [Google Scholar]
- 8.Kovacs L, Yassouridis A, Zimmermann A, et al. Optimisation of the three-dimensional imaging of the breast region with 3D Laser Scanners. Ann Plast Surg 2006;56:229–36 [DOI] [PubMed] [Google Scholar]
- 9.Lee HY, Hong K, Kim EA Measurement protocol of women's nude breasts using a 3D scanning technique. Appl Ergon 2004;35:353–9 [DOI] [PubMed] [Google Scholar]
- 10.Losken A, Seify H, Denson DD, et al. Validating three dimensional imaging of the breast. Ann Plast Surg 2005;54:471–6, discussion 477–8 [DOI] [PubMed] [Google Scholar]
- 11.Losken A, Fishman I, Denson DD, et al. An objective evaluation of breast symmetry and shape differences using 3-dimensional images. Ann Plast Surg 2005;55:571–5 [DOI] [PubMed] [Google Scholar]
- 12.Isogai N, Sai K, Kamiishi H, et al. Quantitative analysis of the reconstructed breast using a 3 dimensional laser light scanner. Ann Plast Surg 2006;56:237–42 [DOI] [PubMed] [Google Scholar]
- 13.Smith DJ Jr, Palin WE Jr, Katch VL, et al. Breast volume and anthropomorphic measurements: normal values. Plast Reconstr Surg 1986;78:331–5 [DOI] [PubMed] [Google Scholar]
- 14.Westreich M Anthropomorphic breast measurement: protocol and results in 50 women with aesthetically perfect breasts and clinical application. Plast Reconstr Surg 1997;100:468–79 [DOI] [PubMed] [Google Scholar]
- 15.Kalbhen CL, McGill JJ, Fendley PM, et al. Mammographic determination of breast volume: comparing different methods. Am J Roentgenol 1999;173:1643–9 [DOI] [PubMed] [Google Scholar]
- 16.Malini S, Smith EO, Goldzieher JW Measurement of breast volume by ultrasound during normal menstrual cycles and with oral contraceptive use. Obstet Gynecol 1985;66:538–41 [PubMed] [Google Scholar]
- 17.Schultz RC, Dolezal RF, Nolan J Further applications of Archimedes' principle in the correction of asymmetrical breasts. Ann Plast Surg 1986;16:98–101 [DOI] [PubMed] [Google Scholar]
- 18.Kirianoff TG Volume measurements of unequal breasts. Plast Reconstr Surg 1974;54:616 [DOI] [PubMed] [Google Scholar]
- 19.Tegtmeier RE A quick, accurate mammometer. Ann Plast Surg 1978;1:625–6 [DOI] [PubMed] [Google Scholar]
- 20.Wilkie T Volumetric breast measurement during surgery. Aesthetic Plast Surg 1977;1:301–5 [DOI] [PubMed] [Google Scholar]
- 21.Campaigne BN, Katch VL, Freedson P, et al. Measurement of breast volume in females: description of a reliable method. Ann Hum Biol 1979;6:363–7 [DOI] [PubMed] [Google Scholar]
- 22.Edsander-Nord A, Wickman M, Jurell G Measurement of breast volume with thermoplastic casts. Scand J Plast Reconstr Surg Hand Surg 1996;30:129–32 [DOI] [PubMed] [Google Scholar]
- 23.Neal AJ, Torr M, Helyer S, et al. Correlation of breast dose heterogeneity with breast size using 3D CT planning and dose–volume histograms. Radiother Oncol 1995;34:210–18 [DOI] [PubMed] [Google Scholar]
- 24.Fowler PA, Casey CE, Cameron GG, et al. Cyclic changes in composition and volume of the breast during the menstrual cycle, measured by magnetic resonance imaging. Br J Obstet Gynaecol 1990;97:595–602 [DOI] [PubMed] [Google Scholar]
- 25.Sommer NZ, Zook EG, Verhulst SJ The prediction of breast reduction weight. Plast Reconstr Surg 2002;109:506. [DOI] [PubMed] [Google Scholar]
- 26.Lejour M Evaluation of fat in breast tissue removed by vertical mammaplasty. Plast Reconstr Surg 1997;99:386–93 [DOI] [PubMed] [Google Scholar]
- 27.Aslan G, Terzioglu A, Tuncali D, Bingul F Breast reduction: Weight versus volume. Plast Reconstr Surg 2003;112:339–40 [DOI] [PubMed] [Google Scholar]