Introduction
Insidious in presentation, ankle valgus may progress with growth, causing pronation, painful sub-fibular impingement, and excessive shoe wear. Children with neuromuscular disease may wear orthoses that provide support, but will not correct this deformity. While supramalleolar osteotomy may be considered, this is an invasive procedure requiring hospitalization, cast immobilization, and delayed weight-bearing. Medial malleolar hemi-epiphysiodesis with a cannulated screw has been used successfully, but there can be problems with hardware bending, migration, and retrieval. We sought to determine the effectiveness of guided growth with plate hemi-epiphysiodesis of the medial distal tibia in the treatment of this clinical problem.
Methods
Demographics
With institutional IRB approval, we undertook this retrospective review of charts and radiographs of patients with ankle valgus who were treated with guided growth to correct ankle valgus. From 2004 – 2009, a single surgeon used the 8-plate (Orthofix, Inc., McKinney, TX) for distal medial tibial epiphysiodesis on 41 patients. Exclusion criteria are as follows: inadequate radiographs or records, or patients with less than one year of follow-up. Using this set of criteria, 33 patients with 57 operative ankles were selected for analysis.
Surgical technique
Of the 33 patients, 15 underwent concomitant surgery. The surgery was undertaken on an outpatient basis, unless the additional procedures dictated otherwise. A 2 cm incision was made, centered over the distal medial tibial physis, with care taken to preserve the periosteum. Under fluoroscopic guidance, a Keith needle was inserted into the physis, in the midsagittal plane. A 12 mm 8-plate was slipped over the Keith needle and transfixed with 2 cannulated 4.5 mm screws. The length of the screw is typically 24 mm, however 16 mm screws may be used in smaller patients; the screws need not be parallel. No cast immobilization was required unless warranted by concomitant procedures. For patients using orthoses, we ascertained that these would not rub on the surgical site. The patients were then followed up every 6 months, obtaining radiographs when clinical correction was apparent.
Data Gathering
We reviewed charts for underlying diagnoses, complications, and time to correction. On pre-operative and follow-up weight-bearing radiographs, we measured the fibular station, as described by Malhotra and the lateral distal tibial angle, or LDTA, as described by Paley.1,2 The fibular station is based on the position of the distal fibular physis relative to the distal tibia physis. The published range for the LDTA is 86–92°.
Clinical and radiographic parameters were used to assess correction. Implants were routinely removed when the heel was clinically neutral to the calf and the ankle was neutral to 5 degrees of varus overcorrection according to the LDTA measurement unless the patient reached skeletal maturity. The rationale for producing slight overcorrection is to compensate for concomitant subtalar valgus and/or mitigate the effects of rebound valgus.
Analytic strategy
The sample was first characterized with respect to demographics, complications, prior medical history, measurements of LDTA, fibular station and rate of correction. Then, bivariate associations between LDTA (at pre-surgery, at follow-up and change in LDTA from pre-surgery to follow-up) and age were examined. Subsequent analysis using paired samples t-test was conducted to see whether there was a significant change in LDTA from pre-surgery to follow-up visit. Holding age, status of complication, those with a concomitant subtalar implant, and those with clubfoot constant, we performed multivariate regressions to determine how much of variations in the change of LDTA could be attributed to pre-surgery LDTA.
Results
The 33 children (57 ankles) who met the inclusion criteria for the study included 13 girls and 20 boys. Bilateral guided growth was performed 24 times with 7 single right-sided and 2 left-sided procedures. The most common underlying diagnosis was talipes equinovarus, noted in 13 patients. The clubfoot patients had all previously undergone a posterior medial release; this is not an uncommon sequela of club foot management.3 The clinical course of one patient with bilateral ankle valgus in the setting of surgically corrected clubfeet demonstrates treatment and LDTA measurement (Figs. 1a-1e). All underlying diagnoses are included in the master table of patient data, Table 1. Concomitant procedure types are represented in Table 2. The mean age range at the time of implant insertion was 10.4 years, with a range of 6.08 to 14.58 years. The mean postoperative follow-up was 27.12 months with a range of 12 to 57.5 months.
Figure 1.
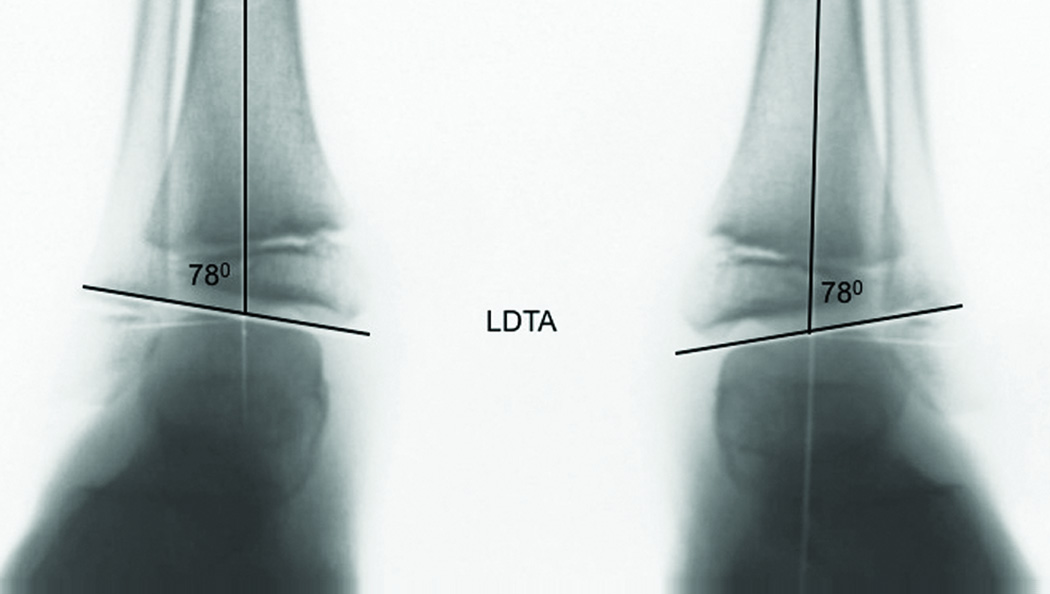
a. At age 6, a weightbearing AP view of the ankles demonstrates lateral impingement, with corresponding enlargement of the distal fibular epiphysis and lateral wedging of the tibial epiphysis. The LDTA (lateral distal tibial angle) = 78° compared to the normal value = 86°–92°.
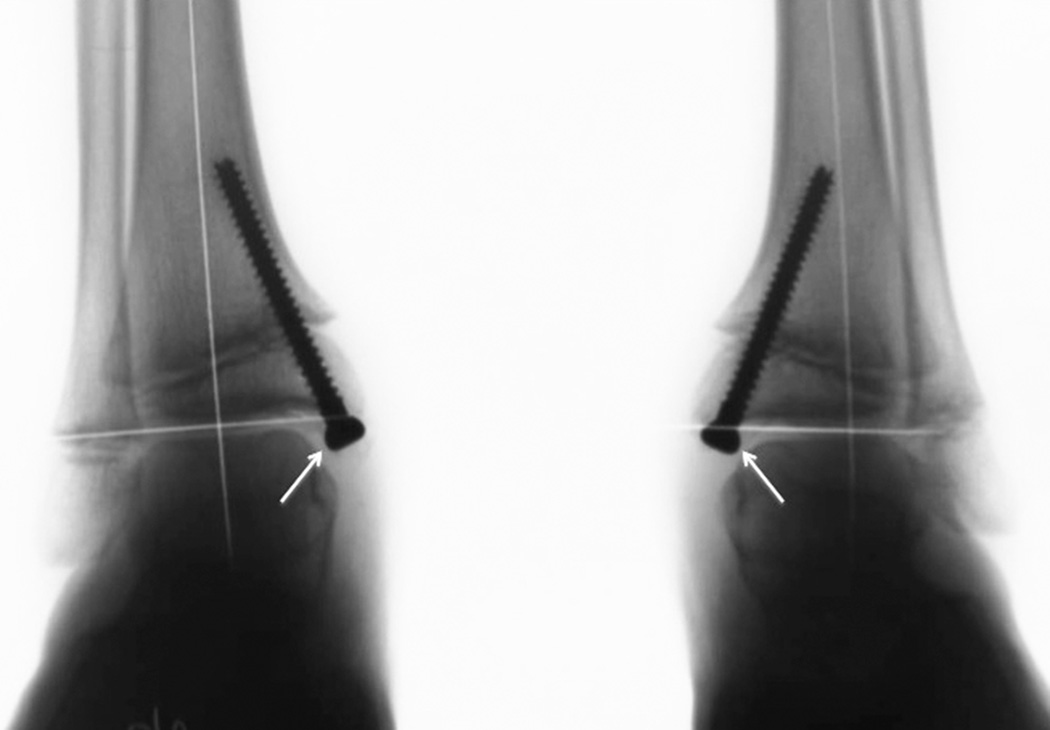
b. Two years following medial malleolar hemi-epiphysiodesis with transphyseal screws, the ankle valgus has corrected. The screw heads have “migrated”, becoming intra-articular and notching the talus.
c. By the age of 10, due to rebound growth, symptomatic ankle valgus has recurred.
d. Two years following guided growth with tension band plates, the ankle valgus has again corrected. The LDTA measures 90°, and the patient is asymptomatic. Note the lateral growth line and corresponding downward slope of the tibial physis.
e. Clinical correction at age 12. Follow-up will continue until maturity, repeating guided growth as necessary.
Table 1.
CTEV, congenital talipes equinovarus; MHE, multiple hereditary exostosis; LLI, limb length inequality; MED, multiple epiphyseal dysplasia;
| Patient | Age at insertion (y) |
Laterality | AssociateDiagnoses | Pre-op LDTA R-L(°) |
Final LDTA R-L(°) |
Pre-op Fibular Station R-L |
Final Fibular Station R-L |
Follow- up (mos) |
|---|---|---|---|---|---|---|---|---|
| 1 | 12.92 | Bil | Spina bifida | 73-69 | 82-84 | 1 1 | 2 2 | 57.50 |
| 2 | 7.75 | Bil | CTEV, genu valgum | 82-82 | 91-90 | 1 1 | 1 1 | 28.50 |
| 3 | 13.83 | L | Post traumatic | X-73 | X-86 | X 0 | X 0 | 38.25 |
| 4 | 12.17 | R | Right congenital vertical talus, genu valgum | 85-X | 90-X | 1-X | 1-X | 25.00 |
| 5 | 10.75 | R | Muscualr dystrophy, CTEV, gen varum | 80-X | 86-X | 1 X | 1 X | 16.00 |
| 6 | 14.00 | Bil | Mobius syndrome, CTEV | 77-74 | 95-91 | 1 1 | 1 1 | 19.50 |
| 7 | 9.67 | Bil | CTEV | 78-75 | 86-89 | 2 2 | 1 1 | 44.50 |
| 8 | 7.00 | Bil | CTEV | 82-82 | 86-87 | 1 1 | 1 1 | 40.25 |
| 9 | 11.58 | Bil | Down syndrome, genu valgum | 78-81 | 89-90 | 2 2 | closed | 45.00 |
| 10 | 6.50 | Bil | CTEV | 74-74 | 89-89 | 2 2 | 0 0 | 42.50 |
| 11 | 11.58 | Bil | CTEV, pes planovalgus, genu valgum | 80-81 | 90-90 | 0 1 | 0 0 | 17.50 |
| 12* | 11.92 | Bil | idiopathic, peroneal spastic flatfoot, hallux valgus | 83-84 | 97-94 | 1 1 | 0 0 | 40.25 |
| 13 | 9.25 | R | CTEV | 81-X | 90-X | 1 X | 1 X | 24.25 |
| 14 | 11.67 | Bil | Stickler syndrome, coxa vara | 71-70 | 80-76 | 2 1 | 1 1 | 38.75 |
| 15 | 8.25 | R | CTEV | 76-X | 83-X | 1 X | 1 X | 29.00 |
| 16 | 8.42 | R | Ollier's | 80-X | 86-X | 2 X | 1 X | 38.25 |
| 17 | 14.58 | Bil | discoid meniscus, miserable malalignment | 83-82 | 85-85 | 0 0 | 0 0 | 13.50 |
| 18 | 13.42 | Bil | right hemiparesis/stroke at age 4 | 74-76 | 71-82 | 1 0 | closed | 38.00 |
| 19 | 13.50 | R | Neurofibromatosis-1 | 76-X | 88-X | 3-X | 2 X | 30.75 |
| 20 | 6.08 | Bil | Apert syndrome, ball and socket ankle | 75-82 | 98-104 | 2 2 | 1 1 | 25.25 |
| 21 | 9.33 | Bil | Femoral anteversion; CTEV | 82-82 | 89-86 | 0 0 | 0 0 | 24.50 |
| 22 | 6.58 | L | CTEV | X-82 | X-90 | X 1 | X 0 | 24.75 |
| 23 | 8.58 | Bil | MHE, LLI, Left coxa valgus | 82-82 | 81-85 | 3 3 | 3 3 | 31.00 |
| 24 | 11.42 | Bil | CTEV with residual adductus | 83-76 | 89-91 | 0 0 | 0 0 | 15.75 |
| 25 | 11.50 | Bil | Autism; unidentified syndrome | 82-82 | 89-90 | 0 0 | 0 0 | 17.25 |
| 26* | 7.92 | Bil | Soto syndrome;pes planovalgus | 79-75 | 92-92 | 1 2 | 1 1 | 18.75 |
| 27 | 11.83 | Bil | CTEV, pes planovalgus, dorsal bunion | 79-83 | 88-94 | 1 1 | 1 1 | 24.75 |
| 28 | 11.75 | Bil | Genu valgum | 81-81 | 89-87 | 0 0 | 0 0 | 12.75 |
| 29* | 7.50 | Bil | Carpenter syndrome | 74-79 | 88-93 | 1 0 | 0 0 | 18.75 |
| 30* | 8.75 | Bil | MED versus pseudoachondroplasia | 76-68 | 90-89 | 1 1 | 1 1 | 13.50 |
| 31 | 12.08 | Bil | Diplegia | 82-79 | 86-87 | 1 1 | 1 1 | 13.75 |
| 32 | 11.75 | R | Idiopathic | 82-X | 86-X | 0 X | 0 X | 12.00 |
| 33 | 10.58 | Bil | Idiopathic | 79-82 | 86-90 | 1 1 | 1 1 | 12.00 |
concomitant bilateral subtalar arthoreisis.
Table 2.
HE, hemi-epiphyseodesis; HWR, hardware removal; TAL, tendo-Achilles lengthening
| Concomitant Procedure |
Number of Patients |
|---|---|
| Distal Femur medial HE | 10 |
| Subtalar Arthroreisis | 4 |
| 1st Metatarsal HE | 2 |
| Proximal tibia HE | 2 |
| Femur HWR | 1 |
| Tibia HWR | 1 |
| TAL | 1 |
| Distal Femur anterior HE | 1 |
| Osteochondritis dissecans drilling | 1 |
| Midfoot osteotomy | 1 |
| Fowler procedure | 1 |
| Adductor release | 1 |
| Psoas release | 1 |
| Patellar realignment | 1 |
| Femoral rotational osteotomy | 1 |
| Midfoot capsulotomy | 1 |
| 3rd toe flexor tenotomy | 1 |
| Distal hamstring release | 1 |
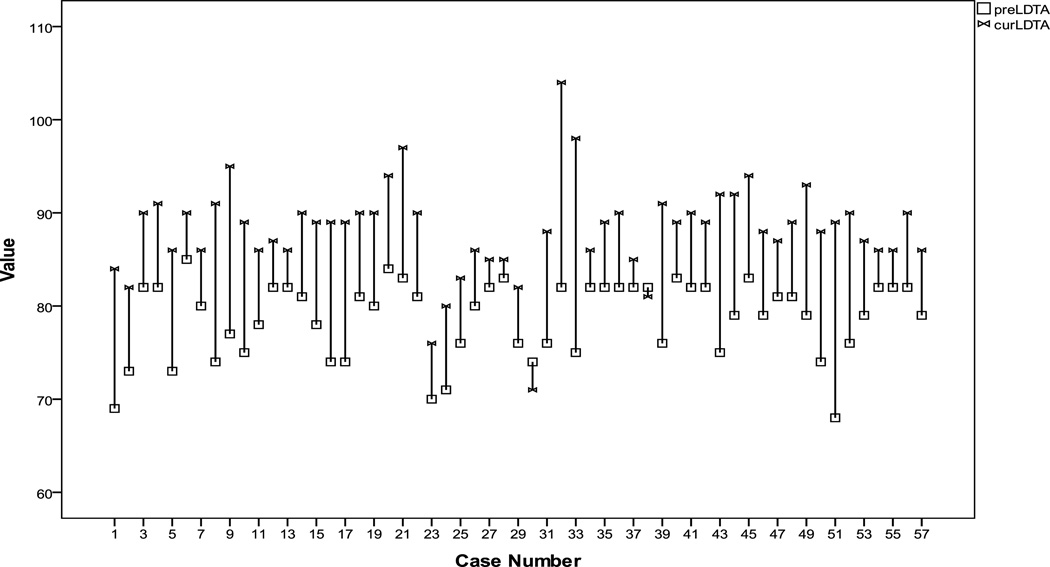
The LDTA was measured to be a preoperative mean of 78.7° (68° – 85°). At time of removal the LDTA averaged 90° (76° – 103°). The removal radiographs were also final radiographs in 22 ankles. On final follow-up radiographs, the LDTA averaged 88.2° (71° – 104°). Figure 2 shows a grand chart of each patient’s pre-op and follow-up LDTA measurements. The mean change in LDTA from pre-op to follow-up was 9.5 with a standard deviation of 5.3. Paired samples t-test reveals that the follow-up LDTA measures were significantly higher than the pre-op LDTA (t=13.4, p<0.05). Furthermore, keeping age, complication status, subtalar status and clubfoot status constant, we found that 19.3% of the variations in the change of LDTA were accounted for by the pre-op LDTA. Gradual return toward valgus after implant removal was sometimes noted but, to date, has been asymptomatic.
Figure 2.
Distribution of patients’ pre-op and follow-up LDTA measurements.
Table 3 represents the bivariate analyses indicating there were significant correlations between age and LDTA at follow-up (r=−0.313, p<0.05), and between age and the change in LDTA (r=−0.264, p<0.05). Younger patients tend to associate with larger LDTA at follow-up and greater improvement in LDTA. There was no correlation between age and LDTA at pre-surgery.
Table 3.
LDTA, lateral distal tibial angle.
| Correlations | ||||
|---|---|---|---|---|
| Pre-LDTA | Cur-LDTA | Δ LDTA | ||
| AGE (years) | Pearson Correlation | −0.040 | −0.313* | −0.264* |
| Sign. (2-tailed) | p= 0.768 | p= 0.018 | p= 0.047 | |
| N | 57 | 57 | 57 | |
Correlation is significant at the p< 0.05 level (2-tailed).
The fibular station improved in 15 of the 57 ankles. The mean preoperative station was 1 (0–3). Fibular station at implant removal averaged 0.8 (0–3). Final fibular station measurements averaged 0.7 (0–3).Thirty-five ankles had no change in fibular station. Thirteen ankles had an improvement of one grade in fibular station. One case, both ankles, of a 6.5 year-old bilateral clubfoot patient improved from station 2 to 0. Both ankles in a 12.9 year-old boy increased in station from 1 to 2. Two patients, four ankles, were skeletally mature at time of final measurement.
The rate of correction of ankle valgus was calculated up to implant removal, most recent follow-up, or skeletal maturity, depending on the situation. The average rate of correction was 0.6°/month (range, 0.15° – 1.6°/month). There was no correlation between rate of correction and age at procedure or underlying diagnosis.
None of these patients have required an osteotomy. Interestingly, one patient with right hemiparesis after a stroke at age 4, previously had supramalleolar osteotomies for ankle valgus. Three patients had previous correction with transmalleolar screws and the 8-plate was employed for their recurrent valgus. One patient, with multiple hereditary exostosis, had reinsertion of transmalleolar screw by another surgeon for a residual valgus LDTA of 81° as this surgeon had removed the 8-plate prior to full correction at an LDTA of 84°.
There were no cases demonstrating symptomatic varus or premature physeal closure. Implant removal, on an outpatient basis, was free of complications. Two skeletally mature patients have plates in situ that may be removed electively. Complications included two deep infections. One was treated with irrigation and debridement and implant removal three weeks after insertion. The ankle with early implant removal resulted in a final LDTA of 71° but had hindfoot varus that resulted in a neutral walking position. The other deep infection was treated with irrigation and debridement, antibiotics, and retention of implants. This patient was autistic and had picked at his incision. There were also two suture reactions treated with oral Clindamycin. One hardware revision for distal screw migration outward and another to change to a longer distal screw were performed.
Of note, in the eight patients excluded for inadequate radiographs, one infection with Klebsiella was present. This was treated with irrigation and debridement and antibiotics with retention of implants. This patient was also autistic and had picked at his incisions.
Discussion
Progressive ankle valgus is common in a variety of conditions. Without appropriate radiographs, ankle valgus may be mistaken for hindfoot valgus and mismanaged accordingly. Orthoses do not change the natural history, which is one of insidious progression.
Etiology
While the relative length of the tibia and fibula are equal, the latter should project more distal at the ankle, providing a stable buttress and bearing up to 15% of weight. In the growing child, the distal fibular physis should be at or below the level of the plafond. Elevation of the distal fibular physis should raise suspicions about ankle valgus. Ankle valgusis seen in a variety of conditions including neuromuscular disorders, clubfoot, hereditary multiple exostoses, neurofibromatosis, skeletal dysplasias, and genetic syndromes such as Down. There is also an idiopathic variety known as Volkman’s ankle, a condition that may be inherited. Unilateral ankle valgus may also be acquired following fracture, supramalleolar osteotomy, free fibular graft harvesting, and limb lengthening.
Pathophysiology
The insidious progression of ankle valgus results in lateral shift of the ground reaction force, wedging of the distal lateral tibial epiphysis and, often, fibular impingement on the hind foot.4–7 Clinically, the heel is shifted laterally; the medial malleolus becomes increasingly prominent and may rub on shoes or orthoses, irritating the skin. Frequently there is lateral pain due to fibular impingement. Radiographically, much of the medial malleolus is delayed in ossifying, thus not visible. In older children, one may observe an os subtibiale, presumably due to traction on the medial ligaments. Typical wedging of the lateral aspect of the distal tibial epiphysis is noted. The distal fibular epiphysis is often relatively broad as a consequence of increased weight bearing, beyond the normal amount of 15%. This reflects the Hueter-Volkmann effect.
Radiographic assessment
On a standing anteroposterior radiograph of the ankles, one should note the fibular station (Malhotra) and the lateral distal tibial angle, LDTA (86–92°). Although the two deformities may occur simultaneously, one must distinguish between ankle valgus and hind foot valgus in order to obtain a satisfactory treatment outcome. Without a standing anteroposterior radiograph of the ankles, ankle valgus may be mistaken for hind foot valgus and mismanaged accordingly.8 Ankle valgus will cause parallax distortion on the lateral weight-bearing radiograph of the foot leading to spurious measurement of the talocalcaneal angle and consequent overestimation of hind foot valgus.9,10
Treatment
A variety strategies have been employed to treat ankle valgus in the growing child with variable success.11–13 Medial malleolar hemiepiphysiodesis may be accomplished with atransphyseal screw.14,15 While this is often successful, implant retrieval may be challenging. Bent and broken screws and those with intrarticular migration may compromise the effort. (Fig. 1b)
Because of these occasional problems, and the theoretical disadvantage of violating the physis with a rigid implant, the senior author began using guided growth with the plate hemi-epiphysiodesis. This has been proven to be efficacious, not only at the knee, but at the ankle as well.16–18 The extra-periosteal flexible tension band provided a rate of correction of 0.6°/month in this group of patients. This is comparable to a rate of 0.59°/month previously reported by Davids, et.al.15, using a medial malleolar screw.
Our series found correlations between age at insertion of the implant, final LDTA and change in LDTA. They finished treatment with overall higher LDTA. These patients should be observed for rebound valgus as they have more growth potential remaining. However, they can also have the procedure easily repeated. Our data do not show that younger patients had greater overall correction but this can be an area of future study.
In analyzing our largest etiologic cohort, the post surgical clubfeet, we found no correlations with LDTA measurements. We also evaluated the patients with concomitant subtalar implants for hindfoot valgus, finding no significant associations with the LDTA. These patients would theoretically have a change in ground reaction force that could alter the distal tibial physis. In our series, ankle valgus and its correction appears to be independent of etiology or concomitant alteration in hindfoot mechanics in the timeframe of the study.
We should stress the importance of excellent post-operative care in patients with propensity to harm their incisions as two of our infections were attributed to this. Perhaps, these children would benefit from a weight bearing cast for 2–3 weeks to allow the wound to heal. Our overall infection rate was 3.5%. The reported rate with transmalleolar screws is 2%–3.4%.14,15 Complaints of implant prominence were not recorded in this series and none of the implants had to be removed prematurely for this reason. However, it is important to educate the parents and orthotist to avoid direct pressure over the implant. As the correction evolves, the hardware prominence becomes less noticeable. The senior also preferentially employs the 24 mm screws to ensure adequate purchase.
In summary, guided growth of the distal medial tibia is, in our opinion, the treatment of choice for ankle valgus in the growing child or adolescent. The use of the non-locking 8-plate as a tension band provides gradual correction. We prefer this over the transmalleolar screw that violates the physis and may be difficult to remove. The ease and efficacy of this minimally invasive form of treatment and have rendered osteotomy unnecessary in this series. It is safe, well tolerated, and may readily be combined with other treatment. Implant removal is facilitated and, by sparing periosteal damage, permanent arrest has not been observed. Should rebound deformity ensue, the process may be easily repeated.
Acknowledgments
Dr. Stevens has licensed the 8-plate to Orthofix, Inc (Verona, Italy/McKinney, Texas).
None of the authors received pharmaceutical or industry support for this study.
This investigation was supported by the Public Health Services research grant numbers UL1-RR025764 and C06-RR11234 from the National Center for Research Resources by the contributions of Man Hung, Ph.D.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Peter M. Stevens, Department of Orthopaedics, University of Utah, Salt lake City, UT
Jason M. Kennedy, Department of Orthopedics, Cook Children’s Medical Center, Fort Worth, TX
Man Hung, Department of Orthopaedics, University of Utah, Salt lake City, UT
References
- 1.Malhotra D, Pau R, Owen R. Valgus Deformity of the Ankle in Children With Spina Bifida Aperta. J Bone Joint Surg. 1984;66:381–385. doi: 10.1302/0301-620X.66B3.6373777. [DOI] [PubMed] [Google Scholar]
- 2.Paley D, Herzenberg JE. Principles of Deformity Correction. Berlin Heidelberg New York: Springer-Verlag; 2002. [Google Scholar]
- 3.Stevens PM, Otis S. Ankle Valgus and Clubfeet. J Pediatr Ortho. 1999;19:515–517. doi: 10.1097/00004694-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Stevens PM, Arms D. Postaxial Hypoplasia of the Lower Extremity. J Peditr Ortho. 2000;20:166–172. [PubMed] [Google Scholar]
- 5.Noonan K, Feinberg, et al. Natural History of Multiple Hereditary Osteochondromatosis of the Lower Extremity and Ankle. J Pediatr Orthop. 2002;22:120–124. [PubMed] [Google Scholar]
- 6.Stevens PM, Aoki S, Olson P. Ball and Socket Ankle. J Pediatr Orthop. 2006;26:427–431. doi: 10.1097/01.bpo.0000217713.80233.c5. [DOI] [PubMed] [Google Scholar]
- 7.Takikawa K, Haga N, Tanaka H, et al. Characteristic factors of ankle valgus with multiple cartilaginous exostoses. J Pediatr Orthop. 2008;28:761–765. doi: 10.1097/BPO.0b013e3181847511. [DOI] [PubMed] [Google Scholar]
- 8.Scott S, Janes P, Stevens PM. Grice Subtalar Arthrodesis Followed to Skeletal Maturity. J Pediatr Orthop. 1988;8:176–183. [PubMed] [Google Scholar]
- 9.Stevens PM. Effect of Ankle Valgus on Radiographic Appearance of the Ankle. J Pediatr Orthop. 1988;8:184–186. [PubMed] [Google Scholar]
- 10.Machen MS, Stevens PM. Should full-length standing anteroposterior radiographs replace the scanogram for measurement of limb length discrepancy? J Pediatr Orthop. 2005;14:30–37. doi: 10.1097/01202412-200501000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Stevens PM, Toomey E. Fibular-Achilles tendodesis for paralytic ankle valgus. J Pediatr Orthop. 1988;8:169–175. [PubMed] [Google Scholar]
- 12.Beals RK. The treatment of ankle valgus by surface epiphysiodesis. Clin Orthop Relat Res. 1991;266:162–169. [PubMed] [Google Scholar]
- 13.Burkus JK, et al. Valgus deformity of the ankle in myelodysplastic patients. J Bone Joint Surg. 1983;65-A:1157–1162. [PubMed] [Google Scholar]
- 14.Stevens PM, Belle R. Screw Epiphysiodesis for Ankle Valgus. J Pediatr Ortho. 1997;17:9–12. [PubMed] [Google Scholar]
- 15.Davids JR, Valadie AL, et al. Surgical Management of Ankle Valgus in Children: Use of a Transphyseal Medial Malleolar Screw. J Pediatr Orthop. 1997;17:3–8. [PubMed] [Google Scholar]
- 16.Stevens PM. Guided Growth: 1933 to the Present. Strat Traum Limb Recon. 2006;1:29–35. [Google Scholar]
- 17.Stevens PM. Guided Growth for Angular Correction. J Pediatr Orthop. 2007;27:253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 18.Stevens PM. [Accessed December 10, 2009];Ankle Valgus, Pediatrics [e-medicine] 2008 November 25; Available at http://emedicine.medscape.com/article/1358051-overview.