Abstract
Background
Telephone helplines are frequently and repeatedly used by individuals with chronic mental health problems and web interventions may be an effective tool for reducing depression in this population.
Aim
To evaluate the effectiveness of a 6 week, web-based cognitive behaviour therapy (CBT) intervention with and without proactive weekly telephone tracking in the reduction of depression in callers to a helpline service.
Method
155 callers to a national helpline service with moderate to high psychological distress were recruited and randomised to receive either Internet CBT plus weekly telephone follow-up; Internet CBT only; weekly telephone follow-up only; or treatment as usual.
Results
Depression was lower in participants in the web intervention conditions both with and without telephone tracking compared to the treatment as usual condition both at post intervention and at 6 month follow-up. Telephone tracking provided by a lay telephone counsellor did not confer any additional advantage in terms of symptom reduction or adherence.
Conclusions
A web-based CBT program is effective both with and without telephone tracking for reducing depression in callers to a national helpline.
Trial Registration
Introduction
Telephone helplines provide 24 hour, non-directive crisis and counselling services to large numbers of callers in the community using a volunteer workforce. In 2009, major helplines in the United Kingdom received over 4 million calls [1]. In Australia, over 850,000 calls are answered annually by the large telecounselling providers, with 20% of callers referred by healthcare providers. Although designed primarily to provide immediate crisis intervention, these services are frequently used by callers experiencing chronic mental health problems. Over 40% of callers phone the service 20 times or more, 78% of callers experience depressive symptoms, and the prevalence of anxiety in this group is between 2 to 6 times that of the population [2], [3], [4]. In addition to providing non-directive counselling, telephone helpline agencies refer callers to mainstream mental health services [5]. However, mental health services are often difficult to access because of cost, structured consultation times, waiting list length, and location. In addition, mainstream mental health services may not inspire trust.
An alternative to referral to another agency is to provide low cost, evidence-based, high quality mental health interventions within the helpline service itself. The telephone and the Internet have been used separately to effectively treat physical and mental health problems [6], [7], [8], [9]. Cognitive behaviour therapy (CBT) offered through the telephone has been shown to significantly reduced depression [10]. A range of software applications available on the web have also delivered effective CBT to depressed samples [11], reduced depression in school settings [12] and in general practice environments [13], [14], either with or without support from mental health professionals, paraprofessionals or teachers [11]. Based on reviews of the evidence, the provision of support or tracking (ongoing contact with users during an intervention) has been proposed to increase adherence to treatment, prevent dropout, and improve efficacy [6]. Reviews of Internet-based interventions for depression have shown that treatments delivered with therapist support show larger between-group effect sizes than unsupported treatments [6], [8]. However, few studies have compared supported and unsupported interventions in the same trial [11] and so the issue of whether support adds unequivocal benefit has not yet been resolved. In addition, efficacy may vary depending on the type of support provided (e.g. automated versus non-automated, professional versus non-professional). Like therapist supported treatments, there is evidence to suggest that treatments involving assistance from a non-professional are more effective than control conditions for depression [7], [15], [16], [17]. Evidence from Titov and colleagues suggests that treatments supported by professionals and non-professionals are equally effective in the treatment of depression [18]. However, to-date, no studies have directly compared the relative efficacy of an Internet-based self-help treatment monitored by non-professionals (such as volunteer telephone counsellors) with a non-guided treatment.
One method of implementing a low cost, high quality intervention within a helpline service may be to provide callers with proven web-based programs for anxiety and depression in combination with telephone tracking by a telecounsellor. Volunteer counsellors constitute a ready made workforce to refer and/or guide callers, making it possible to use the existing call centre structure to deliver immediate, cost-effective, evidence-based help. However, it is important to establish the effectiveness of such a service and to what extent if at all counsellor guidance is likely to improve the outcomes of the service.
To our knowledge, no trials have evaluated the effectiveness of web based interventions within existing helpline or call centre services. Our study aimed to evaluate the effectiveness of a web-based CBT program delivered within a helpline, and to examine the benefit of weekly telephone contact (tracking) on efficacy, adherence and dropout. Over a period of 6 weeks, participants were randomised to one of four conditions: web only, where participants received web-based automated depression psychoeducation combined with 5 modules of CBT, web with tracking, where callers received the web intervention and were phoned weekly by telephone counsellor to monitor their completion of the intervention, tracking only, where callers were telephoned weekly but were not provided with the web intervention, and the control condition, where participants received neither the web intervention nor weekly telephone calls. In all four conditions, participants were able to contact and receive usual care from the helpline service, if required.
We hypothesised that (a) the delivery of a web-based CBT program would be more effective than the control condition; (b) that the combination of tracking with the web intervention would be superior to the other three conditions, and (c) that the addition of tracking to the web intervention (web with tracking) would be superior to delivery of the web only condition in terms of effectiveness and adherence.
Methods
The protocol for this trial and supporting CONSORT checklist are available as supporting information; see Checklist S1 and Protocol S1.
Ethics statement
Ethical approval for the trial was granted by the Australian National University Human Research Ethics Committee (Protocol no. 2007/12).
Participants
Callers to Lifeline's 24 hour telephone counselling service in four major Australian cities were invited to participate in the trial by a telephone counsellor either during or at the conclusion of a counselling call, between July 2007 and January 2009. Callers who were considered by the telephone counsellor to be suicidal or experiencing high levels of distress were excluded from receiving a recruitment invitation. Callers willing to receive further information about the trial provided contact information and were later telephoned and screened for eligibility by the trial coordinator. Callers were eligible for inclusion if they spoke English, had Internet access for at least half an hour a week, were aged 18 years or older, and scored 22 or above on the 10 item Kessler Psychological Distress Scale (K10) [19]. The exclusion criteria were a current or previous diagnosis of schizophrenia or bipolar disorder, current treatment with CBT, and significant reading impairment, and these were assessed directly using single item questions. Ineligible participants were offered brochures containing information about the online interventions.
Design and procedures
Following screening, informed written consent was obtained from participants and baseline data were collected through a self report questionnaire mailed to participants. A block randomisation procedure with stratification based on sex, site of recruitment and severity of psychological distress at screening was used. Allocation of participants to trial conditions was conducted independently by a research assistant not otherwise involved with the trial. Following randomisation, all participants were contacted by telephone and mailed the relevant materials for their allocated condition.
Intervention and trial conditions
Web only
The web only intervention delivered online psychoeducation (in Week 1, provided by BluePages: bluepages.anu.edu.au) combined with CBT (in weeks 2–6, provided by MoodGYM: moodgym.anu.edu.au). Both BluePages and MoodGYM have been shown to reduce depressive symptoms in community users [15]. A printed manual containing week by week instructions for accessing the web programs (via a login) was sent to participants by mail at the start of the trial.
BluePages is a freely accessible, psychoeducational website that contains information and resources related to depression. The website includes information about the symptoms of depression, ratings of the effectiveness of various depression treatments, and links to available help and resources. The MoodGYM program is a free to end-user, online CBT program for depression. The program is divided into 5 modules designed to be completed sequentially. Each module focuses on a particular aspect of CBT, such as cognitive restructuring, the relationship between thoughts and feelings, behavioural activation, relaxation, and problem solving. Each MoodGYM module contains written information, animations, interactive exercises and quizzes.
Web with tracking
In the web with tracking condition, participants completed the web intervention and also received a weekly 10 minute telephone call from a telephone counsellor, with the call addressing any issues associated with the participants' use of the online programs.
Tracking only
In the tracking only condition, participants received a weekly 10 minute phone call from a telephone counsellor. The calls focussed on various environmental and lifestyle factors associated with depression. No advice, therapy or counselling was offered in either of the tracking conditions.
Control condition
In the control condition, participants received neither tracking nor the web intervention.
Participants in all 4 conditions were invited to use the helpline, which provided usual emergency or support services if required.
Measures
Data were obtained by self report questionnaires mailed to participants at baseline, post intervention, and 6 months post intervention.
Screening and demographic variables
Previous history of depression, panic, social phobia and specific phobia were assessed at screening. Sex, age, years of education, relationship status, and employment status were assessed at baseline.
Depression
Depression symptoms were measured by the Center for Epidemiologic Studies Depression Scale [20] (CES-D), a widely used, 16 item scale with strong reliability and validity [20], [21], [22], [23], [24], [25], with a range of scores of 0 to 60. The CES-D was used as a continuous variable to examine symptom severity, and was also dichotomised into depression ‘cases’ and ‘non-cases’ in order to map the results into clinically meaningful outcomes. Depression caseness was measured by a score of 16 or above on the CES-D [20]. Studies have estimated reasonable sensitivity (84%–93%) and specificity (69%–74%) of the CES-D using this cutoff [26], [27].
Dropout
Dropout was measured by questionnaire completion at post intervention and 6 months.
Adherence
Program adherence was measured by number of visits to the BluePages psychoeducation site and by the number of MoodGYM program modules completed (ranging from 0 to 5).
Power
The total target sample size was 400 with 100 participants assigned to each intervention arm. This would enable the detection of differences of means of less than 0.3 standard deviation (SD) units comparing treatment arms, with 80% power and ά = .05, conservatively assuming a correlation of 0.5 between measurements on different occasions. This sample size was motivated by the desire to evaluate the augmentation of the web intervention with tracking, a difference which was not expected to be as large as for the intervention itself. However, the rate of recruitment prompted reconsideration of the target sample size. The achieved sample size of 155 participants maintained power above 80% to detect differences of means of less than 0.5 standard deviation (SD) units in planned comparisons between individual treatment arms. Power calculations were undertaken using G*Power 3.1.0 [28].
Statistical analysis
Data were analysed using SPSS release 18.0.1 for Windows [29]. A significance level of .05 was used for all outcome variables. The primary outcome variable was analysed on an intention to treat (ITT) basis using mixed models repeated measures ANOVA, with measurement occasion as a within groups factor and intervention condition as a between groups factor. Within person variation was modelled using an unstructured covariance matrix. Widely used methods of dealing with missing observations due to drop out such as ‘last observation carried forward’, treat the substituted values as real observations and make uncertain assumptions about the mechanism of missingness. Mixed modelling allows the use of all available data for each participant to yield unbiased estimates of effects under the assumption that missingness is either completely at random (MCAR) or at random conditional on observed data (MAR) [30]. Planned contrasts were used to compare intervention and control groups at post intervention and 6 month follow up. While multiple tests are reported post intervention and at 6 month follow-up, adjustments to p-values were not undertaken in the primary analyses due to the a priori nature of the comparisons involved and to ensure comparability of results with simpler two-arm trials.
Effect sizes (Hedges' g) were calculated by dividing the mean difference between conditions at post intervention and 6 month-follow up by the pooled standard deviation of the groups, which was computed using the method proposed by Hedges [31]. Confidence intervals for the effect sizes were calculated using the method proposed by Kelley [32]. Logistic and linear regressions examined differences between conditions on all baseline variables, and logistic regressions were used to assess the effect of the intervention on participant dropout. Logistic regressions were also used to investigate predictors of missingness (failure to complete a questionnaire) post intervention and at 6 month follow-up. The number needed to treat (NNT) was calculated for participants above caseness criteria at baseline. NNT is an index of the effectiveness of an intervention reflecting the average number of participants meeting criteria for a disorder who need to be treated in order to result in one person remitting from the condition. Confidence intervals for NNT may include infinity and extend to regions which imply that, comparatively, participants are harmed by an intervention as indexed by an analogous number needed to be harmed (NNH) value [33]. Confidence intervals were estimated using the method proposed by Bender [34]. Data inspection prior to analysis suggested that two cases in the web with tracking condition had aberrant patterns of change, each having moderate CES-D scores at baseline and extremely severe scores post intervention. In one case, this was able to be linked to the diagnosis of a life threatening illness. Due to distortion of the variance and violation of the assumption of normality [35], these participants were deleted for the primary analyses. However, additional analyses were conducted with these cases included.
Results
Participation rates and sample characteristics
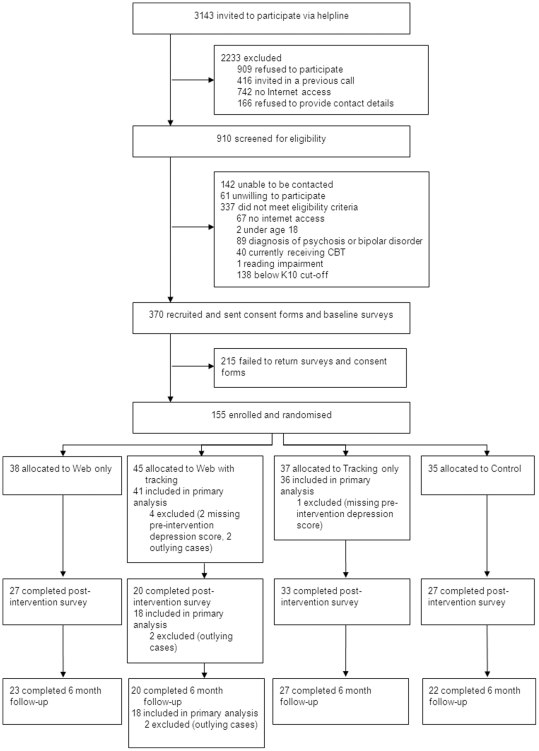
3143 callers were invited to be screened for participation in the trial during the recruitment period (Figure 1). Of these, 910 (28.9%) agreed to be screened for eligibility. 142 (15.6%) were unable to be contacted, 61 (6.7%) were later unwilling to participate, and 337 (37.0%) did not meet eligibility criteria. The most common reasons for ineligibility were a score of less than 22 on the K10 (138; 40.9%), a diagnosis of schizophrenia or bipolar disorder (89; 26.4%), or no Internet access (67; 19.9%). 370 people were eligible for inclusion in the trial, and of these, 155 completed informed consent procedures and baseline assessments, and were randomised to trial conditions, resulting in a 42% acceptance rate. 107 (69%) returned post intervention surveys, and 92 (59%) completed the 6 month follow up.
Figure 1. Flow of participants through the trial.
There were no significant differences across trial conditions on any baseline variables (Table 1). Trial condition and number of MoodGYM modules completed were significant predictors of missingness (failure to complete a questionnaire) at post intervention. The odds of missingness at post intervention were greater for participants in the Internet plus tracking condition, relative to participants in the control condition (odds ratio 6.46, 95% CI: 2.01 to 20.77, p = .002). Those who completed more MoodGYM modules had reduced odds of missingness at post intervention (odds ratio 0.49, 95% CI: 0.35 to 0.69, p<.001). At 6 month follow-up, those who completed more MoodGYM modules also had reduced odds of missingness (odds ratio 0.56, 95% CI: 0.41 to 0.75, p<.001). Pre intervention psychological distress, sex, age, pre intervention depression symptoms, pre intervention anxiety symptoms and whether participants received their “preferred” trial condition did not predict missingness at post intervention or 6 month follow-up.
Table 1. Baseline characteristics of randomised participants.
| Condition | ||||
| Web only (n = 38) | Web with tracking (n = 45) | Tracking only (n = 37) | Control (n = 35) | |
| Sex (female), n (%) | 33 (86) | 37 (82) | 29 (78) | 28 (80) |
| Age (years), mean (SD) | 37.5 (12.0) | 41.7 (12.1) | 43.4 (12.6) | 43.7 (12.3) |
| Years spent in education*, mean (SD) | 13.3 (2.7) | 14.0 (2.7) | 13.1 (2.6) | 13.4 (2.7) |
| Relationship status, n (%): | ||||
| Married/cohabiting | 10 (26) | 11 (24) | 14 (38) | 8 (23) |
| Divorced/separated/widowed | 11 (29) | 21 (47) | 16 (43) | 16 (46) |
| Never married | 17 (45) | 13 (29) | 7 (18) | 11 (31) |
| Employment status*, n (%): | ||||
| Employed full time | 8 (21) | 9 (20) | 10 (27) | 9 (26) |
| Employed part time | 11 (29) | 13 (29) | 4 (11) | 8 (23) |
| Not in labour force | 19 (50) | 22 (49) | 23 (62) | 18 (51) |
| History of previous depression*, n (%) | 35 (92) | 41 (91) | 33 (89) | 35 (100) |
| Experience of panic attacks in last 4 weeks*, n (%) | 26 (68) | 33 (73) | 27 (73) | 29 (83) |
| History of social phobia*, n (%) | 19 (50) | 29 (64) | 24 (65) | 21 (60) |
| History of specific phobia*, n (%) | 8 (21) | 7 (16) | 5 (14) | 5 (14) |
| K-10 score, mean (SD) | 32.4 (6.3) | 32.4 (5.6) | 32.4 (5.9) | 34.0 (5.5) |
| CES-D score*, mean (SD) | 35.0 (10.8) | 34.4 (10.2) | 37.6 (10.7) | 38.6 (8.8) |
| Caseness (score on CES-D ≥16)*, n (%) | 36 (95) | 42 (93) | 35 (95) | 35 (100) |
Not all participants completed all questions.
K-10 = Kessler 10 Psychological Distress Scale.
CES-D = Centre for Epidemiological Studies - Depression Scale.
*Education (n = 150); Employment (n = 154); Depression history (n = 154); Panic attacks (n = 153); Social phobia (n = 151); Specific phobia (n = 152); Baseline CES-D (n = 152); Caseness (n = 152).
Depression symptoms
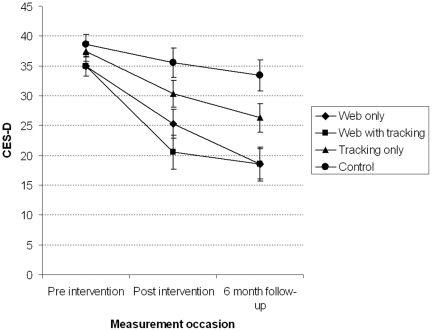
A significant occasion by condition interaction was found for depression symptoms, F(6,100.5) = 2.97, p = .01), indicating different patterns of change between conditions across measurement occasion. Observed means for all conditions at baseline, post intervention and 6 month follow-up are shown in Table 2. Figure 2 displays mean depression symptoms over time for each condition. Planned contrasts tested the differences in change across conditions from baseline to post intervention and 6 month follow up (Table 3). Compared to the control condition, decline in depression symptoms from baseline to post intervention was greater for participants in the web only and web with tracking conditions. Decline in symptoms did not differ significantly between the web only and web with tracking conditions from baseline to post intervention. Symptoms for participants in the tracking only condition fell between the control and the web only conditions, and did not differ significantly from either. This pattern of results was repeated in all contrasts comparing change from baseline to the 6 month follow-up. Effect sizes for the difference between the intervention and control conditions at post intervention and 6 month follow-up are presented in Table 4. Post intervention, large effect sizes were observed between the web only and the control condition (g = 0.76) and the web with tracking and the control condition (g = 1.04). The sizes of these effects increased at 6 month follow-up (g = 1.19 and 1.26, respectively). Moderate effects were observed when the web intervention conditions were compared to the tracking only condition at post intervention and at 6 month follow-up.
Table 2. Observed means (SD) and caseness (%) on the CES-D for each trial condition at pre intervention, post intervention and six month follow up.
| Measurement occasion | |||||||||
| Pre intervention | Post intervention | 6 month follow-up | |||||||
| n | Mean (SD) | Caseness (%) | n | Mean (SD) | Caseness (%) | n | Mean (SD) | Caseness (%) | |
| CES-D | |||||||||
| Web only | 38 | 35.0 (10.8) | 36 (94.7) | 27 | 24.4 (13.6) | 19 (70.4) | 23 | 18.0 (13.0) | 10 (43.5) |
| Web with tracking | 41 | 34.9 (10.1) | 40 (97.6) | 18 | 21.0 (12.4) | 12 (66.7) | 18 | 18.4 (10.4) | 9 (50.0) |
| Tracking only | 36 | 37.6 (10.7) | 35 (97.2) | 33 | 29.6 (13.2) | 29 (87.9) | 27 | 26.0 (13.7) | 18 (66.6) |
| Control | 35 | 38.6 (8.8) | 35 (100.0) | 27 | 35.1 (13.9) | 25 (92.6) | 22 | 34.2 (13.5) | 20 (90.9) |
Figure 2. Estimated marginal means and standard errors (±1 SE) for depression (CES-D) symptoms.
Table 3. Contrast estimates and significance tests for contrasts between conditions at post intervention and 6 month follow up.
| Pre intervention to post intervention | ||||
| Control | Tracking only | Web only | ||
| Web with tracking | Estimate | −11.32 | −7.33 | 4.68 |
| 95% CI | −18.04–−4.60 | −13.83–−0.83 | −2.03–11.40 | |
| Test value | t(109.2) = −3.34, p = 0.00 | t(109.5) = −2.23, p = 0.03 * | t(109.2) = 1.38, p = 0.17 | |
| Web only | Estimate | −6.63 | −2.64 | |
| 95% CI | −12.74–−0.53 | −8.50–3.22 | ||
| Test value | t(105.8) = −2.16, p = 0.03 * | t(105.7) = −0.89, p = 0.37 | ||
| Tracking only | Estimate | −3.99 | ||
| 95% CI | −9.86–1.88 | |||
| Test value | t(105.4) = −1.35, p = 0.18 | |||
Significant findings are bolded.
*These contrasts are not significant (p<.05) under adjustment (Bonferroni correction) for multiple comparisons.
Table 4. Effect sizes (Hedges' g) and 95% confidence intervals for differences between the intervention and control conditions at each measurement occasion.
| Measurement occasion | ||||
| Post intervention | 6 month follow up | |||
| g | 95% CI | g | 95% CI | |
| Web only vs control | 0.76 | 0.21–1.31 | 1.19 | 0.55–1.83 |
| Web with tracking vs control | 1.04 | 0.40–1.67 | 1.26 | 0.57–1.94 |
| Web only vs Tracking only | 0.38 | 0.14–0.89 | 0.58 | 0.01–1.15 |
| Web with tracking vs control | 0.65 | 0.06–1.24 | 0.60 | 0.02–1.20 |
Analyses were repeated with the two outlying cases included. The findings were consistent with those reported above but resulted in slightly attenuated effect sizes and reduced or quasi significant test results. For example, pre to post intervention change remained significantly different comparing web with tracking to control (t(112.6) = −2.09, p = .039) and nearly so for web only condition compared to the control condition (t(109.0) = −1.98, p = .051). At 6 months, comparable outcomes were (t(107.7) = −1.72, p = .089) and (t(107.7) = −2.83, p = 0.006) respectively.
Clinical caseness
Table 2 shows numbers and percentages of participants meeting clinical caseness criteria in each condition at each measurement occasion. Four participants were not classified as clinical cases pre intervention. Of those for whom post intervention data were available, 92.6% of those in the control condition continued to meet clinical caseness, compared to 70.4% in the web only and 66.7% in the web with tracking condition. A univariate logistic regression analysis revealed that the odds of caseness were significantly lower in participants in the web with tracking condition compared to participants in the control condition (odds ratio 0.16, 95% CI: 0.03 to 0.91, p = .039). At 6 month follow up, 43.5% in the web only condition and 50.0% in the web plus tracking condition met clinical caseness compared with 90.9% in the control condition. The odds of meeting caseness criteria were lower in the web with tracking (odds ratio 0.10, 95% CI: 0.02 to 0.56, p = .009) and web only (odds ratio 0.08, 95% CI: 0.01 to 0.41, p = .003) conditions, compared with the control condition. Post intervention, the number needed to be treated (NNT) under the web only intervention was estimated to be 6.03 (95% CI: 2.72 – ∞ – NNH 27.15) and for the web with tracking intervention 4.43 (95% CI: 2.22–265.75).
Repeating these analyses under the conservative assumption that all participants who discontinued the trial (i.e. failed to complete a post intervention or follow-up questionnaire) retained their last assessed caseness status attenuated effects post intervention. However, 6 month follow-up effects retained, or only narrowly escaped, significance, as the odds of achieving caseness status were lower in participants in the web only (odds ratio 0.17, 95% CI: 0.04 to 0.67, p = .010) and web with tracking conditions (odds ratio 0.28, 95% CI: 0.07 to 11.1, p = .072), compared to the control condition. This yields NNTs of 6.09 (95% CI: 3.07 – ∞ – NNH 90.15) and 3.63 (95% CI: 2.23–12.29) [33] respectively.
Dropout and adherence
Dropout
Participants who received the web with tracking intervention were less likely to complete a survey at post intervention (odds ratio 0.13, 95% CI: 0.03 to 0.66, p = .013), compared with those in the control condition. Neither trial condition nor symptom severity predicted dropout at 6 month follow up.
Adherence to the intervention
No significant differences were found in average number of BluePages visits (t(81) = 0.388, p = .70) or average visit duration (t(81) = 0.728, p = .47) between participants in the web only and web with tracking conditions, with average number of visits at 2.2 (mean duration 7.4 minutes), and 1.0 (mean duration 3.8 minutes) respectively. Similarly, there was no significant difference in the number of MoodGYM modules completed for the web only and web with tracking conditions (Mann-Whitney U = 696.0, p = .13). Participants in the web only condition completed an average of 1.5 (SD = 1.89) modules while participants in the web with tracking condition completed an average of 2.0 (SD = 1.88). Approximately one quarter of participants in the web only (15.8%) and web with tracking (17.8%) conditions completed all five modules of the MoodGYM program. 31.6% of participants in the web only and 37.7% of participants in the web with tracking conditions completed 3 or more MoodGYM modules. Half of participants in the web only condition (50.0%) and approximately one third of participants in the web with tracking condition (31.1%) did not complete any modules of the program.
Discussion
Summary findings
Web-based CBT, whether delivered with or without tracking, was found to be effective in reducing symptoms of depression both post intervention and at 6 months within a national helpline service. Tracking alone did not differ significantly from the control condition at post intervention or 6 months. At 6 month follow-up, numbers of participants meeting the criteria for clinical caseness on the CES-D were halved in those who received the web intervention compared to those in the control intervention. The effect sizes associated with the web interventions were large, with effects at post intervention and at 6 months equal to those reported for face to face clinician delivered CBT programs for depression [36] and online CBT programs delivered by professionals [37]. The effect sizes exceeded those previously reported for the MoodGYM and BluePages programs [15]. Effects were also larger than any previous reported effect sizes across 11 RCTs comparing Internet interventions to waitlist, treatment as usual or placebo control conditions for depression [6], [15], [17], [38], [39], [40], [41], [42], [43], [44], [45]. This suggests that call centres may be a particularly appropriate setting in which to place evidence-based web programs. The positive results may reflect several factors. Helpline users in particular may prefer to treat themselves, to manage their own health, and to retain a greater sense of control over their treatment. Also, the high baseline depression symptom levels observed in this sample may have enabled greater change in symptoms from pre to post-intervention.
In the context of web delivered programs, weekly telephone support provided by a lay telephone counsellor did not confer any additional advantage in terms of symptom reduction or adherence. Telephone tracking alone was not effective. These findings contribute to the current debate in the e-health literature as to whether guided e-health interventions are more effective or improve adherence [6]. With respect to the latter, we found no evidence that tracking increased program adherence. In fact, somewhat paradoxically, telephone tracking was associated with decreased participant retention in the trial from baseline to post intervention for the web with tracking condition. It is possible that weekly contact from the telephone counsellor provided the opportunity for participants in the more demanding web condition to “opt out” of the trial, resulting in higher dropout at the time of the post intervention questionnaire. Telephone contact when not associated with requests to engage with web material (tracking only condition) did not result in increased dropout. It may be that weekly telephone tracking in association with a web intervention was construed as “policing”. There are a number of possible explanations for our findings compared to other online research, reporting better outcomes and adherence for guided interventions for social phobia [46]. Guidance in a study by Titov and colleagues [46] was provided by clinicians who, in contrast to the volunteers in the current study, may have provided clinical input and support. Further, there may be differences in the effects of tracking for depression and social phobia. The content of the tracking call in the current study may also partially account for the results. Unlike other studies, in which telephone support is delivered by a therapist who provides tailored feedback and encouragement, the content of the tracking call in the current study was standardised and telephone counsellors were discouraged from providing any form of personalised counselling during these calls. Finally, the differences may be due, at least in part, to differences in the type of service user. As mentioned previously, the helpline users may prefer greater autonomy in managing their own health.
Limitations
Intervention completion rates were lower in our study relative to some other trials of web-based treatments for depression [47] but not of other telephone-based services [48]. The reasons for this are unclear. Telephone callers to helplines may experience more stressful events that preclude trial completion. The current trial was a true effectiveness trial employing a volunteer workforce for recruitment and tracking, and hence would be expected to be associated with recruitment and adherence issues relative to the more controlled environment of an efficacy study [49].
Despite the strong effect sizes associated with the intervention, symptom severity remained quite high at post intervention. However, this accords with data on the effectiveness of antidepressants for depression, where overall only about 50% of patients randomised to active treatment were considered improved using intention to treat analyses at post test [50]. Similar rates are reported following face to face CBT [51]. Moreover, the intervention was short, delivered by non-health professionals, and may have constituted the only service received.
Greater dropout in the web with tracking condition may have inflated the effects observed in this condition. It is noteworthy, however, that dropout was not greater in the web only condition, so that the finding of differential dropout from the web with tracking condition does not undermine the primary finding that the web programs were more effective than either tracking alone or the control condition. Two outliers were identified and excluded from the main analysis. Secondary analyses with outliers included confirmed the direction of findings, although we acknowledge that effect sizes were attenuated. A further limitation of the current study was that depression caseness was estimated using a cutoff on the CES-D. Telephone assessment by a health professional using a diagnostic tool such as the Mini-International Neuropsychiatric Interview [52] or the Composite International Diagnostic Interview [53] would have been a better method of determining cases of depression. However, at the start of the trial we were not convinced that participants who normally retain an anonymous, and short but frequent relationship with the helpline service would be willing to undergo extensive psychological testing at baseline. It was of interest, however, that in the context of the current trial, callers were willing to forgo anonymity to receive the intervention.
Future directions
As far as we can ascertain, the present study is the first to demonstrate that web-based CBT can be effective in the context of a generic, national helpline. The effect sizes were well within the range of those obtained in face to face efficacy trials of CBT delivered by clinicians. In addition, the study demonstrated that a generic helpline could deliver a brief effective intervention within its current service model, and that users of the service were willing to give up their anonymity to participate in the program. The trial demonstrates the potential for individuals in remote or rural locations, those unable to leave home (because of carer responsibilities or mental health symptom severity), and those not wishing to seek traditional medical contact to receive an effective intervention through the telephone and the Internet. At the same time, the trial demonstrates that volunteer counsellors trained to provide “one off” telephone counselling were able to offer a new form of service within their organisation.
From a policy perspective, the volunteer sector was able to provide evidence-based care to individuals with anxiety or depression. Recently, governments in both the United Kingdom and the United States of America have recognised the importance of delivering CBT through general practice by training CBT technicians [54], or through community channels [55]. The current trial offers support for an additional model. Given that it harnesses an existing workforce, this model may well provide a highly cost effective alternative to technician delivered programs in general practice.
The implications for research and service are clear. First, the trial requires replication through other national helplines. Secondly, the replication trial should incorporate either telephone or Internet based diagnosis. In addition, the role of tracking needs to be explored further including the potential role of email contact. There is also a need to find methods for engaging those who dropout before commencing or during the intervention. Critically, given the large number of callers contacting telecounselling services there is a need to ensure that counsellors are prepared to offer the service.
Supporting Information
Trial Protocol.
(RTF)
CONSORT Checklist.
(DOC)
Acknowledgments
Nicole Burgess coordinated and conducted data collection for the trial. Dawn O'Neil was involved in obtaining funding for the trial and coordinating Lifeline Australia's collaboration with the ANU. Assoc Prof Richard O'Kearney was a member of LF's PhD supervisory panel. Trevor Carlyon was also involved in coordinating Lifeline staff and volunteer involvement in the trial and supported Nicole in her role.
Footnotes
Competing Interests: HC and KG are authors of the web based treatment programs BluePages (bluepages.anu.edu.au) and MoodGYM (moodgym.anu.edu.au). LF has received a postgraduate scholarship from the Australian Research Council. KG has received funding from the National Health and Medical Research Council and receives support from numerous sources (list of funders upon request, for conference support) to deliver conference presentations on the MoodGYM and BluePages programs. HC has received funding from industry partner Lifeline for consultancy following completion of the research involving the submitted work and receives support (list of funders upon request, for conference support) to deliver presentations on the MoodGYM and BluePages programs. HC and KG receive royalties from editing a book containing information about the MoodGYM and BluePages programs. There are no patents, products in development or marketed products to declare. This does not alter the authors' adherence to all the PLoS ONE policies on sharing data and materials.
Funding: Funding for the trial was provided by an Australian Research Council Linkage Project Grant (LP0667970) (http://www.arc.gov.au/). LF is supported by an Australian Postgraduate Award Industry scholarship. KG is supported by a National Health and Medical Research Council Fellowship (No. 525413) and HC is supported by a National Health and Medical Research Council Fellowship (No. 525411). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.The Samaritans. The Samaritans: Facts and figures. 2010. The Samaritans.: http://www.samaritans.org/about_samaritans/facts_and_figures.aspx (Accessed October 14, 2010)
- 2.Leach LS, Christensen H. A systematic review of telephone-based interventions for mental disorders. J Telemed Telecare. 2006;12:122–129. doi: 10.1258/135763306776738558. [DOI] [PubMed] [Google Scholar]
- 3.Perkins D, Fanaian M. Who calls Lifeline: Baseline study of callers and their needs (Final Report). 2004. University of New South Wales: CEPHRIS: Centre for Equity and Primary Health Care Research in the Illawarra and Shoalhaven.
- 4.Christensen H, Hocking BM, Smith D. Web and telecounselling in Australia. Med J Aust. 2004;180:604–605. doi: 10.5694/j.1326-5377.2004.tb06118.x. [DOI] [PubMed] [Google Scholar]
- 5.Urbis Keys Young. National Review of Tele Counselling and Web Counsellling Services: Final Report. Canberra: Australian Government Department of Health and Ageing; 2003. [Google Scholar]
- 6.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, et al. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 7.van Straten A, Cuijpers P, Smits N. Effectiveness of a web-based self-help intervention for symptoms of depression, anxiety, and stress: randomized controlled trial. J Med Internet Res. 2008;10:e7. doi: 10.2196/jmir.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: A meta-analysis. Cognitive Behaviour Therapy. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- 9.Barak A, Hen L, Boniel-Nissim M, Shapira N. A comprehensive review and a meta-analysis of the effectiveness of Internet-based psychotherapeutic interventions. Journal of Technology in Human Services. 2008;26:109–160. [Google Scholar]
- 10.Mohr DC, Hart SL, Julian L, Catledge C, Honos-Webb L, et al. Telephone-administered psychotherapy for depression Archives of General. Psychiatry. 2005;65:1007–1014. doi: 10.1001/archpsyc.62.9.1007. [DOI] [PubMed] [Google Scholar]
- 11.Griffiths KM, Farrer L, Christensen H. The efficacy of internet interventions for depression and anxiety disorders: a review of randomised controlled trials. Med J Aust. 2010;192:S4–11. doi: 10.5694/j.1326-5377.2010.tb03685.x. [DOI] [PubMed] [Google Scholar]
- 12.Calear AL, Christensen H, Mackinnon A, Griffiths KM, O'Kearney R. The YouthMood Project: A cluster randomized controlled trial of an online cognitive behavioral program with adolescents. Journal of Consulting and Clinical Psychology. 2009;77:1021–1032. doi: 10.1037/a0017391. [DOI] [PubMed] [Google Scholar]
- 13.Kessler D, Lewis G, Kaur S, Wiles N, King M, et al. Therapist-delivered Internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet. 2009;374:628–634. doi: 10.1016/S0140-6736(09)61257-5. [DOI] [PubMed] [Google Scholar]
- 14.Hickie IB, Davenport TA, Luscombe GM, Moore M, Griffiths KM, et al. Practitioner-supported delivery of internet-based cognitive behaviour therapy: evaluation of the feasibility of conducting a cluster randomised trial. Med J Aust. 2010;192:S31–35. doi: 10.5694/j.1326-5377.2010.tb03690.x. [DOI] [PubMed] [Google Scholar]
- 15.Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. British Medical Journal. 2004;328:265–269. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clarke G, Eubanks D, Reid E, Kelleher C, O'Connor E, et al. Overcoming Depression on the Internet (ODIN) (2): a randomized trial of a self-help depression skills program with reminders. J Med Internet Res. 2005;7:e16. doi: 10.2196/jmir.7.2.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Warmerdam L, van Straten A, Twisk J, Riper H, Cuijpers P. Internet-based treatment for adults with depressive symptoms: randomized controlled trial. J Med Internet Res. 2008;10:e44. doi: 10.2196/jmir.1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Titov N, Andrews G, Davies M, McIntyre K, Robinson E, et al. Internet treatment for depression: a randomized controlled trial comparing clinician vs. technician assistance. PLoS One. 2010;5:e10939. doi: 10.1371/journal.pone.0010939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler R, Andrews G, Colpe L, Hiripi E, Mroczek D, et al. Short screening scales to monitor population prevalence and trends in nonspecific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 21.Knight RG, Williams S, McGee R, Olaman S. Psychometric properties of the Center for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behavior Research and Therapy. 1997;35:373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- 22.Ross CE, Mirowsky J. Components of depressed mood in married men and women: The Center for Epidemiologic Studies Depression Scale. American Journal of Epidemiology. 1984;119:997–1004. doi: 10.1093/oxfordjournals.aje.a113819. [DOI] [PubMed] [Google Scholar]
- 23.Roberts RE. Reliability of the CES-D Scale in different ethnic contexts. Psychiatry Research. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 24.Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: It's use in a community sample. American Journal of Psychiatry. 1983;140:41–46. doi: 10.1176/ajp.140.1.41. [DOI] [PubMed] [Google Scholar]
- 25.Husaini BA, Neff JA, Harrington JB, Hughes MD, Stone RH. Depression in rural communities: Validating the CES-D scale. Journal of Community Psychology. 1980;8:20–27. [Google Scholar]
- 26.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams JWJ, Pignone M, Ramirez G, Perez Stellato C. Identifying depression in primary care: a literature synthesis of case-finding instruments. Gen Hosp Psychiatry. 2002;24:225–237. doi: 10.1016/s0163-8343(02)00195-0. [DOI] [PubMed] [Google Scholar]
- 28.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 29.SPSS Inc. PASW Release 18.0. 2009. SPSS Inc.
- 30.Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. American Journal of Psychiatry. 2009;166:639–641. doi: 10.1176/appi.ajp.2009.09040458. [DOI] [PubMed] [Google Scholar]
- 31.Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. Orlando: Academic Press; 1985. [Google Scholar]
- 32.Kelley K. Constructing confidence intervals for standardized effect sizes: Theory, application, and implementation. Journal of Statistical Software. 2007;20:1–24. [Google Scholar]
- 33.Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317:1309–1312. doi: 10.1136/bmj.317.7168.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bender R. Calculating confidence intervals for the number needed to treat. Controlled Clinical Trials. 2001;21:102–110. doi: 10.1016/s0197-2456(00)00134-3. [DOI] [PubMed] [Google Scholar]
- 35.Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer-Verlag; 2000. [Google Scholar]
- 36.Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 37.Andrews G, Cuijpers P, Craske M, McEvoy P, Titov N. Computer Therapy for the Anxiety and Depressive Disorders Is Effective, Acceptable and Practical Health Care: A Meta-Analysis. PLoS ONE. 2010;5:e13196. doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spek V, Nyklicek I, Smits N, Cuijpers P, Riper H, et al. Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: a randomized controlled clinical trial. Psychol Med. 2007;37:1797–1806. doi: 10.1017/S0033291707000542. [DOI] [PubMed] [Google Scholar]
- 39.Perini S, Titov N, Andrews G. Clinician-assisted Internet-based treatment is effective for depression: randomized controlled trial. Aust N Z J Psychiatry. 2009;43:571–578. doi: 10.1080/00048670902873722. [DOI] [PubMed] [Google Scholar]
- 40.Meyer B, Berger T, Caspar F, Beevers CG, Andersson G, et al. Effectiveness of a novel integrative online treatment for depression (Deprexis): randomized controlled trial. J Med Internet Res. 2009;11:e15. doi: 10.2196/jmir.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Calear AL, Christensen H, Mackinnon A, Griffiths KM, O'Kearney R. The YouthMood Project: a cluster randomized controlled trial of an online cognitive behavioral program with adolescents. J Consult Clin Psychol. 2009;77:1021–1032. doi: 10.1037/a0017391. [DOI] [PubMed] [Google Scholar]
- 42.Ruwaard J, Schrieken B, Schrijver M, Broeksteeg J, Dekker J, et al. Standardized web-based cognitive behavioural therapy of mild to moderate depression: a randomized controlled trial with a long-term follow-up. Cogn Behav Ther. 2009;38:206–221. doi: 10.1080/16506070802408086. [DOI] [PubMed] [Google Scholar]
- 43.Clarke G, Kelleher C, Hornbrook M, Debar L, Dickerson J, et al. Randomized effectiveness trial of an Internet, pure self-help, cognitive behavioral intervention for depressive symptoms in young adults. Cogn Behav Ther. 2009;38:222–234. doi: 10.1080/16506070802675353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Graaf LE, Gerhards SA, Arntz A, Riper H, Metsemakers JF, et al. Clinical effectiveness of online computerised cognitive-behavioural therapy without support for depression in primary care: randomised trial. Br J Psychiatry. 2009;195:73–80. doi: 10.1192/bjp.bp.108.054429. [DOI] [PubMed] [Google Scholar]
- 45.Sethi S, Campbell AJ, Ellis LA. The use of computerized self-help packages to treat adolescent depression and anxiety. Journal of Technology in Human Services. 2010;28:144–160. [Google Scholar]
- 46.Titov N, Andrews G, Choi I, Schwencke G, Mahoney A. Shyness 3: randomized controlled trial of guided versus unguided Internet-based CBT for social phobia. Aust N Z J Psychiatry. 2008;42:1030–1040. doi: 10.1080/00048670802512107. [DOI] [PubMed] [Google Scholar]
- 47.Christensen H, Griffiths KM, Farrer L. Adherence in Internet interventions for anxiety and depression: Systematic review. Journal of Medical Internet Research. 2009;11:e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rhee WK, Merbaum M, Strube MJ, Self SM. Efficacy of brief telephone psychotherapy with callers to a suicide hotline. Suicide Life Threat Behav. 2005;35:317–328. doi: 10.1521/suli.2005.35.3.317. [DOI] [PubMed] [Google Scholar]
- 49.Flay BR. Efficacy and effectiveness trials (and other phases of research) in the development of health promotion programs. Prev Med. 1986;15:451–474. doi: 10.1016/0091-7435(86)90024-1. [DOI] [PubMed] [Google Scholar]
- 50.Bollini P, Pampallona S, Tibaldi G, Kupelnick B, Munizza C. Effectiveness of antidepressants. Meta-analysis of dose-effect relationships in randomised clinical trials. Br J Psychiatry. 1999;174:297–303. doi: 10.1192/bjp.174.4.297. [DOI] [PubMed] [Google Scholar]
- 51.DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62:409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- 52.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33;quiz 34–57. [PubMed] [Google Scholar]
- 53.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 54.Seward J, Clark M. Establishing the Improved Access to Psychological Therapies Programme: lessons from large-scale change in England. In: Bennett-Levy J, Richards DA, Farrand P, Christensen H, Griffiths KM, et al., editors. Oxford Guide to Low Intensity CBT Interventions. Oxford: Oxford University Press; 2010. [Google Scholar]
- 55.McHugh RK, Barlow DH. The dissemination and implementation of evidence-based psychological treatments. A review of current efforts. Am Psychol. 2010;65:73–84. doi: 10.1037/a0018121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol.
(RTF)
CONSORT Checklist.
(DOC)