Abstract
Chronic stress produces sustained elevation of corticosteroid levels, which is why it is considered one of the most potent negative regulators of adult hippocampal neurogenesis (AHN). Several mood disorders are accompanied by elevated glucocorticoid levels and have been linked to alterations in AHN, such as major depression (MD). Nevertheless, the mechanism by which acute stress affects the maturation of neural precursors in the dentate gyrus is poorly understood. We analyzed the survival and differentiation of 1 to 8 week-old cells in the dentate gyrus of female C57/BL6 mice following exposure to an acute stressor (the Porsolt or forced swimming test). Furthermore, we evaluated the effects of the glucocorticoid receptor (GR) antagonist mifepristone on the cell death induced by the Porsolt test. Forced swimming induced selective apoptotic cell death in 1 week-old cells, an effect that was abolished by pretreatment with mifepristone. Independent of its antagonism of GR, mifepristone also induced an increase in the percentage of 1 week-old cells that were AMPA+. We propose that the induction of AMPA receptor expression in immature cells may mediate the neuroprotective effects of mifepristone, in line with the proposed antidepressant effects of AMPA receptor potentiators.
Introduction
Adult neurogenesis takes place in the brain of numerous vertebrates [1], including humans [2]. Under normal physiological conditions, this production of new neurons occurs in two brain regions: the subventricular zone of the lateral ventricles, and the subgranular zone (SGZ) of the dentate gyrus (DG) in the hippocampus. Growing evidence indicates that adult hippocampal neurogenesis (AHN) is crucial for learning and memory [3] [4]. Furthermore, alterations in AHN have been implicated in several mood disorders [5], and many antidepressants require AHN to exert their behavioral effects [6]. Numerous external stimuli have been shown to modulate AHN, including physical activity [7], environmental enrichment [8] and stress [9].
At the molecular level, the rate of AHN is regulated by a large variety of signaling molecules, including: growth factors such as brain-derived neurotrophic factor (BDNF) [10], insulin-like growth factor I (IGF-I) [11] [12] [13] and vascular endothelial growth factor (VEGF) [14]; neurotransmitters such as glutamate [15] [16]; and pro-inflammatory cytokines [17]. Among the strongest modulators of the rate of AHN are the adrenal corticosteroids. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, resulting in an increase in the levels of circulating glucocorticoids (GCs). In general terms, high GC levels are considered negative regulators of AHN [18] [19] [10], although the complex regulation of AHN by GCs remains poorly understood, with many conflicting reports in the literature [20] [21]. The physiological response to acute stress and the accompanying increase in GC levels appear to be adaptative in nature, and these events are critical for hippocampal long-term potentiation (LTP) [22] and memory consolidation [23]. However, long-term exposure to elevated GC levels triggers a series of alterations that may provoke neurodegeneration in sensitive brain areas [24] [25]. In conjunction with genetic risk factors, the inability to return to the basal state following long- term exposure to high GC levels, known as allostatic load [26], is considered by some authors to be a critical factor in the development of neurodegenerative diseases such as Alzheimeŕs disease (AD) [27] [28] [29], and of mood disorders like MD [30] [31]. The hippocampus is highly sensitive to the effects of both GC and stress, and it expresses high levels of corticosteroid receptors of both high (mineralocorticoid receptors, MR) and low (glucocorticoid receptors, GR) affinity [32] [33]. Chronic exposure to stress induces permanent synaptic and dendritic alterations [34] [35], increases hippocampal glutamate levels [36] [37] and decreases AHN [9]. Thus, understanding the molecular mechanisms that regulate responses to stress, whether chronic or acute (as studied here) is particularly important to identify therapeutic targets that modulate these responses and that avoid the damage caused by prolonged exposure to stress.
In recent years, GR antagonists have been proposed for the treatment of diverse mood disorders. One such compound with a high degree of clinic relevance is mifepristone (RU-486), which has been shown to normalize some of the hippocampal alterations provoked by chronic stress [38] [39]. However, the mode of action of this drug remains a matter of much debate and indeed, it has been proposed that its neuroprotective effects may even be independent of its action as a GR antagonist [40].
In the present study, we evaluated the effects of an acute stress, the forced swim or Porsolt test, on the survival of hippocampal newborn neurons of different ages in order to identify populations particularly sensitive to acute stress. In addition, we evaluated the effects of the GR antagonist mifepristone on the alterations in hippocampal neurons induced by stress. Given the growing interest in potentiators of AMPA-mediated glutamatergic signaling in the treatment of depression (also known as ampakines) [41] [42] [43], we investigated the relationship between GR blockage and AMPA receptor expression in different populations of hippocampal newborn neurons.
Materials and Methods
Animals
Ninety five female C57/BL6J mice (8 weeks of age, Harlan Laboratories) were housed at 22±1°C on a 12/12 h light/dark cycle, with ad libitum access to food and water. Mice were kept under standard laboratory conditions in accordance with European Community Guidelines (directive 86/609/EEC). Moreover, all the animals were handled in strict accordance with good animal practice as defined by the national animal welfare bodies (at the Cajal Institute and CSIC, the Spanish Higher Research Council), and all the animal work was approved by the appropriate committees (Bioethics Committee of the Cajal Institute and CSIC, approval certificate number BFU2007-60195, issued June 7, 2007).
Experimental design and injection of thymidine analogues
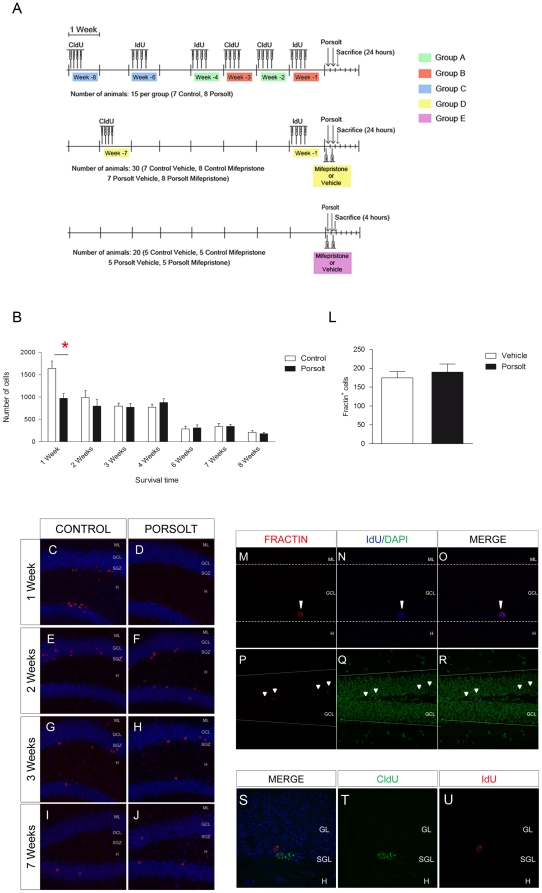
One week after their arrival, the mice were distributed into five groups (A–E) as summarized in Figure 1 . Newborn hippocampal neurons of 1, 2, 3, 4, 6, 7 and 8 weeks of age were labeled with different thymidine analogues (see Figure 1 ). The animals in groups A–C were used to evaluate the effect of the Porsolt test on survival, differentiation and marker expression in hippocampal cells of 1 to 8 weeks of age. Table 1 summarizes the injection regimes used for 5-Chloro-2′-deoxy-Uridine (CldU, 57.65 mg/Kg i.p., Sigma-Aldrich, St. Louis, US) and 5-Iodo-2′-deoxy-Uridine (IdU, 42.75 mg/Kg i.p., Sigma-Aldrich). These doses were based on equimolar doses of 50 mg/Kg BrdU [8]. To avoid any spurious effects of the estrous cycle, each animal received one CldU or IdU injection over 4 successive days, as described previously [44]. After the periods of time indicated, half of the animals from each group were subjected to the forced swim test [45], and they were then sacrificed 4 or 24 hours later and compared with the control animals. The effect of the GR antagonist mifepristone was assessed on cell populations of different ages in both control animals and those subjected to the forced swim test (Group D). Hence, animals in group E were used to determine the effect of mifepristone on the expression of different genes in both control animals and those subjected to the forced swim test.
Figure 1. Experimental design and the effects of the Porsolt test on cell survival in different age cells.
A Timing of thymidine analogue injection, CldU and IdU. 1 to 8 weeks old adult newborn cells were labeled in the different experimental groups. The effect of the glucocorticoid receptor anatgonist mifepristone was evaluated in control animals and those subjected to the Porsolt test. B The Porsolt test significantly reduced the survival of 1 week-old IdU+ cells (p<0.001), but not those in any other age group. Data are presented as total number of IdU+/CldU+ cells ± standard error of the mean (SE). C–J Immunohistochemistry against IdU or CldU (red) in cells counterstained with DAPI (blue) under different experimental conditions and from different age groups. L Total number of apoptotic fractin+ cells. Forced swimming did not modify the total number of fractin+ cells (p = 0.628). M–R Representative images of fractin staining. M–O A double labeled IdU+ (blue)/Fractin+ (red) cells. P–R Low magnification fractin (red) staining of cells counterstained with DAPI (green). S–U Representative images of double immunohistochemistry for CldU (green) and IdU (red) showing no co-localization in 2 and 4 week-old cells. ML: Molecular layer; GCL: Granule cell layer; SGZ: Subgranular zone; H: Hilus. Scale bar = 100 µm.
Table 1. Injection dates and doses of IdU and CldU (mg/Kg) administered to animals in each experimental group.
| CldU | IdU | ||||
| Date (Days) | Dosage (mg/Kg) | Date (Days) | Dosage (mg/Kg) | ||
| GROUP A | −14, −13, −12, −11 | 57.65 | −28, −27, −26, −25 | 42.75 | |
| GROUP B | −21, −20, −19, −18 | 57.65 | −7, −6, −5, −4 | 42.75 | |
| GROUP C | −56, −55, −54, −53 | 57.65 | −42, −41, −40, −39 | 42.75 | |
| GROUP D | −49, −48, −47, −36 | 57.65 | −7, −6, −5, −4 | 42.75 | |
| GROUP E | - | - | - | - | |
Group E animals received no injections and they were used to determine the hippocampal mRNA expression. Note that the doses were based on equimolar doses of 50 mg/kg BrdU. To avoid ethe ffects of the estrous cycle, animals received one injection of CldU or IdU on 4 successive days.
Porsolt test and Mifepristone administration
Animals were placed in cylindrical containers filled with water (12 cm diameter and 29 cm tall, 23°C) for 6 minutes each day on two consecutive days. The behavior of the animals was scored as described previously [46]. The animals in groups D and E received a single injection of the vehicle alone (sesame oil, Sigma-Aldrich) or of mifepristone (i.p., 20 mg/Kg, Sigma-Aldrich) diluted in the vehicle 30 minutes before each swim-test session. The control animals were moved to the behavioral testing rooms along with swim test animals, where they remained in their cages for the duration of the tests.
Sacrifice
Mice were completely anaesthetized with pentobarbital 24 (groups A, B, C and D) or 4 hours (group E) after the last swim-test session and they were then perfused with saline followed by 4% paraformaldehyde in phosphate buffer (PB). The brains of the mice were removed and post-fixed overnight in the same fixative (groups A, B, C and D), while the animals in group E were perfused with saline alone. The hippocampus from each of the animals in group E was dissected out on ice and frozen at −80°C.
Histology
Coronal sections (50 µm thick) from one hemisphere were obtained on a Leica VT1000S vibratome and series of sections were generated comprised of every 8th section. Double or triple immunohistochemistry was performed as described previously [47], incubating the sections with the following primary antibodies for 24 to 48 hours: rat anti-CldU (1:400, Accurate Chemicals, New York, USA); mouse anti-IdU (1:500, BD Biosciences, New Jersey, USA); rabbit anti-phospho-histone 3 (pH3,1:500, Upstate-Cell Signaling, Boston, MA, USA); goat anti-doublecortin (DCX, 1:500, Santa Cruz, CA, USA); rabbit anti-fractin (1:500, BD Biosciences); rabbit anti-AMPA receptor (AMPAR, 1:2000, Abcam, Cambridge, UK), rabbit anti-GR H-300 (1:1000, Santa Cruz); and goat anti-MR (1:400, Abcam). The binding of these antibodies was then detected over 24 at hours at 4°C with the following donkey Alexa-conjugated secondary antibodies as appropriate (1:1000, Molecular Probes, Eugene, OR, US): Anti-rabbit alexa 594-conjugated or anti-rabbit Alexa 555-conjugated (pH3, fractin and GR detection); or anti-rat alexa 488-conjugated (CldU detection). To visualize DCX and MR in triple immunohistochemistry experiments, antibody binding was detected with a biotin-conjugated horse anti-goat antibody (1:1000 Vector Laboratories Burlingame, CA, USA), followed by incubation with a Alexa 633-conjugated Strepatividin. All the sections were counterstained for 10 minutes with DAPI (1:1000, Calbiochem-EMD Darmstadt, Germany).
Cell Counting
The total number of cells labeled for pH3, fractin, CldU and IdU were counted under an optical fluorescence microscope (Leica DMI 6000 B, oil immersion 40x objective), using the optical-dissector method. Briefly, series composed of every 8th section were used to analyze each of these markers, the cells labeled for each marker in every section were counted, and the total number of cells counted was then multiplied by 8 in order to obtain the total number of cells [48].
The total number of immature (DCX+) and mature granule neurons was calculated using the physical-dissector method adapted for confocal microscopy (Leica TCS SP5) [47]. DG volume was stereologically estimated by applying the Cavalieri method to one series in conjunction with Nissl staining. To investigate their phenotypes, 50 IdU or CldU positive cells per animal were examined (1, 2, 3, 4, 6 and 7 weeks old cells) and co-localization with either fractin, GR, MR, DCX or AMPAR was analyzed in confocal images using the Leica Application Suite Colocalization tool (Leica TCS SP5, oil immersion 63x objective, Zoom factor: 3). Due to the small number of cells in 8 week-old cells, the percentage co-localization was not calculated at this age. In the case of 6 and 7 week-old cells, two series have been analyzed for each marker. The distance between the cell nuclei and the Hilus layer was measured in confocal images immunolabeled for both IdU (or CldU) and AMPA, and counterstained with DAPI. A line was traced through the subgranular layer at the point where hilus begins, and the distance between this line and the nucleus was measured. 100 cells per animal were analyzed in this case.
Quantitative real-time Polymerase chain reaction (qPCR)
Total RNA was isolated from the Hippocampal tissues in one hemisphere of each animal from Group E using the Illustra RNAspin Mini kit (GE Healthcare, Uppsala, Sweden) and 1 µg was reverse transcribed (RT) using the High capacity cDNA Reverse Transcription kit (Applied Biosystems, Carlsbad, California, US). Subsequently, qPCR was performed on a 7500 Sequence detection system thermal cycler (Applied Biosystems), analyzing the data with the aid of the 7500 System SDS Software (Applied Biosystems) using the Pfaffl method [49]. TaqMan gene expression assays (Applied Biosystems) were used to study the expression of Interleukin-6 (IL-6, Mm99999064_m1), Tumor Necrosis Factor (TNF, Mm00443259_g1), vesicular Glutamate Transporter 1 (Mm00812886_m1), Glutamic Acid Decarboxylase 65 (Mm00484623_m1), Brain Derived Neurotrophic factor (BDNF, Mm00432069_m1), Insulin-like Growth factor 1 (IGF-I, Mm00439560_m1), Glucocorticoid receptor (GR, Mm00433832_m1) and the Mineralocorticoid receptor (MR, Mm01241597_m1). Mouse GAPDH (Primer limited, Part Number 4352339E) was used as an endogenous control.
Statistical Analysis
Data from experiments A, B and C were analyzed by two-way ANOVA, with “age” and the “Porsolt test” as independent variables. When significant interactions were detected, we conducted a one-way ANOVA followed by a post hoc Tukey test to identify categories significantly affected by “age” or “Porsolt test”. For experiments D and E, the data were analyzed by two-way ANOVA to compare the four experimental groups (Control vehicle; Control mifepristone; Porsolt vehicle and Porsolt mifepristone). SPSS 17.0.1 software (SPSS, 1989; Apache Software Foundation) was used for all the statistical analyses.
Results
Exposure to the Porsolt swim-test induces the selective death of 1 week-old cells
When the number of newborn cells was analyzed, a significant effect of “age” (F6,126 = 22.650, p<0.001) but not of the “Porsolt test” (F1,126 = 2.822, p = 0.096) was evident when a two-Way ANOVA analysis was performed, and there was also a significant interaction with this factor (F6,126 = 2.772, p = 0.015). Indeed, post hoc analysis revealed that exposure to the Porsolt test significantly reduced the number of 1 week-old cells (p = 0.001, Figure 1 B), although there was no significant effect on cell number in 2, 3, 4, 6, 7 or 8 week-old cells (p>0.1 for all). Accordingly, in animals from groups A and B, exposure to the Porsolt test failed to alter the total number of apoptotic fractin+ cells (F1,26 = 0.303, p = 0.587: Figure 1 L). Representative images of the total number of IdU+ or CldU+ cells in the different age groups (Figure 1 C–J) and of fractin staining (Figure 1 M– R) are shown. Dual immunohistochemistry against CldU and IdU, revealed no co-localization in 2 and 4 week-old cells (Figure 1 S– U).
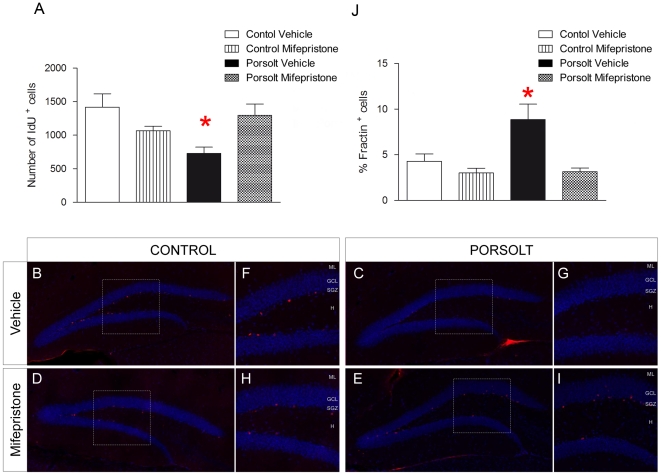
Mifepristone selectively prevents Porsolt test-induced apoptosis in 1 week-old hippocampal neurons
Mifepristone prevented the reduction in the number of 1 week-old cells provoked by the Porsolt test (Mifepristone F1,27 = 0.579, p = 0.454; Porsolt F1,27 = 2.616, p = 0.119; Interaction F3,27 = 10.490, p = 0.003; Figure 2 A), as also evident in the representative images of the number of 1 week-old cells in each experimental group (Figure 2 B– I). The percentage of IdU-labeled cells that also expressed fractin+ at the moment of the sacrifice was also measured. Exposure to the Porsolt test increased the percentage of fractin+ 1 week-old cells, an effect that was attenuated by mifepristone treatment (Mifepristone F1,28 = 11.301, p = 0.002; Porsolt F1,28 = 6.174, p = 0.02; Interaction F3,28 = 6.174, p = 0.020; Figure 2 J). However, neither the Porsolt test nor mifepristone modified the total number of DCX+ cells (Mifepristone F1,28 = 1.236, p = 0.277; Porsolt F1,28 = 0.070, p = 0.793; Interaction F1,28 = 0.197, p = 0.661) (Figure S1 A), pH3+ cells (Mifepristone F1,27 = 0.002, p = 0.967; Porsolt F1,27 = 0.098, p = 0.757; Interaction F1,27 = 0.017, p = 0.899) (Figure S1 B), mature granule cells (Mifepristone F1,29 = 0.003, p = 0.717; Porsolt F1,29 = 0.378, p = 0.544; Interaction F1,29 = 0.468, p = 0.444) (Figure S1 C), or the volume of the DG (Mifepristone F1,27 = 0.003, p = 0.090; Porsolt F1,27 = 0.378, p = 0.337; Interaction F1,27 = 0.468, p = 0.459) (Figure S1 D). Likewise, neither the Porsolt test or mifepristone affected the total number of 7 week-old CldU+ cells (Mifepristone F1,28 = 0.073, p = 0.789; Porsolt F1,28 = 0.052, p = 0.821; Interaction F1,28 = 0.202, p = 0.657) (Figure S1 E), and as expected, acute mifepristone treatment had no effect on the immobility time in the Porsolt test (F1,23 = 0.742, p = 0.398) (Figure S1 F).
Figure 2. Effects of mifepristone and the Porsolt test on the survival of 1 week-old cells.
A Mifepristone prevented the decrease in the number of 1 week-old IdU+ cells induced by exposure to the Porsolt test (interaction p = 0.005). B-I Immunohistochemistry against IdU (red) in cells counterstained with DAPI (blue). Representative images of 1 week-old cells from each of the four experimental groups (B–E), and magnifications (F–I). Mifepristone blocked the decrease in cell survival provoked by the Porsolt test (E, I) but it had no effect on control, unstressed animals (D, H). J Exposure to the Porsolt test increased the percentage of 1 week-old IdU+ cells that were also fractin+ (p = 0.02), an effect that was blocked by mifepristone treatment (interaction p = 0.02). ML: Molecular layer; GCL: Granule cell layer; SGZ: Subgranular zone; H: Hilus. Scale bar = 100 µm.
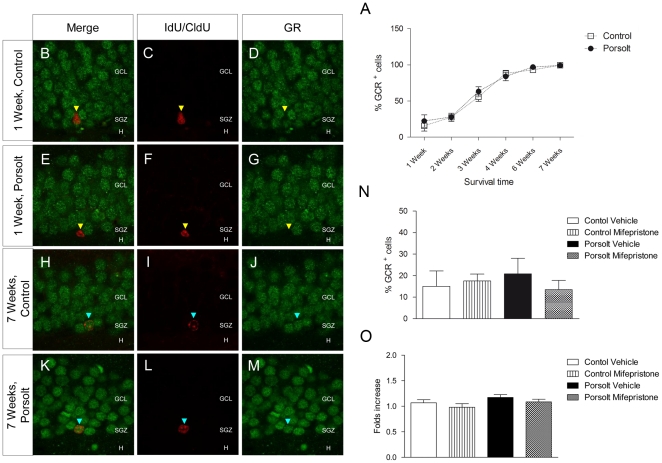
The effects of the Porsolt test and mifepristone administration on GR and MR levels
GR expression was evaluated in immature neurons of different ages by dual immunohistochemistry (Figure 3 B– M). Two-way ANOVA revealed an increase in the percentage of GR+ cells as cell age increased (F5,89 = 93.226, p<0.001), while the Porsolt test had no effect on the proportion of GR+ cells at any of the ages studied (F1,86 = 1.586, p = 0.212; no significant interaction, F5,8 = 0.845, p = 0.522; Figure 3 A). Accordingly, hippocampal GR mRNA expression was unaffected by either the Porsolt test or mifepristone treatment (Mifepristone F1,17 = 2.011, p = 0.178; Porsolt F1,17 = 2.924, p = 0.109; Interaction F1,17 = 0.000, p = 0.997; Figure 3 O). The percentage of 1 week-old GR+ cells also remained unaffected by either the Porsolt test or mifepristone treatment (Mifepristone F1,29 = 0.273, p = 0.606; Porsolt F1,29 = 0.068, p = 0.796; Interaction F1,29 = 0.916, p = 0.347).
Figure 3. Glucocorticoid receptor (GR) expression.
A Percentage of GR+ cells. The percentage of GR+ cells increased with age (p<0.001). Exposure to the Porsolt test did not alter the percentage of GR+ cells in any of the age groups studied (p = 0.212). B–M Representative images of double immunohistochemistry against IdU or CldU (red) and GR (green). Most 1 week-old cells were GR- (yellow triangles), whereas almost all 7 week-old cells were GR+ (purple triangles). N Percentage of 1 week-old IdU+ cells that were also GR+, and neither mifepristone (p = 0.606) nor the Porsolt test (p = 0.796) altered this percentage. O Hippocampal GR mRNA expression. Neither mifepristone (p = 0.178) nor the Porsolt test (p = 0.109) altered GR mRNA expressionin the hippocampus when measured 4 hours after testing. GCL: Granule cell layer; SGZ: Subgranular zone; H: Hilus. Scale bar: 30 µm.
MR expression was also evaluated in cells of different ages and like GR, the percentage of MR+ cells increased with age (F5,82 = 11.532, p<0.001) but was not affected by the Porsolt test at any of the ages studied (F1,82 = 0.383, p = 0.538; Interaction F5,82 = 0.371, p = 0.867. Similarly there were no changes in hippocampal MR mRNA expression in response to either the Porsolt test or mifepristone treatment (Mifepristone F1,19 = 0.516, p = 0.483; Porsolt F1,19 = 0.105, p = 0.749; Interaction F1,19 = 3.447, p = 0.082). Furthermore, the proportion of 1 week-old MR+ cells was not altered by either the Porsolt test or mifepristone treatment (Mifepristone F1,27 = 1.218, p = 0.385; Porsolt F1,27 = 0.345, p = 0.642; Interaction F1,27 = 0.123, p = 0.536). The relative mRNA expression of these and other genes are shown in Table 2 .
Table 2. Relative hippocampal mRNA expression (fold increase) in Group E animals.
| Control | Porsolt | |||
| Vehicle | Mifepristone | Vehicle | Mifepristone | |
| IL-6 | 1.24±0.14 | 1.22±0.27 | 1.23±0.24 | 1.41±0.24 |
| TNF | 0.97±0.08 | 1.15±0.25 | 0.80±0.13 | 1.22±0.32 |
| BDNF | 0.98±0.05 | 0.93±0.08 | 1.05±0.06 | 1.15±0.08 |
| IGF-I | 0.6±0.1 | 0.60±0.03 | 0.69±0.09 | 0.56±0.04 |
| vGLUT1 | 1.09±0.07 | 1.07±0.08 | 1.15±0.1 | 1.02±0.07 |
| GAD65 | 1.08±0.11 | 0.99±0.07 | 0.9±0.04 | 1.06±0.11 |
| GR | 1.06±0.06 | 0.98±0.07 | 1.05±0.12 | 0.98±0.1 |
| MR | 0.87±0.04 | 1.06±0.08 | 0.9±0.1 | 0.82±0.03 |
Neither the Porsolt test nor mifepristone administration significantly altered the mRNA expression of IL-6 (F3,18 = 0.777, p = 0.525), TNF (F3,15 = 1.331, p = 0.31), BDNF (F3,19 = 1.733, p = 0.201), IGF-I (F3,19 = 1.733, p = 0.201), vGLUT1 (F3,18 = 0.759, p = 0.31), GAD65 (F3,18 = 0.848, p = 0.489), GR (F3,18 = 1.654, p = 0.222), nor MR (F3,19 = 2.043, p = 0.148). Mouse GAPDH was used as an endogenous control. The data is presented as the relative increase (Pfaffl method). IL-6: Interleukin 6. TNF: Tumor necrosis factor. BDNF: Brain-derived neurotrophic factor. IGF-I: Insulin-like growth factor. vGLUT1: vesicular glutamate transporter 1. GAD65: Glutamic acid decarboxylase 65. GR: Glucocorticoid receptor. MR: Mineralocorticoid receptor.
The effects of the Porsolt test and mifepristone administration on inflammation, glutamatergic and gabaergic transmission, and on the expression of trophic factors in the hippocampus
The mRNA expression of hippocampal pro-inflammatory cytokines (IL-6 and TNF), and of the presynaptic markers of glutamaergic (vGLUT1) and GABAergic (GAD65) neurotransmission was measured by qPCR in Group E animals. Neither exposure to the Porsolt test nor mifepristone administration modified the expression of IL-6 (Mifepristone F1,18 = 1.156, p = 0.299; Porsolt F1,18 = 0.049, p = 0.828; Interaction F1,18 = 1.302, p = 0.272), TNF (Mifepristone F1,15 = 0.049, p = 0.828; Porsolt F1,15 = 2.818, p = 0.119; Interaction F1,15 = 0.737, p = 0.408), vGLUT1 (Mifepristone F1,18 = 0.585, p = 0.456; Porsolt F1,18 = 1.209, p = 0.289; Interaction F1,18 = 0.738, p = 0.404) or GAD65 mRNA (Mifepristone F1,18 = 1.830, p = 0.196; Porsolt F1,18 = 0.001, p = 0.979; Interaction F1,18 = 0.826, p = 0.378).
The hippocampal mRNA expression of BDNF and IGF-I was also evaluated by qPCR in Group E animals and again, neither the Porsolt test nor mifepristone administration significantly modified BDNF (Mifepristone F1,19 = 0.101, p = 0.755; Porsolt F1,19 = 3.892, p = 0.066; Interaction F1,19 = 1.205, p = 0.289) or of IGF-I mRNA expression (Mifepristone F1,19 = 0.330, p = 0.575; Porsolt F1,19 = 0.677, p = 0.426; Interaction F1,19 = 1.205, p = 0.289).
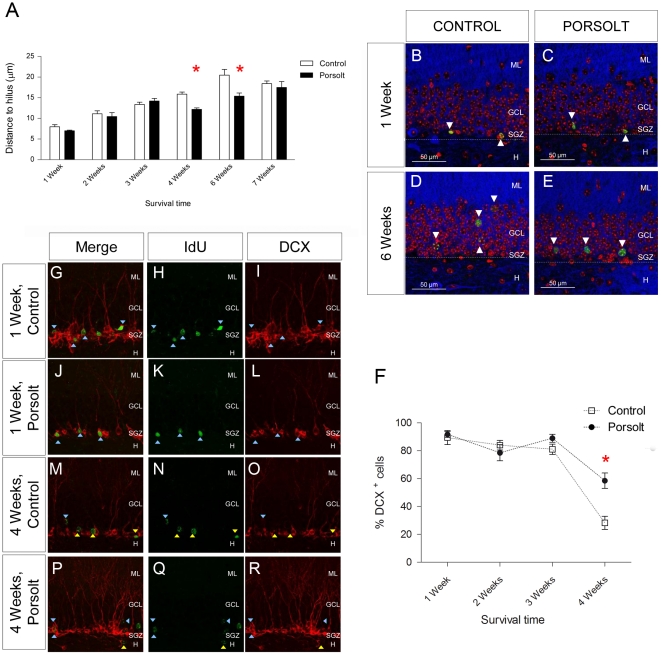
The effects of the Porsolt test and mifepristone administration on the maturation and differentiation of newborn cells
The distance from the nucleus of each newborn cell to the hilus layer was measured in at different ages and under distinct experimental conditions. Two-way ANOVA revealed a significant influence on this distance of “age” (F5,88 = 34.212, p<0.001) and of the “Porsolt test” (F1,25 = 11.655, p<0.001), as well as a significant interaction (F5,25 = 20.220, p = 0.014). The distance to the hilus border increased with age (as shown in Figure 4 A) and a post hoc analysis revealed that exposure to the Porsolt test significantly reduced the distance to hilus in 4 (p = 0.001) and 6 (p = 0.002) week-old cells (Figure 4 A). These changes were evident in images of cells taken from representative locations in 1 and 6 week-old cells from the different experimental groups (Figure 4 B–E).
Figure 4. Maturation of newborn cells.
A Distance between the nucleus of different aged cells and the hilus. This distance increased with cell age (p<0.001). Exposure to the Porsolt test reduced the distance in 4 (p = 0.001) and 6 week-old (p = 0.002) cells. B–E Representative images of immunohistochemistry against IdU or CldU (green) and AMPA (blue), in cells counterstained with DAPI (red), showing the relative position of 1 and 6 week-old cells inside the GCL of control animals and those exposed to the Porsolt test. F DCX expression in newborn cells of different ages. The Porsolt test increased the percentage of 4 week-old cells that were also DCX+(p = 0.022), but had no effect in cells of 1, 2 or 3 weeks of age. G–R Representative images of double immunohistochemistry for DCX (red) and IdU or CldU (green). DCX+ and DCX- cells are represented by purple and yellow triangles, respectively. ML: Molecular layer; GCL: Granule cell layer; SGZ: Subgranular zone; H: Hilus. Scale bar = 20 µm.
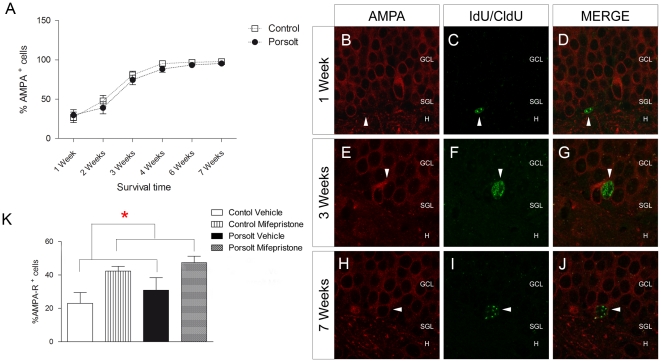
DCX expression in neurons from 1, 2, 3 and 4 week old cells was evaluated in control animals and those subjected to the Porsolt test (Figure 4 F, G– R). Two-way ANOVA revealed a significant effect of “age” (F3,58 = 39.598, p<0.001) and of the “Porsolt test” (F1,58 = 6.966, p = 0.011) on the percentage of newborn cells expressing DCX, as well as a significant interaction (F3,57 = 2.547, p = 0.067). Indeed, a post hoc analysis revealed an increase in the percentage of DCX+ cells in 4 week-old cells following exposure to the Porsolt test when compared to the controls (p = 0.022). Interestingly, the percentage of AMPA+ cells increased with age (Age F6,98 = 69.256, p<0.001; Porsolt F1,98 = 3.884, p = 0.152; Interaction F6,98 = 0.269, p = 0.929: Figure 5 A– J), and there was an increase in the percentage of AMPA+ cells in 1 week-old cells in response to mifepristone treatment (Mifepristone F1,27 = 10.900, p = 0.003; Porsolt F1,27 = 1.433, p = 0.244; Interaction F1,27 = 0.062, p = 0.805: Figure 5 K).
Figure 5. Effects of mifepristone and the Porsolt test on AMPA receptor expression in newborn cells.
A AMPA receptor expression in cells of different ages. AMPA receptor expression increased with age (p<0.001). B–J Images of double immunohistochemistry for the AMPA receptor (red) and IdU or CldU (green). The majority of 7 week-old cells were AMPA+. K Modulation of AMPA receptor expression by mifepristone. Mifepristone increased the proportion of AMPA+ cells in 1 week-old newborn cells (p = 0.003). ML: Molecular layer; GCL: Granule cell layer; SGZ: Subgranular zone; H: Hilus. Scale bar = 50 µm.
Discussion
There is considerable evidence linking AHN to mood disorders [50] [51]. Chronic stress is widely considered to be a pathogenic factor for major depression (MD) and it also provokes a reduction in AHN [52]. Furthermore, many beneficial strategies to treat of symptoms of depression selectively enhance AHN [53]. Nonetheless, little is known about the mechanisms through which glucocorticoids interact with developing neurons during AHN. We quantified the survival of different subpopulations of newborn hippocampal neurons in response to the Porsolt or forced swim test, a commonly used a model of acute stress. While chronic stress is known to induce a general decrease in AHN [9] [54] [25] [55], there it unclear how acute stress affects this process [56] [57]. In agreement with our findings, numerous studies have reported that the proliferation of neuronal precursors in the rodent DG is not drastically modified by exposure to different acute stresses [58] [59] [60] [61] [62], although a reduced rate of proliferation in the hippocampus of shrew monkeys has been described following acute stress [63].
The exact role of immature newborn neurons remains poorly understood, although they increasingly appear to be very relevant in hippocampal functioning [64] [65,66] [67] [68] [69]. The acute stress induced by the Porsolt test selectively decreased the number of 1 week-old cells in the DG. Moreover, while this swim test did not produce a net increase in the total number of apoptotic cells, the percentage of 1 week-old IdU+ cells undergoing apoptotic death did augment. This is consistent with several recent studies of the effects of stress exposure using a stereological approach, in which no massive apoptotic cell death was reported [61] [32] [70]. Nonetheless, we identified a cell population particularly sensitive to the effects of acute stress, as well as several populations of more-mature newborn neurons that are apparently more resistant to these effects.
Corticosteroids activate two types of receptors, MR and GR, and while GR activation is involved in acute, stress-induced and suppressive effects, MR activation is thought to contribute to tonic, long-term permissive effects [71]. Interestingly, studies in GR knockout mice have demonstrated significant alterations in hippocampal neurogenesis [72]. Both receptors are strongly expressed in limbic structures such as the hippocampus [20] [32] and our data suggest that increasing corticosteroids exerts an indirect regulatory effect that is probably mediated by other components of the stem cell niche [73]. Indeed, many cells whose survival is affected by acute stress express neither GR nor MR, and in fact only ∼15% of 1 week-old cells express GR+. Furthermore, the survival of these cells fell by 50% when compared to the controls. Our data also corroborate the age dependent increase in the percentage of hippocampal newborn cells expressing both GR and MR seen elsewhere [33] [74]. Although the percentage of GR+ 1 week-old cells we found was relatively low [33], the expression of GR was previously established in different subpopulations of immature cells while here we analyzed the expression of GR in a largely heterogeneous population of 4 to 7 day-old cells, regardless of the subtype. Methodological differences such as the GR antibody used, the thresholds established and the different cell populations analyzed may explain the apparent discrepancies in the proportions of GR+ cells here and elsewhere [33] [74].
Acute exposure to high levels of GC is known to prevent neural differentiation in 4 week-old newborn neurons in the DG [75]. Indeed, we found that the swim test-provoked stress that prevents the maturation of 4 week-old cells, blocking the decrease in the proportion of DCX+ cells observed in control animals [76] [77], and reducing other indirect indicators of differentiation, like migration to the granule layer [78]. The latter observation was recently linked to the manifestation of depressive-like behaviors [79]. An alternative explanation for the reduction in the distance to the hilus in 4 and 6 week-old cells, is that these cells move toward the hilus in response to stress, or that the loss of cells at 1 week (i.e., those closest to the hilus) results in 4 and 6 week-old cells appearing closer to the hilus.
Numerous cytokines modify the migration and differentiation of precursor cells [80] [81]. However, the expression of the pro-inflammatory cytokines IL-6 or TNF was not altered by the Porsolt test in the hippocampus, as seen elsewhere [82] [83].
There is growing evidence that several growth factor systems are modulated by both the development and treatment of MD. In fact, both chronic antidepressant treatments and stress regulates BDNF expression in a complex manner, although the underlying mechanisms remain poorly understood [84] [85] [86]. We found no significant changes in hippocampal BDNF expression following the Porsolt test, in agreement with previous reports [87], nor of IGF-I. More comprehensive studies will be necessary to determine if the expression of these growth factors or their receptors can be detected at different intervals post-stress, or in response to different stress protocols (e.g., different durations and intensity of stress).
Deregulation of glutamatergic neurotransmission has recently been implicated in the etiology of several mood disorders [36], leading to the development of several antidepressant strategies targeting the glutamatergic system [88] [89]. Transient alterations in pre-synaptic markers of glutamatergic (vGLUT1) and GABAergic (GAD65) transmission have been reported in models of chronic mild stress (CMS) [90] [58]. In the present study, the acute stress of the Porsolt test did not alter the expression of these markers in the hippocampus 4 hours after the last session, although later transient modifications cannot be ruled out. One of the proposed mechanisms mediating glutamate-provoked neurotoxicity in stress models is the sustained activation of ionotropic NMDA glutamate receptors [91] [88]. Ionotropic AMPA receptors play a very different role in these processes, and possess multiple sites at which ligand binding can fine-tune receptor activity [92]. AMPA receptors have been functionally linked to a variety of signal transduction events involving Src-family kinases, G-proteins, and MAP kinase [43]. Chronic antidepressant treatment increases the expression of AMPA receptors at the membrane [42] and requires AMPA activation to exert antidepressant effects [93] [41]. Moreover, ampakines exhibit antidepressant-like properties [94] and they are considered to be potential targets for the treatment of MD [95]. In fact, enhancing the activity of AMPA receptors regulates dendritogenesis [96] and importantly, upregulates AHN [16]. Very immature and synaptically-silent neurons approximately 1 week old respond to glutamate by activating both NMDA and AMPA receptors [98], of which the latter is thought to play an important role in the proliferation and survival of these cells [16].
The glucocorticoid antagonist family also shows some potential for the treatment of depression [92] [99] [100] [101]. In particular, the GR (but not MR) antagonist mifepristone (RU-486) is currently under study in phase III clinical trials for the treatment of depression with psychotic features [102]. Short-term treatment with mifepristone produces antidepressant effects in animal models of depression [105] and in clinical trials [103] [104]. Its rapid action is very important given the significant delay between administration of conventional antidepressants and the onset of therapeutic effects. Other methods of inhibiting activity in the HPA axis produce antidepressant effects, such as CRF1 receptor blockade, as well as normalizing AHN levels in animal models of depression [106] [107].
We found that mifepristone prevents the increase in apoptosis among 1 week-old cells induced by acute stress. This observation is consistent with reports that GR blockade can normalize the reduction in cell survival produced by the elevated GC levels mediated by chronic stress [38] [39]. In our study, the effects of mifepristone on cell survival were not associated with short term effects on animal behavior in the Porsolt test, an interesting observation given that AHN integrity is essential for different forms of learning [4] [108]. The absence of an antidepressant effect in the Porsolt test observed following acute mifepristone treatment is consistent with the dependence of the antidepressant effects of GR antisense mRNAs on the exact moment of administration in animal models of stress [109].
In conjunction with the classically-described effects of GR antagonism [110] [103], the intrinsic antioxidant properties of mifepristone are thought to promote neuronal survival [40], as oxidative stress produced by glucocorticoids appears to underlie some of their neurotoxic effects [111] [73]. However, the effects of mifepristone are more potent in environments with high glucocorticoid levels, as it does not modify proliferation or survival in control animals [38]. Moreover, the pro-survival effects of mifepristone appear to be selective for this cell population, as it did not modify the size of any of the other populations analyzed.
Mifepristone selectively increased the percentage of 1 week-old IdU+ cells expressing the AMPA receptor. Further studies will be necessary to determine whether this increase in AMPA expression contributes to the increase in cell survival in high glucocorticoid environments. However, we hypothesize that AMPA receptor expression may exert a neuroprotective effect on this cell population. Indeed, diverse ampakines have been attributed neuroprotective properties [97], making them novel targets for the treatment of depression [95]. The putative pro-survival effect of increased AMPA receptor expression in cell populations particularly sensitive to stress suggests a novel mechanism of action underlying the neuroprotective effects of mifepristone.
Supporting Information
Neither the Porsolt test nor mifepristone modified the total number of DCX+ cells (Mifepristone F1,28 = 1.236, p = 0.277; Porsolt F1,28 = 0.070, p = 0.793; Interaction F1,28 = 0.197, p = 0.661) (A), pH3+ cells (Mifepristone F1,27 = 0.002, p = 0.967; Porsolt F1,27 = 0.098, p = 0.757; Interaction F1,27 = 0.017, p = 0.899) (B), mature granule cells (Mifepristone F1,29 = 0.003, p = 0.717; Porsolt F1,29 = 0.378, p = 0.544; Interaction F1,29 = 0.468, p = 0.444) (C), or the volume of the DG (Mifepristone F1,27 = 0.003, p = 0.090; Porsolt F1,27 = 0.378, p = 0.337; Interaction F1,27 = 0.468, p = 0.459) (D). Likewise, neither the Porsolt test or mifepristone affected the total number of 7 week-old CldU+ cells (Mifepristone F1,28 = 0.073, p = 0.789; Porsolt F1,28 = 0.052, p = 0.821; Interaction F1,28 = 0.202, p = 0.657) (E). F: Acute mifepristone treatment had no effect on the immobility time in the Porsolt test (F1,23 = 0.742, p = 0.398).
(TIF)
Acknowledgments
The authors wish to thank Carmen Hernández, Belén García and José Luis Rojas for their technical assistance with confocal microscopy. We also appreciate the assistance of Ana LLorens-Martín in revising the manuscript and Dr Fabio Cafini for critical discussion of the results.
Footnotes
Competing Interests: María Llorens-Martín is not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this manuscript. José Luis Trejo is not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this manuscript.
Funding: This work was funded by grant BFU2007-60195/BFI and BFU2010-20396 from Ministerio de Educación y Ciencia to José Luis Trejo. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gage FH. Mammalian neural stem cells. Science. 2000;287:1433–1438. doi: 10.1126/science.287.5457.1433. [DOI] [PubMed] [Google Scholar]
- 2.Eriksson PS, Perfilieva E, Bjork-Eriksson T, Alborn AM, Nordborg C, et al. Neurogenesis in the adult human hippocampus. Nat Med. 1998;4:1313–1317. doi: 10.1038/3305. [DOI] [PubMed] [Google Scholar]
- 3.Deng W, Aimone JB, Gage FH. New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosci. 2010;11:339–350. doi: 10.1038/nrn2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garthe A, Behr J, Kempermann G. Adult-generated hippocampal neurons allow the flexible use of spatially precise learning strategies. PLoS One. 2009;4:e5464. doi: 10.1371/journal.pone.0005464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malberg JE, Duman RS. Cell proliferation in adult hippocampus is decreased by inescapable stress: reversal by fluoxetine treatment. Neuropsychopharmacology. 2003;28:1562–1571. doi: 10.1038/sj.npp.1300234. [DOI] [PubMed] [Google Scholar]
- 6.Santarelli L, Saxe M, Gross C, Surget A, Battaglia F, et al. Requirement of hippocampal neurogenesis for the behavioral effects of antidepressants. Science. 2003;301:805–809. doi: 10.1126/science.1083328. [DOI] [PubMed] [Google Scholar]
- 7.Van PH, Kempermann G, Gage FH. Running increases cell proliferation and neurogenesis in the adult mouse dentate gyrus. Nat Neurosci. 1999;2:266–270. doi: 10.1038/6368. [DOI] [PubMed] [Google Scholar]
- 8.Llorens-Martin M, Tejeda GS, Trejo JL. PLoS One. Vol. 5. 10.1371/journal.pone.0012188 [doi]; 2010. Differential regulation of the variations induced by environmental richness in adult neurogenesis as a function of time: a dual birthdating analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cameron HA, Gould E. Adult neurogenesis is regulated by adrenal steroids in the dentate gyrus. Neuroscience. 1994;61:203–209. doi: 10.1016/0306-4522(94)90224-0. [DOI] [PubMed] [Google Scholar]
- 10.Sairanen M, Lucas G, Ernfors P, Castren M, Castren E. Brain-derived neurotrophic factor and antidepressant drugs have different but coordinated effects on neuronal turnover, proliferation, and survival in the adult dentate gyrus. J Neurosci. 2005;25:1089–1094. doi: 10.1523/JNEUROSCI.3741-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trejo JL, Llorens-Martin MV, Torres-Aleman I. The effects of exercise on spatial learning and anxiety-like behavior are mediated by an IGF-I-dependent mechanism related to hippocampal neurogenesis. Mol Cell Neurosci. 2008;37:402–411. doi: 10.1016/j.mcn.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 12.Trejo JL, Carro E, Torres-Aleman I. Circulating insulin-like growth factor I mediates exercise-induced increases in the number of new neurons in the adult hippocampus. J Neurosci. 2001;21:1628–1634. doi: 10.1523/JNEUROSCI.21-05-01628.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Llorens-Martin M, Torres-Aleman I, Trejo JL. Exercise modulates insulin-like growth factor 1-dependent and -independent effects on adult hippocampal neurogenesis and behaviour. Mol Cell Neurosci. 2010;44:109–117. doi: 10.1016/j.mcn.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Schanzer A, Wachs FP, Wilhelm D, Acker T, Cooper-Kuhn C, et al. Direct stimulation of adult neural stem cells in vitro and neurogenesis in vivo by vascular endothelial growth factor. Brain Pathol. 2004;14:237–248. doi: 10.1111/j.1750-3639.2004.tb00060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gould E, Cameron HA, McEwen BS. Blockade of NMDA receptors increases cell death and birth in the developing rat dentate gyrus. J Comp Neurol. 1994;340:551–565. doi: 10.1002/cne.903400408. [DOI] [PubMed] [Google Scholar]
- 16.Bai F, Bergeron M, Nelson DL. Chronic AMPA receptor potentiator (LY451646) treatment increases cell proliferation in adult rat hippocampus. Neuropharmacology. 2003;44:1013–1021. doi: 10.1016/s0028-3908(03)00104-7. [DOI] [PubMed] [Google Scholar]
- 17.Monje ML, Toda H, Palmer TD. Inflammatory blockade restores adult hippocampal neurogenesis. Science. 2003;302:1760–1765. doi: 10.1126/science.1088417. [DOI] [PubMed] [Google Scholar]
- 18.Gould E, Woolley CS, McEwen BS. Adrenal steroids regulate postnatal development of the rat dentate gyrus: I. Effects of glucocorticoids on cell death. J Comp Neurol. 1991;313:479–485. doi: 10.1002/cne.903130308. [DOI] [PubMed] [Google Scholar]
- 19.Wong EY, Herbert J. Roles of mineralocorticoid and glucocorticoid receptors in the regulation of progenitor proliferation in the adult hippocampus. Eur J Neurosci. 2005;22:785–792. doi: 10.1111/j.1460-9568.2005.04277.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joels M. Role of corticosteroid hormones in the dentate gyrus. Prog Brain Res. 2007;163:355–370. doi: 10.1016/S0079-6123(07)63021-0. [DOI] [PubMed] [Google Scholar]
- 21.Reagan LP, McEwen BS. Controversies surrounding glucocorticoid-mediated cell death in the hippocampus. J Chem Neuroanat. 1997;13:149–167. doi: 10.1016/s0891-0618(97)00031-8. [DOI] [PubMed] [Google Scholar]
- 22.Ahmed T, Frey JU, Korz V. Long-term effects of brief acute stress on cellular signaling and hippocampal LTP. J Neurosci. 2006;26:3951–3958. doi: 10.1523/JNEUROSCI.4901-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quirarte GL, de lT, I, Casillas M, Serafin N, Prado-Alcala RA, et al. Corticosterone infused into the dorsal striatum selectively enhances memory consolidation of cued water-maze training. Learn Mem. 2009;16:586–589. doi: 10.1101/lm.1493609. [DOI] [PubMed] [Google Scholar]
- 24.Maes M, Yirmyia R, Noraberg J, Brene S, Hibbeln J, et al. The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression. Metab Brain Dis. 2009;24:27–53. doi: 10.1007/s11011-008-9118-1. [DOI] [PubMed] [Google Scholar]
- 25.Sterner EY, Kalynchuk LE. Behavioral and neurobiological consequences of prolonged glucocorticoid exposure in rats: relevance to depression. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:777–790. doi: 10.1016/j.pnpbp.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 26.McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54:200–207. doi: 10.1016/s0006-3223(03)00177-x. [DOI] [PubMed] [Google Scholar]
- 27.Dhikav V, Anand KS. Glucocorticoids may initiate Alzheimer's disease: a potential therapeutic role for mifepristone (RU-486). Med Hypotheses. 2007;68:1088–1092. doi: 10.1016/j.mehy.2006.09.038. [DOI] [PubMed] [Google Scholar]
- 28.Luine V, Villegas M, Martinez C, McEwen BS. Stress-dependent impairments of spatial memory. Role of 5-HT. Ann N Y Acad Sci. 1994;746:403–404. doi: 10.1111/j.1749-6632.1994.tb39268.x. [DOI] [PubMed] [Google Scholar]
- 29.Li WZ, Li WP, Yao YY, Zhang W, Yin YY, et al. Glucocorticoids increase impairments in learning and memory due to elevated amyloid precursor protein expression and neuronal apoptosis in 12-month old mice. Eur J Pharmacol. 2010;628:108–115. doi: 10.1016/j.ejphar.2009.11.045. [DOI] [PubMed] [Google Scholar]
- 30.Sousa N, Cerqueira JJ, Almeida OF. Corticosteroid receptors and neuroplasticity. Brain Res Rev. 2008;57:561–570. doi: 10.1016/j.brainresrev.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 31.Fitzsimons CP, van Hooijdonk LW, Morrow JA, Peeters BW, Hamilton N, et al. Antiglucocorticoids, neurogenesis and depression. Mini Rev Med Chem. 2009;9:249–264. doi: 10.2174/138955709787316001. [DOI] [PubMed] [Google Scholar]
- 32.Sousa N, Almeida OF. Corticosteroids: sculptors of the hippocampal formation. Rev Neurosci. 2002;13:59–84. doi: 10.1515/revneuro.2002.13.1.59. [DOI] [PubMed] [Google Scholar]
- 33.Garcia A, Steiner B, Kronenberg G, Bick-Sander A, Kempermann G. Age-dependent expression of glucocorticoid- and mineralocorticoid receptors on neural precursor cell populations in the adult murine hippocampus. Aging Cell. 2004;3:363–371. doi: 10.1111/j.1474-9728.2004.00130.x. [DOI] [PubMed] [Google Scholar]
- 34.Tata DA, Anderson BJ. The effects of chronic glucocorticoid exposure on dendritic length, synapse numbers and glial volume in animal models: implications for hippocampal volume reductions in depression. Physiol Behav. 2010;99:186–193. doi: 10.1016/j.physbeh.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Kloet ER, Joels M, Holsboer F. Stress and the brain: from adaptation to disease. Nat Rev Neurosci. 2005;6:463–475. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- 36.Zarate CA, Jr, Du J, Quiroz J, Gray NA, Denicoff KD, et al. Regulation of cellular plasticity cascades in the pathophysiology and treatment of mood disorders: role of the glutamatergic system. Ann N Y Acad Sci. 2003;1003:273–291. doi: 10.1196/annals.1300.017. [DOI] [PubMed] [Google Scholar]
- 37.Lowy MT, Wittenberg L, Yamamoto BK. Effect of acute stress on hippocampal glutamate levels and spectrin proteolysis in young and aged rats. J Neurochem. 1995;65:268–274. doi: 10.1046/j.1471-4159.1995.65010268.x. [DOI] [PubMed] [Google Scholar]
- 38.Oomen CA, Mayer JL, de Kloet ER, Joels M, Lucassen PJ. Brief treatment with the glucocorticoid receptor antagonist mifepristone normalizes the reduction in neurogenesis after chronic stress. Eur J Neurosci. 2007;26:3395–3401. doi: 10.1111/j.1460-9568.2007.05972.x. [DOI] [PubMed] [Google Scholar]
- 39.Mayer JL, Klumpers L, Maslam S, de Kloet ER, Joels M, et al. Brief treatment with the glucocorticoid receptor antagonist mifepristone normalises the corticosterone-induced reduction of adult hippocampal neurogenesis. J Neuroendocrinol. 2006;18:629–631. doi: 10.1111/j.1365-2826.2006.01455.x. [DOI] [PubMed] [Google Scholar]
- 40.Behl C, Trapp T, Skutella T, Holsboer F. Protection against oxidative stress-induced neuronal cell death–a novel role for RU486. Eur J Neurosci. 1997;9:912–920. doi: 10.1111/j.1460-9568.1997.tb01442.x. [DOI] [PubMed] [Google Scholar]
- 41.Karasawa J, Shimazaki T, Kawashima N, Chaki S. AMPA receptor stimulation mediates the antidepressant-like effect of a group II metabotropic glutamate receptor antagonist. Brain Res. 2005;1042:92–98. doi: 10.1016/j.brainres.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 42.Martinez-Turrillas R, Del RJ, Frechilla D. Neuronal proteins involved in synaptic targeting of AMPA receptors in rat hippocampus by antidepressant drugs. Biochem Biophys Res Commun. 2007;353:750–755. doi: 10.1016/j.bbrc.2006.12.078. [DOI] [PubMed] [Google Scholar]
- 43.Suppiramaniam V, Bahr BA, Sinnarajah S, Owens K, Rogers G, et al. Member of the Ampakine class of memory enhancers prolongs the single channel open time of reconstituted AMPA receptors. Synapse. 2001;40:154–158. doi: 10.1002/syn.1037. [DOI] [PubMed] [Google Scholar]
- 44.Llorens-Martin MV, Rueda N, Martinez-Cue C, Torres-Aleman I, Florez J, et al. Both increases in immature dentate neuron number and decreases of immobility time in the forced swim test occurred in parallel after environmental enrichment of mice. Neuroscience. 2007;147:631–638. doi: 10.1016/j.neuroscience.2007.04.054. [DOI] [PubMed] [Google Scholar]
- 45.Porsolt RD, Le PM, Jalfre M. Depression: a new animal model sensitive to antidepressant treatments. Nature. 1977;266:730–732. doi: 10.1038/266730a0. [DOI] [PubMed] [Google Scholar]
- 46.Detke MJ, Rickels M, Lucki I. Active behaviors in the rat forced swimming test differentially produced by serotonergic and noradrenergic antidepressants. Psychopharmacology (Berl) 1995;121:66–72. doi: 10.1007/BF02245592. [DOI] [PubMed] [Google Scholar]
- 47.Llorens-Martin M, Torres-Aleman I, Trejo JL. Pronounced individual variation in the response to the stimulatory action of exercise on immature hippocampal neurons. Hippocampus. 2006;16:480–490. doi: 10.1002/hipo.20175. [DOI] [PubMed] [Google Scholar]
- 48.Leuner B, Glasper ER, Gould E. Thymidine analog methods for studies of adult neurogenesis are not equally sensitive. J Comp Neurol. 2009;517:123–133. doi: 10.1002/cne.22107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pfaffl MW. The ongoing evolution of qPCR. Methods. 2010;50:215–216. doi: 10.1016/j.ymeth.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 50.Becker S, Wojtowicz JM. A model of hippocampal neurogenesis in memory and mood disorders. Trends Cogn Sci. 2007;11:70–76. doi: 10.1016/j.tics.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 51.Duman RS. Role of neurotrophic factors in the etiology and treatment of mood disorders. Neuromolecular Med. 2004;5:11–25. doi: 10.1385/NMM:5:1:011. [DOI] [PubMed] [Google Scholar]
- 52.Mirescu C, Gould E. Stress and adult neurogenesis. Hippocampus. 2006;16:233–238. doi: 10.1002/hipo.20155. [DOI] [PubMed] [Google Scholar]
- 53.Encinas JM, Vaahtokari A, Enikolopov G. Fluoxetine targets early progenitor cells in the adult brain. Proc Natl Acad Sci U S A. 2006;103:8233–8238. doi: 10.1073/pnas.0601992103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tanapat P, Galea LA, Gould E. Stress inhibits the proliferation of granule cell precursors in the developing dentate gyrus. Int J Dev Neurosci. 1998;16:235–239. doi: 10.1016/s0736-5748(98)00029-x. [DOI] [PubMed] [Google Scholar]
- 55.Brummelte S, Galea LA. Chronic high corticosterone reduces neurogenesis in the dentate gyrus of adult male and female rats. Neuroscience. 2010;168:680–690. doi: 10.1016/j.neuroscience.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 56.Dagyte G, Van der Zee EA, Postema F, Luiten PG, Den Boer JA, et al. Chronic but not acute foot-shock stress leads to temporary suppression of cell proliferation in rat hippocampus. Neuroscience. 2009;162:904–913. doi: 10.1016/j.neuroscience.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 57.Heine VM, Maslam S, Zareno J, Joels M, Lucassen PJ. Suppressed proliferation and apoptotic changes in the rat dentate gyrus after acute and chronic stress are reversible. Eur J Neurosci. 2004;19:131–144. doi: 10.1046/j.1460-9568.2003.03100.x. [DOI] [PubMed] [Google Scholar]
- 58.Autry AE, Grillo CA, Piroli GG, Rothstein JD, McEwen BS, et al. Glucocorticoid regulation of GLT-1 glutamate transporter isoform expression in the rat hippocampus. Neuroendocrinology. 2006;83:371–379. doi: 10.1159/000096092. [DOI] [PubMed] [Google Scholar]
- 59.Thomas RM, Hotsenpiller G, Peterson DA. Acute psychosocial stress reduces cell survival in adult hippocampal neurogenesis without altering proliferation. J Neurosci. 2007;27:2734–2743. doi: 10.1523/JNEUROSCI.3849-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee KJ, Kim SJ, Kim SW, Choi SH, Shin YC, et al. Chronic mild stress decreases survival, but not proliferation, of new-born cells in adult rat hippocampus. Exp Mol Med. 2006;38:44–54. doi: 10.1038/emm.2006.6. [DOI] [PubMed] [Google Scholar]
- 61.Leverenz JB, Wilkinson CW, Wamble M, Corbin S, Grabber JE, et al. Effect of chronic high-dose exogenous cortisol on hippocampal neuronal number in aged nonhuman primates. J Neurosci. 1999;19:2356–2361. doi: 10.1523/JNEUROSCI.19-06-02356.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thomas RM, Urban JH, Peterson DA. Acute exposure to predator odor elicits a robust increase in corticosterone and a decrease in activity without altering proliferation in the adult rat hippocampus. Exp Neurol. 2006;201:308–315. doi: 10.1016/j.expneurol.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 63.Gould E, McEwen BS, Tanapat P, Galea LA, Fuchs E. Neurogenesis in the dentate gyrus of the adult tree shrew is regulated by psychosocial stress and NMDA receptor activation. J Neurosci. 1997;17:2492–2498. doi: 10.1523/JNEUROSCI.17-07-02492.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wiskott L, Rasch MJ, Kempermann G. A functional hypothesis for adult hippocampal neurogenesis: avoidance of catastrophic interference in the dentate gyrus. Hippocampus. 2006;16:329–343. doi: 10.1002/hipo.20167. [DOI] [PubMed] [Google Scholar]
- 65.Kee N, Teixeira CM, Wang AH, Frankland PW. Preferential incorporation of adult-generated granule cells into spatial memory networks in the dentate gyrus. Nat Neurosci. 2007;10:355–362. doi: 10.1038/nn1847. [DOI] [PubMed] [Google Scholar]
- 66.Schmidt-Hieber C, Jonas P, Bischofberger J. Enhanced synaptic plasticity in newly generated granule cells of the adult hippocampus. Nature. 2004;429:184–187. doi: 10.1038/nature02553. [DOI] [PubMed] [Google Scholar]
- 67.Van PH, Schinder AF, Christie BR, Toni N, Palmer TD, et al. Functional neurogenesis in the adult hippocampus. Nature. 2002;415:1030–1034. doi: 10.1038/4151030a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang S, Scott BW, Wojtowicz JM. Heterogenous properties of dentate granule neurons in the adult rat. J Neurobiol. 2000;42:248–257. [PubMed] [Google Scholar]
- 69.Lagace DC, Donovan MH, DeCarolis NA, Farnbauch LA, Malhotra S, et al. Adult hippocampal neurogenesis is functionally important for stress-induced social avoidance. Proc Natl Acad Sci U S A. 2010;107:4436–4441. doi: 10.1073/pnas.0910072107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Czeh B, Lucassen PJ. What causes the hippocampal volume decrease in depression? Are neurogenesis, glial changes and apoptosis implicated? Eur Arch Psychiatry Clin Neurosci. 2007;257:250–260. doi: 10.1007/s00406-007-0728-0. [DOI] [PubMed] [Google Scholar]
- 71.Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21:55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- 72.Kronenberg G, Kirste I, Inta D, Chourbaji S, Heuser I, et al. Reduced hippocampal neurogenesis in the GR(+/-) genetic mouse model of depression. Eur Arch Psychiatry Clin Neurosci. 2009;259:499–504. doi: 10.1007/s00406-009-0036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Behl C, Lezoualc'h F, Trapp T, Widmann M, Skutella T, et al. Glucocorticoids enhance oxidative stress-induced cell death in hippocampal neurons in vitro. Endocrinology. 1997;138:101–106. doi: 10.1210/endo.138.1.4835. [DOI] [PubMed] [Google Scholar]
- 74.Cameron HA, Woolley CS, Gould E. Adrenal steroid receptor immunoreactivity in cells born in the adult rat dentate gyrus. Brain Res. 1993;611:342–346. doi: 10.1016/0006-8993(93)90524-q. [DOI] [PubMed] [Google Scholar]
- 75.Wong EY, Herbert J. Raised circulating corticosterone inhibits neuronal differentiation of progenitor cells in the adult hippocampus. Neuroscience. 2006;137:83–92. doi: 10.1016/j.neuroscience.2005.08.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Brown JP, Couillard-Despres S, Cooper-Kuhn CM, Winkler J, Aigner L, et al. Transient expression of doublecortin during adult neurogenesis. J Comp Neurol. 2003;467:1–10. doi: 10.1002/cne.10874. [DOI] [PubMed] [Google Scholar]
- 77.Kempermann G, Jessberger S, Steiner B, Kronenberg G. Milestones of neuronal development in the adult hippocampus. Trends Neurosci. 2004;27:447–452. doi: 10.1016/j.tins.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 78.Kempermann G, Gast D, Kronenberg G, Yamaguchi M, Gage FH. Early determination and long-term persistence of adult-generated new neurons in the hippocampus of mice. Development. 2003;130:391–399. doi: 10.1242/dev.00203. [DOI] [PubMed] [Google Scholar]
- 79.Lussier AL, Caruncho HJ, Kalynchuk LE. Repeated exposure to corticosterone, but not restraint, decreases the number of reelin-positive cells in the adult rat hippocampus. Neurosci Lett. 2009;460:170–174. doi: 10.1016/j.neulet.2009.05.050. [DOI] [PubMed] [Google Scholar]
- 80.Whitney NP, Eidem TM, Peng H, Huang Y, Zheng JC. Inflammation mediates varying effects in neurogenesis: relevance to the pathogenesis of brain injury and neurodegenerative disorders. J Neurochem. 2009;108:1343–1359. doi: 10.1111/j.1471-4159.2009.05886.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Das S, Basu A. Inflammation: a new candidate in modulating adult neurogenesis. J Neurosci Res. 2008;86:1199–1208. doi: 10.1002/jnr.21585. [DOI] [PubMed] [Google Scholar]
- 82.Lucassen PJ, Meerlo P, Naylor AS, van Dam AM, Dayer AG, et al. Regulation of adult neurogenesis by stress, sleep disruption, exercise and inflammation: Implications for depression and antidepressant action. Eur Neuropsychopharmacol. 2010;20:1–17. doi: 10.1016/j.euroneuro.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 83.Frank MG, Miguel ZD, Watkins LR, Maier SF. Prior exposure to glucocorticoids sensitizes the neuroinflammatory and peripheral inflammatory responses to E. coli lipopolysaccharide. Brain Behav Immun. 2010;24:19–30. doi: 10.1016/j.bbi.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 84.Castren E, Voikar V, Rantamaki T. Role of neurotrophic factors in depression. Curr Opin Pharmacol. 2007;7:18–21. doi: 10.1016/j.coph.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 85.Duman RS. Neurotrophic factors and regulation of mood: role of exercise, diet and metabolism. Neurobiol Aging. 2005;26(Suppl 1):88–93. doi: 10.1016/j.neurobiolaging.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 86.Dias BG, Banerjee SB, Duman RS, Vaidya VA. Differential regulation of brain derived neurotrophic factor transcripts by antidepressant treatments in the adult rat brain. Neuropharmacology. 2003;45:553–563. doi: 10.1016/s0028-3908(03)00198-9. [DOI] [PubMed] [Google Scholar]
- 87.Nair A, Vadodaria KC, Banerjee SB, Benekareddy M, Dias BG, et al. Stressor-specific regulation of distinct brain-derived neurotrophic factor transcripts and cyclic AMP response element-binding protein expression in the postnatal and adult rat hippocampus. Neuropsychopharmacology. 2007;32:1504–1519. doi: 10.1038/sj.npp.1301276. [DOI] [PubMed] [Google Scholar]
- 88.Papp M, Moryl E. New evidence for the antidepressant activity of MK-801, a non-competitive antagonist of NMDA receptors. Pol J Pharmacol. 1993;45:549–553. [PubMed] [Google Scholar]
- 89.Sapolsky RM. The possibility of neurotoxicity in the hippocampus in major depression: a primer on neuron death. Biol Psychiatry. 2000;48:755–765. doi: 10.1016/s0006-3223(00)00971-9. [DOI] [PubMed] [Google Scholar]
- 90.Elizalde N, Garcia-Garcia AL, Totterdell S, Gendive N, Venzala E, et al. Sustained stress-induced changes in mice as a model for chronic depression. Psychopharmacology (Berl) 2010;210:393–406. doi: 10.1007/s00213-010-1835-6. [DOI] [PubMed] [Google Scholar]
- 91.Boyer PA, Skolnick P, Fossom LH. Chronic administration of imipramine and citalopram alters the expression of NMDA receptor subunit mRNAs in mouse brain. A quantitative in situ hybridization study. J Mol Neurosci. 1998;10:219–233. doi: 10.1007/BF02761776. [DOI] [PubMed] [Google Scholar]
- 92.Manji HK, Quiroz JA, Sporn J, Payne JL, Denicoff K, et al. Enhancing neuronal plasticity and cellular resilience to develop novel, improved therapeutics for difficult-to-treat depression. Biol Psychiatry. 2003;53:707–742. doi: 10.1016/s0006-3223(03)00117-3. [DOI] [PubMed] [Google Scholar]
- 93.Maeng S, Zarate CA, Jr, Du J, Schloesser RJ, McCammon J, et al. Cellular mechanisms underlying the antidepressant effects of ketamine: role of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptors. Biol Psychiatry. 2008;63:349–352. doi: 10.1016/j.biopsych.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 94.Li X, Tizzano JP, Griffey K, Clay M, Lindstrom T, et al. Antidepressant-like actions of an AMPA receptor potentiator (LY392098). Neuropharmacology. 2001;40:1028–1033. doi: 10.1016/s0028-3908(00)00194-5. [DOI] [PubMed] [Google Scholar]
- 95.Zarate CA, Jr, Manji HK. The role of AMPA receptor modulation in the treatment of neuropsychiatric diseases. Exp Neurol. 2008;211:7–10. doi: 10.1016/j.expneurol.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Voss OP, Milne S, Sharkey J, O'Neill MJ, McCulloch J. Molecular mechanisms of neurite growth with AMPA receptor potentiation. Neuropharmacology. 2007;52:590–597. doi: 10.1016/j.neuropharm.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 97.Su XW, Li XY, Banasr M, Koo JW, Shahid M, et al. Chronic treatment with AMPA receptor potentiator Org 26576 increases neuronal cell proliferation and survival in adult rodent hippocampus. Psychopharmacology (Berl) 2009;206:215–222. doi: 10.1007/s00213-009-1598-0. [DOI] [PubMed] [Google Scholar]
- 98.Ambrogini P, Minelli A, Lattanzi D, Ciuffoli S, Fanelli M, et al. Synaptically-silent immature neurons show gaba and glutamate receptor-mediated currents in adult rat dentate gyrus. Arch Ital Biol. 2006;144:115–126. [PubMed] [Google Scholar]
- 99.DeBattista C, Belanoff J, Glass S, Khan A, Horne RL, et al. Mifepristone versus placebo in the treatment of psychosis in patients with psychotic major depression. Biol Psychiatry. 2006;60:1343–1349. doi: 10.1016/j.biopsych.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 100.Belanoff JK, Flores BH, Kalezhan M, Sund B, Schatzberg AF. Rapid reversal of psychotic depression using mifepristone. J Clin Psychopharmacol. 2001;21:516–521. doi: 10.1097/00004714-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 101.Murphy BE, Filipini D, Ghadirian AM. Possible use of glucocorticoid receptor antagonists in the treatment of major depression: preliminary results using RU 486. J Psychiatry Neurosci. 1993;18:209–213. [PMC free article] [PubMed] [Google Scholar]
- 102.Nihalani ND, Schwartz TL. Mifepristone, a glucocorticoid antagonist for the potential treatment of psychotic major depression. Curr Opin Investig Drugs. 2007;8:563–569. [PubMed] [Google Scholar]
- 103.Flores BH, Kenna H, Keller J, Solvason HB, Schatzberg AF. Clinical and biological effects of mifepristone treatment for psychotic depression. Neuropsychopharmacology. 2006;31:628–636. doi: 10.1038/sj.npp.1300884. [DOI] [PubMed] [Google Scholar]
- 104.Belanoff JK, Rothschild AJ, Cassidy F, DeBattista C, Baulieu EE, et al. An open label trial of C-1073 (mifepristone) for psychotic major depression. Biol Psychiatry. 2002;52:386–392. doi: 10.1016/s0006-3223(02)01432-4. [DOI] [PubMed] [Google Scholar]
- 105.Veldhuis HD, De Korte CC, de Kloet ER. Glucocorticoids facilitate the retention of acquired immobility during forced swimming. Eur J Pharmacol. 1985;115:211–217. doi: 10.1016/0014-2999(85)90693-4. [DOI] [PubMed] [Google Scholar]
- 106.Overstreet DH, Griebel G. Antidepressant-like effects of CRF1 receptor antagonist SSR125543 in an animal model of depression. Eur J Pharmacol. 2004;497:49–53. doi: 10.1016/j.ejphar.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 107.Alonso R, Griebel G, Pavone G, Stemmelin J, le FG, et al. Blockade of CRF(1) or V(1b) receptors reverses stress-induced suppression of neurogenesis in a mouse model of depression. Mol Psychiatry. 2004;9:278–86, 224. doi: 10.1038/sj.mp.4001464. [DOI] [PubMed] [Google Scholar]
- 108.Dupret D, Fabre A, Dobrossy MD, Panatier A, Rodriguez JJ, et al. Spatial learning depends on both the addition and removal of new hippocampal neurons. PLoS Biol. 2007;5:e214. doi: 10.1371/journal.pbio.0050214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Korte SM, de Kloet ER, Buwalda B, Bouman SD, Bohus B. Antisense to the glucocorticoid receptor in hippocampal dentate gyrus reduces immobility in forced swim test. Eur J Pharmacol. 1996;301:19–25. doi: 10.1016/0014-2999(96)00064-7. [DOI] [PubMed] [Google Scholar]
- 110.Peeters BW, Ruigt GS, Craighead M, Kitchener P. Differential effects of the new glucocorticoid receptor antagonist ORG 34517 and RU486 (mifepristone) on glucocorticoid receptor nuclear translocation in the AtT20 cell line. Ann N Y Acad Sci. 2008;1148:536–541. doi: 10.1196/annals.1410.072. [DOI] [PubMed] [Google Scholar]
- 111.You JM, Yun SJ, Nam KN, Kang C, Won R, et al. Mechanism of glucocorticoid-induced oxidative stress in rat hippocampal slice cultures. Can J Physiol Pharmacol. 2009;87:440–447. doi: 10.1139/y09-027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Neither the Porsolt test nor mifepristone modified the total number of DCX+ cells (Mifepristone F1,28 = 1.236, p = 0.277; Porsolt F1,28 = 0.070, p = 0.793; Interaction F1,28 = 0.197, p = 0.661) (A), pH3+ cells (Mifepristone F1,27 = 0.002, p = 0.967; Porsolt F1,27 = 0.098, p = 0.757; Interaction F1,27 = 0.017, p = 0.899) (B), mature granule cells (Mifepristone F1,29 = 0.003, p = 0.717; Porsolt F1,29 = 0.378, p = 0.544; Interaction F1,29 = 0.468, p = 0.444) (C), or the volume of the DG (Mifepristone F1,27 = 0.003, p = 0.090; Porsolt F1,27 = 0.378, p = 0.337; Interaction F1,27 = 0.468, p = 0.459) (D). Likewise, neither the Porsolt test or mifepristone affected the total number of 7 week-old CldU+ cells (Mifepristone F1,28 = 0.073, p = 0.789; Porsolt F1,28 = 0.052, p = 0.821; Interaction F1,28 = 0.202, p = 0.657) (E). F: Acute mifepristone treatment had no effect on the immobility time in the Porsolt test (F1,23 = 0.742, p = 0.398).
(TIF)