Abstract
Study Objectives:
RBD may result in sleep related injury (SRI) particularly if a patient exits the bed during dream enactment behavior (DEB). The complex auditory processing and low arousal threshold of REM sleep offers a therapeutic window to halt behavior prior to SRI. We evaluated whether a recorded message prevents SRI in medically refractory RBD.
Design:
Case Series.
Setting:
Sleep disorders center.
Patients:
Four consecutive RBD patients with continued SRI despite both clonazepam and melatonin therapy.
Intervention:
A pressurized bed alarm customized with a familiar voice to deliver a calming message during vigorous DEB.
Measurements and Results:
The RBDQ-HK evaluated RBD symptoms, and SRI was further quantified with a new clinical tool, the Minnesota Parasomnia Injury Scale. All patients reported a decrease in RBD symptoms and SRI. No injuries occurred post-intervention. Pre-treatment: 5 serious events (SE), 80 minor events (ME), and 193 near events (NE) were noted over 66 patient-months (4.21 events/pt-mo). Post-treatment: 0 SE, 0 ME, and 3 NE were noted after a follow up period of 63 pt-months (0.05 event/pt-mo). There were 176 total bed alarm interventions (2.79 interventions/pt-mo). No adverse effects were reported, and all 4 patients described a minimal burden of treatment. RBD symptoms improved as the average RBDQ-HK score decreased from 68 (range: 53-80) to 54 (range 42-65).
Conclusion:
A customized bed alarm may be an effective method to prevent SRI in RBD. This intervention is most suitable for cases of medically refractory RBD and/or for those patients who are unable to tolerate medical therapy.
Citation:
Howell MJ; Arneson PA; Schenck CH. A novel therapy for REM sleep behavior disorder (RBD). J Clin Sleep Med 2011;7(6):639-644.
Keywords: REM sleep behavior disorder, bed alarm, clonazepam, melatonin, Parkinson disease, Minnesota Parasomnia Injury Scale
REM sleep behavior disorder (RBD) is characterized by dream enactment behavior (DEB) resulting from a loss of REM skeletal muscle atonia.1,2 Both patients and bed partners may experience sleep related injury (SRI) from behaviors such as punching or kicking. Exiting the bed while acting out a dream is a particularly high-risk behavior and may result in severe traumatic injury.3–5
Although clonazepam and melatonin are usually effective therapies,6–8 they are often inadequate in the setting of neurodegenerative disease. RBD is often the cardinal finding among patients with impending synucleinopathies such as Parkinson disease, as well as other neurodegenerative disorders such as spinocerebellar ataxia.9,10 In these patients, the most commonly prescribed medication, clonazepam, has several limitations. Clonazepam has a prolonged duration of action resulting in daytime consequences such as sedation, cognitive impairment, and falls.11 Furthermore, clonazepam may exacerbate sleep disordered breathing; long-term follow-up studies are confounded by escalating dosages as well as high drop-out rates.6,12,13 Other pharmacological agents have been explored as potential therapies, particularly melatonin; however, breakthrough SRI commonly occurs.7,8,13 Further, the long-term efficacy and tolerability of CNS agents in the setting of progressive dementing illnesses are unknown, in contrast with the longitudinal data in idiopathic RBD.14 These findings suggest that alternative, non-pharmacologic therapies are needed to augment the treatment of RBD. Modification of the sleeping environment is recommended in current management guidelines; however, the efficacies of specific interventions are unknown.15
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep related injury is common and potentially life threatening in REM sleep Behavior Disorder (RBD). However, the unique features of REM sleep, low arousal threshold and capacity for complex auditory processing, suggests that a bed alarm with voice recording could potentially halt injurious dream enactment behavior in RBD.
Study Impact: This is the first study to demonstrate a therapy to prevent sleep related injury in RBD. This treatment is most useful in the setting of medication resistent RBD or in cases associated with neurodegeneration who are unable to tolerate medical therapy.
While RBD is a challenging condition to treat, the low arousal threshold of REM sleep and its rapid transition to alert wakefulness and orientation offers a therapeutic window to halt behavior prior to SRI.16,17 During in-laboratory polysomnography (PSG) we have observed that patients can often be verbally redirected during DEB (see video online at www.aasmnet.org/jcsm). Additionally, bed partners have described pacifying patients with a calming phrase such as: “David, you're having a dream, go back to sleep.” However, patients may not have a bed partner, or the bed partner may be sleeping deeply and be unresponsive at the initial stages of the patient's DEB.
This study investigates whether a novel therapy, a bed alarm customized with a familiar voice, prevents SRI in the setting of medically refractory RBD. In order to better quantify injuries and potential injuries, we developed and administered the Minnesota Parasomnia Injury Scale.
METHODS
We selected a consecutive group of medication-resistant RBD patients for treatment with a customized bed alarm. Ideal voices, typically those of family members, were identified, and calming commands to halt dream enactment behavior were then recorded. All RBD patients who were given this treatment are reported here.
Three of the 4 patients were fitted with a Posey Sitter Select bed alarm system; one patient (patient #2) acquired a TABS bed exit monitor. The Posey Sitter Select works through a pressure-sensing pad placed underneath the shoulders of a sleeping patient. In addition to a pressure pad, the TABS unit also has a tethered cord with clothing clip that alarms when pulled from the bedside unit. When the patient arises from bed or moves enough to during the night to pull the cord from its magnetic seal, a recorded voice emanates from a bed side speaker on a repeating loop until the patient returns to lying down on the pressure pad and/or replaces the magnetic tether.
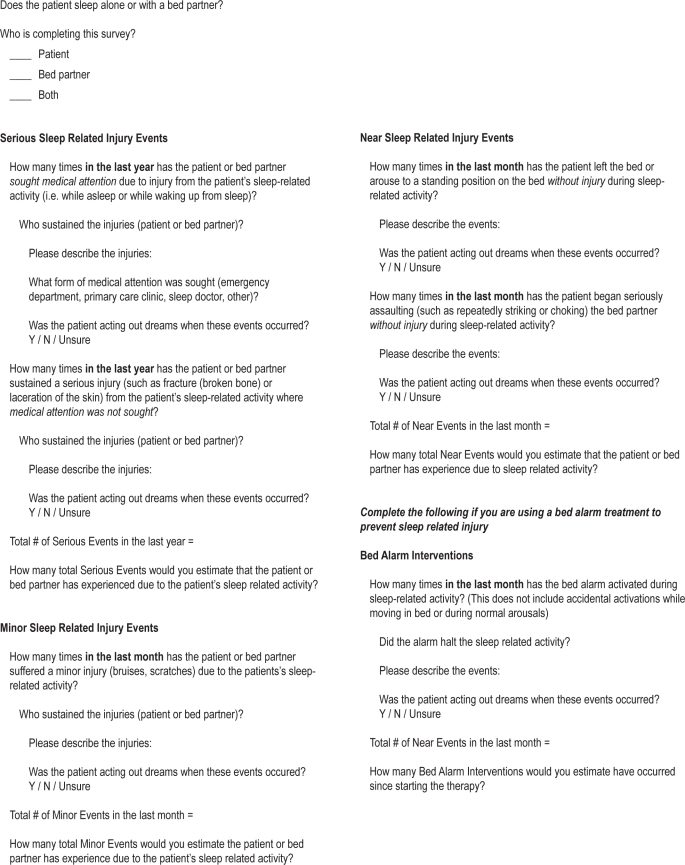
We surveyed patients and bed partners for RBD symptoms and SRI pre- and post-intervention (bed partner report was available for patients #2 and #3). The RBDQ-HK is a validated 13-item measure with scores ranging from 0-100. A higher score indicates a greater severity of parasomnia symptoms.18 The RBDQ-HK has high internal consistency and test-retest reliability. When > 18, the RBDQ-HK has a positive predictive value of 86%, while a score ≤ 18 has a negative predictive value of 83%. In order to better quantify patient and bed partner SRI we developed and administered the Minnesota Parasomnia Injury Scale (see Table 2 and Appendix, appendix is available online at www.aasmnet.org/jcsm). The MPIS registered a serious SRI event (SE) if medical attention was sought or if the injury resulted in significant musculoskeletal injury such as a fracture or laceration. Minor SRI events (ME) included bruises and scratches in the last month. Near SRI events (NE) occurred if the patient arose from bed or was aggressive towards the bed partner without injury. MEs and NEs were quantified over the preceding month, while SEs were quantified over the preceding year, as they tended to be both more memorable and less frequent. Based upon previous RBD investigations,19 a bed partner's report, if available, was preferred.
Table 2.
Sleep related injury events pre- and post- bed alarm treatment
| Patient |
||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Serious Events | ||||
| Pre (yr avg) | 2 (2/y) | 2 (1/y) | 1 (0.75/y) | 0 (0/y) |
| Post (yr avg) | 0 (0/y) | 0 (0/y) | 0 (0/y) | 0 (0/y) |
| Minor Events | ||||
| Pre (mo avg) | 24 (2/mo) | 48 (2/mo) | 3 (0.17/mo) | 5 (0.17/mo) |
| Post (mo avg) | 0 (0/mo) | 0 (0/mo) | 0 (0/mo) | 0 (0/mo) |
| Near Events | ||||
| Pre (mo avg) | 96 (8/mo) | 72 (6/mo) | 20 (1.11/mo) | 5 (0.17/mo) |
| Post (mo avg) | 0 (0/mo) | 1 (0.07/mo) | 2 (0.33/mo) | 0 (0/mo) |
| RBDQ-HK | ||||
| Pre | * | 80 | 70 | 53 |
| Post | 32 | 65 | 55** | 42** |
| follow-up | 36 months | 15 months | 6 months | 6 months |
No pretreatment HBDQ-HK data.
As patient #3 and #4 only had 6 months of follow up. RBDQ-HK post-scores were based on average symptoms in the last 6 months instead of the last 1 year.
RESULTS
The patients ranged in age from 61 to 87 years, and all had a clinical and PSG diagnosis of RBD. Additionally, patient #1 had a longstanding sleepwalking disorder, and thus was diagnosed as parasomnia overlap disorder (see Table 1).2 Two patients (#2 and #4) had associated Parkinson disease. All patients were previously treated with both clonazepam and melatonin to maximum tolerated doses; bed alarm therapy was then initiated after persistence of SRI (see individual patient narratives below).
Table 1.
RBD patient characteristics
| Patient |
||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Gender | F | M | F | M |
| Age | 87 | 61 | 62 | 70 |
| Previous medical therapy | ||||
| Clonazepam | + | + | + | + |
| Melatonin | + | + | + | + |
| Current medical therapy | ||||
| Clonazepam | + | + | – | + |
| Melatonin | – | + | + | + |
All patients demonstrated a reduction in SRI events and RBD symptoms after initiating bed alarm therapy (Tables 2 and 3). The strongest treatment responses were noted in the patients with the highest disease burden, especially patients #1 and #2. Patient # 1 reported complete elimination of SRI events despite a preceding history of at least weekly SRI events as well as 2 previous hospitalizations for SRI. Further, over 36 months of bed alarm treatment, she reported that the average monthly intervention dropped from 10/mo to 2/mo. Patient #2 also noted a striking reduction in SRI as well as a drop in the number of needed interventions after the first 3 months of usage (from 8/mo to 4/mo). Patients #3 and #4 also had an improvement in SRI, although the reductions were less striking (as they were having less frequent SRI events at baseline).
Table 3.
All events pre- and post- bed alarm treatment
| Pre-treatment | Post-treatment | |
|---|---|---|
| Serious Events | 5 in 5.5 pt-yr (0.91 events/pt-yr) | 0 in 5.25 pt-yr (0 events/pt-yr) |
| Minor Events | 80 in 66 pt-mo (1.21 events/pt-mo) | 0 in 63 pt-mo (0 Events/pt-mo) |
| Near Events | 193 in 66 pt-mo (2.92 events/pt-mo) | 3 in 63 pt-mo (0.05 Events/pt-mo) |
| All SRI Events | 278 in 66 pt-mo (4.21 events/pt-mo) | 3 in 63 pt-mo (0.05 Events/pt-mo) |
| Average RBDQ-HK score* | 68 (range 53-80) | 54 (range 42-65) |
| Bed alarm activations | NA | 176 in 63 pt-mo (2.79 activations/pt-mo) |
Not including pt #1 who did not have pretreatment data.
Combined patient data (Table 3) demonstrated a striking reduction in all SRI events after starting bed alarm treatment. There were a total of 176 bed alarm interventions over 63 pt-months (2.79 interventions/pt-mo), with a downward trend over time. SE fell from from 5 in 5.5 pt-yr (0.91 events/pt-yr) to 0 in 5.25 pt-yr (0 events/pt-yr). ME declined from 80 in 66 pt-mo (1.21 events/pt-mo) to 0 in 63 pt-mo (0 events/pt-mo). NE declined from 193 in 66 pt-mo (2.92 events/pt-mo) to 2 in 63 pt-mo (0.03 Events/pt-mo). Total events in aggregate fell from 278 in 66 pt-mo (4.21 events/pt-mo) to 2 in 63 pt-months (0.03 events/pt-mo). Generalized RBD symptoms improved as measured by RBDQ-HK (average pre-treatment score 68 [range: 53-80]; average post-treatment [range: 42-65]) with the most consistent improvement noted in the 3 questions related to SRI (Q9, Q10, Q11).
All 4 patients reported that the burden of bed alarm treatment was low and primarily related to convenience issues. No adverse effects were reported.
Patient #1
The index case was an 87-year-old female with a lifelong history of sleepwalking who had increasingly violent dream enactment with near nightly ME or NE for several years. This DEB became more consequential when she was started on anticoagulation therapy (Coumadin) and had 2 SE resulting in hospitalizations for ecchymosis extending over her trunk and extremities. After PSG confirmation of both a NREM and REM parasomnia, she was diagnosed with parasomnia overlap disorder. The need for anticoagulation therapy was reconsidered; however, Coumadin was continued. Over 3-year follow-up, she has not demonstrated evidence of parkinsonism or neurodegenerative disease.
Her response to medication was suboptimal. Despite a decrease in dream intensity with 1 mg of bedtime clonazepam, the patient continued to have at least weekly NEs during which she would suddenly exit the bed. Higher doses were not tolerated, as she had residual morning sleepiness with gait impairment. Multiple attempts of low-dose melatonin administration resulted in diarrhea within hours of administration.
The patient's family labored to improve the sleeping environment and reduce SRI. Potentially injurious objects were removed, and when events continued suggested that she begin sleeping in a tent. When family members slept in the same room they noted that DEB could be quickly halted with a calming phrase, in particular “wake up mom”. Because of this observation, an author (PA) customized a Posey Sitter Select bed alarm with the author's voice commanding the patient to “wake up.” When the batteries were replaced and the recording lost, the patient's son reset the command.
The effect of the bed alarm therapy was striking, with immediate and complete resolution of SRI events. The patient reported the bed alarm consistently wakes her in the act of attempting to exit the bed in the midst of clearly recalled dream scenarios. One compelling example involved a dream in which she was chasing a man who had stolen her purse. Once she had arisen, the alarm immediately oriented her and she lay back down. After initiating the intervention, family was able to successfully stop co-sleeping with the patient. The patient continued upon the maximum tolerated dose of 1 mg clonazepam. Prior to bed alarm treatment she was having frequent SRI events (SE = 2/yr; ME = 2/mo; NE = 8/mo). Impressively, there have been no reported events in the subsequent 36 months. Interestingly, after only 3 months she noted fewer bed alarm interventions and decreased anticipatory anxiety towards sleep and possible SRI. The patient described the experience as if a caring family member is watching over her while she is sleeping.
Patient #2
A 61-year-old male with Parkinson disease and RBD presented with increasing SRI. Originally clonazepam at 0.25-1 mg decreased the frequency and severity of events, but effectiveness decreased over time. On 2 occasions, he left the bed and attempted to thrust his head through the television. Patient underwent a PSG that demonstrated REM without atonia and dream enactment, as well as mild obstructive sleep apnea (AHI = 10). Despite resolution of sleep disordered breathing with a mandibular advancement device, REM without atonia and DEB persisted on repeat PSG. The patients gait and cognition deteriorated with dose > 1 mg of clonazepam. Melatonin administration > 4.5 mg led to complaints of nocturnal amnesia. Despite these interventions, the patient continued to have violent SRI, either leaving the bed or attacking his wife during DEB.
The patient's wife had discovered that calmly telling him to turn over would halt the behavior. The phrase also worked when non-family members spoke it to him during DEB. In particular, on a camping trip, his friends described resolution of agitated nocturnal behaviors once they instructed him to “turn over” (as suggested by his wife). The effectiveness of this intervention was confirmed when during a subsequent PSG, a recording from his wife immediately halted DEB.
The patient was so impressed by these results that he independently obtained a TABS bed exit monitor. After weekly SRI events (1 SE/yr, 2 ME/mo, and 6 NE/mo) he claims to have had only one NE in 15 months of follow-up. He reported several compelling anecdotes of the bed alarm preventing serious injury. One example involved acting out a scene from the animated film Toy Story 3, in which he dreamed he was choking an attacking character. He awoke after the bed alarm oriented him to find that he had wrapped his arms around his wife's neck. Despite repeated discussions and warnings, the patient's wife still slept in the same bed. His one breakthrough event occurred despite the bed alarm when he fled so quickly that the device did not wake him prior to hitting his head on the television without injury. As with patient #1, over time the bed alarm became activated less frequently and appears to have attenuated his anxiety about falling asleep. He describes great enthusiasm for the device and claims no burden of treatment.
Patient #3
Over 18 months, a 62-year-old female noted 20 NEs where she had left the bed or attacked her sleeping boyfriend, and she sustained a serious head injury due to DEB. These events lead to nocturnal anxiety about the potential for SRI, and despite several assaults the boyfriend refused to sleep in a separate bed.
The patient had comorbid RLS symptoms effectively treated with low-dose pramipexole without an improvement in DEB. PSG demonstrated REM without atonia with subtle dream enactment. The patient did not have parkinsonian tremor, bradykinesia, or cogwheeling rigidity; however, she described anosmia, suggesting the possibility of an early synucleinopathy.
Various treatments had failed to resolve the SRI events, which continued to occur at least monthly. She was started on clonazepam that was later stopped because residual morning sleepiness was noted even at low doses. Melatonin up to 6 mg was modestly effective at decreasing dream intensity, but at higher doses she paradoxically developed frightening nightmares.
The patient was initiated on a bed alarm, with her own voice instructing her to go back to sleep. After 6 months the patients describes her overall experience with the treatment as “excellent” without any breakthrough events as long as she is using the device at an adequate volume. One NE occurred while she was traveling and did not have the bed alarm. She awoke to realize she had started to strangle her boyfriend. Subsequently she claims to be using the device with near 100% compliance, even while traveling.
Patient #4
A 70 male with Parkinson disease and RBD presented with his wife to discuss intermittent but frightening SRI events. Examples included bruises on his hands and his wife's arms after violently striking out against presumed assailants. His wife subsequently slept in a separate room. Prior to bed alarm therapy the patient had been on high-dose melatonin (9-12 mg) and low-dose clonazepam (limited to 0.25 mg due to morning hypersomnolence and gait concerns) with continued SRI events (5 ME [0.17/mo] and 5 NE [0.17/mo]).
During the patient's PSG, increased phasic muscle activity was noted throughout REM sleep. He had one striking example of DEB, during which he lifted his arms and legs and subsequently made climbing motions while dreaming he was climbing a telephone pole. During the event the technologist played a recording of his wife's voice and the DEB was immediately halted (see pictures).
Over the 30 months prior to bed alarm treatment the patient had 5 ME (0.17/mo) and 5 NE (0.17/mo); he has not experienced any SRI events in the subsequent 6 months. He recalls the device halting one event in the first 3 months, but afterward it has not gone off during sleep. Admittedly, the device does not halt all potentially injurious behaviors, as he has frequent DEB while lying flat in bed (such as the event noted during his PSG). This has been addressed by removing injurious objects that he could potentially strike at from a lying position. The patient describes only a minimal burden of treatment; however, he admits to using it sporadically, as his SRI events are rare.
DISCUSSION
Medication refractory RBD is a daunting and potentially life-threatening condition with limited management options.3–5 This study demonstrates that a customized bed alarm augments pharmacological treatment in refractory cases and prevents SRI. No SE have occurred over 63 patient-months since starting bed alarm treatment. Not unexpectedly, as the device is designed to prevent exiting the bed, the greatest improvement was seen in the reduction of NE.
The patients described compelling examples of the device halting violent behavior before injury could occur (see above). All patients described a low burden of therapy, and at the end of 63 patient-months, they were all still using the device, although patient #4 was considering ceasing therapy. This response from patient #4 is not unexpected, as he had the lowest level of disease burden with only rare near events (0.17 per month) and thus far no serious events, suggesting that the ideal candidate is a patient with a high burden of disease with frequent serious or near events.
Interestingly, even though this treatment is designed to halt already established DEB, all four patients described a decrease in all DEB episodes and reported that the frequency of bed alarm activation decreased over time. Further, one patient (#2) noted such an impressive improvement that he voluntarily decreased his dosage of clonazepam without significant exacerbation of DEB or SRI. In addition to halting events that could lead to SRI, we speculate that a modified bed alarm decreases violent DEB in RBD by reducing nocturnal anxiety. Our cases demonstrate how an anticipatory anxiety towards sleep (bordering on “sleep phobia”) can result from recurrent SRI, associated with chronic RBD. This reasoning is echoed by all four patients, who prior to initiating treatment endorsed a fear of falling asleep that often exacerbated dream mentation.
The burdens of this treatment include unintentional alarm discharges, pressure pads that require changing (typically 3-6 months), and the need to re-record calming phrases when the batteries need replacing.
While the majority of RBD cases initially demonstrate a good clinical response to clonazepam, long-term follow-up studies demonstrate mixed outcomes, ranging from sustained benefit without dose escalation to the eventual need to consider alternative or augmenting therapies, as tolerance and treatment failures may occur.11,13,14,20 In one series, 58% of patients on clonazepam reported clinically significant adverse effects, with 50% either stopping the agent or reducing the dose.13
Other agents have been explored as potential RBD therapies however rigorous clinical trials are lacking. Reports have described limited success with carbamazepine, levodopa, pramipexole, donepezil, sodium oxybate, triazolam, zopiclone, quetiapine, and clozapine.6,13,15 The only agent that has been studied in a controlled, randomized, double-blind fashion is melatonin (see below).8,21
As RBD is a chronic disorder indicating impending neurodegeneration, it is imperative to develop alternative therapies that do not suppress the CNS. In addition to Parkinson disease, RBD is often the cardinal finding among patients with other synucleinopathies such as dementia with Lewy bodies and multiple system atrophy. RBD has also been reported among patients with spinal cerebellar ataxia-3, Alzheimer disease, Huntington disease, and amyotrophic lateral sclerosis.10,22 Benzodiazepines and other CNS suppressing agents are often poorly tolerated in these conditions, with increased cognitive impairment and falls.
Melatonin is an intriguing option in patients with neurodegenerative disease and was used in all four patients. Melatonin treatment in RBD suppresses, but does not eliminate, REM motor activity, and its effect persists for weeks even after the agent is discontinued.8 However, no agent, including melatonin, eliminates all REM motor activity or DEB; in our series SRI events persisted in all 3 cases in which melatonin was tolerated.
Despite apparent unconsciousness, the brain is readily responsive to the environment during REM sleep. Complex auditory sound processing, similar to wakefulness, occurs during REM sleep, and there is a lower threshold for reversibility to wakefulness with auditory stimuli17,23 compared to NREM. Further, it has been demonstrated that dream mentation can be altered by verbal stimulation, and in fact this strategy has been used to redirect patients from other REM pathologies such as nightmares.16,24,25
Conversely, NREM sleep is characterized by a higher arousal threshold and relatively diminished cognitive processing in response to external stimuli compared to REM sleep and wakefulness.26 Not unexpectedly, patients with parasomnias arising from NREM sleep (sleepwalking and confusional arousals) are often poorly responsive to external stimulation.27,28 In fact, auditory stimuli can precipitate NREM parasomnias, and attempts by family members to calm sleepwalkers often paradoxically exacerbate confusion and agitation.27–29
Thus we conclude that this therapy of RBD has strong biological plausibility that along with minimal safety concerns deserves careful clinical application and further investigation. Currently this treatment should be directed towards patients who are at high risk of arising and leaving the bed. Events that have occurred despite the bed alarm typically involve trashing and kicking events without a change in body position.
Since SRI is a predominant feature of RBD, a more quantifiable scale is needed to evaluate clinical interventions. This study demonstrates the utility of the Minnesota Parasomnia Injury Scale (MPIS) in classifying and measuring SRI for both patients and bed partners. The MPIS is particularly useful in combination with the RBDQ-HK, which measures broader RBD symptoms. A validation study of the MPIS is currently in progress. The RBDQ-HK is a validated instrument that includes SRI but without specifying event severity or enumerating frequency. The incidences of severe events—those most typically described in previous treatment studies—are not adequate, as their incidence even in severe RBD is rare. Thus the MPIS is particularly useful by addressing minor and near events that occur more often. The MPIS also helps characterize the nature of SRI, indentifies which patients sought medical attention, and describes the level of awareness of dream mentation. Future RBD therapeutic trials should quantify SRI as an outcome measure, and the MPIS represents a tool to evaluate these treatments.
Finally, case #1 is the second oldest reported case of RBD, and the oldest reported case of female RBD (87-year-old female).30 The oldest reported case involved an 88-year-old male with Alzheimer disease and rivastigmine-induced RBD.31 Also, case #1 demonstrates the importance of “host vulnerability factors” related to injuries resulting from RBD, as previously discussed in detail.5 Although all of our patients had anticipatory anxiety about sleeping and sustaining SRI, it is intriguing that in cases #2 and #3, the spouse/boyfriend continued to sleep in the same bed despite sustaining repeated blows from DEB (in contrast, the wife of patient #4 eventually slept in a separate room). This is an impressive and apparently common phenomenon previously described, in which the spouses of patients with vigorous and violent RBD adamantly continue to sleep in the same bed, reportedly out of care and concern for the patient with RBD.5
DISCLOSURE STATEMENT
This was not an industry supported study. Posey provided bed alarms to patients without charge. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was performed at the University of Minnesota Medical Center Sleep Disorders Center
Appendix. The Minnesota Parasomnia Injury Scale
REFERENCES
- 1.Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep. 1986;9:293–308. doi: 10.1093/sleep/9.2.293. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Sleep Medicine. International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd Edition ed. Westchester. IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 3.Schenck CH, Milner DM, Hurwitz TD, Bundlie SR, Mahowald MW. A polysomnographic and clinical report on sleep-related injury in 100 adult patients. Am J Psychiatry. 1989;146:1166–73. doi: 10.1176/ajp.146.9.1166. [DOI] [PubMed] [Google Scholar]
- 4.Schenck C. Paradox Lost: midnight in the battleground of sleep and dreams. Minneapolis: Extreme-Nights-LLC; 2006. [Google Scholar]
- 5.Schenck CH, Lee SA, Bornemann MA, Mahowald MW. Potentially lethal behaviors associated with rapid eye movement sleep behavior disorder: review of the literature and forensic implications. J Forensic Sci. 2009;54:1475–84. doi: 10.1111/j.1556-4029.2009.01163.x. [DOI] [PubMed] [Google Scholar]
- 6.Gagnon JF, Postuma RB, Montplaisir J. Update on the pharmacology of REM sleep behavior disorder. Neurology. 2006;67:742–7. doi: 10.1212/01.wnl.0000233926.47469.73. [DOI] [PubMed] [Google Scholar]
- 7.Boeve BF, Silber MH, Ferman TJ. Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: results in 14 patients. Sleep Med. 2003;4:281–4. doi: 10.1016/s1389-9457(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 8.Kunz D, Mahlberg R. A two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorder. J Sleep Res. 2010;19:591–6. doi: 10.1111/j.1365-2869.2010.00848.x. [DOI] [PubMed] [Google Scholar]
- 9.Schenck CH, Bundlie SR, Mahowald MW. Delayed emergence of a parkinsonian disorder in 38% of 29 older men initially diagnosed with idiopathic rapid eye movement sleep behaviour disorder. Neurology. 1996;46:388–93. doi: 10.1212/wnl.46.2.388. [DOI] [PubMed] [Google Scholar]
- 10.Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain. 2007;130:2770–88. doi: 10.1093/brain/awm056. [DOI] [PubMed] [Google Scholar]
- 11.Chouinard G. Issues in the clinical use of benzodiazepines: potency, withdrawal, and rebound. J Clin Psychiatry. 2004;65(S5):7–12. [PubMed] [Google Scholar]
- 12.Schuld A, Kraus T, Haack M, Hinze-Selch D, Pollmacher T. Obstructive sleep apnea syndrome induced by clonazepam in a narcoleptic patient with REM-sleep-behavior disorder. J Sleep Res. 1999;8:321–2. doi: 10.1046/j.1365-2869.1999.00162.x. [DOI] [PubMed] [Google Scholar]
- 13.Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med. 2009;5:235–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Schenck CH, Mahowald MW. Long-term, nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100:333–7. doi: 10.1016/S0002-9343(97)89493-4. [DOI] [PubMed] [Google Scholar]
- 15.Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD) J Clin Sleep Med. 2010;6:85–95. [PMC free article] [PubMed] [Google Scholar]
- 16.Hobson JA. REM sleep and dreaming: towards a theory of protoconsciousness. Nat Rev Neurosci. 2009;10:803–13. doi: 10.1038/nrn2716. [DOI] [PubMed] [Google Scholar]
- 17.Jones BE. Paradoxical sleep and its chemical/structural substrates in the brain. Neuroscience. 1991;40:637–56. doi: 10.1016/0306-4522(91)90002-6. [DOI] [PubMed] [Google Scholar]
- 18.Li SX, Wing YK, Lam SP, et al. Validation of a new REM sleep behavior disorder questionaire (RBDQ-HK) Sleep Med. 2010;11:43–8. doi: 10.1016/j.sleep.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 19.Boeve B, Silber M, Ferman T, Smith G. Validation of a questionnaire for the diagnosis of REM sleep behavior disorder. Sleep. 2002;25:A486. [Google Scholar]
- 20.Gugger JJ, Wagner ML. Rapid eye movement sleep behavior disorder. Ann Pharmacother. 2007;41:1833–41. doi: 10.1345/aph.1H587. [DOI] [PubMed] [Google Scholar]
- 21.Takeuchi N, Uchimura N, Hashizume Y, et al. Melatonin therapy for REM sleep behavior disorder. Psychiatry Clin Neurosci. 2001;55:267–9. doi: 10.1046/j.1440-1819.2001.00854.x. [DOI] [PubMed] [Google Scholar]
- 22.Boeve BF. REM sleep behavior disorder: Updated review of the core features, the REM sleep behavior disorder-neurodegenerative disease association, evolving concepts, controversies, and future directions. Ann N Y Acad Sci. 2010;1184:15–54. doi: 10.1111/j.1749-6632.2009.05115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Atienza M, Cantero JL. Complex sound processing during human REM sleep by recovering information from long-term memory as revealed by the mismatch negativity (MMN) Brain Res. 2001;901:151–60. doi: 10.1016/s0006-8993(01)02340-x. [DOI] [PubMed] [Google Scholar]
- 24.Voss U, Holzmann R, Tuin I, Hobson JA. Lucid dreaming: a state of consciousness with features of both waking and non-lucid dreaming. Sleep. 2009;32:1191–200. doi: 10.1093/sleep/32.9.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aurora RN, Zak RS, Auerbach SH, et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6:389–401. [PMC free article] [PubMed] [Google Scholar]
- 26.Busby KA, Mercier L, Pivik RT. Ontogenetic variations in auditory arousal threshold during sleep. Psychophysiology. 1994;31:182–8. doi: 10.1111/j.1469-8986.1994.tb01038.x. [DOI] [PubMed] [Google Scholar]
- 27.Wills L, Garcia J. Parasomnias: epidemiology and management. CNS Drugs. 2002;16:803–10. doi: 10.2165/00023210-200216120-00002. [DOI] [PubMed] [Google Scholar]
- 28.Kotagal S. Parasomnias in childhood. Sleep Med Rev. 2009;13:157–68. doi: 10.1016/j.smrv.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Pilon M, Montplaisir J, Zadra A. Precipitating factors of somnambulism: impact of sleep deprivation and forced arousals. Neurology. 2008;70:2284–90. doi: 10.1212/01.wnl.0000304082.49839.86. [DOI] [PubMed] [Google Scholar]
- 30.Bodkin CL, Schenck CH. Rapid eye movement sleep behavior disorder in women: relevance to general and specialty medical practice. J Womens Health (Larchmt) 2009;18:1955–63. doi: 10.1089/jwh.2008.1348. [DOI] [PubMed] [Google Scholar]
- 31.Yeh SB, Yeh PY, Schenck CH. Rivastigmine-induced REM sleep behavior disorder (RBD) in a 88-year-old man with Alzheimer's disease. J Clin Sleep Med. 2010;6:192–5. [PMC free article] [PubMed] [Google Scholar]