Abstract
Preeclampsia, a hypertensive disorder of pregnancy, affects 5–8% of women. Large studies demonstrate a strong association between preeclampsia and future cardiovascular disease. Despite cardiovascular disease being the leading cause of mortality for women, there has been little education for internal medicine physicians or obstetrician-gynecologists about this association, and published guidelines do not include preeclampsia as a risk factor for future cardiovascular disease. Therefore, women with a history of preeclampsia may not receive adequate risk reduction counseling for cardiovascular disease. It is unclear whether primary care physicians are aware of the association; thus, we sought to determine whether primary care providers at our institution were aware of preeclampsia’s association with future cardiovascular disease and whether they were providing appropriate counseling.
An anonymous on-line survey was sent to all internists and obstetrician-gynecologists at our hospital. Although most internists (95%) and obstetrician-gynecologists (70%) provide routine cardiovascular risk reduction counseling, a substantial proportion of them were unaware of any health risk associated with a history of preeclampsia. Many internists were unsure or did not know if preeclampsia is associated with ischemic heart disease (56%), stroke (48%) and decreased life expectancy (79%). The corresponding proportions for obstetrician-gynecologists were 23%, 38% and 77%. A majority of internists (88%) and obstetrician-gynecologists (79%) were incorrect about or unaware whether preeclampsia was included as a risk factor in the American Heart Association guidelines for prevention of ischemic heart disease. Only 9% of internists and 38% of obstetrician-gynecologists were providing cardiovascular risk reduction counseling to women with a history of preeclampsia.
Keywords: preeclampsia, cardiovascular disease, ischemic heart disease, stroke, primary prevention
INTRODUCTION
Preeclampsia is a hypertensive disorder of pregnancy that affects 5–8% of pregnant women and typically presents with proteinuria and hypertension; it is one of the leading causes of maternal and neonatal morbidity and mortality.1 Previously, preeclampsia was thought to be a condition confined to pregnancy that resolved with delivery of the placenta; however, recent large studies have demonstrated that preeclampsia has long-term associations with cardiovascular disease (CVD), cerebrovascular disease, renal disease and shorter life expectancy.2–6 The pathophysiology of preeclampsia is still being elucidated; yet, evidence supports the release of soluble proteins from the placenta that alter the angiogenic balance and cause systemic endothelial damage.7–9 This systemic endothelial damage seen in preeclampsia may be a precursor to vascular disease.10
CVD is the leading cause of mortality in women in the United States.11 Large cohort studies indicate that preeclampsia is a risk factor for CVD2–5, 12, 13 with up to an 8-fold increased risk compared to women with no history of preeclampsia.3 Using linked birth and medical registries in Norway, Irgens et al. found a significantly higher risk of CVD among women with a history of preterm preeclampsia, even when controlling for fetal growth restriction.3 A cohort study of 37,000 women in Israel found preeclampsia to be an independent risk factor for CVD mortality.2 A recent prospective study by Magnussen et al. which included 15,000 women and found that a history of hypertensive disorders in pregnancy was strongly associated with cardiovascular risk factors later in life13.
Together, this evidence suggests that a woman’s obstetrical history is an important part of her risk profile for future CVD. Recent studies have recommended that women with a history of preeclampsia be counseled regarding their increased risk for cardiovascular sequelae and be followed closely for modifiable cardiovascular risk factors.12, 13 However, the American Heart Association (AHA) currently does not include preeclampsia in the risk assessment guidelines for the primary prevention of CVD and stroke11. Furthermore, the American College of Obstetrics and Gynecology (ACOG) does not address the association between preeclampsia and future CVD1 and does not provide guidelines as to the proper counseling for these patients.
We hypothesized that providers who care for women with a history of preeclampsia have limited knowledge about its association with future CVD and that few provide risk reduction counseling to these high-risk women. We included internal medicine physicians (internists) and obstetricians/gynecologists (ob-gyns) in our study, because female patients typically present to these two types of providers for well-woman annual exams.14 The primary objective of this study was to assess physicians’ knowledge of the association between preeclampsia and future CVD. We also sought to examine whether this knowledge varied by physician specialty.
METHODS
Following institutional review board approval, a link to a web-based survey was sent electronically to all 295 resident and attending internists and 108 resident and attending ob-gyns at Beth Israel Deaconess Medical Center. The resident lists were created from the graduate medical education office for the academic year. The attendings included all faculty with admitting privileges in their respective departments. The survey responses were collected through an anonymous web-based program between March 1st and June 10th, 2009. One survey was created for each group of physicians; the surveys for internists and ob-gyns were the same with the exception of type of practice and one question on the ob-gyn survey that referred to the ACOG. The version of the survey distributed to the ob-gyns is included as Appendix 1.
The survey collected demographic and practice characteristics and assessed the physician’s knowledge of the association between preeclampsia and future CVD risk, specifically, the association with renal disease, stroke, ischemic heart disease, and hypertension as these outcomes were studied by other researchers in large cohort studies. The survey also included two outcomes, malignancy and liver disease, that are not associated with preeclampsia. Finally, the survey asked the provider about his or her typical counseling for cardiovascular risk reduction among women with a history of preeclampsia. This is the first known survey to assess this knowledge in these groups of providers.
Data are presented as proportions; comparisons between the two groups of providers were conducted with the chi-square or Fisher’s exact test as appropriate. All P values were two-sided, and values <0.05 were considered statistically significant.
RESULTS
One hundred eighteen internists and 53 ob-gyns completed the survey, yielding response rates of 40% and 49%, respectively. The demographic and practice characteristics of the respondents are shown in Table 1. The internists were more likely to be residents (P<0.0001) and, consequently, were more likely to have 5 or fewer years of clinical experience (P<0.0001) compared with the ob-gyns. The ob-gyns were less likely to have a substantial proportion of patients over 50 years of age (P<0.0001). Both groups of providers routinely counseled regarding Pap test screening.
Table 1.
Characteristics of respondents
| Characteristic | Internists | Obstetrician-Gynecologists | P Value |
|---|---|---|---|
| n=118 | n=53 | ||
| n (%) | n (%) | ||
| Level of training | <0.0001 | ||
| Resident | 85 (72) | 19 (36) | |
| Attending | 33 (28) | 34 (64) | |
| Years of experience | <0.0001 | ||
| ≤5 years | 101 (86) | 25 (47) | |
| >5 years | 17 (14) | 28 (53) | |
| Sex | <0.01 | ||
| Female | 70 (59) | 43 (81) | |
| Male | 48 (41) | 10 (19) | |
| Proportion of patients >50 years | <0.0001 | ||
| ≤10% | 18 (15) | 30 (57) | |
| 10 to <31% | 45 (38) | 16 (30) | |
| 31 to <51% | 24 (20) | 3 (6) | |
| ≥51% | 31 (26) | 4 (8) | |
| Performs routine counseling for Pap test surveillance | 0.24 | ||
| Yes | 115 (97) | 100 (100) | |
| No | 3 (3) | 0 (0) | |
| Performs routine counseling for cardiovascular disease risk reduction | <0.0001 | ||
| Yes | 112 (95) | 37 (70) | |
| No | 6 (5) | 16 (30) | |
| Includes preeclampsia in history | <0.0001 | ||
| Yes | 6 (5) | 22 (42) | |
| No | 112 (95) | 31 (58) |
Nearly all (95%) internists and 70% of ob-gyns routinely counseled patients on CVD risk reduction (P<0.0001); however, only 5% of internists and 42% of ob-gyns included preeclampsia as part of the medical history (P<0.0001), as shown in Table 1. Of these respondents, only a subset provided counseling specifically to those patients with a history of preeclampsia about the increased risk of CVD. Specifically, 9% of internists and 38% of ob-gyns counseled women with a history of preeclampsia regarding their increased CVD risk.
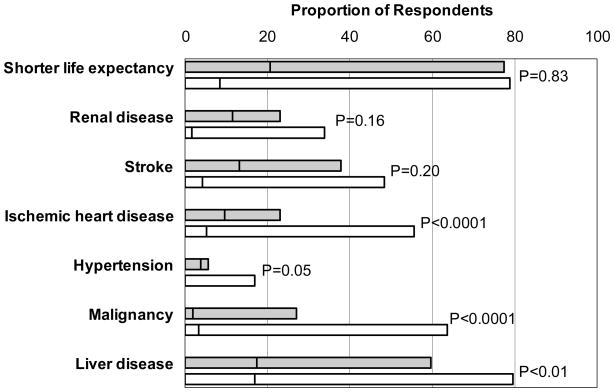
A majority of the physicians in either group were unaware of any association between preeclampsia and risk of future CVD. Figure 1 shows the proportions of internists and ob-gyns that were incorrect about or unsure whether there was an increased risk of the listed comorbidities following preeclampsia. In all instances, internists were more likely than ob-gyns to be incorrect or unsure about the risk following preeclampsia; however, some of these differences were not statistically significant. Fifty-six percent of internists and 23% of ob-gyns were incorrect or unsure about the increased risk of ischemic heart disease following preeclampsia (P<0.0001). Seventy-nine percent and 77% of internists and ob-gyns, respectively, were incorrect or unsure about the association of preeclampsia with shorter life expectancy. (P=0.83) With respect to stroke, 48% of the internists and 38% of the ob-gyns were incorrect or unaware of its association with prior preeclampsia (P=0.20). Although many internists (77%) were more likely than ob-gyns (62%) to be aware of the AHA guidelines for primary prevention of CVD and stroke (P=0.04), they were also more likely to be incorrect about or uncertain whether preeclampsia was included as a risk factor (88% for internist versus 79% for ob-gyns, P=0.13).
Figure 1.
Incorrect or unsure responses of physicians regarding future conditions associated with preeclampsia. All of the listed conditions are associated with preeclampsia with the exception of malignancy and liver disease. The grey bars represent the ob-gyns’ responses and the white bars represent the internists’ responses. The left segment of each bar is the unsure responses, and the right segment is the incorrect responses. The P values are for the comparison between internists and ob-gyns.
Conversely, the majority of providers were aware of the association between preeclampsia and future hypertension with only 6% of ob-gyns and 17% of internists being unsure or incorrect about this association.
DISCUSSION
Our results suggest that internists and ob-gyns have limited knowledge of the increased cardiovascular risks for women following preeclampsia. Up to 8% of parous women have a history of preeclampsia and therefore an increased risk for CVD. However, our study shows that few providers include preeclampsia in the medical history and even fewer counsel women with a history of preeclampsia regarding the increased risk of future CVD. While preeclampsia may provide an early window15 into a woman’s long-term risk of CVD, only a minority of providers recognize this opportunity for primary prevention and appropriately counsel these high-risk women.
Although most physicians were aware of an association between preeclampsia and future hypertension, these same physicians did not apply this knowledge to patient counseling as only 9% of internists and 38% of ob-gyns counseled women with a history of preeclampsia regarding their increased CVD risk. Nearly all internists and ob-gyns in our study provide preventative counseling on Pap test surveillance, and the majority reported providing CVD risk reduction counseling. However, our data indicate that physicians who routinely counsel for primary prevention of CVD are not well informed about the increased risk conferred by a history of preeclampsia. Thus, this increased risk is not assessed and the high-risk women with prior preeclampsia are not routinely counseled about their elevated risk of CVD.
While the precise pathophysiology of preeclampsia is not understood, large cohort studies2–5, 13 confirm the strong association with future CVD, stroke and renal disease, and there is evidence supporting a plausible biologic mechanism. The systemic endothelial damage caused by preeclampsia may indicate an underlying vascular condition that increases the risk for CVD or perhaps an unknown genetic predisposition for CVD first presenting during a woman’s pregnancy.
A history of preeclampsia identifies a group of women at higher risk of developing CVD. Although additional research is needed to determine whether specific cardio-protective interventions for women with a history of preeclampsia decrease morbidity, risk reduction counseling and close monitoring of modifiable risk factors such as cholesterol, hypertension and weight may reduce this group of women’s CVD risk. However, this risk reduction counseling can only occur if providers are aware of both the association and their patients’ obstetrical history.
Our results are similar to prior studies evaluating primary care providers’ knowledge of CVD prevention for women. A large study found that ob-gyns, internists and cardiologists assigned women to a lower-risk category than men with identical risk profiles.16 In this study, fewer than half of the providers counseled their patients about basic primary preventative measures to prevent CVD such as diet, exercise and weight loss. A minority of physicians knew that more women than men died of CVD annually.16 A study analyzing preventive services used by female patients found only 23% of women received counseling on diet and exercise.14 These studies, coupled with our findings, suggest that knowledge among primary care providers for primary prevention of CVD in women is limited.
In the United States, CVD remains the leading cause of death among women.11 There were 325 million primary care visits for women in this country in 200617 with each visit offering an opportunity for cardiovascular protection counseling. Successful adoption of practice guidelines has been correlated to physician awareness.16 The majority of internists and ob-gyns in this study were unaware of the positive correlation between preeclampsia and future CVD, cerebrovascular disease and renal disease, indicating that primary care providers may need more education about this association. The development of national guidelines may help physicians better identify and counsel this group of high-risk women.
Our study has a few limitations. One limitation is its potentially limited external validity given the large proportion of respondents who were residents. Though residents in a tertiary care center may have more didactic training and more exposure to recent clinical updates than the average primary care provider. Therefore, the percentage of providers knowledgeable about the association between preeclampsia and future CVD may be elevated compared to providers outside of an academic medical center. Ob-gyns demonstrated better knowledge of disease risks following preeclampsia and were more likely to obtain an obstetrical history that included preeclampsia. These findings may be secondary to more preeclampsia-related research and provider education in the department. In addition, respondents’ answers may have been influenced by how they suspected the authors wanted them to answer. Although we attempted to create questions that did not suggest a particular answer and asked about diseases unrelated to preeclampsia, we cannot eliminate this possibility. If this did occur, the level of knowledge demonstrated in our study may be artificially high.
In conclusion, this survey of internists and ob-gyns at an academic medical center indicates that knowledge about the association between preeclampsia and future CVD for women is deficient, thereby limiting the application of this risk factor to clinical care. Development of guidelines to assist providers in identifying and counseling women with a history of preeclampsia may help reduce CVD morbidity.
PERSPECTIVES
Large, well-designed cohort studies have definitively demonstrated a strong association between preeclampsia and future development of CVD, thus identifying preeclampsia as a new risk factor for CVD in women. This risk factor should be incorporated into national guidelines to assist primary care providers in tailoring risk reduction counseling and primary prevention for women who have an increased risk of CVD. Targeted risk reduction counseling and close monitoring of modifiable risk factors may prove beneficial in decreasing the impact of CVD for women with a history of preeclampsia; however, the necessary first step is improving provider education to increase their knowledge about this association.
Acknowledgments
We are grateful to Laura Dodge for her assistance with preparing and editing this manuscript. We thank Dr. John Yeh for his editing of the manuscript.
References
- 1.ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33. Obstet Gynecol. 2002 January;99(1):159–67. doi: 10.1016/s0029-7844(01)01747-1. [DOI] [PubMed] [Google Scholar]
- 2.Funai EF, Friedlander Y, Paltiel O, Tiram E, Xue X, Deutsch L, et al. Long-term mortality after preeclampsia. Epidemiology. 2005;16(2):206–15. doi: 10.1097/01.ede.0000152912.02042.cd. [DOI] [PubMed] [Google Scholar]
- 3.Irgens HU, Reisaeter L, Irgens LM, Lie RT. Long term mortality of mothers and fathers after pre-eclampsia: population based cohort study. BMJ. 2001;323(7323):1213–7. doi: 10.1136/bmj.323.7323.1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet. 2005;366(9499):1797–803. doi: 10.1016/S0140-6736(05)67726-4. [DOI] [PubMed] [Google Scholar]
- 5.Smith GC, Pell JP, Walsh D. Pregnancy complications and maternal risk of ischaemic heart disease: a retrospective cohort study of 129,290 births. Lancet. 2001;357(9273):2002–6. doi: 10.1016/S0140-6736(00)05112-6. [DOI] [PubMed] [Google Scholar]
- 6.Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359(8):800–9. doi: 10.1056/NEJMoa0706790. [DOI] [PubMed] [Google Scholar]
- 7.Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350(7):672–83. doi: 10.1056/NEJMoa031884. [DOI] [PubMed] [Google Scholar]
- 8.Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355(10):992–1005. doi: 10.1056/NEJMoa055352. [DOI] [PubMed] [Google Scholar]
- 9.Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003;111(5):649–58. doi: 10.1172/JCI17189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts JM, Taylor RN, Musci TJ, Rodgers GM, Hubel CA, McLaughlin MK. Preeclampsia: an endothelial cell disorder. Am J Obstet Gynecol. 1989;161(5):1200–4. doi: 10.1016/0002-9378(89)90665-0. [DOI] [PubMed] [Google Scholar]
- 11.Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115(11):1481–501. doi: 10.1161/CIRCULATIONAHA.107.181546. [DOI] [PubMed] [Google Scholar]
- 12.Craici I, Wagner S, Garovic VD. Preeclampsia and future cardiovascular risk: formal risk factor or failed stress test? Ther Adv Cardiovasc Dis. 2008;2(4):249–59. doi: 10.1177/1753944708094227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magnussen EVL, Smith GD, Romundstad PR. Hypertensive disorders in pregnancy and subsequently measured cardiovascular risk factors. Obstet Gynecol. 2009;114(5):961–970. doi: 10.1097/AOG.0b013e3181bb0dfc. [DOI] [PubMed] [Google Scholar]
- 14.Lewis BG, Halm EA, Marcus SM, Korenstein D, Federman AD. Preventive services use among women seen by gynecologists, general medical physicians, or both. Obstet Gynecol. 2008;111(4):945–52. doi: 10.1097/AOG.0b013e318169ce3e. [DOI] [PubMed] [Google Scholar]
- 15.Saade G. Pregnancy as a window to future health. Obstet Gynecol. 2009;114(5):958–9. doi: 10.1097/AOG.0b013e3181bf5588. [DOI] [PubMed] [Google Scholar]
- 16.Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111(4):499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- 17.Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2006. Natl Health Stat Report. 2008;(8):1–29. [PubMed] [Google Scholar]