Abstract
Intimate partner violence and abuse (IPV/A) have been shown to have a major impact on mental health functioning. This study assessed the longitudinal association between recent IPV/A and depressive symptoms in order to identify potential targets for preventive interventions for women. Random effects models were used to examine four waves of data collected at 6-month intervals from a cohort of 1438 female healthcare workers. Recent IPV/A (e.g., sexual and physical violence, psychological abuse) in the past 5 years was associated with higher CES-D 10 scores across 4 waves after adjustment for age, time, marital status, and childhood trauma. Women who reported IPV/A in the past 5 years had higher CES-D 10 scores (β 1.31, 95% CI .79-1.82, p<.0001) than non-abused women. This association was generally constant with time, suggestive of a cross-sectional association across all four waves of data. Additionally, recent IPV/A was associated with change in depressive symptoms over time among the full cohort and those with CES-D 10 scores below 10 (the threshold for likely depression) at baseline. Recent IPV/A was independently associated with depressive symptoms both cross-sectionally and longitudinally. The longitudinal association was stronger among those not depressed at baseline. Implications for healthcare settings and workplace policies addressing IPV/A are discussed.
Introduction
Violence within the context of a romantic relationship is a national and international public health concern. Intimate partner violence and abuse (IPV/A) describes a broad range of abusive behaviors within adult relationships, including physical and/or sexual harm involving the use of force, as well as psychological abuse directed toward current or former romantic partners (Jewkes, 2002; Krantz & Garcia-Moreno, 2005). Nearly 5.3 million women in the U.S. are victims of IPV/A each year (Tjaden & Thoennes, 2000). The gender differences in perpetration and victimization with regard to context, severity, and differential psychological outcomes prompt the focus of the majority of extant literature to be on the female experience of IPV/A. The present study examines the association between recent IPV/A and depressive symptoms over time among female healthcare workers.
The negative effects of violence against women on mental health have been widely described (Bonomi et al., 2006; J. Campbell et al., 2002; Plichta, 2004), and research on the impact of IPV/A on interpersonal and professional relationships is growing. Depression, post traumatic stress disorder, suicidality, and substance use are serious psychiatric consequences of IPV/A, existing as independent or comorbid conditions (Coker et al., 2002; Coker, Weston, Creson, Justice, & Blakeney, 2005; Golding, 1999; Nixon, Resick, & Nishith, 2004; Pico-Alfonso et al., 2006). Depression and depressive symptoms are especially prevalent among abused women, particularly among women with histories of both IPV/A and childhood trauma (Fogarty, Fredman, Heeren, & Liebschutz, 2008). Recent research also suggests that the association between violence victimization on health and occupational outcomes (e.g., employment stability) may be partially mediated through elevated depressive symptoms (Crowne et al., 2011).
Major depression is a complex, multifactorial disorder, with a lifetime prevalence of 20% for U.S. women compared to only 13% of men.(Kessler, 2003) Risk factors and correlates for major depression include age, socioeconomic status (Nolen-Hoeksema, 1990; Turner & Lloyd, 1999), marital status and quality, and childhood trauma in the form of physical and/or sexual abuse (J. C. Campbell, 2002; Golding, 1999; Kendler, Hettema, Butera, Gardner, & Prescott, 2003; Kendler, Kuhn, & Prescott, 2004; Nixon, et al., 2004; Widom, DuMont, & Czaja, 2007). The clinical diagnosis of major depression depends upon the presence of a number of potential predisposing factors, and these depressive symptoms are associated with an increased risk of first-onset major depression in adults (Horwath, Johnson, Klerman, & Weissman, 1992). Recent work suggests that depressive symptoms have a stable course over time (Minor, Champion, & Gotlib, 2005; Tram & Cole, 2006); however, major depression is also particularly sensitive to recent stressful life events, including exposure to violence (J. Campbell, et al., 2002; Golding, 1999; Nixon, et al., 2004).
Although there is an ample literature attesting to the strong positive association between violence victimization and depressive symptoms, an over-reliance on cross-sectional data may mask the temporality and change over time in this relationship. The association between IPV/A and depressive symptoms has not been well investigated, especially among employed women from a full range of economic and educational resources.
Most previous studies have explored the impact of IPV/A on depressive symptoms over time using clinic-based samples of women leaving the violent relationship or using shelter services (Anderson & Saunders, 2003; Kernic, Holt, Stoner, Wolf, & Rivara, 2003). Little is known about its effect on depressive symptoms in the broader population context. Longitudinal studies are needed to determine if IPV/A alters the pattern of depressive symptoms over time. To fill these gaps, the current study examines the influence of recent IPV/A on change in depressive symptoms using models that account for confounders and the temporal nesting of observations. Because the presence of participants clinically depressed at baseline may bias inferences toward the null, preplanned sensitivity analyses will evaluate this association after removing participants with elevated depressive symptoms at baseline. This a priori decision to exclude prevalent cases of depression at baseline helps to clarify temporal ordering of exposure and outcome to better detect the longitudinal effect of IPV/A on depressive symptoms among those for whom the violence-depression relationship has not yet played out. In this study, we evaluate the hypothesis that recent IPV/A is associated with elevated depressive symptoms in a cohort of female healthcare workers.
Methods
Analytical sample
This study examined the longitudinal influence of experiences of violence on depressive symptoms among a cohort of female healthcare workers. Data were collected from 2007-2009 as part of the Safe at Work study, a nested case-control study of experiences of IPV/A, workplace violence, and health outcomes among a cohort of nursing staff employed at three hospitals in the Baltimore, Maryland, U.S.A. area. The Institutional Review Board at Johns Hopkins University approved this study, and written consent was obtained from all participants.
Study participants were recruited via flyers posted in their hospital and electronic communication to complete a confidential, Internet-based (90%) or paper (10%) survey on their experiences in the workplace. Participants were eligible if they were English speaking, at least 18 years of age, and had been employed at their present hospital for at least 4 weeks prior to baseline assessment. Of the eligible 4165 hospital employees, baseline assessments of violence victimization, occupational outcomes, socio-demographic characteristics, and physical and mental health status were completed by 2166 employees (52% response rate). A subset of 1690 participants was selected at random for follow up using a random number generator, including all respondents who reported experiencing physical or psychological WPV (N=652) and a random sample of respondents who did not report experiencing WPV (N=1038). Men were excluded from the primary analyses due to insufficient representation (<10%) with which to make reasonable inference. Available data consisted of baseline (T1) and three separate, follow-up assessments at 6-month intervals, T2, T3, and T4 respectively. Although the study maintained a 70% retention rate throughout 4 waves, additional retention criteria were introduced at the variable level. Participants who completed the baseline interview but who were not selected for follow-up (i.e., missing by design) were excluded from the analyses, resulting in a final sample size of n= 1438. Additional details on sample selection are available elsewhere (Bracken, Messing, Campbell, La Flair, & Kub, 2010).
Measures
Outcomes
Depressive symptoms experienced in the past week were measured using the Center for Epidemiologic Studies Depression Scale short form (CES-D 10), a 10-item screening questionnaire. This brief scale taps similar depression symptom domains as the full-length 20-item original CES-D, including depressed mood, feelings of helplessness and hopelessness, psychomotor retardation, and sleep disturbance. The CES-D 10 has not yet been validated with a gold standard diagnostic interview, but when using a cut-off score of 10, it has sensitivity and specificity of 96% and 100%, respectively, when compared with the original CES-D 20 (E.M. Andresen, J.A. Malmgren, W.B. Carter, & D.L. Patrick, 1994). The 10 items were scored on a standard 4-point Likert scale of a potential range of 0 to 30, with higher number indicating severity of depressive symptoms. While cut-off scores of 16 and 28 indicate significant and severe depressive symptoms, respectively, in the CES-D 20, the corresponding thresholds in the CES-D 10 are 10 (significant) and 15 (severe) (Kilbourne et al., 2002; Swenson, Rose, Vittinghoff, Stewart, & Schillinger, 2008). The internal consistency of the CES-D 10 in this cohort was .86.
Predictors
IPV/A was assessed using an adaptation of the Abuse Assessment Screen (AAS) reflecting the Centers for Disease Control and Prevention definitions of IPV/A (Saltzman, 2002). The AAS is both a reliable and valid measure of detecting partner abuse (Soeken, Parker, McFarlane, & Lominak, 1998). Four questions were asked of the participant at T1 to assess IPV/A: (1) Have you ever been physically assaulted, sexually assaulted, threatened with physical or sexual assault or stalked by a former or current intimate partner? (2) Have you been hit, slapped, kicked, pushed, or otherwise physically hurt by a former or current intimate partner? (3) As an adult, have you ever been forced into sexual activities by a former or current intimate partner? (4) As an adult, have you ever been emotionally abused or sexually harassed by a former or current intimate partner? Respondents who answered in the affirmative to any one of the four questions within the past 5 years were considered to have experienced IPV/A.
Childhood trauma was ascertained with three questions: (1) As a child, were you ever physically abused (spanked a lot, whipped, hit with objects, etc.) by a parent or another adult or caretaker? (physical abuse) (2) As a child, did anyone ever touch you in a way you did not wish to be touched, or force you into any kind of sexual activity? (sexual abuse), and (3) While you were growing up, was your parent or guardian physically abused by his or her partner? (child witness to IPV/A). Responses to each were coded as dichotomous variables.
Covariates
Age was centered at the mean age for females (39.1); marital status was dichotomized into married or coupled (“1”) and neither married nor currently in a relationship (“0”); race/ethnicity categories were collapsed into Black (“1”) and non-Black (“0”). Time was measured in one-month increments since the baseline interview.
Analyses
Descriptive statistics were calculated on baseline data; t-tests and chi-square tests were used to evaluate mean differences and associations between categorical variables, respectively. Demographic characteristics are displayed in Table 1. All statistical analyses in this study were conducted using SAS, Version 9.1.
Table 1.
Baseline demographic information by violence victimization status
| Full cohort (n=1438) | IPV/A (past 5 years) (n=106) | No IPV/A (n=1332) | χ 2 | p-value | |
|---|---|---|---|---|---|
| Age, M (s.d.) | 38.3 (11.3) | 34.2 (9.8) | 38.6 (11.3) | <.001 | |
| Race/ethnicity, (%) | 5.72 | 0.22 | |||
| White | 873 (61.7) | 63 (60.6) | 810 (61.8) | ||
| Black | 339 (24.0) | 32 (30.8) | 307 (23.4) | ||
| Asian | 132 (9.3) | 7 (6.7) | 125 (9.5) | ||
| Latina | 29 (2.1) | 0 | 29 (2.2) | ||
| Other | 42 (3.0) | 2 (1.9) | 40 (3.1) | ||
| Marital Status, (%) | 22.4 | <.0001 | |||
| Married/Coupled | 802 (56.5) | 38 (36.5) | 764 (58.1) | ||
| Previously Married | 195 (13.7) | 27 (26.0) | 168 (12.8) | ||
| Never Married | 422 (29.7) | 39 (37.5) | 383 (29.1) | ||
| Childhood Abuse | |||||
| Physical | 265 (18.5) | 35 (33.0) | 230 (17.3) | 16.1 | <.0001 |
| Sexual | 254 (17.7) | 29 (27.6) | 225 (17.0) | 7.58 | 0.009 |
| Witness to IPV | 155 (10.8) | 20 (18.9) | 135 (10.2) | 7.67 | 0.006 |
| Children at home | 716 (50.3) | 54 (51.4) | 662 (50.2) | 0.06 | 0.8 |
| Education | 14.6 | 0.06 | |||
| High school/less | 148 (10.8) | 17 (16.2) | 131 (10.0) | ||
| Post h.s. certificate | 47 (3.3) | 5 (4.8) | 42 (3.2) | ||
| 2 years of college | 320 (22.5) | 33 (31.4) | 287 (21.8) | ||
| 4+ years of college | 902 (63.4) | 49 (46.7) | 853 (64.8) | ||
| Income ($) | 22.8 | <.0001 | |||
| <10,000-29,999 | 155 (11.1) | 20 (18.9) | 135 (10.5) | ||
| 30,000-59,999 | 300 (21.5) | 36 (34.0) | 264 (20.5) | ||
| 60,000-99,999 | 507 (36.4) | 32 (30.2) | 475 (36.9) | ||
| > 100,000 | 431 (30.9) | 18 (17.0) | 413 (32.1) | ||
| Registered Nurse, (%) | 1089 (75.8) | 65 (61.3) | 1024 (76.9) | 13 | <.001 |
Random effects (RE) regression modeling was used to examine the association between IPV/A and CES-D 10 scores across T1-T4 while accounting for temporal nesting of observations within persons and partitioning the variance into between-person and within-person components (Singer & Willet, 2003). A series of multilevel growth models of CES-D 10 score were fitted using SAS PROC MIXED with a maximum likelihood estimator. We first modeled an unconditional growth model of CES-D 10 score and time, allowing the intercept to vary by individual but modeling time as both and a fixed and a random effect. A time-squared parameter was included to account for the curvilinear pattern of change in CES-D 10 score over time; this became the base model for subsequent explorations. We then introduced the main effect of IPV/A exposure on CES-D 10 score (Model 1), followed by a set of potential confounders hypothesized to influence the relationship between violence victimization anddepressive symptoms, including age, childhood trauma, having children in the home, marital status, and race/ethnic group (Models 2-3). The final step was to include an interaction term between IPV/A exposure and time, testing the true longitudinal hypothesis that violence exposure at T1 independently affects the slope of CES-D 10 score (Model 4). All models were full nested, and we maintained all control variables according to theoretical support for their inclusion. By way of sensitivity analyses, the same models were re-estimated using only those female participants with baseline CES-D 10 scores below 10, a threshold value above which likely indicates depression.(E. M. Andresen, J. A. Malmgren, W. B. Carter, & D. L. Patrick, 1994) This permitted us to test our hypotheses among participants for whom the violence-depression relationship has not yet been pronounced. Of the 1438 participants completing the baseline assessment, 301 had CES-D 10 scores of 10 or higher and subsequently were removed from this portion of the analyses.
Results
Table 1 reports the results of the descriptive and bivariate analyses for the key study variables. Victimized and non-victimized women did not differ significantly in terms of race, education, and children living in the home. In contrast, significant differences were observed with regard to marital status, age, income, and childhood trauma. CES-D 10 scores ranged from 0 to 25, and the mean at T1 was 6.01. CES-D 10 scores were moderately correlated with each other across all 4 waves in an autoregressive manner (Cronbach α = 0.86). Women with a history of IPV/A or childhood trauma had significantly higher mean CES-D 10 scores than non-victimized women. Age and marital status were inversely associated with CES-D 10, while race, income, and having a child living at home were not significantly associated with depressive symptoms.
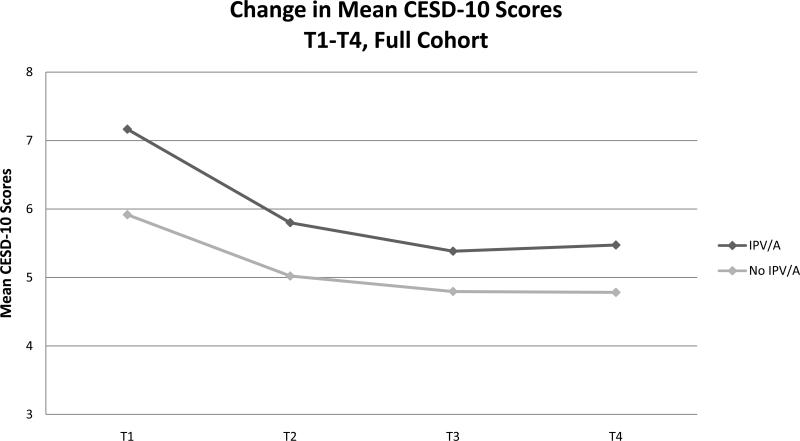
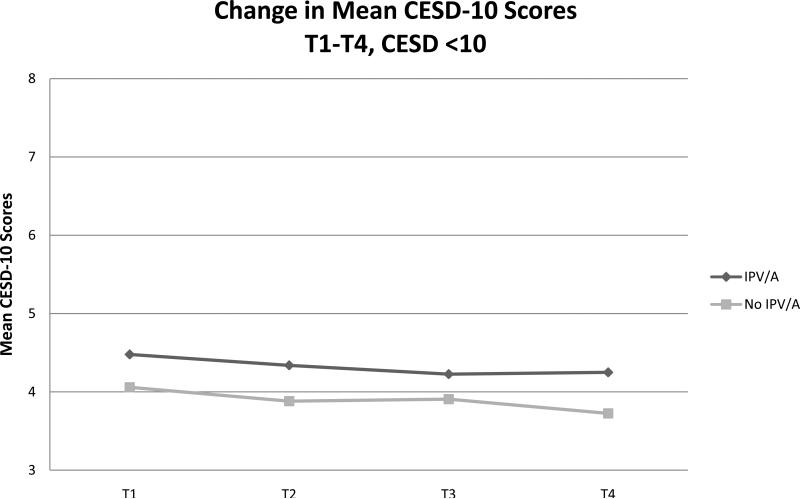
Figure 1a. shows the mean change in CES-D 10 scores by IPV/A status among all female participants. In the full cohort (n=1438), average depression scores declined over time regardless of exposure to violence, but abused women had steady high scores across the 2 years of data collection compared to non-abused women. Figure 1b. shows the mean change in CES-D 10 scores among women meeting study criteria with CES-D 10 scores below 10 at T1 (n=1137). Similar to the full cohort, this subset of abused women also has consistently higher CES-D 10 scores than their non-abused counterparts, but their symptoms remit at a slower rate.
Figure 1a.
Change in mean CESD-10 by violence victimization status among full cohort, n=1438
Figure 1b.
Change in mean CESD-10 by violence victimization status among women with CESD-10 <10, n=1137
Table 2 presents results from a series of RE regression models investigating the association between recent IPV/A and depressive symptoms across the 4 waves. In Model 1, IPV/A was associated with a 1.47 unit increase in CES-D 10 score (p<.0001). Potential confounders were added in Model 2, and the association between IPV/A and depressive symptoms remained significant after adjusting for age and marital status. Specifically, women experiencing recent IPV/A had increased CES-D 10 scores (1.39, 95% CI .87-1.91, p<.001) compared to non-abused women. After adjusting for childhood trauma plus age and marital status, the effect of IPV/A on CES-D 10 score remained positive and significant, and a modest 5.4% decrease in CES-D 10 score was observed (Model 3).
Table 2.
Nested random effects models of CESD-10 and Recent Intimate Partner Violence/Abuse among All Female Participants (n=1438)a
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Fixed effects | β (SE) | β (SE) | β (SE) | β (SE) |
| Intercept | 5.86 (.12)*** | 5.50 (.14)*** | 5.86 (.18)*** | 5.90 (.19)*** |
| Intimate Partner Violence /Abuse |
1.47 (.24)*** | 1.39 (.26)*** | 1.31 (.26)*** | .65 (.39) |
| Time in months | -.15 (.02)*** | -.16 (.02)*** | -.16 (.02)*** | -.16 (.02)*** |
| Time squared | .005 (.001)*** | .006 (.001)*** | .006 (.001)*** | .006 (.001)*** |
| Age in yearsb | -.02 (.01) | -.02 (.01)** | -.02 (.009)** | |
| Marital Statusc | -.89 (.22)*** | -.80 (.22)*** | -.80 (.19)*** | |
| Child Sexual Abuse | 1.02 (.31)*** | 1.02 (.31)** | ||
| Child Physical Abuse | 1.04 (.31)*** | 1.05 (.30)** | ||
| Child Witness to IPV | .87 (.38)* | .86 (.37)* | ||
| Time X Intimate Partner Violence /Abuse |
.08 (.03)* | |||
| -2LL | 25336.7 | 24297.4 | 24032.2 | 24025.4 |
Only fixed effects are shown, although random effects were fitted for both intercept and time.
Age is centered at the mean age in years for females (39.1)
Marital status is a binary variable of married/coupled vs. unmarried or uncoupled.
p<.05.
p<.01.
p<.001
Model 4 included an interaction term of IPV/A and time, thereby testing the hypothesized longitudinal association between recent IPV/A and the rate of change in CES-D 10 score. The significant IPV/A by time interaction term indicates that IPV/A influenced the trajectory of depressive symptoms over time (β=.08, p=.03). However, this addition did not result in an improvement in observed model fit for this model (df = 3, χ2 = .08).
The same RE models were refitted after excluding female participants with baseline CES-D 10 scores above 10 from the analysis (see Table 3). Models 1-4 resulted in similar conclusions as the full cohort except that the random effect of time was unsupported by model fit indices; therefore, the base model included only a fixed effect of time. Although the main effect of IPV/A remained positive and significant across models, a one-third reduction in strength of association between IPV/A and depressive symptoms was observed in this subset of women. In Models 3 and 4, only childhood sexual abuse remained (marginally) significant after removing those with elevated depressive symptoms from analysis, indicating a possible carry-over effect on depressive symptoms from childhood trauma in analyses with the full cohort. Model 4 included the time by IPV/A interaction, again testing the hypothesis that the CES-D 10 slope changed as a function of IPV/A experience. Whereas previous models have assumed fixed slopes, the significant IPV/A by time interaction term, after accounting for age, childhood trauma, and marital status, provided support for the true longitudinal influence of violence exposure on depressive symptoms(β=.10, p=.006). The IPV/A by time effect observed in the full cohort was amplified after removing individuals with elevated depressive symptoms at baseline from analysis. These results corroborate the relationships observed in Figures 1a and 1b.
Table 3.
Nested random effects models of CESD-10 and Recent Intimate Partner Violence/Abuse among Female Participants with Baseline CESD-10 Score < 10 (n=1137)a
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Fixed effects | β (SE) | β (SE) | β (SE) | β (SE) |
| Intercept | 3.99 (.08)*** | 4.38 (.13)*** | 4.22 (.13)*** | 4.26 (.12)*** |
| Intimate Partner Violence /Abuse |
.98 (.26)*** | .89 (.26)*** | .85 (.26)*** | (.34) |
| Time in months | -.008 (.006) | -.008 (.006) | -.008 (.006) | -.013 (.006)* |
| Age in yearsb | -.02 (.007)*** | -.02 (.007)*** | -.02 (.007)*** | |
| Marital Statusc | -.61 (.16)*** | -.58 (.16)*** | -.59 (.16)*** | |
| Child Sexual Abuse | .47 (.23)* | .49 (.23)* | ||
| Child Physical Abuse | .30 (.23) | .32 (.23) | ||
| Child Witness to IPV | .35 (.31) | .35 (.31) | ||
| Time X Intimate Partner Violence /Abuse |
.10 (.04)** | |||
| -2LL | 18335.3 | 17644.2 | 17538.6 | 17527.1 |
Only fixed effects are shown, although random effects were fitted for both intercept and time.
Age is centered at the mean age in years for females (39.1)
Marital status is a binary variable of married/coupled vs. unmarried or uncoupled.
p<.05.
p<.01.
p<.001
Discussion
The results of the present study substantiate an independent and consistent association between recent exposure to violence and abuse by an intimate partner on depressive symptoms over a two-year period while accounting for various forms of childhood trauma and previous elevated depressive symptoms. Our main finding is a clear cross-sectional association between IPV/A in the last 5 years and depressive symptoms in this cohort of women. The results also support a moderate, longitudinal association between IPV/A and change in depressive symptoms.
The analyses in this paper were presented in two ways: among the full cohort of women, and among a subset of women with depressive symptoms below threshold at baseline. The relative stability of the depressive construct over time is observed among the full cohort. When women with depressive symptoms above threshold at baseline were excluded, the slope of depressive symptoms remains stable in a manner consistent with a kindling effect, suggesting that women experiencing multiple previous episodes of major depression are less sensitized to the effects of stressful life events than women with fewer depressive episodes (Kendler, Thornton, & Gardner, 2000). This stability of elevated depressive symptoms over time has been noted in other research with women experiencing significant life stress (Carter, Martinez-Pedraza Fde, & Gray, 2009). Women who have experienced recent IPV/A not only have consistently higher CES-D 10 scores than their non-abused counterparts, but also their symptoms appear to remit at a slower rate.
There are several strengths to note in this study. For example, the longitudinal design permits analysis of changes within individuals over time and differences among individuals in their baseline level. The web-based administration of the baseline and follow-up questionnaires is an additional strength of this research as it provided a means for participants to complete the survey at work rather than at home where an abusive partner might be present. Also, RE modeling permitted a longitudinal examination of this relationship while accounting for serial correlation of measurements within individuals.
The results of these analyses should be interpreted with respect to several limitations. The CES-D 10 has been shown to be a valid method for assessing depressive symptoms; however, it is subject to criticism as to whether or not the imposed cutpoint successfully reflects the severity, chronicity, and level of impairment that might otherwise be captured with a diagnostic instrument. Similarly, the use of an adapted screening tool as a broad measure of IPV/A did not permit examination of changes in type and severity of abuse over time. Another limitation to these analyses is the lack of information about the quality of the relationship to the perpetrator and whether or not the relationship is ongoing since the baseline interview. Trauma symptoms may dissipate with time, but psychological outcomes may vary according to recency of separation (Anderson & Saunders, 2003). Several studies point to the eventual amelioration of mental health difficulties, including depression, after leaving an abusive partner (Kernic, et al., 2003; Mertin & Mohr, 2001). However, secondary stressors co-occurring with IPV/A may continue to contribute to a depressed state (e.g., financial losses, childcare, shifting social support). The extent to which current, elevated depressive symptoms may detain an abuse victim from exiting the relationship is an area of future research. Although the study is large, all of the participants are employed within one particular health care system, and thus, are not representative of the entire population of victims of violence. However, the prevalence of lifetime IPV and IPA in this cohort of female nursing staff (25.24% and 22.87%, respectively) was similar to that reported by women in population-based studies (Bracken, et al., 2010). Lastly, the study's 52% response rate raises concern about comparability between respondents and non-respondents. Although the data for such direct comparison is unavailable, we can make comparisons between participants in the Safe at Work Study and participants in similar research. Safe at Work Study participants attained a higher education level, and were younger in age and more ethnically diverse than their regional and national counterparts, as previously described elsewhere (J. C. Campbell et al., 2011).
Although the longitudinal study design enabled us to explore the temporal ordering of exposure to violence and depressive symptoms, we cannot infer causality regarding this association. Since the sample included individuals who were and were not exposed to IPV/A at baseline, we are unable to determine whether new exposure of IPV/A was associated with the changes in depressive symptoms over time. As a result, we conducted an additional set of sensitivity analyses (not reported) in which we restricted our sample participants who had not experienced IPV/A at baseline (n=944 and found a similar pattern of findings, whereby a general consistency in strength of association between IPV/A and depressive symptoms was observed in spite of the loss of power.
There are several future research questions which can be examined to better understand the association between IPV/A and major depression. For example, the specific form of IPV/A (physical, sexual, psychological) or its severity may be associated with a particular pattern of depressive symptoms. Similarly, the timing of exposure to IPV/A may be critical to understanding its relationship to depressive symptoms. The present study lacks the granularity to capture the exact timing of IPV or clinically significant depressive symptoms. Future work would benefit from studies that can measure more precisely timing of exposure and onset of major depression.
The results from this study have implications which span interpersonal and professional domains. Depressive symptoms and other psychiatric issues may impair a woman's ability to leave an abusive partner, thereby placing her at risk for continued victimization (Barnett, 2001). While recent attention has been given to the occupational and health consequences of workplace violence for nursing staff, few studies have investigated the impact of violence occurring outside the hospital. This study adds to the mounting evidence that employed, healthcare professionals are not immune from psychiatric distress resulting from violence and abuse by an intimate partner. The effect of depressive symptoms and violence in this group of healthcare workers is of particular concern. The consequences of IPV/A among healthcare staff and its implications for job performance and health are numerous, including absenteeism, quality of patient care, and workplace violence perpetrated by an intimate partner (Bracken, et al., 2010). As cessation of IPV/A may result in a decrease in depressive symptoms, employers are encouraged to review policies to help women identify supportive resources, including those to help them transition out of an abusive relationship if that is their desired goal (Gielen et al., 2000; Kernic, et al., 2003). Taken together, the results of this study emphasize the importance of addressing depressive symptoms among female healthcare workers, particularly recently victimized women. Possible targets for such intervention include working conditions or community characteristics such as workplace inequality, neighborhood monitoring, social attributes, and communication networks (O'Campo, Burke, Peak, McDonnell, & Gielen, 2005; O'Campo, Eaton, & Muntaner, 2004). Institutional resources may be critical to improving depressive symptoms related to violence perpetrated by an intimate partner, although further study is needed to identify appropriate screening methods and intervention types for women with such histories of abuse.
Acknowledgments
This research was supported by National Institute of Alcoholism and Alcohol Abuse Grant F31AA 018935-01A1 awarded to Lareina N. La Flair.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson DK, Saunders DG. Leaving an abusive partner: an empirical review of predictors, the process of leaving, and psychological well-being. Trauma Violence Abuse. 2003;4(2):163–191. doi: 10.1177/1524838002250769. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Barnett OW. Why Battered Women Do Not Leave, Part 2. Trauma, Violence, & Abuse. 2001:3–35. [Google Scholar]
- Bonomi AE, Thompson RS, Anderson M, Reid RJ, Carrell D, Dimer JA, et al. Intimate partner violence and women's physical, mental, and social functioning. Am J Prev Med. 2006;30(6):458–466. doi: 10.1016/j.amepre.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Bracken MI, Messing JT, Campbell JC, La Flair LN, Kub J. Intimate partner violence and abuse among female nurses and nursing personnel: prevalence and risk factors. Issues Ment Health Nurs. 2010;31(2):137–148. doi: 10.3109/01612840903470609. [DOI] [PubMed] [Google Scholar]
- Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O'Campo P, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162(10):1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Messing JT, Kub J, Agnew J, Fitzgerald S, Fowler B, et al. Workplace violence: prevalence and risk factors in the safe at work study. J Occup Environ Med. 2011;53(1):82–89. doi: 10.1097/JOM.0b013e3182028d55. [DOI] [PubMed] [Google Scholar]
- Carter AS, Martinez-Pedraza Fde L, Gray SA. Stability and individual change in depressive symptoms among mothers raising young children with ASD: maternal and child correlates. J Clin Psychol. 2009;65(12):1270–1280. doi: 10.1002/jclp.20634. [DOI] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23(4):260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Coker AL, Weston R, Creson DL, Justice B, Blakeney P. PTSD symptoms among men and women survivors of intimate partner violence: the role of risk and protective factors. Violence Vict. 2005;20(6):625–643. [PubMed] [Google Scholar]
- Crowne SS, Juon HS, Ensminger M, Burrell L, McFarlane E, Duggan A. Concurrent and long-term impact of intimate partner violence on employment stability. J Interpers Violence. 2011;26(6):1282–1304. doi: 10.1177/0886260510368160. [DOI] [PubMed] [Google Scholar]
- Fogarty CT, Fredman L, Heeren TC, Liebschutz J. Synergistic effects of child abuse and intimate partner violence on depressive symptoms in women. Prev Med. 2008;46(5):463–469. doi: 10.1016/j.ypmed.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Gielen AC, O'Campo PJ, Campbell JC, Schollenberger J, Woods AB, Jones AS, et al. Women's opinions about domestic violence screening and mandatory reporting. Am J Prev Med. 2000;19(4):279–285. doi: 10.1016/s0749-3797(00)00234-8. [DOI] [PubMed] [Google Scholar]
- Golding J. Intimate Partner Violence as a Risk Factor for Mental Disorders: A Meta-Analysis. Journal of Family Violence. 1999;14(2):99–132. [Google Scholar]
- Horwath E, Johnson J, Klerman GL, Weissman MM. Depressive symptoms as relative and attributable risk factors for first-onset major depression. Arch Gen Psychiatry. 1992;49(10):817–823. doi: 10.1001/archpsyc.1992.01820100061011. [DOI] [PubMed] [Google Scholar]
- Jewkes R. Intimate partner violence: causes and prevention. Lancet. 2002;359(9315):1423–1429. doi: 10.1016/S0140-6736(02)08357-5. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch Gen Psychiatry. 2003;60(8):789–796. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Prescott CA. Childhood sexual abuse, stressful life events and risk for major depression in women. Psychol Med. 2004;34(8):1475–1482. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the “kindling” hypothesis. Am J Psychiatry. 2000;157(8):1243–1251. doi: 10.1176/appi.ajp.157.8.1243. [DOI] [PubMed] [Google Scholar]
- Kernic MA, Holt VL, Stoner JA, Wolf ME, Rivara FP. Resolution of depression among victims of intimate partner violence: is cessation of violence enough? Violence Vict. 2003;18(2):115–129. doi: 10.1891/vivi.2003.18.2.115. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Justice AC, Rollman BL, McGinnis KA, Rabeneck L, Weissman S, et al. Clinical importance of HIV and depressive symptoms among veterans with HIV infection. J Gen Intern Med. 2002;17(7):512–520. doi: 10.1046/j.1525-1497.2002.10803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krantz G, Garcia-Moreno C. Violence against women. J Epidemiol Community Health. 2005;59(10):818–821. doi: 10.1136/jech.2004.022756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertin P, Mohr PB. A follow-up study of posttraumatic stress disorder, anxiety, and depression in Australian victims of domestic violence. Violence Vict. 2001;16(6):645–654. [PubMed] [Google Scholar]
- Minor KL, Champion JE, Gotlib IH. Stability of DSM-IV criterion symptoms for major depressive disorder. J Psychiatr Res. 2005;39(4):415–420. doi: 10.1016/j.jpsychires.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Resick PA, Nishith P. An exploration of comorbid depression among female victims of intimate partner violence with posttraumatic stress disorder. J Affect Disord. 2004;82(2):315–320. doi: 10.1016/j.jad.2004.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Sex differences in depression. Stanford University Press; Stanford, CA: 1990. [Google Scholar]
- O'Campo P, Burke J, Peak GL, McDonnell KA, Gielen AC. Uncovering neighbourhood influences on intimate partner violence using concept mapping. J Epidemiol Community Health. 2005;59(7):603–608. doi: 10.1136/jech.2004.027227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Campo P, Eaton WW, Muntaner C. Labor market experience, work organization, gender inequalities and health status: results from a prospective analysis of US employed women. Soc Sci Med. 2004;58(3):585–594. doi: 10.1016/s0277-9536(03)00230-2. [DOI] [PubMed] [Google Scholar]
- Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburua E, Martinez M. The impact of physical, psychological, and sexual intimate male partner violence on women's mental health: depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. J Womens Health (Larchmt) 2006;15(5):599–611. doi: 10.1089/jwh.2006.15.599. [DOI] [PubMed] [Google Scholar]
- Plichta SB. Intimate partner violence and physical health consequences. Journal of Interpersonal Violence. 2004;19(11):1296–1323. doi: 10.1177/0886260504269685. [DOI] [PubMed] [Google Scholar]
- Saltzman LE, Fanslow JL, McMahon PM, Shelley GA. Intimate partner violence surveillance: Uniform definitions and recommended data elements, version 1.0. In: Singer JD, Willet JB, editors. Applied longitudinal data analysis : modeling change and event occurrence. Oxford University Press; Oxford; New York: 2002. 2003. [Google Scholar]
- Soeken K, Parker B, McFarlane J, Lominak MC, editors. The abuse assessment screen: A clinical instrument to measure frequency, severity, and perpetrator of abuse against women. Sage; Newbury Park: 1998. [Google Scholar]
- Swenson SL, Rose M, Vittinghoff E, Stewart A, Schillinger D. The influence of depressive symptoms on clinician-patient communication among patients with type 2 diabetes. Med Care. 2008;46(3):257–265. doi: 10.1097/MLR.0b013e31816080e9. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Extent, nature and consequences of intimate partner violence: Findings from the national violence against women survey (NCJ 181867) National Institute of Justice; Washington, D.C.: 2000. [Google Scholar]
- Tram JM, Cole DA. A multimethod examination of the stability of depressive symptoms in childhood and adolescence. J Abnorm Psychol. 2006;115(4):674–686. doi: 10.1037/0021-843X.115.4.674. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. The stress process and the social distribution of depression. J Health Soc Behav. 1999;40(4):374–404. [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007;64(1):49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]